Abstract
Background
Late adolescence is a time of increased drinking, and alcohol plays a predominant role in college social experiences. Colleges seeking to prevent students’ hazardous drinking may elect to implement brief alcohol interventions (BAIs). However, numerous manualized BAIs exist, so an important question remains regarding the comparative effectiveness of these different types of BAIs for college students.
Aim
This study uses network meta-analyses (NMA) to compare seven manualized BAIs for reducing problematic alcohol use among college students.
Methods
We systematically searched multiple sources for literature, and we screened studies and extracted data in duplicate. For the quantitative synthesis, we employed a random-effects frequentist NMA to determine the effectiveness of different BAIs compared to controls, and estimated the relative effectiveness ranking of each BAI.
Results
A systematic literature search resulted in 52 included studies: on average, 58% of participants were male, 75% were binge drinkers, and 20% were fraternity/sorority-affiliated students. Consistency models demonstrated that BASICS was consistently effective in reducing students’ problematic alcohol use (ES range: g=−0.23, 95%CI [−0.36,−0.16] to g=−0.36, 95% CI [−0.55,−0.18]), but AlcoholEDU (g=−0.13, 95%CI [−0.22,−0.04]), e-CHUG (g=−0.35, 95%CI [−0.45,−0.05]), and THRIVE (g=−0.47, 95%CI [−0.60,−0.33]) were also effective for some outcomes. Intervention rankings indicated that BASICS, THRIVE, and AlcoholEDU hold the most promise for future trials.
Conclusions
Several BAIs appear effective for college students. BASICS was the most effective but is resource intensive and may be better suited for higher risk students; THRIVE and e-CHUG are less resource intensive and show promise for universal prevention efforts.
Keywords: Brief Alcohol Intervention, College Students, Network Meta-Analysis
Consumption of alcohol peaks for most people during late adolescence and early adulthood (SAMHSA, 2017), the developmental period in which many U.S. youth are enrolled in college. In 2016, approximately 11% of full-time college students reported heavy drinking and 38% of full-time college students reported binge drinking at least once in the past 30 days (SAMHSA, 2016a; 2016b). Drinking rates on college campuses over the past 30 years have remained fairly stable (Hingson & White, 2014), and evidence suggests that college students engage in heavier drinking than their non-student peers (Schulenberg, Johnston, O’Malley, Bachman, Meich, & Patrick, 2017). Given that college attendance is often a period of experimentation with alcohol, and that alcohol plays a predominant role in many college social experiences, college administrators often focus on harm reduction by implementing programs aimed at preventing hazardous or heavy levels of drinking. Hazardous drinking patterns such as binge drinking (i.e., drinking that brings blood alcohol concentration levels to 0.08 g/dL) can result in a variety of negative alcohol related consequences including aggression and assaultive behaviors, unplanned sex, injuries, sexual victimization, and future alcohol use disorder (Abbey et al., 2014; Jennison, 2004; Kingree & Thompson, 2015; Valenstein-Mah, Larimer, Zoellner, & Kaysen, 2015; Voloshyna, Bonar, Cunningham, Ilgen, Blow, & Walton, 2016; Wechsler, Davenport, Dowdall, Moeykens, & Castillo, 1994).
Prevention and Intervention
Given the public health impact of heavy and hazardous drinking among students, colleges and universities are increasingly implementing brief alcohol interventions (BAIs), broadly defined here as interventions delivered in a circumscribed time frame that aim to promote changes in alcohol use behaviors or their determinants. Evidence suggests that these briefer modalities may be preferable among this age group (Buscemi, Murphy, Martens, McDevitt-Murphy, Pederson, & Skidmore, 2010). A number of evidence-based BAIs exist, including manualized programs available for free or purchase.
One example of a highly studied BAI is the Brief Alcohol Screening Intervention for College Students (BASICS; Dimeff, Baer, Kivlahan, & Marlatt, 1999), which aims to reduce alcohol consumption and related negative consequences for students who already drink heavily or are at-risk of experiencing such problems. The intervention is typically delivered in two 50-minute counseling sessions, wherein the provider uses a motivational interviewing therapeutic style to enhance students’ motivations and skills to change drinking behaviors. Other manualized BAIs that are often implemented on college campuses include Alcohol 101/Alcohol 101 Plus (Century Council, 1997; 2003), AlcoholEdu (www.alcoholedu.com), Check Your Drinking (CYD; www.checkyourdrinking.net), Electronic CHECKUP TO GO (e-CHUG; www.e-chug.com), College Drinker’s Check-up (CDCU; www.collegedrinkerscheckup.com), and Tertiary Health Research Intervention Via Email (THRIVE; http://ceriph.curtin.edu.au/thrive). These BAIs vary in length between five minutes and two hours, and can vary in delivery mode and personnel; thus, effectiveness of these BAIs may differ for programs with different implementation features. For example, six of these seven BAIs involve computer activities, while BASICS is provided through an in-person encounter. THRIVE is the shortest, a five-minute survey, that gives brief personalized feedback, while the other computer programs are longer surveys with more comprehensive feedback or involve interactive decision making (e.g., such as at a bar). See Table 1 for other key components of these interventions. Additionally, other study and participant characteristics, such as study quality (e.g., allocation concealment to reduce selection bias: Pildal, Hrobjartsson, Jørgensen, Hilden, Altman, & Gøtzsche, 2007), length of time studied (Tanner-Smith & Lipsey, 2015), membership in a fraternity or sorority organization (Barry, 2007; Meisel & Barnett, 2017; Voloshyna, et al., 2016), or gender (Ham & Hope, 2003; Pederson, 2013), may also moderate the effectiveness of BAIs for college students.
Table 1.
Intervention Characteristics
| Brand | Aim | Description | Delivery | Dose |
|---|---|---|---|---|
| Alcohol 101/ Alcohol 101 Plus | Educate students about effects of alcohol misuse and “normal” peer drinking | 1. Make decisions for virtual characters at a party 2. Feedback given based on participant behavior and peer norms |
Interactive CD rom program set on a virtual campus | 45–60 minutes |
| AlcoholEdu | Alcohol misuse prevention course | 1. Pretest of alcohol knowledge 2. Precourse survey on drinking behavior, attitudes, demographics 3. Interactive alcohol education: students must receive a grade of ≥ 65% on postcourse knowledge test to pass |
Online | 2 hours |
| Brief Alcohol Screening and Intervention for College Students (BASICS) | Alcohol harm reduction | 1. Assessment of drinking patterns, attitudes, motivations 2. Feedback on personal risk factors and advice to moderate drinking |
Interviews; brief assessment survey | 2 interviews (50–60 minutes each) |
| Check Your Drinking (CYD) | Reduce high risk drinking | 1. Complete survey: demographics; drinking consumption, behavior, consequence 2. Personalized feedback and sensible drinking guidelines |
Online: http://www.checkyourdrinking.net | 15 minutes |
| Electronic CHECKUP TO GO (e-CHUG) | Personalized prevention intervention to motivate individuals to reduce alcohol or marijuana consumption | 1. Complete online assessment 2. Personalized feedback report: quantity/frequency drinking; comparison to U.S. drinking norms; estimated risk level (AUDIT score, genetic risk of alcoholism, tolerance); money per year on alcohol; cigarettes smoked per month; explanation, advice, local referral |
Online: http://www.echeckuptogo.com/usa/ | 20–30 minutes (optional 15–20 min. personal reflection) |
| College Drinker’s Check-up (CDCU) | Intervention for heavy drinking college students | Video “interviewer” gives instructions, offers encouragement and interpretive information about the feedback, and asks open-ended questions | CD (Windows) or Internet: http://www.collegedrinkerscheckup.com/ | 40 minutes |
| Tertiary Health Research Intervention Via Email (THRIVE) | Target unhealthy alcohol use in college students | 1. Complete survey: demographics; drinking last year; AUDIT; largest number of drinks consumed once last month, duration of the drinking episode, height weight; secondhand effects; opinions on alcohol beverage labeling; smoking history 2. Personalized feedback |
Online: http://ceriph.curtin.edu.au/thrive/ | 5 minutes |
Previous Syntheses and Extensions to Address Gaps
Meta-analytic reviews quantitatively synthesize findings across multiple primary studies, and thus provide a useful method for evaluating the current best evidence regarding intervention effectiveness and potential moderators of effects. Previous reviews demonstrate that alcohol interventions, including BAIs, can reduce drinking among college students (Carey, Scott-Sheldon, Garey, Elliott, & Carey, 2016; Fachini, Aliane, Martinez, & Furtado, 2012; Huh et al., 2015; Tanner-Smith & Lipsey, 2015). However, these reviews focus on comparing manualized interventions to a control group or a single suboptimal intervention(s); that is, they do not assess the relative effectiveness among manualized interventions and rank them accordingly. Thus, an assessment of which manualized BAI, if any, outperforms others will be useful for colleges wishing to maximize use of limited funds and most effectively change problematic drinking behaviors among students. Whereas traditional pairwise meta-analysis synthesizes direct evidence about a single intervention-comparison contrast (e.g., BASICS vs. e-CHUG reported in one or more trials), network meta-analysis (Petropoulou et al., 2017) can assess the comparative effectiveness of multiple interventions simultaneously by pooling direct and indirect evidence, as long as the included studies form a connected network of both direct and indirect information (Mavridis, Giannatsi, Cipriani, & Salanti, 2015). That is, a network meta-analysis incorporates (a) direct evidence from studies where two groups were compared with (b) indirect evidence, which is generated across evidence loops in a network where different studies compared different groups, but have at least one group in common with at least one other study in the network. For example, if the two BAIs, BASICS and e-CHUG, have both separately been compared with a common other treatment (AlcoholEdu), in two different sets of trials, then the relative effectiveness between BASICS and e-CHUG can be estimated indirectly through their common comparator, AlcoholEdu. Network meta-analyses can therefore provide more precise estimates of effects and permit comparison of interventions that were not directly compared in any one trial (Cipriani, Higgins, Geddes, & Salanti, 2013; Mavridis et al.2015). One key assumption of network meta-analysis is transitivity: i.e., the distributions of potential effect modifiers are balanced and randomly distributed across all pairwise comparisons within the network of interventions being compared (Salanti, 2012). Transitivity is empirically explored by comparing the distribution of pre-specified effect modifiers across treatment comparisons (Chaimani, Caldwell, Li, Higgins, & Salanti, 2017; Salanti, 2012). Network meta-analysis also assumes consistency in the network, which is the statistical manifestation of transitivity (Cipriani et al., 2013) whereby the direct and indirect evidence agree (Mavridis et al., 2015). In the methods section, we further discuss specific methods we used to assess whether these assumptions were met for this analysis.
Objective
This network meta-analysis examines the comparative effectiveness of seven manualized BAIs for college students, and aims to identify which of these BAIs are more or less effective in reducing students’ problematic alcohol consumption. The following BAIs were all initially identified by reviewing manualized programs developed specifically for use with college students from a comprehensive meta-analysis examining the overall effectiveness of BAIs for adolescents and young adults (see Tanner-Smith & Lipsey, 2015): Alcohol 101/Alcohol 101 Plus, AlcoholEdu, BASICS, CYD, CDCU, e-CHUG, and THRIVE. A new systematic literature search was then conducted to identify primary trials that evaluated the effects of those interventions (see methods). A secondary aim of the study is to assess whether heterogeneity in intervention effectiveness could be explained with any of the following factors: fraternity/sorority membership, sex (male/female), sample mandated to the intervention, and allocation concealment risk of bias.
Methods
The review protocol (including full strategy for our PubMed search) was registered in the online database for systematic reviews (see PROSPERO 2016 CRD42016035952 for the protocol and a link to the data and syntax needed to reproduce the analysis). The PRISMA-NMA statement document guided review steps and reporting (Hutton et al., 2015).
Eligibility Criteria
There were no geographic or language limitations on eligibility. Studies were eligible if they were conducted in 1980 or later to be relevant to current intervention practices. Eligible studies were those that assessed intervention effects for undergraduate college students from any country, who were no older than 30 years of age. Given the analytical assumptions required for a network meta-analysis, only randomized controlled trials (RCTs) were eligible for inclusion; that is, we only included RCTs due to their ability to reduce threats of selection bias and to prevent concerns that including multiple types of study design would further increase the chances of inconsistency. Eligible trials were those that evaluated one of the seven BAIs in Table 1 along with a comparison condition consisting of either a control group or an eligible comparator BAI. Finally, studies had to report at least one of the following alcohol consumption outcomes to be eligible for inclusion: (1) Frequency of heavy alcohol consumption (e.g., how many times per week a large number of drinks were consumed); (2) Quantity of alcohol consumption (e.g., number of drinks consumed in a week); and (3) Quantity of alcohol consumption during a peak drinking period (e.g., alcohol consumption at social events). Studies were ineligible if they only provided outcomes for a single occasion (e.g., 21st birthday celebration).
Information Sources and Search Strategy
Using a comprehensive search strategy, published and unpublished studies that met the above criteria were identified for inclusion in the review. The following electronic bibliographic databases were searched through April 18, 2016: ERIC, PsycARTICLES, PsycINFO, Sociological Abstracts, PubMed, Dissertation Abstracts International, Clinical Trials Register, and NIH RePORTER. Search terms were adapted to be appropriate for each database, but generally used three blocks of terms that described (1) intervention name, (2) alcohol outcomes, and (3) research design. The following gray literature sources were also searched: Australasian Medical Index, Campbell Collaboration Library, Cochrane Collaboration CENTRAL, College on Problems of Drug Dependence conference presentations, EPPI-Centre Database of Health Promotion Research, Google Scholar, Index to Theses in Great Britain and Ireland, International Clinical Trials Registry, NIAAA Web site, and SAMHSA Web site. Bibliographies of all screened and eligible studies and of prior narrative reviews and meta-analyses were reviewed. Hand searches of three journals were conducted: Alcoholism: Clinical and Experimental Research, American Journal on Addictions, and Journal of Substance Abuse Treatment.
Study Selection and Data Collection Process
All articles were double-screened for eligibility first at the title/abstract level; any potentially eligible articles were then double-screened for eligibility at the full-text level. After all eligibility decisions were completed, the research team coded information independently and in duplicate from the eligible study reports using a piloted, standardized coding protocol. At each stage of the process, disagreements were discussed until consensus was reached. If primary studies did not include the information needed to estimate effect sizes, primary study authors were contacted. We did not include studies for which data necessary to estimate effect sizes were not given or provided.
Data items
In addition to collecting data needed to estimate effect sizes, we also collected data on the following characteristics: participant demographics (age, percent male, White, fraternity/sorority membership, mandated sample); attrition; control group type; intervention name; intervention duration (minutes); time between intervention end and posttest (weeks); study location (site; country); study design (intent-to-treat [ITT] analysis [yes/no]; methods used to account for missing outcome data [type]; and monitoring of program fidelity [yes/no]).
Summary Measures
All effect sizes were transformed to the same metric, the standardized mean difference (SMD), to permit comparisons on group means measured using different continuous measurement scales (Lipsey & Wilson 2001). For binary outcomes, the Cox transformation was used to convert log odds ratio effect sizes into SMD effect sizes (Sánchez-Meca et al., 2003).
Synthesis of Results
Eligible outcomes were categorized into the three primary outcomes (frequency of heavy use, quantity, quantity during peak drinking episode) and analyzed separately, by three waves of follow-up timing (0–3 months post-intervention; 3–6 months post-intervention; 6+ months post-intervention), resulting in nine potential networks for analysis. If a study reported multiple follow-up points within the same wave, the follow-up with the shortest duration and/or most different in duration to the other studies in that category was dropped and only the longer/similar duration was used in the analysis. Sensitivity analyses for these outcomes were conducted.
