Abstract
Objective:
Parent knowledge about developmental disabilities (DDs) may facilitate access to DD care; however, parents may vary in their knowledge and familiarity with common DDs. This study aimed to assess racial/ethnic and language differences in low-income families’ familiarity, knowledge, and personal experience with DDs.
Methods:
We conducted a child development survey among 539 low-income parents of young children attending visits at the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC), in six Oregon counties in 2015. Survey items assessed parent familiarity with early signs of DDs, self-reported knowledge about DDs, and personal experience with a friend or family member with a DD. Bivariable and multivariable analyses assessed differences in outcomes among non-Latino white [white], Latino-English proficient [Latino-EP], Latino-limited English proficient [Latino-LEP], and non-Latino other race English proficient [other race] parents.
Results:
Overall, parent participants correctly identified 64.7% of early signs of DDs. White parents correctly identified the earliest signs, even after adjustment for socio-demographic factors. Latino-LEP, Latino-EP and other race parents were less likely to have heard of prevalent DDs such as ADHD and autism, and were less likely to have a friend or family member with a DD compared to white parents.
Conclusions:
Low-income Latino-LEP and other race parents have less familiarity or personal experience with DDs, and are less aware of DD early signs compared to low-income white parents. Study findings suggest that interventions to reduce disparities in DD diagnosis and treatment should include increasing information transfer to parents in racial/ethnic and language minority communities.
What’s New:
Low-income racial/ethnic minority parents, and particularly Latinos parents with limited English proficiency, have less familiarity or personal experience with DDs, and are less aware of DD early signs compared to low-income white parents.
Keywords: developmental disabilities; healthcare disparities; child development; Women, Infants, and Children Special Supplemental Nutrition Program; health services accessibility
INTRODUCTION
Developmental disabilities (DDs) affect one in six U.S. children,1 and include conditions such as autism spectrum disorder (ASD), attention-deficit/hyperactivity disorder (ADHD), cerebral palsy, and Down syndrome. Early identification and treatment of many DDs improves child functioning, development,2 academic achievement,3 and/or family outcomes.4 However, disparities exist in early identification and treatment of DDs: low-income and racial/ethnic minority children are identified later and with more severe symptoms, and when they do receive a diagnosis, they receive less treatment, and less evidence-based treatment, than more affluent white children.5–8
Though structural aspects of the health and education systems and provider behaviors contribute to racial/ethnic and/or income disparities in DDs,9–12 families’ DD knowledge and familiarity may also contribute by affecting affect how parents seek developmental care for their children.13 However, little is known about low-income and racial/ethnic minority families’ DD knowledge or familiarity.
Parents from disadvantaged backgrounds may differ from other parents in understanding of developmental milestones and parenting,13–15 and parent education correlates with increased parenting knowledge, at least among White mothers.13 Among families of children diagnosed with DDs, research suggests racial/ethnic disparities exist in family knowledge about their child’s condition and in how many people they know with DDs. One study16 found Latina mothers knew less about developmental milestones and aspects of ASD care than white mothers. Another study revealed “lack of knowledge about ASD” was the most common barrier to ASD diagnosis reported by Latino parents.17 Latino and Black/African American caregivers of children with ASD and ADHD have reported not knowing anyone else with the condition.18,19 One recent study showed that a child was more likely to be diagnosed with ASD if he/she lives in proximity to another child with the condition.20 Exposure to community members with DDs may increase early identification by raising awareness of early signs, improving access to condition-specific information, and reducing stigma. Sources of advice-seeking for DDs may also be important in early DD identification and may be another contributor to disparities. For instance, white mothers with less parenting knowledge are more likely to rely on relatives for advice-seeking and support in child rearing as opposed to developmental professionals.13 Similar studies on advice-seeking have not been conducted among families of other races and ethnicities.