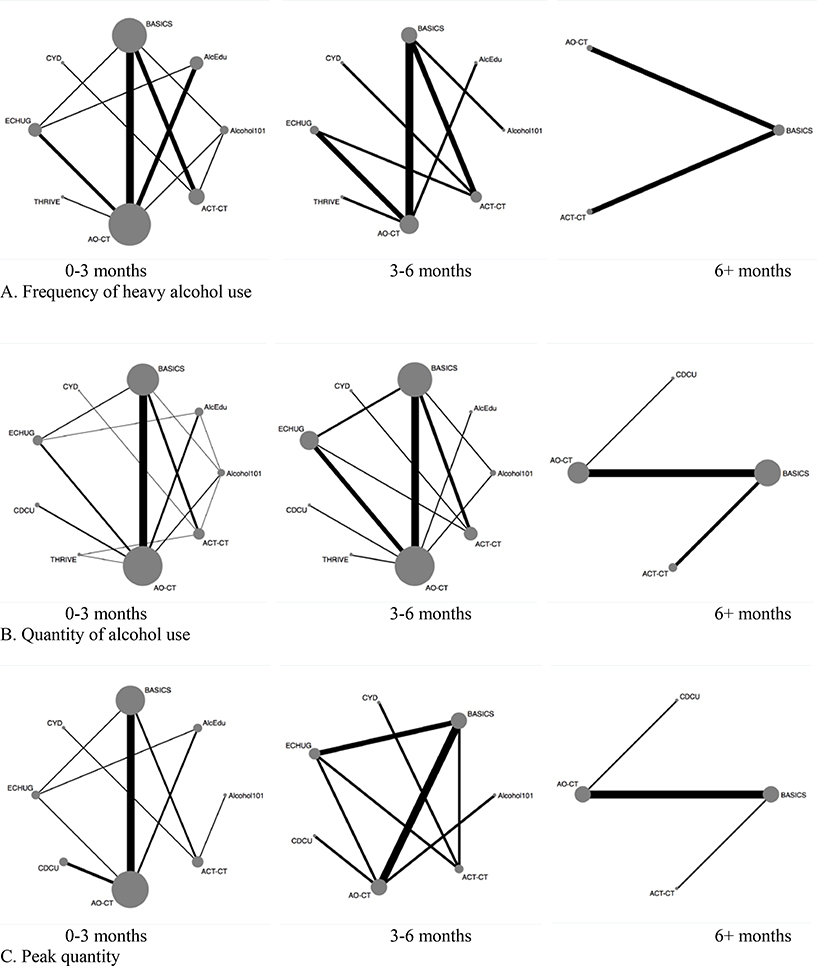
This study conducted network meta-analysis within a frequentist approach using the network package (White 2015) in StataSE (14.2; StatCorp, 2015). Network plots (Chaimani et al., 2013) are a visual tool to understand the components of a particular network of treatments and display the network size and comparisons of different interventions (see Figure 3): nodes (bubbles) specify each unique intervention and the number of studies providing information about that intervention (larger = more studies) whereas edges (lines) indicate the number of comparisons between different intervention/comparison groups (thicker = more comparisons). We used the multivariate random-effects meta-regression approach (White et al 2012) with the use of the network package in Stata (White 2015). This approach treats the possible comparisons within a multi-arm trial as different outcomes and proceeds to fitting the model taking the correlation between treatment effects within a multi-arm trial into account. We chose the assessment-only control group (AO-CT) as the reference group and estimated the effectiveness of each intervention relative to this group. To interpret the results, emphasis is given to the results from the consistency models, which are meta-analytic models generated from the pairwise estimates using direct, indirect, and mixed evidence; however, results from the treatment rankings based on inferences about each network using the surface area under the cumulative ranking curve (SUCRA; Salanti, Ades, & Ioannidis, 2011) are also presented. SUCRA values represent the percentage of effectiveness of a treatment in relation to an (imaginary) treatment that always performs the best with no uncertainty: thus, the highest SUCRA value indicates the most likely optimal treatment.1
Figure 3. Network plots for networks in main analysis, split by timing and outcome.
Note. Alcohol101 = Alcohol 101/Alcohol 101 Plus. AlcEDU = AlcoholEdu. AO-CT = Assessment-only control. ACT-CT = Active control. BASICS = Brief Alcohol Screening Intervention for College Students. CYD = Check Your Drinking. CDCU = College Drinker’s Check-up. ECHUG = Electronic CHECKUP TO GO. THRIVE = Tertiary Health Research Intervention Via Email.
A network meta-analysis includes additional analyses to assess whether transitivity and consistency assumptions are met. Namely, inconsistency statistics and plots assessed global inconsistency and (local) loop-specific heterogeneity (Chaimani et al., 2013; White, 2015). A global assessment of all inconsistency parameters, i.e., to reject the hypothesis of consistency across the network, is conducted using the Wald test statistic, which follows a χ2 distribution. In the inconsistency plots, an inconsistency factor (IF) is calculated as the absolute difference between direct and indirect evidence. Inconsistency factors closer to zero indicate that direct and indirect evidence are in agreement. Contribution plots, which demonstrate the influence of the direct, mixed, and indirect evidence sources in the network, were used to assess whether single comparisons were unduly influencing the results (Chaimani et al., 2013). Finally, node-splitting was conducted to assess the effect of leaving one study out of the network at a time: good model fit is indicated by non-significant χ2 test results (Dias, Welton, Caldwell, & Ades, 2010).
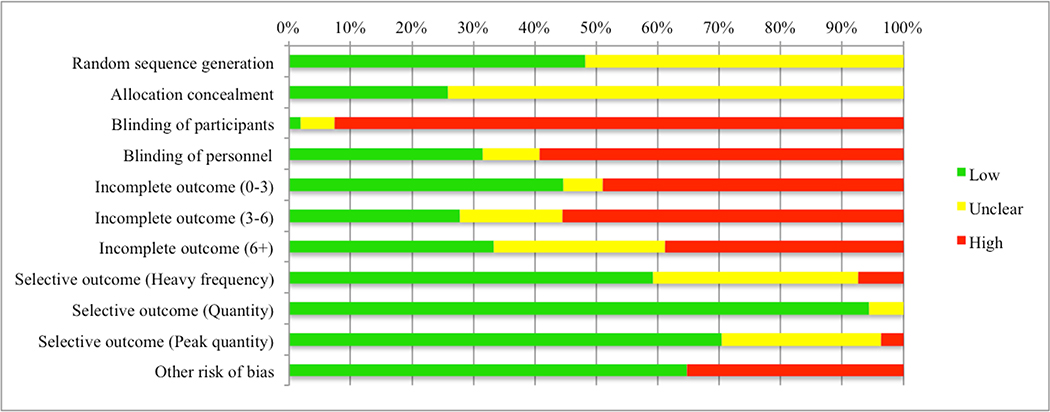
Study Quality and Risk of Bias Across Studies
Two independent raters used the Cochrane Risk of Bias tool to assess risk of bias (Higgins et al., 2011), modified to separately examine selective reporting for each of the three outcomes in the review and incomplete outcome data for each of the three waves selected. The tool was also modified to separately assess participant and personnel blinding.
Moderator and Sensitivity Analysis
Given the size of the networks and number of treatment comparisons included, multivariate meta-regression for moderators was not conducted. However, seven studies enrolled students who were mandated to the BAI2, so sensitivity analyses were conducted with these studies removed. Sensitivity analyses also examined networks where one follow-up outcome was dropped in studies with multiple effect sizes. The protocol specified additional sensitivity analyses, but we were unable to quantitatively explore these factors given the small size of the networks. Finally, we explored for small study effects as a proxy for assessing potential publication bias, using the contour enhanced funnel plot: this plot allows us explore if smaller studies more often show statistically significant results (Chaimani et al., 2013; Mavridis & Salanti, 2014; Peters, Sutton, Jones, Abrams, & Rushton, 2008).
Results
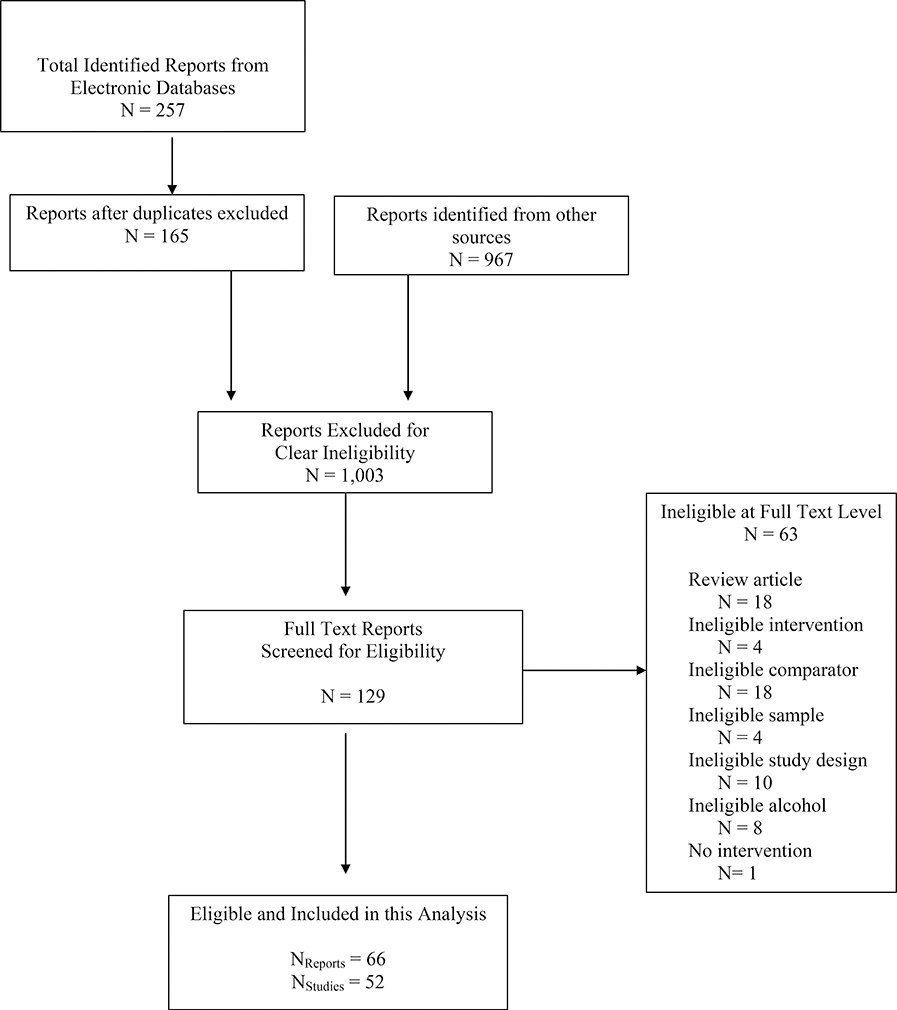
Of 1132 identified studies, 52 trials met the inclusion criteria for this network meta-analysis (Figure 1). Most studies involved pairwise comparisons, but three involved multi-arm trials (Appendix D provides study characteristics and effect sizes for every included study). Most studies utilized AO-CT groups (AO-CT; k = 39) and 14 utilized active comparison groups (ACT-CT). The BASICS (k = 34) and e-CHUG (k = 9) programs were the most prevalent interventions evaluated on college campuses, whereas the THRIVE program was the newest and least evaluated (k = 2). On average 58% of participants were male, 84% were White (k = 47), 75% were reported as hazardous drinkers at baseline, and 20% were fraternity/sorority organization members (k = 24).
Figure 1.
Study identification flow diagram.
Study Quality Assessment
Overall, the risk of bias was mixed across the studies (see Figure 2 for overall summary: see Appendix A, Table 4 for individual item ratings for each study). None of the studies were rated as high risk of bias for random sequence generation or allocation concealment, although a majority were rated unclear (52% and 74%, respectively). Participant and personnel blinding was uncommon, with participant blinding rated as high risk of bias in 93% of the studies. Risk of bias for incomplete outcome reporting did not vary substantially across the waves and ranged from 39–56% of studies at high risk of bias and 28–45% at low risk of bias. The majority of studies were ranked as low risk of bias in selective reporting for each of the outcomes. Other risks of bias were identified in 35% of studies, and included factors such as trialists’ potential conflicts of interest.
Figure 2.
Risk of Bias across included studies.
Primary Outcomes
Figure 3 displays a network plot for each of the nine unique networks; however, because several networks were fairly sparse and/or not well connected, we discuss the more connected networks in the text: frequency of heavy alcohol use (0–3 months), quantity of alcohol use (0–3 and 3–6 months), and quantity of alcohol use during peak consumption (0–3 months). We also conducted network meta-analysis for the networks of heavy frequency, 3–6 months post-intervention (k = 12) and quantity of use during peak consumption, 3–6 months post-intervention (k =11), the details of which are reported in full in Appendix B given the limited size of the networks. In brief, results from both networks indicated that no comparisons significantly reduced the occurrence of frequent heavy alcohol consumption or the quantity of alcohol consumption during peak drinking episodes for outcomes measured 3–6 months post-intervention. The following networks of outcomes for six or more months post-intervention were too sparse to be informative, although it is worth noting that they all primarily focused on BASICS: heavy frequency (k = 4), quantity of use, (k = 11), and quantity of use during peak consumption (k = 7).
Frequency of Heavy Alcohol Use: 0–3 Months
Frequency of heavy alcohol use outcomes measured at 0–3 months post-intervention represents a connected network (Fig. 3a) of 21 studies comparing six interventions, and the AO-CT and ACT-CT groups. Two studies were multi-arm trials. As the size of the nodes indicate, THRIVE and CYD were compared the least while BASICS was compared the most; indeed, the most informative direct evidence in this network was for BASICS versus ACT-CT (17.4% contribution). Results from the consistency model indicate that relative to the AO-CT, all comparisons reduced the frequency of heavy alcohol use (Table 2); yet, only three interventions significantly reduced the frequency of heavy drinking: BASICS (−0.36, 95% CI [−0.55, −0.18]), e-CHUG (−0.35, 95% CI [−0.59, −0.11]), and the ACT-CT (−0.29, 95% CI [−0.56, −0.02]). The global test for inconsistency was non-significant (χ2 (4) = 3.88, p = 0.4218) and there was no loop-specific inconsistency, indicating that the results from the direct and indirect estimates were largely consistent. Node-splitting also indicated that the consistency model fit well. When each intervention was ranked against all others, BASICS had the largest SUCRA value indicating it was most likely to be successful at reducing frequency of heavy alcohol use (Table 3): e-CHUG had the second largest. In sensitivity analysis, when the single study that utilized a mandated sample was dropped (Doumas et al., 2009), the CYD intervention was no longer included in the network, yet the results remained largely the same (Tables 2–3). Sensitivity analysis replacing the measurement duration from one study (4.3 versus 8.6 weeks: Terry, 2012) did not change the results (Tables 2–3).
Table 2.