This study sought to fill research gaps about racial/ethnic and language differences in parent familiarity with DDs and their early signs. First, little research assesses racial/ethnic differences in familiarity with the early signs of DDs among community samples of parents. Research on early signs in community samples (e.g., lower DD risk, non-research-based samples) is important because many DD symptoms develop over time; as a result, community parents’ views may be a proxy for what parents of children who have DDs understand prior to diagnosis. However, most previous studies have been conducted in high-risk populations,21 have narrowly focused on specific DDs,16,17,22 or have focused on parenting knowledge rather than early signs of DDs.13–15,23 Existing studies have also not assessed how income might mediate cultural differences in familiarity with DDs, even though income plays a mediating role in identification and treatment of common DDs.24,25 Furthermore, little is known about the role of English proficiency in parents’ knowledge about child development or DDs, even though limited English proficiency (LEP) is associated with adverse child outcomes.26 Only one study has assessed the role of LEP in parents’ knowledge of child development generally,15 and no studies have examined the role of LEP in knowing people with DDs, or in knowing early signs of DDs. Finally, no studies have assessed advice-seeking behaviors in racial/ethnic groups beyond white mothers.
In this study, we aimed to determine if family race/ethnicity and English proficiency are associated with familiarity with child development, self-reported DD knowledge, advice-seeking, and personal experience with individuals with DDs among low-income families. This study focused on the U.S. Latino population for several reasons. First, Latino children are the largest U.S. racial/ethnic minority population and are one of the fastest-growing child population groups in the U.S. Second, due to high rates of LEP among Latinos, studying this population provides opportunity to examine the effects of both race/ethnicity and LEP on DD knowledge and familiarity.
We studied families enrolled in Oregon’s Special Supplemental Nutrition Program for Women, Infants, and Children (WIC). WIC is a federal program providing supplemental food, referrals, and nutrition education to low-income families who are pregnant, breastfeeding, or with children under age five. About 9.3 million women and children participate in WIC, and nearly all WIC households earn under 185% of the U.S. Federal Poverty Level. WIC participants are racially/ethnically diverse: about 40% are Latino ethnicity, and about 40% are non-white race.27 As a result, WIC presents an opportunity to assess differences in familiarity with DDs among diverse low-income families, and could also be a promising future setting for interventions.
In the study, we compared familiarity with early signs of DDs, self-reported knowledge of DDs, personal experience with DDs, and advice seeking for DDs among families who were non-Latino white, non-Latino other race, Latino with English proficiency, and Latino with LEP. We hypothesized that Latino families with LEP would have the lowest knowledge and familiarity with DDs, and would differ from other groups in their sources of advice.
METHOD
Study Design and Sample
In 2015, we conducted a cross-sectional survey of families from 10 WIC clinics in six Oregon counties. Clinics were chosen for large Latino populations and varying urbanicity. Eligible parents or guardians (herein, “parents”) had a child age 2–5 years enrolled in WIC, were present at WIC clinics on dates when the survey was administered, and spoke English or Spanish. English-Spanish bilingual/bicultural research assistants offered the survey in written or oral format per parent request. A parent could request oral format for any reason, including literacy reasons or logistical reasons (e.g., she/he was holding a baby). Of 707 of eligible families, 539 participated yielding a response rate of 79%.28 Oregon Health & Science University Institutional Review Board approved the study.
Survey
We identified no measures of development and DDs familiarity that were brief, validated in Spanish, and written at a low reading level. New survey items were therefore developed through an iterative process similar to Townsend and colleagues.29 We first examined existing survey items assessing general familiarity with child development,14,15 DDs,22 and developmental milestones used in validated screeners (Ages and Stages–3,30 Modified Checklist for Autism in Toddlers—R/F31), and parent checklists (Center for Disease Control and Prevention’s [CDC] Learn the Signs Act Early Parent Checklists32) for potential use, and adapted items for inclusion. Items on socio-demographics and access to care were adapted from the 2011 National Survey of Children’s Health and the U.S. Census American Community Survey [ACS]. The survey was written at a sixth-grade reading level, according to the Flesch-Kinkaid Grade Level Test. To facilitate understanding in a population with lower literacy, the survey had large text, color visuals, and clear item sequencing.29 Survey items were translated to Spanish by a bilingual research assistant and reviewed by two Spanish translators of different national origins; existing Spanish translations of measures were used if possible. Cognitive interviews were conducted in English or Spanish with 25 parents participating in WIC to refine item wording, clarify response options, and assess overall survey design.
Measures
Child development familiarity.