Intervention effects compared to assessment-only control groups
| 0–3 Months | 0–3 Months | 3–6 Months | 0–3 Months | |||||||||
| Frequency | Quantity | Quantity | Peak quantity | |||||||||
| SMD | LCL | UCL | SMD | LCL | UCL | SMD | LCL | UCL | SMD | LCL | UCL | |
| Alc101 | −0.10 | −0.41 | 0.22 | −0.11 | −0.26 | 0.05 | −0.25 | −0.69 | 0.18 | 0.38 | −0.73 | 1.49 |
| AlcEDU | −0.04 | −0.15 | 0.06 | −0.13 | −0.22 | −0.04 | −0.07 | −0.55 | 0.42 | −0.41 | −0.84 | 0.02 |
| BASICS | −0.36 | −0.55 | −0.18 | −0.26 | −0.36 | −0.16 | −0.23 | −0.44 | −0.02 | −0.34 | −0.59 | −0.08 |
| CYD | −0.35 | −0.95 | 0.24 | −0.37 | −0.93 | 0.20 | −0.10 | −1.02 | 0.82 | 0.12 | −0.85 | 1.10 |
| e-CHUG | −0.35 | −0.59 | −0.11 | −0.25 | −0.45 | −0.05 | −0.12 | −0.39 | 0.16 | −0.33 | −0.86 | 0.21 |
| CDCU | NA | NA | NA | −0.19 | −0.43 | 0.05 | −0.08 | −0.74 | 0.59 | −0.36 | −0.76 | 0.05 |
| THRIVE | −0.15 | −0.44 | 0.14 | −0.47 | −0.60 | −0.33 | −0.47 | −0.95 | 0.02 | NA | NA | NA |
| ACT-CT | −0.29 | −0.56 | −0.02 | −0.18 | −0.39 | 0.02 | 0.03 | −0.36 | 0.42 | −0.17 | −0.77 | 0.43 |
| ES replaceda1 | ES replaceda2 | ES replaceda3 | ||||||||||
| SMD | LCL | UCL | SMD | LCL | UCL | SMD | LCL | UCL | ||||
| Alc101 | −0.10 | −0.41 | 0.21 | −0.11 | −0.26 | 0.05 | −0.28 | −0.62 | 0.06 | |||
| AlcEDU | −0.04 | −0.15 | 0.06 | −0.13 | −0.22 | −0.04 | −0.07 | −0.38 | 0.24 | |||
| BASICS | −0.36 | −0.55 | −0.18 | −0.26 | −0.36 | −0.16 | −0.21 | −0.37 | −0.04 | |||
| CYD | −0.36 | −0.96 | 0.23 | −0.36 | −0.93 | 0.20 | −0.11 | −0.91 | 0.70 | |||
| e-CHUG | −0.35 | −0.59 | −0.11 | −0.25 | −0.45 | −0.05 | −0.11 | −0.34 | 0.12 | |||
| CDCU | NA | NA | NA | −0.19 | −0.43 | 0.05 | −0.08 | −0.63 | 0.47 | |||
| THRIVE | −0.15 | −0.44 | 0.14 | −0.47 | −0.60 | −0.33 | −0.47 | −0.78 | −0.15 | |||
| ACT-CT | −0.30 | −0.57 | −0.03 | −0.18 | −0.39 | 0.02 | 0.03 | −0.28 | 0.33 | |||
|
Mandated removed |
Mandated removed |
Mandated removed |
Mandated removed |
|||||||||
| SMD | LCL | UCL | SMD | LCL | UCL | SMD | LCL | UCL | SMD | LCL | UCL | |
| Alc101 | −0.10 | −0.41 | 0.22 | −0.03 | −0.34 | 0.27 | −0.26 | −0.69 | 0.16 | 0.40 | −0.73 | 1.53 |
| AlcEDU | −0.04 | −0.15 | 0.06 | −0.16 | −0.29 | −0.03 | −0.07 | −0.53 | 0.40 | −0.41 | −0.85 | 0.03 |
| BASICS | −0.36 | −0.55 | −0.18 | −0.26 | −0.38 | −0.15 | −0.24 | −0.44 | −0.03 | −0.32 | −0.63 | 0.00 |
| CYD | NA | NA | NA | NA | NA | NA | −0.01 | −0.92 | 0.91 | NA | NA | NA |
| e-CHUG | −0.35 | −0.59 | −0.11 | −0.25 | −0.46 | −0.05 | −0.1 | −0.37 | 0.17 | −0.32 | −0.87 | 0.22 |
| CDCU | NA | NA | NA | −0.19 | −0.44 | 0.06 | −0.08 | −0.73 | 0.57 | −0.36 | −0.77 | 0.06 |
| THRIVE | −0.15 | −0.44 | 0.14 | −0.46 | −0.64 | −0.28 | −0.47 | −0.93 | 0.00 | NA | NA | NA |
| ACT-CT | −0.29 | −0.56 | −0.02 | −0.17 | −0.40 | 0.05 | 0.123 | −0.27 | 0.52 | −0.15 | −0.79 | 0.49 |
Note. Bolded effect sizes indicate intervention produced significant effects compared to assessment-only control groups.
Alcohol101 = Alcohol 101/Alcohol 101 Plus. AlcEDU = AlcoholEdu. AO-CT = Assessment-only control. ACT-CT = Active control. BASICS = Brief Alcohol Screening Intervention for College Students. CYD = Check Your Drinking. CDCU = College Drinker’s Check-up. ECHUG = Electronic CHECKUP TO GO. THRIVE = Tertiary Health Research Intervention Via Email.
This analysis involved replacing an effect size used in the original network analysis due to dependency between outcomes reported within the same follow-up wave category with the dropped effect size: (1.) One study replaced the 8.6 week follow-up ES with the 4.3 week follow-up. (2.) One study replaced the 8.6 week follow-up ES with the 4.3 week follow-up. (3). Three studies replaced the 25.8 week follow-up ES with the 12.9 week follow-up ES.
Table 3.
Treatment rankings
| 0–3 Months | 0–3 Months | 3–6 Months | 0–3 Months | |||||
| Heavy Frequency | Quantity | Quantity | Peak Quantity | |||||
| SUCRA | PrBest | SUCRA | PrBest | SUCRA | PrBest | SUCRA | PrBest | |
| Alc101 | 32.2 | 1.20 | 27.2 | 0.00 | 65.1 | 13.80 | 17.5 | 4.30 |
| AlcEDU | 23.0 | 0.00 | 33.5 | 0.00 | 41.8 | 4.30 | 74.6 | 25.90 |
| BASICS | 80.1 | 19.40 | 66.0 | 0.20 | 66.2 | 2.90 | 69.6 | 12.40 |
| CYD | 68.5 | 41.40 | 70.6 | 36.20 | 46.9 | 17.70 | 28.3 | 5.50 |
| e-CHUG | 76.3 | 27.70 | 62.8 | 2.10 | 48.5 | 1.40 | 65 | 21.70 |
| CDCU | NA | NA | 47.4 | 1.00 | 42.7 | 10.20 | 67.7 | 21.20 |
| THRIVE | 42.8 | 3.60 | 94.7 | 60.30 | 85.3 | 49.50 | NA | NA |
| ACT-CT | 65.9 | 6.70 | 44.4 | 0.20 | 26.7 | 0.20 | 50.6 | 9.00 |
| AO-CT | 11.1 | 0.00 | 3.6 | 0.00 | 27.0 | 0.00 | 26.6 | 0.00 |
| ES removeda1 | ES removeda2 | ES removeda3 | ||||||
| SUCRA | PrBest | SUCRA | PrBest | SUCRA | PrBest | |||
| Alc101 | 31.4 | 1.40 | 28.9 | 0.00 | 70.5 | 13.00 | ||
| AlcEDU | 22.7 | 0.00 | 32.6 | 0.00 | 39.9 | 1.20 | ||
| BASICS | 80.0 | 19.50 | 65.7 | 0.30 | 65.1 | 1.10 | ||
| CYD | 70.6 | 41.20 | 69.2 | 35.90 | 46.6 | 17.20 | ||
| e-CHUG | 76.0 | 25.80 | 61.9 | 3.40 | 46.1 | 0.60 | ||
| CDCU | NA | NA | 47.4 | 1.40 | 43.8 | 7.10 | ||
| THRIVE | 40.6 | 4.30 | 94.1 | 58.80 | 91.4 | 59.60 | ||
| ACT-CT | 67.7 | 7.80 | 46.3 | 0.20 | 22.4 | 0.20 | ||
| AO-CT | 11.0 | 0.00 | 4.0 | 0.00 | 24.3 | 0.00 | ||
| Mandated removed | Mandated removed | Mandated removed | Mandated removed | |||||
| SUCRA | PrBest | SUCRA | PrBest | SUCRA | PrBest | SUCRA | PrBest | |
| Alc101 | 33.5 | 2.40 | 19.1 | 0.80 | 68.4 | 15.50 | 14.4 | 4.80 |
| AlcEDU | 24.8 | 0.00 | 43.6 | 0.10 | 43.3 | 4.90 | 73.9 | 29.10 |
| BASICS | 85.9 | 38.10 | 70.3 | 2.20 | 68.3 | 4.20 | 64.5 | 9.80 |
| CYD | NA | NA | NA | NA | 41.7 | 12.60 | NA | NA |
| e-CHUG | 80.1 | 36.20 | 64.5 | 7.70 | 46.9 | 1.20 | 62.6 | 21.80 |
| CDCU | NA | NA | 49.9 | 3.90 | 46.9 | 10.10 | 67.6 | 25.00 |
| THRIVE | 44.2 | 5.50 | 96.9 | 84.10 | 86.9 | 51.50 | NA | NA |
| ACT-CT | 70.1 | 17.80 | 47.0 | 1.20 | 18.1 | 0.00 | 45.5 | 9.50 |
| AO-CT | 11.4 | 0.00 | 8.6 | 0.00 | 29.7 | 0.00 | 21.6 | 0.00 |
Note. SUCRA = Surface under the curve. PrBest = Probability that the treatment will perform the best. Bolded values indicate highest SUCRA value of that intervention in that network. NA = not applicable due to the intervention not being included in that network analysis. Alcohol101 = Alcohol 101/Alcohol 101 Plus. AlcEDU = AlcoholEdu. AO-CT = Assessment-only control. ACT-CT = Active control. BASICS = Brief Alcohol Screening Intervention for College Students. CYD = Check Your Drinking. CDCU = College Drinker’s Check-up. ECHUG = Electronic CHECKUP TO GO. THRIVE = Tertiary Health Research Intervention Via Email.
Replaced an effect size used in the original network analysis with the dropped effect size: (1.) One study replaced the 8.6 week follow-up ES with the 4.3 week follow-up. (2.) One study replaced the 8.6 week follow-up ES with the 4.3 week follow-up. (3). Three studies replaced the 25.8 week follow-up ES with the 12.9 week follow-up ES.
Quantity of Alcohol Use: 0–3 Months
Quantity of alcohol use measured at 0–3 months post-intervention is a connected network (Fig. 3b) of 37 studies comparing all seven eligible interventions and both types of control groups. This network also included three multi-arm trials. As the size of the nodes indicate, CYD was compared the least while BASICS was compared the most; indeed, the most informative direct evidence in this network was for the BASICS intervention versus AO-CT (16.3% contribution). Results from the consistency model indicate that relative to the AO-CT, only THRIVE (−0.47, 95% CI [−0.60, −0.33]), BASICS (−0.26, 95% CI [−0.36, −0.16]), e-CHUG (−0.25, 95% CI [−0.45, −0.05]), and AlcoholEdu (−0.13, 95% CI [−0.22, −0.04]) significantly reduced the quantity of alcohol use when compared to the AO-CT group (Table 2). The global test for inconsistency was non-significant (χ2 (6) = 3.68, p = 0.7194), and there was no loop-specific inconsistency, indicating that the results from the direct and indirect estimates were largely consistent. Node-splitting also supported the consistency model. When compared against all other interventions, THRIVE had the largest SUCRA value, followed by CYD (Table 3). Removing the six studies with a mandated sample from this network3, resulted in removing the CYD intervention, but the results remained largely the same (Tables 2–3). Sensitivity analysis replacing the measurement duration in one study (4.3 versus 8.6 weeks: Terry, 2012) did not change the final model results.
Quantity of Alcohol Use: 3–6 months
Quantity of alcohol use measured between 3–6 months post-intervention is a connected network (Fig. 3b) of 21 studies comparing all 7 interventions and both types of control groups. As the size of the nodes indicate, CDCU, CYD, and THRIVE were compared the least while BASICS was compared the most, followed by e-CHUG. The most informative direct evidence in this network was for the e-CHUG intervention versus AO-CT with a total contribution of only 14.4% to network estimates. Results from the consistency model indicate that relative to the AO-CT (Table 2), only the BASICS intervention significantly reduced the quantity of alcohol use (−0.23, 95% CI [−0.44, −0.02]). The global test for inconsistency was non-significant (χ2 (3) = 1.57, p = 0.6657) and there was no significant loop-specific inconsistency. However, the confidence interval for the Alcohol 101, BASICS, and AO-CT loop was large (IF = 0.55, 95% CI [0.00, 1.70]) because, although BASICS was compared often, only two studies with inconsistent results assessed Alcohol 101. Node-splitting, however, supported the consistency model. When compared against all other interventions, THRIVE held the largest SUCRA value (Table 3). Both sensitivity analyses for this network produced similar results to the original analyses, but when the single study that utilized a mandated sample was dropped (Logan et al., 2015), THRIVE now significantly reduced drinking compared to the AO-CT (Table 2). Sensitivity analysis replacing the measurement duration in three studies (12.9 versus 25.8 weeks4) demonstrated that THRIVE produced significantly reduced results compared to the AO-CT (Table 2).
Quantity of Alcohol Use During Peak Consumption: 0–3 months
Quantity of alcohol use during peak consumption measured at 0–3 months post-intervention is a connected network (Fig. 3c) of 18 studies comparing six interventions and both types of control groups. This network included one multi-arm trial. As the size of the nodes indicate, Alcohol101 and CYD were compared the least while BASICS was compared the most; indeed, BASICS comparisons contributed a larger amount of direct evidence in this network compared to the other networks (21.3% compared to AO-CT and 21.7% compared to ACT-CT groups), suggesting that these results should be interpreted with caution. Results from the consistency model indicated that relative to the AO-CT (Table 2), only the BASICS intervention produced significantly improved results from the AO-CT (−0.34, 95% CI [−0.59, −0.08]). The global test for inconsistency was non-significant (χ2 (2) = 0.29, p = 0.8639), and there was no significant loop-specific inconsistency; however, the confidence interval for the BASICS, e-CHUG, AO-CT loop was large (IF = 0.25, 95% CI [0.00, 1.91]). In this network, two trials utilizing e-CHUG had inconsistent results (in opposite directions) but null in both cases. Thus, the loop-specific findings suggest caution when comparing e-CHUG to other interventions in this network. Node-splitting supported the consistency model. When compared against all other interventions AlcoholEDU had the largest SUCRA value (Table 3). Removing the four studies that utilized a mandated sample from this network5, removed the sole comparison involving CYD and three comparisons of BASICS, but did not substantively change the model results (Tables 2–3).
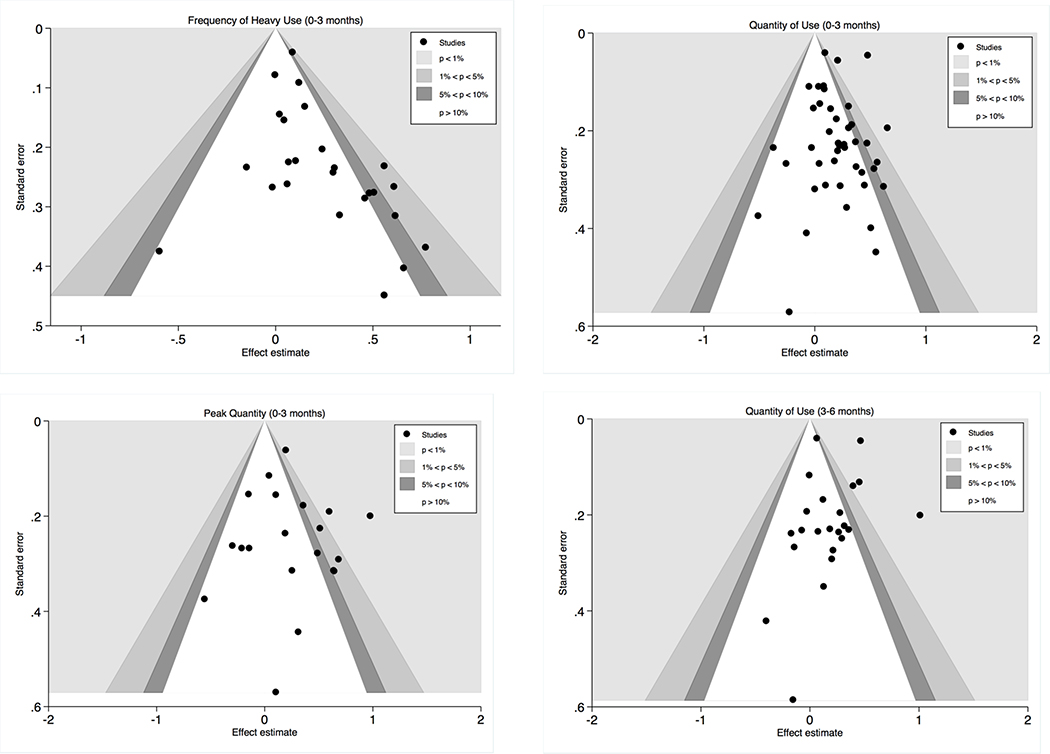
Small Study Bias
Funnel plots demonstrated potential small study bias for frequency of heavy alcohol use and peak quantity of alcohol use, with gaps in negative effect sizes among small studies. Funnel plots for quantity of alcohol use outcomes appeared symmetrical, although gaps in the bottom half of the funnel plots suggest that some small studies may be missing (Appendix A, Figure 4). However, overall, most studies appear in the statistically non-significant area of the figure and smaller studies do not appear to show statistically significant results more than larger studies.
Discussion
This network meta-analysis examined the comparative effectiveness of seven manualized BAIs for college students, in an effort to identify which BAIs may be more or less effective in reducing college students’ problematic alcohol use. The results indicated that the AlcoholEDU, BASICS, e-CHUG, and THRIVE interventions all led to reduced problematic alcohol use among college students, relative to AO-CT groups for outcomes measured 0–3 months post-intervention. However, only the BASICS intervention consistently led to reductions across all alcohol outcomes, including heavy frequency, quantity, and quantity during a peak drinking episode. Relative to AO-CT conditions, the AlcoholEDU and e-CHUG interventions were effective in the short term for reducing heavy frequency and quantity of alcohol use, respectively. AlcoholEDU, however, had the smallest reduction in use compared to the three other successful interventions. Finally, THRIVE yielded significant benefits over AO-CT groups for short-term quantity outcomes and these effects were nearly double the magnitude of those observed for the other successful interventions. Sensitivity analyses also indicated that THRIVE may be particularly effective for non-mandated college students. Evidence from the studies with longer outcomes was sparse and did not suggest any one intervention was most effective.
When all seven BAIs were ranked in terms of effectiveness, AlcoholEDU, BASICS, and THRIVE ranked the best, but the rankings varied by type of alcohol consumption outcome. That is, BASICS had the largest SUCRA value for frequency of heavy use, THRIVE the largest for quantity of alcohol use, and AlcoholEdu the largest for peak drinking quantity. However, e-CHUG and CYD also had higher SUCRA values and BASICS maintained high SUCRA values across all outcomes. The rankings are estimates of potential future intervention effectiveness that are based on evidence from direct and indirect evidence. Thus, given the size of these networks and availability of treatment comparisons, the rankings should be interpreted with caution.
One important finding to note from the current study is that, among these seven manualized BAIs, the programs varied in their success by the different measures of alcohol consumption, a finding that has previously been demonstrated in the BAI literature (Tanner-Smith & Risser, 2016). Namely, this review purposely examined three different measures of problematic alcohol use. Although we anticipated that the BAIs may have operated similarly across all measures of problematic drinking, the results indicated that the mechanisms of change associated with BAIs likely vary depending on the measure of problematic drinking. All of the included BAIs reported using some form of personalized feedback, so different results could be due to better/worse tailoring by the particular intervention. That is, BASICS could be more effective because of the in-person interview component, which may provide better tailoring. It may also take a stronger intervention dose (e.g., BASICS) to change the frequency of heavy drinking, e.g., by working with students to change factors leading them to environments where heavy drinking may be encouraged, while briefer, online assessments (e.g., THRIVE) may be more appropriate for enabling students to reflect on their drinking habits and consequently drink less when engaged in social drinking situations.
Limitations
This review focused only on seven manualized BAIs, and thus it is unclear how these BAIs compare to other manualized or non-manualized BAIs. Given that the BASICS trials included in this review tended to enroll heavier drinking/mandated students, future researchers may need to consider whether these follow-up effects generalize to other populations of college students. Of note, this review did not assess frequency of any type of alcohol use outcomes so intervention effectiveness rankings might change if we focused on that outcome. Although we sought to identify published and unpublished sources through a comprehensive and systematic literature search, there remains a potential that we missed eligible studies due to not exhaustively searching all available databases (e.g., Embase) or of small study bias in this research area. Despite the sole inclusion of RCT designs, the risk of bias was mixed and trials often did not report enough information to accurately assess risk of bias. Although often not feasible to blind participants in behavioral intervention research (e.g., see Grant, Pedersen, Osilla, Kulesza, & D’amico, 2016), blinding of study personnel is often possible, but was uncommon in the included trials.
Conclusions
This network meta-analysis builds on previous reviews by directly comparing multiple interventions for problematic alcohol use among college students and highlighting what interventions might be best for which type of risky consumption. The results indicated that the BASICS intervention yielded the most consistent beneficial effects in terms of reducing problematic alcohol use among college students, yet AlcoholEDU, CYD, e-CHUG, and THRIVE also performed well and may be particularly useful for universal prevention efforts. Given the few studies on THRIVE and CYD that nevertheless suggest their effectiveness, future research with these interventions is warranted, especially because these interventions are less resource intensive than the BASICS intervention. Considering the effectiveness-resource tradeoff, universities may choose to implement e-CHUG as a form of universal prevention and implement BASICS for smaller groups of higher risk students (e.g., mandated students). Of note, few trials employed long-term follow-up designs. Thus, although the current study finds that some BAIs may be effective in the short term, it is unclear how most BAIs perform beyond three months. Finally, one important future direction for research will be examining specific mechanisms of these interventions as well as whether these interventions are effective for reducing problematic drinking patterns among subpopulations of college students.
Acknowledgments
a. Funding - Funding for the original review was provided by the National Institute on Alcohol Abuse and Alcoholism (NIAAA) Grant 1R01AA020286-01A1. (2011-2015)
Appendix A
Table 4.
Risk of bias
| Study | Random sequence generation | Allocation Concealment | Participant blinding | Personnel blinding | Incomplete outcome | Selective outcome reporting | |||||
| 0–3 mos | 3–6 mos | 6+ mos | Heavy frequency | Quantity | Quantity during peak drinking | Other risk of bias identified | |||||
| Alfonso et al., 2012 | Low | Unclear | High | High | Unclear | Unclear | N/A | Unclear | Low | Low | No |
| Baer et al., 1995; 2001; Roberts et al., 2000 | Low | Unclear | Unclear | High | N/A | Low | Low | Unclear | Low | Low | Yes |
| Borsari & Carey, 2000; Borsari et al., 2009 | Low | Unclear | High | High | Low | N/A | Unclear | Low | Low | Unclear | No |
| Bowley et al., 2013 | Unclear | Unclear | High | Unclear | Low | N/A | N/A | Unclear | Low | Unclear | No |
| Braitman, 2012 | Unclear | Unclear | High | Unclear | High | N/A | N/A | Low | Low | Low | No |
| Bryant, 2009; Bryant et al., 2013 | Unclear | Unclear | High | High | High | N/A | N/A | Low | Low | Unclear | No |
| Butler, 2007; Butler & Correia, 2009 | Unclear | Unclear | High | High | High | N/A | N/A | Low | Low | Low | No |
| Carey et al., 2011; Carey & DeMartini, 2010; Reid et al., 2015 | Unclear | Unclear | High | Low | Low | High | High | Unclear | Unclear | Unclear | No |
| Croom et al., 2009 | Unclear | Unclear | High | Low | High | N/A | N/A | Low | Unclear | Unclear | Yes |
| Dimeff, 1997; Dimeff & McNeely, 2000 | Low | Low | High | Low | High | N/A | N/A | Low | Low | Low | Yes |
| Doumas & Andersen, 2009 | Unclear | Low | High | High | High | N/A | N/A | Low | Low | Unclear | Yes |
| Doumas & Haustveit, 2008 | Unclear | Unclear | High | Low | High | N/A | N/A | Unclear | Low | Low | Yes |
| Doumas et al., 2009 | Low | Unclear | High | Low | Low | N/A | N/A | Low | Low | Low | No |
| Doumas et al., 2010 | Unclear | Unclear | High | Low | Low | Low | N/A | Low | Low | Low | No |
| Doumas et al., 2011; 2014 | Low | Unclear | High | Unclear | High | N/A | N/A | Low | Low | Low | Yes |
| Eggleston, 2007 | Unclear | Unclear | High | High | N/A | High | N/A | Low | Low | Unclear | No |
| Fernandez et al., 2011; Wood et al., 2010 | Low | Unclear | High | High | N/A | N/A | Low | Low | Low | High | No |
| Geisner, 2008 | Low | Unclear | High | Low | Low | N/A | N/A | Unclear | Low | Low | No |
| Grossbard et al., 2010; Tollison et al., 2013 | Low | Low | High | High | N/A | N/A | Unclear | High | Low | Low | Yes |
| Hallett et al., 2009; Hustad & Borsari, 2010; Kypri et al., 2009 | Low | Low | Low | Low | Low | High | N/A | Low | Low | Low | Yes |
| Henslee et al., 2006 | Unclear | Unclear | High | Low | High | N/A | N/A | Low | Low | Low | No |
| Henslee, 2008; Henslee & Correia, 2009 | Unclear | Unclear | High | High | High | N/A | N/A | Low | Low | Low | No |
| Hester et al., 2012 | Unclear | Unclear | High | High | Low | N/A | Low | Unclear | Low | Low | Yes |
| Hester et al., 2012 | Unclear | Unclear | High | Low | Low | N/A | Low | Unclear | Low | Low | Yes |
| Study | Random sequence generation | Allocation Concealment | Participant blinding | Personnel blinding | Incomplete outcome | Selective outcome reporting | |||||
| 0–3 mos | 3–6 mos | 6+ mos | Heavy frequency | Quantity | Quantity during peak drinking | Other risk of bias identified | |||||
| Horner, 2010 | Unclear | Unclear | High | High | High | N/A | N/A | Unclear | Low | Low | No |
| Hustad et al., 2010 | Low | Low | High | Low | Low | N/A | N/A | Low | Low | Low | Yes |
| Juarez, 2001; Juarez et al., 2006 | Unclear | Unclear | High | High | High | N/A | N/A | Low | Unclear | High | Yes |
| Kerr-Corrêa et al., 2008; Simão et al., 2008 | Unclear | Unclear | High | High | N/A | N/A | High | Low | Low | Low | No |
| Kulesza et al., 2010 | Unclear | Unclear | High | High | Low | N/A | N/A | Unclear | Low | Unclear | No |
| Kulesza et al., 2013 | Unclear | Unclear | High | High | Low | N/A | N/A | High | Low | Unclear | Yes |
| LaBrie et al.,, 2013 | Low | Low | High | Low | Low | Unclear | Unclear | Unclear | Low | Low | No |
| Larimer et al., 2001; O’Leary et al., 2002 | Unclear | Unclear | High | High | N/A | N/A | Unclear | Low | Low | Low | Yes |
| Larimer et al., 2007 | Low | Low | High | Low | N/A | N/A | High | Low | Low | Low | No |
| Lau, 2006; Lau-Barraco & Dunn, 2008 | Unclear | Unclear | High | High | Low | N/A | N/A | Low | Low | Unclear | No |
| Leffingwell et al., 2005 | Unclear | Unclear | High | Low | Low | Low | Unclear | Unclear | Low | Low | No |
| Logan, 2013; Logan et al., 2015 | Unclear | Unclear | High | High | High | High | N/A | Unclear | Low | Low | Yes |
| Lovecchio, 2009; Lovecchio et al., 2010 | Low | Low | High | Low | High | N/A | N/A | Low | Low | Low | No |
| Martin, 2014 | Unclear | Unclear | Unclear | Unclear | Unclear | N/A | N/A | Low | Low | Low | No |
| Mastroleo, 2008; Orchowski et al., 2012 | Low | Unclear | High | High | Low | N/A | N/A | Low | Low | Low | No |
| Matteucci et al., 2016; Paschall et al., 2011a; 2011b; 2014 | Unclear | Unclear | High | Low | Low | High | High | Low | Low | Low | Yes |
| McNally, 2003; Mcnally et al., 2005 | Unclear | Unclear | High | High | Low | N/A | N/A | Low | Low | Unclear | No |
| McPherson, 2012 | Low | Unclear | High | High | High | N/A | N/A | Unclear | Low | Low | Yes |
| Miller, 2000 | Low | Unclear | Unclear | Unclear | Low | Low | Low | Unclear | Low | Low | No |
| Monahan et al., 2013; Murphy et al., 2010; 2015 | Low | Low | High | High | High | High | N/A | Low | Low | Unclear | No |
| Murphy et al., 2001 | Unclear | Unclear | High | High | Low | N/A | Low | Low | Low | Unclear | No |
| Schaus et al., 2009 | Low | Low | High | High | High | High | High | Low | Low | Low | No |
| Teeters et al., 2015 | Low | Low | High | High | Low | Low | N/A | Low | Low | Unclear | No |
| Study | Random sequence generation | Allocation Concealment | Participant blinding | Personnel blinding | Incomplete outcome | Selective outcome reporting | |||||
| 0–3 mos | 3–6 mos | 6+ mos | Heavy frequency | Quantity | Quantity during peak drinking | Other risk of bias identified | |||||
| Terlecki et al., 2008; Terlecki et al., 2011 | Low | Low | High | High | High | N/A | N/A | High | Low | Low | Yes |
| Terlecki et al., 2015 | Low | Unclear | High | High | High | High | High | Unclear | Low | Low | No |
| Terlecki, 2008; Terlecki et al., 2010; 2012 | Low | Low | High | High | High | N/A | N/A | High | Low | Low | Yes |
| Terlecki, 2011 | Low | Unclear | High | High | High | High | High | Unclear | Low | Low | No |
| Terry, 2012 | Low | Low | High | High | High | N/A | N/A | Low | Low | Low | No |
| Walters et al., 2007 | Unclear | Unclear | High | Low | Unclear | Unclear | N/A | Unclear | Low | Low | No |
| Whiteside, 2010 | Low | Unclear | High | High | High | High | N/A | Low | Low | Low | No |
Figure 4.