To assess participants’ familiarity with early signs of DDs, we posited a scenario in which a friend had a son who “just turned two years old” and had concerns about 11 possible behaviors (Online Appendix). Behaviors ranged from typical for age (“he does not recognize any letters or numbers”) to atypical and potentially a sign of a DD (“he does not respond to his name when his mom calls”). Response options were “no, not very concerned” or “yes, concerned” for each behavior; behaviors included social, cognitive, gross motor, and fine motor tasks. The total number of correct responses were used to measure familiarity with early childhood development.
Knowledge of DDs.
Participants were asked how much they knew about DDs using items similar to Bussing.22 We intentionally selected a variety of prevalent DDs that were either “visible” or “invisible.” These included mental retardation or intellectual disability, autism or ASD, cleft lip or palate, cerebral palsy, and Down syndrome. Rett syndrome was added as a manipulation check because we expected low knowledge in all groups because of low condition prevalence.” Response options included “never heard of it,” “heard of it but don’t know much about it,” “know a little about it,” and “know a lot about it.”
Personal experience with DDs.
To determine if participants knew someone with a DD, they were asked to respond yes or no to the item: “Do you have a friend or family member with any of these conditions?” (also similar to Bussing).22 Conditions asked about were the same as in the DDs knowledge items.
Advice-seeking.
Following the child development scenario, participants were asked: “Who would you advise your friend to talk to about [his/her child development] concerns?” Response options included: doctor, family member, spouse/partner, teacher, WIC staff member, other parents, church, childcare provider, nobody, and other.
Demographics.
Parent socio-demographic characteristics were self-reported and included age, sex, education, and nativity. Race and Latino/Hispanic ethnicity were assessed using U.S. Census ACS items, and participant English proficiency was assessed using the ACS item, “How well do you speak English?” Participants responding “very well” were categorized as English proficient. Participants responding “well,” “not well,” or “not at all,” were categorized as having limited English proficiency. This cutoff point for English proficiency is based on federal guidelines and shows strong concurrent validity with comprehensive measures.33
We created a composite “ethnicity/language” variable with four mutually exclusive categories: non-Latino, white, English proficient (“white”); non-Latino, other race, English proficient (“other race”); Latino, English proficient (“Latino-EP”); and Latino, limited English proficient (“Latino-LEP”). Because the survey was administered in English and Spanish, participants who completed a survey in English but reported limited English proficiency (n=15), or with missing data for race/ethnicity and English proficiency (n=23) were excluded.
Data analysis
We computed descriptive statistics to characterize the sample. Child development familiarity was assessed with mean scores and standard deviations. To determine associations between ethnicity/language and child development familiarity, we fit a multiple linear regression model in which the scale score was the dependent variable and ethnicity/language was the primary independent variable. In these models, the “Constant” represents the score for a subject with referent values for characteristics listed in Table 2. β-coefficients associated with each characteristic indicate the degree to which the score is raised/lowered, adjusting for other factors in the model.
Table 2.
Linear regression model results: Associations of ethnicity/language and other factors with child development familiarity (N=539)
| Adjusted β coefficient (95% CI) | |
|---|---|
| Constant (95% CI) | 8.26 (6.76, 9.75)b |
| Latino ethnicity, race, and English proficiency | |
| Non-Latino, white, English proficient (n = 155) | ref |
| Non-Latino, other race, English proficient (n = 55) | −1.55 (−2.37, −0.73)b |
| Latino, English proficient (n = 100) | −0.72 (−1.39, −0.05) |
| Latino, limited English proficiency (n = 191) | −1.04 (−1.79, −0.30)a |
| Age, years | −0.03 (−0.07, −0.002) |
| Gender | |
| Female (n = 473) | ref |
| Male (n = 49) | −0.76 (−1.50, −0.02) |
| Education | |
| 8th grade or less (n = 82) | ref |
| High school without diploma or current student (n = 89) | 0.10 (−0.72, 0.92) |
| High school graduate or GED completed (n = 145) | 0.92 (0.15, 1.69) |
| Associate degree or some college credit but no degree (n = 175) | 1.31 (0.47, 2.15)a |
| Bachelor’s degree or higher (n = 30) | 2.30 (1.09, 3.50)b |
| Mode of survey administration | |
| Self-administered survey (n = 379) | ref |
| Orally as an interview (n = 160) | 1.92 (1.32, 2.51)b |
“Constant” represents the score for a subject with referent values for all characteristics listed in the table.