Assessment of small study bias: Contour enhanced funnel plots for networks in main analysis, split by timing and outcome
Appendix B
Additional Networks
Frequency of Heavy Alcohol Use: 3–6 Months
Frequency of heavy alcohol use outcomes measured at 3–6 months post-intervention represents a limited network (Fig. 3a) of 12 studies comparing five interventions, and the AO-CT and ACT-CT groups. As the size of the nodes indicate, BASICS was compared the most while the other interventions were only studied once, with the exception of e-CHUG, which was included in two trials. The most informative direct evidence in this network was for BASICS versus AO-CT as it contributed 20.9%, which is likely overly influential given the representation of other interventions in this network. Results from the consistency model indicate that relative to the AO-CT, no comparisons significantly reduced the frequency of heavy drinking (Table B1). The global test for inconsistency was non-significant (χ2 (1) = 0.03, p = 0.8518), and for the single loop available, there was no evidence of loop-specific inconsistency. Node-splitting also indicated that the consistency model fit well. When compared against all other interventions BASICS had the largest SUCRA value, followed by THRIVE (Table B2).
Sensitivity analysis: Frequency of heavy alcohol use, 3–6 months
Sensitivity analysis replacing the measurement duration from one study (12.9 versus 25.8 weeks: Schaus et al., 2009) did not change the results (Table B2).
Quantity of Alcohol Use During Peak Consumption: 3–6 months
Quantity of alcohol use during peak consumption measured at 3–6 months post-intervention is a network (Fig. 3c) of 11 studies comparing five interventions and both types of control groups. As the size of the nodes indicate, BASICS was compared the most while the other interventions were only studied once, with the exception of e-CHUG, which was included in four trials. The most informative direct evidence in this network was for e-CHUG versus AO-CT as it contributed 17.3%. Results from the consistency model indicate that relative to the AO-CT, no comparisons significantly reduced the quantity of alcohol consumption during peak drinking episodes (Table B1). The global test for inconsistency was non-significant (χ2 (2) = 1.73, p = 0.4216); however, one loop (BASICS, e-CHUG, ACT-CT) demonstrated significant inconsistency (IF = 1.04, 95% CI [0.42, 1.65]). Node-splitting, however, supported the consistency model. When compared against all other interventions BASICS had the largest SUCRA value, followed by Alcohol101 (Table B2).
Sensitivity analysis: Quantity of alcohol use during peak consumption, 3–6 months
Removing the two studies that utilized a mandated sample from this network (Alfonso et al., 2012; Horner, 2010), resulted in removing one comparison involving e-CHUG and two comparisons of BASICS, but did not substantively change the model results (Table B2). The global test for inconsistency remained non-significant (χ2 = 2.35, df = 2, p = 0.3086). There was, however, evidence of significant loop-specific inconsistency for two evidence loops: (1) BASICS, e-CHUG, ACT-CT, IF = 1.89, 95% CI [0.59, 3.20]) and (2) BASICS, e-CHUG, AO-CT, IF = 0.87, 95% CI [0.00, 2.17].
Sensitivity analysis replacing the measurement duration from three studies (12.9 versus 25.8 weeks: Labrie et al., 2013; Schaus et al., 2009; Terlecki et al., 2015) did not change the results of the effects compared to the AO-CT, but Alcohol101 and BASICS switched their rankings such that Alcohol 101 had the largest SUCRA value (Table B2).
Table B1.
Intervention effects compared to assessment-only control groups
| 3–6 Months | 3–6 Months | |||||
| Heavy Frequency |
Peak quantity |
|||||
| SMD | LCL | UCL | SMD | LCL | UCL | |
| Alc101 | 0.33 | −0.22 | 0.87 | −0.42 | −1.48 | 0.64 |
| AlcEDU | 0.05 | −0.03 | 0.13 | NA | NA | NA |
| BASICS | −0.05 | −0.28 | 0.18 | −0.36 | −0.94 | 0.22 |
| CYD | 0.49 | −0.27 | 1.25 | 0.30 | −1.26 | 1.87 |
| e-CHUG | 0.04 | −0.24 | 0.33 | −0.16 | −0.91 | 0.59 |
| CDCU | NA | NA | NA | 0.27 | −0.85 | 1.40 |
| THRIVE | −0.07 | −0.40 | 0.26 | NA | NA | NA |
| ACT-CT | 0.42 | 0.09 | 0.76 | 0.41 | −0.55 | 1.36 |
| ES replaceda1 | ES replaceda2 | |||||
| SMD | LCL | UCL | SMD | LCL | UCL | |
| Alc101 | 0.33 | −0.22 | 0.87 | −0.42 | −0.99 | 0.14 |
| AlcEDU | 0.05 | −0.03 | 0.13 | NA | NA | NA |
| BASICS | −0.05 | −0.28 | 0.18 | −0.22 | −0.55 | 0.11 |
| CYD | 0.43 | −0.33 | 1.19 | −0.13 | −1.13 | 0.88 |
| e-CHUG | 0.04 | −0.24 | 0.33 | −0.17 | −0.62 | 0.28 |
| CDCU | NA | NA | NA | 0.27 | −0.41 | 0.96 |
| THRIVE | −0.07 | −0.40 | 0.26 | NA | NA | NA |
| ACT-CT | 0.37 | 0.05 | 0.68 | −0.03 | −0.56 | 0.51 |
| Mandated removed |
||||||
| SMD | LCL | UCL | ||||
| Alc101 | −0.42 | −1.66 | 0.82 | |||
| AlcEDU | NA | NA | NA | |||
| BASICS | −0.54 | −1.33 | 0.26 | |||
| CYD | 0.14 | −1.67 | 1.96 | |||
| e-CHUG | −0.30 | −1.30 | 0.71 | |||
| CDCU | 0.27 | −1.02 | 1.57 | |||
| THRIVE | NA | NA | NA | |||
| ACT-CT | 0.24 | −0.92 | 1.41 | |||
Note. NA = not applicable. Alcohol101 = Alcohol 101/Alcohol 101 Plus. AlcEDU = AlcoholEdu. AO-CT = Assessment-only control. ACT-CT = Active control. BASICS = Brief Alcohol Screening Intervention for College Students. CYD = Check Your Drinking. CDCU = College Drinker’s Check-up. ECHUG = Electronic CHECKUP TO GO. THRIVE = Tertiary Health Research Intervention Via Email.
This analysis involved replacing an effect size used in the original network analysis due to dependency between outcomes reported within the same follow-up wave category with the dropped effect size: (1.) One study replaced the 25.8 week follow-up ES with the 12.9 week follow-up. (2.) Three studies replaced the 25.8 week follow-up ES with the 12.9 week follow-up ES.
Table B2.
Treatment rankings
| 3–6 Months | 3–6 Months | |||
| Heavy Frequency |
Peak Quantity |
|||
| SUCRA | PrBest | SUCRA | PrBest | |
| Alc101 | 27.2 | 3.9 | 73.6 | 42.1 |
| AlcEDU | 53.5 | 0.6 | NA | NA |
| BASICS | 77.9 | 31.4 | 77.8 | 26 |
| CYD | 18.6 | 4.1 | 35 | 11.6 |
| e-CHUG | 60.2 | 14.8 | 61.3 | 11.8 |
| CDCU | NA | NA | 33.3 | 7.2 |
| THRIVE | 77 | 39.8 | NA | NA |
| ACT-CT | 14.8 | 0 | 21.8 | 0.4 |
| AO-CT | 70.8 | 5.4 | 47.3 | 0.9 |
| ES removeda1 |
ES removeda2 |
|||
| SUCRA | PrBest | SUCRA | PrBest | |
| Alc101 | 26.2 | 4.9 | 81.2 | 52.4 |
| AlcEDU | 52.2 | 1.9 | NA | NA |
| BASICS | 77.7 | 26.8 | 68.3 | 9.7 |
| CYD | 21.8 | 7.1 | 52.5 | 24.7 |
| e-CHUG | 58.6 | 14.2 | 58.6 | 8.7 |
| CDCU | NA | NA | 15.2 | 1.7 |
| THRIVE | 75.7 | 39.6 | NA | NA |
| ACT-CT | 17.3 | 0 | 39.7 | 2.8 |
| AO-CT | 70.5 | 5.5 | 34.5 | 0 |
| Mandated removed |
||||
| SUCRA | PrBest | |||
| Alc101 | 66.4 | 31.1 | ||
| AlcEDU | NA | NA | ||
| BASICS | 78.5 | 29.6 | ||
| CYD | 40.1 | 15.1 | ||
| e-CHUG | 61.2 | 15.3 | ||
| CDCU | 33.6 | 6.5 | ||
| THRIVE | NA | NA | ||
| ACT-CT | 28.4 | 1.3 | ||
| AO-CT | 42 | 1.1 | ||
Note. SUCRA = Surface under the curve. PrBest = Probability that the treatment will perform the best. Bolded values indicate highest SUCRA value of that intervention in that network. NA = not applicable. Alcohol101 = Alcohol 101/Alcohol 101 Plus. AlcEDU = AlcoholEdu. AO-CT = Assessment-only control. ACT-CT = Active control. BASICS = Brief Alcohol Screening Intervention for College Students. CYD = Check Your Drinking. CDCU = College Drinker’s Check-up. ECHUG = Electronic CHECKUP TO GO. THRIVE = Tertiary Health Research Intervention Via Email.
This analysis involved replacing an effect size used in the original network analysis due to dependency between outcomes reported within the same follow-up wave category with the dropped effect size: (1.) One study replaced the 25.8 week follow-up ES with the 12.9 week follow-up. (2.) Three studies replaced the 25.8 week follow-up ES with the 12.9 week follow-up ES.
Appendix C
Further Reading: References of studies included in the review
- *.Alfonso J, Hall TV, & Dunn ME (2012). Feedback-based alcohol interventions for mandated students: An effectiveness study of three modalities. Clinical Psychology and Psychotherapy, Epub ahead of print. doi: 10.1002/cpp.1786 [DOI] [PubMed] [Google Scholar]
- *.Baer JS, Kivlahan DR, & Marlatt GA (1995). High-risk drinking across the transition from high school to college. Alcoholism: Clinical and Experimental Research, 19(1), 54–61. [DOI] [PubMed] [Google Scholar]
- *.Baer JS, Kivlahan DR, Blume AW, McKnight P, & Marlatt GA (2001). Brief intervention for heavy-drinking college students: 4-year follow-up and natural history. American Journal of Public Health, 91(8), 1310–1316. doi: 10.2105/ajph.91.8.1310 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Borsari B, & Carey KB (2000). Effects of a brief motivational intervention with college student drinkers. Journal of Consulting and Clinical Psychology, 68(4), 728–733. doi: 10.1037/0022-006x.68.4.728 [DOI] [PubMed] [Google Scholar]
- *.Borsari B, Murphy JG, & Carey KB (2009). Readiness to change in brief motivational interventions: A requisite condition for drinking reductions? Addictive Behaviors, 34(2), 232–235. doi: 10.1016/j.addbeh.2008.10.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Bowley C, Faricy C, Hegarty B, Johnstone SJ, Smith JL, Kelly PJ, & Rushby JA (2013). The effects of inhibitory control training on alcohol consumption, implicit-alcohol related cognitions and brain electrical activity. International Journal of Psychophysiology, 89, 342–348. doi: 10.1016/j.ijpsycho.2013.04.011 [DOI] [PubMed] [Google Scholar]
- *.Braitman AL (2012). The effects of personalized boosters for a computerized intervention targeting college student drinking. (Doctoral dissertation, Old Dominion University). [Google Scholar]
- *.Bryant Z (2009). Testing the effectiveness of e-mailed BASICS feedback with college students (Doctoral dissertation, Auburn University). Dissertation Abstracts International, Ph.D., 198. (University Microfilms No. 3386183) [Google Scholar]
- *.Bryant ZE, Henslee AM. & Correia CJ (2013). Testing the effects of e-mailed personalized feedback on risky alcohol use among college students. Addictive Behaviors, 38(10), 2563–7. doi: 10.1016/j.addbeh.2013.06.007 [DOI] [PubMed] [Google Scholar]
- *.Butler LH (2007). Brief alcohol intervention with college students using BASICS: Face-to-face versus computerized feedback (Doctoral dissertation, Auburn University). Dissertation Abstracts International, M.S., 83. [DOI] [PubMed] [Google Scholar]
- *.Butler LH, & Correia CJ (2009). Brief alcohol intervention with college student drinkers: Face-to-face versus computerized feedback. Psychology of Addictive Behaviors, 23(1), 163–167. doi: 10.1037/a0014892 [DOI] [PubMed] [Google Scholar]
- *.Carey KB, & DeMartini KS (2010). The motivational context for mandated alcohol interventions for college students by gender and family history. Addictive Behaviors, 35(3), 218–229. doi: 10.1016/j.addbeh.2009.10.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Carey KB, Carey MP, Henson JM, Maisto SA, & DeMartini KS (2011). Brief alcohol interventions for mandated college students: Comparison of face-to-face counseling and computer-delivered interventions. Addiction, 106(3), 528–537. doi: 10.1111/j.1360-0443.2010.03193.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Croom K, Lewis D, Marchell T, Lesser ML, Reyna VF, Kubicki-Bedford L, Feffer M, & Staiano-Coico L (2009). Impact of an online alcohol education course on behavior and harm for incoming first-year college students: Short-term evaluation of a randomized trial. Journal of American College Health, 57(4), 445–454. doi: 10.3200/jach.57.4.445-454 [DOI] [PubMed] [Google Scholar]
- *.Dimeff LA (1997). Brief intervention for heavy and hazardous college drinkers in a student primary health care setting (Doctoral dissertation, University of Washington). Dissertation Abstracts International, Ph.D.(58, 12-B), 96. (University Microfilms No. 9819231) [Google Scholar]
- *.Dimeff LA, & McNeely M (2000). Computer-enhanced primary care practitioner advice for high-risk college drinkers in a student primary health-care setting. Cognitive and Behavioral Practice, 7(1), 82–100. doi: 10.1016/s1077-7229(00)80010-3 [DOI] [Google Scholar]
- *.Doumas DM, & Andersen LL (2009). Reducing alcohol use in first-year university students: Evaluation of a Web-based personalized feedback program. Journal of College Counseling, 12(1), 18–32. doi: 10.1002/j.2161-1882.2009.tb00037.x [DOI] [Google Scholar]
- *.Doumas DM, & Haustveit T (2008). Reducing heavy drinking in intercollegiate athletes: Evaluation of a web-based personalized feedback program. The Sport Psychologist, 22(2), 212–228. [Google Scholar]
- *.Doumas DM, Haustveit T, & Coll KM (2010). Reducing heavy drinking among first year intercollegiate athletes: A randomized controlled trial of web-based normative feedback. Journal of Applied Sport Psychology, 22(3), 247–261. doi: 10.1080/10413201003666454 [DOI] [Google Scholar]
- *.Doumas DM, Kane CM, Navarro B, & Roman J (2011). Decreasing heavy drinking in first-year students: Evaluation of a web-based personalized feedback program administered during orientation. Journal of College Counseling, 14(1), 5–20. doi: 10.1002/j.2161-1882.2011.tb00060.x [DOI] [Google Scholar]
- *.Doumas DM, McKinley LL, & Book P (2009). Evaluation of two Web-based alcohol interventions for mandated college students. Journal of Substance Abuse Treatment, 36(1), 65–74. doi: 10.1016/j.jsat.2008.05.009 [DOI] [PubMed] [Google Scholar]
- *.Doumas DM, Nelson K, DeYoung A, & Renteria CC (2014). Alcohol-related consequences among first-year university students: Effectiveness of a web-based personalized feedback program. Journal of College Counseling, 17, 150–162. doi: 10.1002/j.2161-1882.2014.00054.x [DOI] [Google Scholar]
- *.Eggleston AM (2007). Components analysis of a brief intervention for college drinkers (Doctoral dissertation, The Ohio State University). Dissertation Abstracts International, Ph.D.(68, 08), 133. (University Microfilms No. 3276684) [Google Scholar]
- *.Fernandez AC, Wood MD, Laforge R, & Black JT (2011). Randomized trials of alcohol-use interventions with college students and their parents: Lessons from the transitions project. Clinical Trials, 8(2), 205–213. doi: 10.1177/1740774510396387 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Geisner I (2008). A randomized clinical trial of a brief, mailed intervention for depressed mood in a college student sample (Doctoral dissertation, University of Washington). Dissertation Abstracts International, Ph.D., 139. (University Microfilms No. 3328400) [Google Scholar]
- *.Geisner IM, Neighbors C, Lee CM, & Larimer ME (2007). Evaluating personal alcohol feedback as a selective prevention for college students with depressed mood. Addictive Behaviors, 32(12), 2776–2787. doi: 10.1016/j.addbeh.2007.04.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Grossbard JR, Mastroleo NR, Kilmer JR, Lee CM, Turrisi R, Larimer ME, & Ray A (2010). Substance use patterns among first-year college students: Secondary effects of a combined alcohol intervention. Journal of Substance Abuse Treatment, 39(4), 384–390. doi: 10.1016/j.jsat.2010.07.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Hallett J, Maycock B, Kypri K, Howat P, & McManus A (2009). Development of a web-based alcohol intervention for university students: Processes and challenges. Drug and Alcohol Review, 28(1), 31–39. doi: 10.1111/j.1465-3362.2008.00008.x [DOI] [PubMed] [Google Scholar]
- *.Henslee A (2008). Providing personalized feedback regarding alcohol use in a group format to college freshmen (Doctoral dissertation, Auburn University). Dissertation Abstracts International, Ph.D.(69, 10), 97. (University Microfilms No. 3333129) [Google Scholar]
- *.Henslee AM, & Correia CJ (2009). The use of freshmen seminar programs to deliver personalized feedback. Journal of Alcohol and Drug Education, 53(3), 39–52. [Google Scholar]
- *.Henslee AM, Irons JG, Day JM, Butler L, Benson TA, & Correia CJ (2006). Using national alcohol screening day to deliver personalized feedback: A pilot study. Journal of Drug Education, 36(4), 271–278. doi: 10.2190/1u8h-41u2-5k03-0j24 [DOI] [PubMed] [Google Scholar]
- *.Hester RK, Delaney HD, & Campbell W (2012). The college drinker’s check-up: Outcomes of two randomized clinical trials of a computer-delivered intervention (STUDY ID 3099 IS FOR EXPERIMENT 2). Psychology of Addictive Behaviors, 26(1), 1–12. doi: 10.1037/a0024753 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Horner K (2010). Brief motivational interviewing: An intervention for alcohol abusing college students (Doctoral dissertation, State University of New York at Albany). Dissertation Abstracts International, Ph.D.(71, 05), 146. (University Microfilms No. 3402364) [Google Scholar]
- *.Hustad JTP, & Borsari B (2010). Web-based screening and brief motivational intervention reduces alcohol use in heavy-drinking undergraduates at up to 6 months. Evidence Based Medicine, 15(1), 17–18. doi: 10.1136/ebm1015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Hustad JTP, Barnett NP, Borsari B, & Jackson KM (2010). Web-based alcohol prevention for incoming college students: A randomized controlled trial. Addictive Behaviors, 35(3), 183–189. doi: 10.1016/j.addbeh.2009.10.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Juarez P (2001). A randomized trial of motivational interviewing and feedback on heavy drinking college students (Doctoral dissertation, University of New Mexico, Albuquerque, New Mexico). Dissertation Abstracts International, M.S., 147. [Google Scholar]
- *.Juarez P, Walters ST, Daugherty M, & Radi C (2006). A randomized trial of motivational interviewing and feedback with heavy drinking college students. Journal of Drug Education, 36(3), 233–246. doi: 10.2190/753n-8242-727t-g63l [DOI] [PubMed] [Google Scholar]
- *.Kerr-Corrêa F, Simão MO, Sumaia SI, Trinca LA, Floripes TMF, Dalben I, Martins RA, Oliveira JB, Cavariani MB, & Tucchi AM (2008). Prevention of risk drinking among university students in a Brazilian university: a clinical trial with a two year follow-up. Paper presented at the meeting of the 5th International Conference of Inebria Alcohol & Drug Problems in Developing Countries, Ribeirão Preto, Brazil. [Google Scholar]
- *.Kulesza M, Apperson M, Larimer ME, & Copeland AL (2010). Brief alcohol intervention for college drinkers: How brief is? Addictive Behaviors, 35(7), 730–733. doi: 10.1016/j.addbeh.2010.03.011 [DOI] [PubMed] [Google Scholar]
- *.Kulesza M, McVay MA, Larimer ME, & Copeland AL (2013). A randomized clinical trial comparing the efficacy of two active conditions of a brief intervention for heavy college drinkers. Addictive Behaviors, 38(4), 2094–2101. doi: 10.1016/j.addbeh.2013.01.008 [DOI] [PubMed] [Google Scholar]
- *.Kypri K, Hallett J, Howat P, McManus A, Maycock B, Bowe S, & Horton NJ (2009). Randomized controlled trial of proactive web-based alcohol screening and brief intervention for university students. Archives of Internal Medicine, 169(16), 1508–1514. doi: 10.1001/archinternmed.2009.249 [DOI] [PubMed] [Google Scholar]
- *.LaBrie JW, Lewis MA, Atkins DC, Neighbors C, Zheng C, Kenney SR, … Ghaidarov TM (2013). RCT of web-based personalized normative feedback for college drinking prevention: Are typical student norms good enough? Journal of Consulting and Clinical Psychology, 81(6), 1074–1086. doi: 10.1037/a0034087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Larimer ME, Lee CM, Kilmer JR, Fabiano PM, Stark CB, Geisner IM, Mallett KA, Lostutter TW, Cronce JM, Feeney M, & Neighbors C (2007). Personalized mailed feedback for college drinking prevention: A randomized clinical trial. Journal of Consulting and Clinical Psychology, 75(2), 285–293. doi: 10.1037/0022-006x.75.2.285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Larimer ME, Turner AP, Anderson BK, Fader JS, Kilmer JR, Palmer RS, & Cronce JM (2001). Evaluating a brief alcohol intervention with fraternities. Journal of Studies on Alcohol, 62(3), 370–380. [DOI] [PubMed] [Google Scholar]
- *.Lau-Barraco C, & Dunn ME (2008). Evaluation of a single-session expectancy challenge intervention to reduce alcohol use among college students. Psychology of Addictive Behaviors, 22(2), 168–175. doi: 10.1037/0893-164x.22.2.168 [DOI] [PubMed] [Google Scholar]
- *.Lau HC (2006). Development and evaluation of a single-session expectancy challenge intervention to reduce alcohol use among heavy drinking college students (Doctoral dissertation, University of Central Florida). Dissertation Abstracts International, Ph.D.(67, 9-B),. (University Microfilms No. 3233658) [Google Scholar]
- *.Leffingwell TR, Leedy MJ, & Lack CW (2005). A multimedia computer-based intervention for college student drinking: Short-term outcomes of a randomized trial. Paper presented at the meeting of the Association for Behavioral and Cognitive Therapies, Washington, DC. [Google Scholar]
- *.Logan DE (2013). Alcohol Interventions for Mandated Students (Project AIMS)(Doctoral Dissertation, University of Washington). [Google Scholar]
- *.Logan DE, Kilmer JR, King KM, & Larimer ME (2015). Alcohol interventions for mandated students: Behavioral outcomes from a randomized controlled pilot study. Journal of Studies on Alcohol and Drugs, 76(1), 31–37. doi: 10.15288/jsad.76.1.31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Lovecchio CP (2009). On-line alcohol education: Impact on knowledge, attitudes and behaviors of first -year college students (Doctoral Dissertation, Villanova University). [Google Scholar]
- *.Lovecchio CP, Wyatt TM, & DeJong W (2010). Reductions in drinking and alcohol-related harms reported by first-year college students taking an online alcohol education course: A randomized trial. Journal of Health Communication, 15(7), 805–819. doi: 10.1080/10810730.2010.514032 [DOI] [PubMed] [Google Scholar]
- *.Martin JL (2014). Does personalized feedback enhance outcomes for students who drink to cope? A pilot study. Alcoholism: Clinical and Experimental Research, S-195, 64A–64A. [Google Scholar]
- *.Mastroleo N (2008). Comparison of supervision training techniques in a motivational enhancement intervention on college student drinking (Doctoral dissertation, The Pennsylvania State University). Dissertation Abstracts International, Ph.D.(69, 11), 180. (University Microfilms No. 3336087) [Google Scholar]
- *.Matteucci A, Reif S, & Paschall MJ (2016). Detecting variation in college student drinking patterns: An argument for creating alcohol-free environments and implementing campus policies. Alcoholism: Clinical and Experimental Research, S-427, 122A–122A. [Google Scholar]
- *.McNally AM (2003). Motivational interventions for problematic alcohol use: In search of the mechanisms of action (Doctoral dissertation, Boston University). Dissertation Abstracts International, Ph.D.(63, 10-B), 144. (University Microfilms No. 3067197) [Google Scholar]
- *.McNally AM, Palfai TP, & Kahler CW (2005). Motivational interventions for heavy drinking college students: Examining the role of discrepancy-related psychological processes. Psychology of Addictive Behaviors, 19(1), 79–87. doi: 10.1037/0893-164x.19.1.79 [DOI] [PubMed] [Google Scholar]
- *.McPherson P (2012). Efficacy of brief alcohol interventions in an Australian tertiary education setting (Doctoral dissertation, Royal Melbourne Institute of Technology University, Melbourne, Australia). Dissertation Abstracts International, Ph.D., 274. [Google Scholar]
- *.Miller ET (2000). Preventing alcohol abuse and alcohol-related negative consequences among freshmen college students: Using emerging computer technology to deliver and evaluate the effectiveness of brief intervention efforts (Doctoral dissertation, University of Washington). Dissertation Abstracts International, Ph.D.(61, 8-B), 271. (University Microfilms No. 9983525) [Google Scholar]
- *.Monahan CJ, McDevitt-Murphy ME, Dennhardt AA, Skidmore JR, Martens MP, & Murphy JG (2013). The impact of elevated posttraumatic stress on the efficacy of brief alcohol interventions for heavy drinking college students (STUDY 3035 is for BASICS-ECHUG STUDY). Addictive Behaviors, 38(3), 1719–1725. doi: 10.1016/j.addbeh.2012.09.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Murphy JG, Dennhardt AA, Skidmore JR, Martens MP, & McDevitt-Murphy ME (2010). Computerized versus motivational interviewing alcohol interventions: Impact on discrepancy, motivation, and drinking (STUDY 3035 is for BASICS-ECHUG STUDY). Psychology of Addictive Behaviors, 24(4), 628–639. doi: 10.1037/a0021347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Murphy JG, Dennhardt AA, Yurasek AM, Skidmore JR, Martens MP, MacKillop J, & McDevitt-Murphy ME (2015). Behavioral economic predictors of brief alcohol intervention outcomes (STUDY 3035 is for BASICS-ECHUG STUDY). Journal of Consulting and Clinical Psychology, 83(6), 1033–1043. doi: 10.1037/ccp0000032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Murphy JG, Duchnick JJ, Vuchinich RE, Davison JW, Karg RS, Olson AM, … Coffey TT (2001). Relative efficacy of a brief motivational intervention for college student drinkers. Psychology of Addictive Behaviors, 15(4), 373–379. doi: 10.1037/0893-164X.15.4.373 [DOI] [PubMed] [Google Scholar]
- *.O’Leary TA, Brown SA, Colby SM, Cronce JM, D’Amico EJ, Fader JS, … Monti PM (2002). Treating adolescents together or individually? Issues in adolescent substance abuse interventions. Alcoholism: Clinical and Experimental Research, 26(6), 890–899. doi: 10.1111/j.1530-0277.2002.tb02619.x [DOI] [PubMed] [Google Scholar]
- *.Orchowski LM, Mastroleo NR, & Borsari B (2012). Correlates of alcohol-related regretted sex among college students. Psychology of Addictive Behaviors, 26(4), 782–790. doi: 10.1037/a0027840 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Paschall MJ, Antin T, Ringwalt CL, & Saltz RF (2011a). Effects of AlcoholEdu for College on alcohol-related problems among freshmen. A randomized multicampus trial. Journal of Studies on Alcohol and Drugs, 72(4), 642–650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Paschall MJ, Antin T, Ringwalt CL, & Saltz RF (2011b). Evaluation of an internet-based alcohol misuse prevention course for college freshmen: Findings of a randomized multicampus trial. American Journal of Preventive Medicine, 41(3), 300–308. doi: 10.1016/j.amepre.2011.03.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Paschall MJ, Ringwalt C, Wyatt T, & DeJong W (2014). Effects of an online alcohol education course among college freshmen: An investigation of potential mediators. Journal of Health Communication, 19(4), 392–412. doi: 10.1080/10810730.2013.811328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Reid AE, Carey KB, Merrill JE, & Carey MP (2015). Social network influences on initiation and maintenance of reduced drinking among college students. Journal of Consulting and Clinical Psychology, 83(1), 36–44. doi: 10.1037/a0037634 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Roberts LJ, Neal DJ, Kivlahan DR, Baer JS, & Marlatt GA (2000). Individual drinking changes following a brief intervention among college students: Clinical significance in an indicated preventive context. Journal of Consulting and Clinical Psychology, 68(3), 500–505. doi: 10.1037/0022-006x.68.3.500 [DOI] [PubMed] [Google Scholar]
- *.Schaus JF, Sole ML, McCoy TP, Mullett N, & O’Brien MC (2009). Alcohol screening and brief intervention in a college student health center: A randomized controlled trial. Journal of Studies on Alcohol and Drugs, (Suppl. 16), 131–141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Simão MO, Kerr-Corrêa F, Smaira SI, Trinca LA, Floripes TMF, Dalben I, … Tucci AM (2008). Prevention of “risky” drinking among students at a Brazilian university. Alcohol and Alcoholism, 43(4), 470–476. doi: 10.1093/alcalc/agn019 [DOI] [PubMed] [Google Scholar]
- *.Teeters JB, Borsari B, Martens MP, & Murphy JG (2015). Brief motivational interventions are associated with reductions in alcohol-impaired driving among college drinkers (STUDY 3090 is for BASICS-ALC101 STUDY). Journal of Studies on Alcohol and Drugs, 76(5), 700–709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Terlecki M (2011). The long-term effect of a brief motivational alcohol intervention for heavy drinking mandated college students (Doctoral dissertation, Louisiana State University, Baton Rouge, Louisiana). Dissertation Abstracts International, 73. [Google Scholar]
- *.Terlecki MA (2008). Alcohol use, negative consequences, and readiness to change in mandated and volunteer college student heavy drinkers before and after a brief alcohol intervention (Doctoral dissertation, Louisiana State University). Dissertation Abstracts International, M.A., 79. [Google Scholar]
- *.Terlecki MA, Buckner JD, Larimer ME, & Copeland AL (2011). The role of social anxiety in a brief alcohol intervention for heavy-drinking college students. Journal of Cognitive Psychotherapy, 25(1), 7–21. doi: 10.1891/0889-8391.25.1.7 [DOI] [Google Scholar]
- *.Terlecki MA, Buckner JD, Larimer ME, & Copeland AL (2012). Brief motivational intervention for college drinking: The synergistic impact of social anxiety and perceived drinking norms. Psychology of Addictive Behaviors, 26(4), 917–923. doi: 10.1037/a0027982 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Terlecki MA, Buckner JD, Larimer ME, & Copeland AL (2015). Randomized controlled trial of brief alcohol screening and intervention for college students for heavy-drinking mandated and volunteer undergraduates: 12-month outcomes. Psychology of Addictive Behaviors, 29(1), 2–16. doi: 10.1037/adb0000056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Terlecki MA, Copeland AL, Larimer ME, & Taylor HA (2008). A brief alcohol intervention for heavy drinking mandated and volunteer college students. Alcoholism: Clinical & Experimental Research, 32(Suppl. 1), 242A–242A. [Google Scholar]
- *.Terlecki MA, Larimer ME, & Copeland AL (2010). Clinical outcomes of a brief motivational intervention for heavy drinking mandated college students: A pilot study. Journal of Studies on Alcohol and Drugs, 71(1), 54–60. [DOI] [PubMed] [Google Scholar]
- *.Terry DL (2012). Screening and brief intervention for hazardous alcohol use: A pilot study in a college counseling center (Doctoral dissertation, Syracuse University). Dissertation Abstracts International, Ph.D.(74, 02-E), 137. (University Microfilms No. 3527869) [Google Scholar]
- *.Tollison SJ, Mastroleo NR, Mallett KA, Witkiewitz K, Lee CM, Ray AE, & Larimer ME (2013). The relationship between baseline drinking status, peer motivational interviewing microskills, and drinking outcomes in a brief alcohol intervention for matriculating college students: a replication. Behavior Therapy, 44(1), 137–151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Walters ST, Vader AM, & Harris TR (2007). A controlled trial of Web-based feedback for heavy drinking college students. Prevention Science, 8(1), 83–88. doi: 10.1007/s11121-006-0059-9 [DOI] [PubMed] [Google Scholar]
- *.Whiteside U (2010). A Brief Personalized Feedback Intervention Integrating a Motivational Interviewing Therapeutic Style and Dialectical Behavioral Therapy Skills for Depressed or Anxious Heavy Drinking Young Adults(Zotero’s generic thesis/dissertation reference - override with correct option) University of Washington, Ann Arbor. [Google Scholar]
- *.Wood MD, Fairlie AM, Fernandez AC, Borsari B, Capone C, Laforge R, & Carmona-Barros R (2010). Brief motivational and parent interventions for college students: A randomized factorial study. Journal of Consulting and Clinical Psychology, 78(3), 349–361. doi: 10.1037/a0019166 [DOI] [PMC free article] [PubMed] [Google Scholar]
Appendix D
Effect sizes for all included studies for all eligible outcomes
Appendix. Table 3 –
Effect Sizes for Networks
|
Frequency of Heavy Use, 0–3 months | ||||
| Study | Group 1 | Group 2 | SMD | SE |
| Hustad et al., 2010 | e-CHUG | AlcoholEdu | −0.0131397 | 0.2679485 |
| Hustad et al., 2010 | AlcoholEdu | AO-CT | 0.4604313 | 0.2867894 |
| Hustad et al., 2010 | e-CHUG | AO-CT | 0.482922 | 0.2777758 |
| Monahan et al., 2013; Murphy et al., 2010; 2015 | e-CHUG | AO-CT | 0.5586971 | 0.232344 |
| Monahan et al., 2013; Murphy et al., 2010; 2015 | BASICS | AO-CT | 0.1067247 | 0.2238358 |
| Monahan et al., 2013; Murphy et al., 2010; 2015 | BASICS | e-CHUG | 0.0696443 | 0.2252482 |
| Matteucci et al., 2016; Paschall et al., 2011a; 2011b; 2014 | AlcoholEdu | AO-CT | 0.0883723 | 0.0409815 |
| Lovecchio, 2009; Lovecchio et al., 2010 | AlcoholEdu | AO-CT | 0.1209321 | 0.0921529 |
| Braitman, 2012 | Alcohol 101 | ACT-CT | −0.5947977 | 0.3757533 |
| Whiteside, 2010 | BASICS | AO-CT | −0.1468197 | 0.2337724 |
| Hallett et al., 2009; Hustad & Borsari, 2010; Kypri et al., 2009 | THRIVE | AO-CT | 0.1505234 | 0.132653 |
| Juarez, 2001; Juarez et al., 2006 | e-CHUG | AO-CT | 0.3317972 | 0.3145816 |
| McNally, 2003; Mcnally et al., 2005 | BASICS | AO-CT | 0.3032855 | 0.235446 |
| Dimeff, 1997; Dimeff & McNeely, 2000 | BASICS | AO-CT | 0.7729614 | 0.3687488 |
| Butler, 2007; Butler & Correia, 2009 | BASICS | AO-CT | 0.5056834 | 0.2766651 |
| Croom et al., 2009 | AlcoholEdu | AO-CT | 0 | 0.0791437 |
| Teeters et al., 2015 | BASICS | Alcohol 101 | 0.2975212 | 0.2427313 |
| Doumas et al., 2009 | CYD | ACT-CT | 0.0635385 | 0.2621579 |
| Lau, 2006; Lau-Barraco & Dunn, 2008 | Alcohol 101 | AO-CT | 0.2423321 | 0.2038409 |
| Henslee et al., 2006 | BASICS | ACT-CT | 0.559514 | 0.4493308 |
| Henslee, 2008; Henslee & Correia, 2009 | BASICS | ACT-CT | 0.0442421 | 0.1553506 |
| Bryant, 2009; Bryant et al., 2013 | BASICS | ACT-CT | 0.0229264 | 0.1449603 |
| Borsari & Carey, 2000; Borsari et al., 2009 | BASICS | AO-CT | 0.6103175 | 0.2664071 |
| Terry, 2012 | BASICS | ACT-CT | 0.659876 | 0.4039006 |
| Martin, 2014 | BASICS | AO-CT | 0.6151792 | 0.3161643 |
|
Frequency of Heavy Use, 3–6 months | ||||
| Study | Group 1 | Group 2 | SMD | SE |
| Mastroleo, 2008; Orchowski et al., 2012 | BASICS | AO-CT | 0.0255337 | 0.169055 |
| Murphy et al., 2001 | BASICS | ACT-CT | 0.4102412 | 0.2766917 |
| Doumas & Andersen, 2009 | e-CHUG | AO-CT | −0.065668 | 0.2915626 |
| Matteucci et al., 2016; Paschall et al., 2011a; 2011b; 2014 | AlcoholEdu | AO-CT | 0.051184 | 0.0409683 |
| Doumas et al., 2011; 2014 | e-CHUG | AO-CT | 0 | 0.222524 |
| Whiteside, 2010 | BASICS | AO-CT | −0.0707541 | 0.2392181 |
| Hallett et al., 2009; Hustad & Borsari, 2010; Kypri et al., 2009 | THRIVE | AO-CT | 0.070593 | 0.168367 |
| Schaus et al., 2009 | BASICS | ACT-CT | 0.492206 | 0.1409888 |
| Monahan et al., 2013; Murphy et al., 2010; 2015 | BASICS | Alcohol 101 | 0.3771957 | 0.2509964 |
| Doumas & Haustveit, 2008 | CYD | ACT-CT | −0.065289 | 0.3496953 |
| Eggleston, 2007 | BASICS | AO-CT | 0.2106767 | 0.2301305 |
| Doumas et al., 2010 | e-CHUG | ACT-CT | −0.0831586 | 0.261467 |
|
Quantity of Alcohol Use, 0–3 Months | ||||
| Study | Group 1 | Group 2 | SMD | SE |
| Hustad et al., 2010 | e-CHUG | AlcoholEdu | 0.0465842 | 0.2679818 |
| Hustad et al., 2010 | e-CHUG | AO-CT | 0.539308 | 0.2787348 |
| Hustad et al., 2010 | AlcoholEdu | AO-CT | 0.4273512 | 0.286277 |
| Terlecki et al., 2008; Terlecki et al., 2011 | BASICS | AO-CT | 0.6233613 | 0.3143511 |
| Hester et al., 2012 | CDCU | AO-CT | 0.2004084 | 0.1766016 |
| LaBrie et al., 2013 | BASICS | AO-CT | 0.0884182 | 0.1151534 |
| Kulesza et al., 2013 | BASICS | AO-CT | 0.309803 | 0.1514086 |
| Monahan et al., 2013; Murphy et al., 2010; 2015 | e-CHUG | AO-CT | 0.2672501 | 0.2289554 |
| Monahan et al., 2013; Murphy et al., 2010; 2015 | BASICS | AO-CT | 0.4747235 | 0.2268034 |
| Monahan et al., 2013; Murphy et al., 2010; 2015 | BASICS | e-CHUG | 0.2134529 | 0.2258194 |
| Matteucci et al., 2016; Paschall et al., 2011a; 2011b; 2014 | AlcoholEdu | AO-CT | 0.09587 | 0.040985 |
| Carey et al., 2011; Carey & DeMartini, 2010; Reid et al., 2015 | AlcoholEdu | AO-CT | 0.0368372 | 0.1099799 |
| Carey et al., 2011; Carey & DeMartini, 2010; Reid et al., 2015 | Alcohol 101 | AO-CT | 0.0840969 | 0.1095011 |
| Carey et al., 2011; Carey & DeMartini, 2010; Reid et al., 2015 | Alcohol 101 | AlcoholEdu | −0.0471421 | 0.1109602 |
| Walters et al., 2007 | e-CHUG | AO-CT | 0.3092513 | 0.1954149 |
| Lovecchio, 2009; Lovecchio et al., 2010 | AlcoholEdu | AO-CT | 0.2116329 | 0.0565116 |
| Logan, 2013; Logan et al., 2015 | BASICS | ACT-CT | −0.069392 | 0.4097957 |
| Braitman, 2012 | Alcohol 101 | ACT-CT | −0.5063631 | 0.3743723 |
| Whiteside, 2010 | BASICS | AO-CT | −0.3714197 | 0.2354262 |
| Hallett et al., 2009; Hustad & Borsari, 2010; Kypri et al., 2009 | THRIVE | AO-CT | 0.4788996 | 0.0464172 |
| Juarez, 2001; Juarez et al., 2006 | e-CHUG | AO-CT | 0.1030538 | 0.3126477 |
| McNally, 2003; Mcnally et al., 2005 | BASICS | AO-CT | 0.2713031 | 0.2351786 |
| Dimeff, 1997; Dimeff & McNeely, 2000 | BASICS | AO-CT | 0.2934548 | 0.3580892 |
| Butler, 2007; Butler & Correia, 2009 | BASICS | AO-CT | 0.3756984 | 0.2747413 |
| Geisner, 2008 | BASICS | AO-CT | −0.008391 | 0.1549015 |
| Kulesza et al., 2010 | BASICS | AO-CT | 0.2273163 | 0.232198 |
| Teeters et al., 2015 | BASICS | Alcohol 101 | 0.2123878 | 0.2420824 |
| Doumas et al., 2009 | CYD | ACT-CT | 0.1819359 | 0.2626119 |
| Horner, 2010 | BASICS | AO-CT | −0.2559756 | 0.2685234 |
| Lau, 2006; Lau-Barraco & Dunn, 2008 | Alcohol 101 | AO-CT | 0.1370167 | 0.2033646 |
| Henslee et al., 2006 | BASICS | ACT-CT | 0.5521266 | 0.4491132 |
| Henslee, 2008; Henslee & Correia, 2009 | BASICS | ACT-CT | 0.1443547 | 0.1555335 |
| Hester et al., 2012 | CDCU | AO-CT | 0.3739442 | 0.2243072 |
| Terlecki, 2011 | BASICS | AO-CT | 0.6591333 | 0.1949856 |
| Bryant, 2009; Bryant et al., 2013 | BASICS | ACT-CT | 0.0509202 | 0.1449789 |
| Borsari & Carey, 2000; Borsari et al., 2009 | BASICS | AO-CT | 0.566366 | 0.2655833 |
| Leffingwell et al., 2005 | CDCU | AO-CT | −0.023189 | 0.2358896 |
| McPherson, 2012 | BASICS | e-CHUG | −0.2274426 | 0.57183 |
| Terry, 2012 | BASICS | ACT-CT | 0.5074358 | 0.3996419 |
| Martin, 2014 | BASICS | AO-CT | 0.4491305 | 0.3128194 |
| Bowley et al., 2013 | THRIVE | ACT-CT | 0.0051054 | 0.3203622 |
| Terlecki, 2008; Terlecki et al., 2010; 2012 | BASICS | AO-CT | 0.2340654 | 0.3142519 |
| Terlecki et al., 2015 | BASICS | AO-CT | 0.3364387 | 0.1886663 |
|
Quantity of Alcohol Use, 3–6 Months | ||||
| Study | Group 1 | Group 2 | SMD | SE |
| Mastroleo, 2008; Orchowski et al., 2012 | BASICS | AO-CT | 0.1264261 | 0.1692169 |
| Murphy et al., 2001 | BASICS | ACT-CT | 0.2147281 | 0.2746396 |
| Doumas & Andersen, 2009 | e-CHUG | AO-CT | 0.203054 | 0.2921708 |
| LaBrie et al., 2013 | BASICS | AO-CT | 0 | 0.1184705 |
| Monahan et al., 2013; Murphy et al., 2010; 2015 | BASICS | e-CHUG | 0.2705603 | 0.2368688 |
| Monahan et al., 2013; Murphy et al., 2010; 2015 | e-CHUG | AO-CT | −0.0735571 | 0.2329142 |
| Monahan et al., 2013; Murphy et al., 2010; 2015 | BASICS | AO-CT | 0.1873487 | 0.2299978 |
| Matteucci, 2016; Paschall et al., 2011a; 2011b; 2014 | AlcoholEdu | AO-CT | 0.0668791 | 0.040973 |
| Walters et al., 2007 | e-CHUG | AO-CT | −0.027574 | 0.1942664 |
| Doumas et al., 2011; 2014 | e-CHUG | AO-CT | 0.3220704 | 0.2239406 |
| Logan, 2013; Logan et al., 2015 | BASICS | ACT-CT | −0.3980921 | 0.42153 |
| Whiteside, 2010 | BASICS | AO-CT | −0.1710859 | 0.2395801 |
| Hallett et al., 2009; Hustad & Borsari, 2010; Kypri et al., 2009 | THRIVE | AO-CT | 0.4668047 | 0.0463849 |
| Schaus et al., 2009 | BASICS | ACT-CT | 0.4007094 | 0.1402939 |
| Teeters et al., 2015 | BASICS | Alcohol 101 | 0.2978334 | 0.2501741 |
| Doumas & Haustveit, 2008 | CYD | ACT-CT | 0.1306662 | 0.3499727 |
| Horner, 2010 | BASICS | AO-CT | −0.137309 | 0.2677464 |
| Eggleston, 2007 | BASICS | AO-CT | 0.3614697 | 0.2313605 |
| Terlecki, 2011 | BASICS | AO-CT | 1.01573 | 0.2017665 |
| Miller, 2000 | Alcohol 101 | AO-CT | 0.4582334 | 0.1331391 |
| Doumas et al., 2010 | e-CHUG | ACT-CT | 0.2787872 | 0.1964494 |
| Leffingwell et al., 2005 | CDCU | AO-CT | 0.0772968 | 0.2359686 |
| McPherson, 2012 | BASICS | e-CHUG | −0.152507 | 0.586367 |
|
Peak Quantity of Alcohol Use, 0–3 Months | ||||
| Study | Group 1 | Group 2 | SMD | SE |
| Hustad et al., 2010 | e-CHUG | AlcoholEdu | −0.2078722 | 0.2686646 |
| Hustad et al., 2010 | e-CHUG | AO-CT | 0.4893903 | 0.2778806 |
| Hustad et al., 2010 | AlcoholEdu | AO-CT | 0.689066 | 0.2913354 |
| Terlecki et al., 2008; Terlecki et al., 2011 | BASICS | AO-CT | 0.6434117 | 0.3148205 |
| Hester et al., 2012 | CDCU | AO-CT | 0.3578802 | 0.1775564 |
| LaBrie et al., 2013 | BASICS | AO-CT | 0.0447274 | 0.1151116 |
| Lovecchio, 2009; Lovecchio et al., 2010 | AlcoholEdu | AO-CT | 0.1971226 | 0.0618565 |
| Braitman, 2012 | Alcohol 101 | ACT-CT | −0.5507706 | 0.3750387 |
| Geisner, 2008 | BASICS | AO-CT | −0.1464643 | 0.155108 |
| Doumas et al., 2009 | CYD | ACT-CT | −0.2924118 | 0.2634284 |
| Horner, 2010 | BASICS | AO-CT | −0.1405973 | 0.2677616 |
| Henslee et al., 2006 | BASICS | ACT-CT | 0.3142058 | 0.4436159 |
| Henslee, 2008; Henslee & Correia, 2009 | BASICS | ACT-CT | 0.1097072 | 0.1554483 |
| Hester et al., 2012 | CDCU | AO-CT | 0.5151408 | 0.226028 |
| Terlecki, 2011 | BASICS | AO-CT | 0.9787726 | 0.200942 |
| Leffingwell et al., 2005 | CDCU | AO-CT | 0.1923832 | 0.2364186 |
| McPherson, 2012 | BASICS | e-CHUG | 0.1058105 | 0.5704653 |
| Martin, 2014 | BASICS | AO-CT | 0.6454946 | 0.316883 |
| Terlecki, 2008; Terlecki et al., 2010; 2012 | BASICS | AO-CT | 0.2546021 | 0.3144466 |
| Terlecki et al., 2015 | BASICS | AO-CT | 0.6002765 | 0.1915174 |
|
Peak Quantity of Alcohol Use, 3–6 Months | ||||
| Study | Group 1 | Group 2 | SMD | SE |
| LaBrie et al., 2013 | BASICS | AO-CT | 0.1391386 | 0.1186138 |
| Doumas et al., 2011; 2014 | e-CHUG | AO-CT | 0.228673 | 0.2232392 |
| Schaus et al., 2009 | BASICS | ACT-CT | 1.235356 | 0.15149 |
| Doumas & Haustveit, 2008 | CYD | ACT-CT | 0.100941 | 0.3498237 |
| Horner, 2010 | BASICS | AO-CT | −0.1820898 | 0.2679848 |
| Terlecki, 2011 | BASICS | AO-CT | 1.028616 | 0.2020603 |
| Miller, 2000 | Alcohol 101 | AO-CT | 0.422202 | 0.1328821 |
| Doumas et al., 2010 | e-CHUG | ACT-CT | 0.071086 | 0.195575 |
| Alfonso et al., 2012; 2013 | BASICS | e-CHUG | 0.2179615 | 0.199841 |
| Leffingwell et al., 2005 | CDCU | AO-CT | −0.2748331 | 0.2369759 |
| McPherson, 2012 | BASICS | e-CHUG | −0.7404641 | 0.6047333 |
Footnotes
SUCRA values include the uncertainty of the different effect estimates and probabilities of assuming another possible treatment ranking so are more stable than the probability of being the best treatment: SUCRA values are thus focused on in the text, however, both values are presented in Table 3.
(Alfonso et al., 2012; Carey et al., 2011; Doumas et al., 2009; Horner, 2010; Logan, 2013; Terlecki, 2011; Terlecki et al., 2011)
Carey et al., 2011; Doumas et al., 2009; Horner, 2010; Logan et al., 2015; Terlecki et al., 2011; Terlecki et al., 2015
Compliance with Ethical Standards
b. Disclosure of potential conflicts of interest - S.G.’s spouse is a salaried-employee of Eli Lilly and Company, and owns stock. S.G. has accompanied his spouse on company-sponsored travel. All other authors declare no known conflicts of interest.
c.-d. Ethical approval/ Informed consent - not applicable as this is a systematic review
References
*References of studies included in the review are located in Appendix C, Further Reading.
- Abbey A, Wegner R, Woerner J, Pegram SE, & Pierce J (2014). Review of survey and experimental research that examines the relationship between alcohol consumption and men’s sexual aggression perpetration. Trauma, Violence, & Abuse, 15(4), 265–282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alfonso J. & Deschenes SD (2013). Do drinking games matter? An examination by game type and gender in a mandated student sample. The American Journal of Drug and Alcohol Abuse, 39(5), 312–319. doi: 10.3109/00952990.2013.770519 [DOI] [PubMed] [Google Scholar]
- Barry AE (2007). Using theory-based constructs to explore the impact of Greek membership on alcohol-related beliefs and behaviors: A systematic literature review. Journal of American College Health, 56(3), 307–315. [DOI] [PubMed] [Google Scholar]
- Buscemi J, Murphy JG, Martens MP, McDevitt-Murphy ME, Dennhardt AA, & Skidmore JR (2010). Help-seeking for alcohol-related problems in college students: correlates and preferred resources. Psychology of Addictive Behaviors, 24(4), 571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carey KB, Scott-Sheldon LA, Garey L, Elliott JC, & Carey MP (2016). Alcohol interventions for mandated college students: A meta-analytic review. Journal of Consulting and Clinical Psychology, 84, 619–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Century Council. (1997). Alcohol 101 Los Angeles. [Google Scholar]
- The Century Council. Alcohol 101 Plus [Computer software] 2003. Retrieved from http://www.alcohol101plus.org/home.html
- Chaimani A, Caldwell DM, Li T, Higgins JP, & Salanti G (2017). Additional considerations are required when preparing a protocol for a systematic review with multiple interventions. Journal of Clinical Epidemiology, 83, 65–74. [DOI] [PubMed] [Google Scholar]
- Chaimani A, Higgins JP, Mavridis D, Spyridonous P, & Salanti G (2013). Graphical tools for network meta-analysis in Stata. PLoS One, 8(10), e76654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cipriani A, Higgins JP, Geddes JR, & Salanti G (2013). Conceptual and technical challenges in network meta-analysis. Annals of internal medicine, 159(2), 130–137. [DOI] [PubMed] [Google Scholar]
- Dias S, Welton NJ, Caldwell DM, Ades AE (2010). Checking consistency in mixed treatment comparison meta-analysis. Statistics in Medicine, 29, 932–944. [DOI] [PubMed] [Google Scholar]
- Dimeff LA, Baer JS, Kivlahan DR, & Marlatt GA (Ed.).(1999). Brief alcohol screening and intervention for college students (BASICS): A harm reduction approach Guilford Press. [Google Scholar]
- Fachini A, Aliane PP, Martinez EZ, & Furtado EF (2012). Efficacy of brief alcohol screening intervention for college students (BASICS): A meta-analysis of randomized controlled trials. Substance abuse treatment, prevention, and policy, 7(1), 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foster C, Caravelis C, & Kopak A (2014). National College Health Assessment Measuring Negative Alcohol-Related Consequences among College Students. American Journal of Public Health Research, 2(1), 1–5. [Google Scholar]
- Grant S, Pedersen ER, Osilla KC, Kulesza M, & D’amico EJ (2016). Reviewing and interpreting the effects of brief alcohol interventions: comment on a Cochrane review about motivational interviewing for young adults. Addiction, 111(9), 1521–1527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ham LS, & Hope DA (2003). College students and problematic drinking: A review of the literature. Clinical Psychology Review, 23(5), 719–759. [DOI] [PubMed] [Google Scholar]
- Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, … & Sterne JA (2011). The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ, 343, d5928. doi: 10.1136/bmj.d5928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hingson R, & White A (2014). New research findings since the 2007 Surgeon General’s Call to Action to Prevent and Reduce Underage Drinking: A review. Journal of studies on alcohol and drugs, 75(1), 158–169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huh D, Mun EY, Larimer ME, White HR, Ray AE, Rhew IC, … & Atkins DC (2015). Brief motivational interventions for college student drinking may not be as powerful as we think: An individual participant-level data meta-analysis. Alcoholism: Clinical and Experimental Research, 39(5), 919–931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hutton B, Salanti G, Caldwell DM, Chaimani A, Schmid CH, Cameron C, … & Mulrow C (2015). The PRISMA Extension Statement for Reporting of Systematic Reviews Incorporating Network Meta-analyses of Health Care Interventions: Checklist and Explanations. Annals of Internal Medicine, 162(11), 777–784. [DOI] [PubMed] [Google Scholar]
- Jennison KM (2004). The Short-term effects and unintended long-term consequences of binge drinking in college: A 10-year follow-up study. The American Journal of Drug and Alcohol Abuse, 30(3), 659–684. [DOI] [PubMed] [Google Scholar]
- Kingree JB, & Thompson M (2015). A comparison of risk factors for alcohol-involved and alcohol-uninvolved sexual aggression perpetration. Journal of Interpersonal Violence, 30(9), 1478–1492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lipsey MW and Wilson DB, 2001. Practical meta-analysis Sage Publications, Inc. [Google Scholar]
- Mavridis D, Giannatsi M, Cipriani A, & Salanti G (2015). A primer on network meta-analysis with emphasis on mental health. Evidence Based Mental Health, 18(2), 40–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mavridis D, & Salanti G (2014). Exploring and accounting for publication bias in mental health: a brief overview of methods. Evidence Based Mental Health, 17, 11–5. doi: 10.1136/eb-2013-101700 [DOI] [PubMed] [Google Scholar]
- Meisel MK, & Barnett NP (2017). Protective and risky social network factors for drinking during the transition from high school to college. Journal of Studies on Alcohol and Drugs, 78(6), 922–929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pedersen DE (2013). Gender differences in college binge drinking: Examining the role of depression and school stress. The Social Science Journal, 50(4), 521–529. [Google Scholar]
- Peters JL, Sutton AJ, Jones DR, Abrams KR, & Rushton L (2008). Contour-enhanced meta-analysis funnel plots help distinguish publication bias from other causes of asymmetry. Journal of Clinical Epidemiology, 61(10), 991–996. [DOI] [PubMed] [Google Scholar]
- Petropoulou M, Nikolakopoulou A, Veroniki AA, Rios P, Vafaei A, Zarin W, … & Egger M (2017). Bibliographic study showed improving statistical methodology of network meta-analyses published between 1999 and 2015. Journal of Clinical Epidemiology, 82, 20–28. 10.1016/j.jclinepi.2016.11.002 [DOI] [PubMed] [Google Scholar]
- Pildal J, Hrobjartsson A, Jørgensen KJ, Hilden J, Altman DG, & Gøtzsche PC (2007). Impact of allocation concealment on conclusions drawn from meta-analyses of randomized trials. International Journal of Epidemiology, 36(4), 847–857. [DOI] [PubMed] [Google Scholar]
- Salanti G (2012). Indirect and mixed-treatment comparison, network, or multiple-treatments meta-analysis: Many names, many benefits, many concerns for the next generation evidence synthesis tool. Research Synthesis Methods, 3(2), 80–97. [DOI] [PubMed] [Google Scholar]
- Salanti G, Ades AE, & Ioannidis JP (2011). Graphical methods and numerical summaries for presenting results from multiple-treatment meta-analysis: An overview and tutorial. Journal of Clinical Epidemiology, 64(2), 163–171. [DOI] [PubMed] [Google Scholar]
- Schulenberg JE, Johnston LD, O’Malley PM, Bachman JG, Meich RA, & Patrick ME, (2017). Monitoring the Future national survey results on drug use, 1975–2016: Volume 2, College students and adults ages 19–55 Ann Arbor: Institute for Social Research, The University of Michigan. [Google Scholar]
- StataCorp (2015). Stata Statistical Software: Release 14 College Station, TX: StataCorp LP. [Google Scholar]
- Steinka-Fry KT, Tanner-Smith EE, & Grant S (2015). Effects of 21st birthday brief interventions on college student celebratory drinking: A Systematic review and meta-analysis. Addictive Behaviors, 50, 13–21. doi: 10.1016/j.addbeh.2015.06.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- SAMHSA (2016a). 2016 National Survey on Drug Use and Health (NSDUH). Table 6.80B—Heavy Alcohol Use in the Past Month among Persons Aged 18 to 22, by College Enrollment Status and Demographic Characteristics: Percentages, 2015 and 2016. Available at: https://www.samhsa.gov/data/sites/default/files/NSDUH-DetTabs-2016/NSDUH-DetTabs-2016.htm#tab6-80B
- SAMHSA (2016b). 2016 National Survey on Drug Use and Health (NSDUH). Table 6.79B. Available at: https://www.samhsa.gov/data/sites/default/files/NSDUH-DetTabs-2016/NSDUH-DetTabs-2016.htm#tab6-79B
- Substance Abuse and Mental Health Services Administration. (2018). Key substance use and mental health indicators in the United States: Results from the 2017 National Survey on Drug Use and Health (HHS Publication No. SMA 18–5068, NSDUH Series H53) Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration; Retrieved from https://www.samhsa.gov/data/ [Google Scholar]
- Tanner-Smith EE, & Lipsey MW (2015). Brief alcohol interventions for adolescents and young adults: A systematic review and meta-analysis. Journal of Substance Abuse Treatment, 51, 1–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanner-Smith EE and Risser MD, 2016. A meta-analysis of brief alcohol interventions for adolescents and young adults: variability in effects across alcohol measures. The American journal of drug and alcohol abuse, 42(2), 140–151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valenstein-Mah H, Larimer M, Zoellner L, & Kaysen D (2015). Blackout drinking predicts sexual revictimization in a college sample of binge-drinking women. Journal of Traumatic Stress, 28(5), 484–488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Voloshyna DM, Bonar EE, Cunningham RM, Ilgen MA, Blow FC, & Walton MA (2016). Blackouts among male and female youth seeking emergency department care. American Journal of Drug and Alcohol Abuse, 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wechsler H, Davenport A, Dowdall G, Moeykens B, & Castillo S (1994). Health and Behavioral Consequences of Binge Drinking in College: A National Survey of Students at 140 Campuses. Journal of the American Medical Association, 272(21), 1672–1677. doi: 10.1001/jama.1994.03520210056032 [DOI] [PubMed] [Google Scholar]
- White IR (2015). Network meta-analysis. Stata Journal, 15(4), 951–85. [Google Scholar]
- White IR, Barrett JK, Jackson D, & Higgins JP (2012). Consistency and inconsistency in network meta-analysis: model estimation using multivariate meta-regression. Research synthesis methods, 3(2), 111–125. [DOI] [PMC free article] [PubMed] [Google Scholar]