β-coefficients associated with each characteristic indicate the degree to which the score is raised lowered for the listed factor, adjusting for all other factors shown in the model.
Abbreviation: CI, confidence interval
Bold values are significant at p<0.05,
p<0.01
p<0.001.
To compare rates of DDs knowledge by ethnicity/language groups, we used descriptive statistics. Bivariate tests were also used to compare rates of personal experiences with DDs by ethnicity/language. Multiple logistic regression was used to determine associations of ethnicity/language with personal experience with DDs, controlling for other socio-demographic factors. Finally, descriptive statistics and chi-square tests were used to assess ethnicity/language group differences in advice-seeking behaviors.
For multivariable models, we used a stepwise backward elimination procedure to select covariates, with an alpha level of 0.15 for elimination and 0.10 for inclusion. Covariates included: parent gender, parent age, parent education, and survey mode (i.e., oral or written self-administered). To account for clustering by location, we controlled for site in all models; urbanicity was not controlled for due to high collinearity with site. All analyses were performed in Stata 13.1 (StataCorp, College Station, Texas).
RESULTS
Sample.
30% of participating parents were white, 37% were Latino-LEP, 19.4% were Latino-EP, and 10.7% were of other races (e.g., Black/African-American, Asian, Pacific Islander). Median participant age was 30 years. Most participants were female (90.6%), self-administered the survey (70.3%), and visited a WIC clinic in or near a metropolitan area (89.4%). Nearly half (45.6%) were U.S. natives; among those who had lived outside the U.S., the average number of years in the U.S. was 13.6 (Table 1).
Table 1.
Study sample characteristics
| Participant Factorsa | Overall % or Mean (N = 539) |
|---|---|
| Age, years | |
| Mean (SD) | 31.1 (6.9) |
| Median | 30.0 |
| Range | 16–70 |
| Gender | |
| Female (n = 473) | 90.6 |
| Male (n = 49) | 9.4 |
| Latino ethnicity, race, and English proficiency | |
| Non-Latino, white, English proficient (n = 155) | 30.0 |
| Non-Latino, other race, English proficient (n = 55) | 10.7 |
| Latino, English proficient (n = 100) | 19.4 |
| Latino, limited English proficiency (n = 191) | 37.0 |
| Parent nativity | |
| Always lived in U.S. (n = 240) | 45.6 |
| Lived outside the U.S. (n = 286) | 54.4 |
| Years lived in U.S. (SD) | 13.6 (6.3) |
| Education | |
| 8th grade or less (n = 82) | 15.7 |
| High school without diploma or current student (n = 89) | 17.1 |
| High school graduate or GED completed (n = 145) | 27.8 |
| Associate degree or some college credit but no degree (n = 175) | 33.6 |
| Bachelor’s degree or higher (n = 30) | 5.8 |
| Mode of survey administration | |
| Self-administered survey (n = 379) | 70.3 |
| Orally as an interview (n = 160) | 29.7 |
| WIC agency location | |
| Metropolitan area (n = 482) | 89.4 |
| Nonmetropolitan, adjacent to a metropolitan area (n = 57) | 10.6 |
Abbreviations: GED, general education development; SD, standard deviation; WIC, Special Supplemental Nutrition Program for Women, Infants, and Children.
not all categories add up to 539 due to item-level non-response
Child development familiarity.
Overall, the mean score on child development familiarity items was 7.5 (SD=2.7) of 11 possible items. Scores differed by ethnicity/language: white participants had the highest unadjusted mean score (M=8.2; SD=2.5) compared to other groups. Latino-EP (M=7.4; SD 2.6) and Latino-LEP (M=7.3 SD=2.4) had intermediate scores, and other race participants had the lowest score (M=6.6; SD=3.2). After adjusting for age, gender, mode of survey administration, and education, all racial/ethnic minority participants scored significantly lower than white participants (Table 2). The other race group had the lowest adjusted score. Significant differences also existed by parental educational attainment, child gender, and survey mode (Table 2).
Knowledge of DDs.
Few participants “knew a lot about” any DD; however, the highest proportions “knew a lot about” ADHD (20.8%), Down syndrome (17.6%), and ASD (16.0%). Except for Rett syndrome, Latinos—particularly those with limited English proficiency—reported the lowest knowledge about DDs. 36.0% of Latino-LEP participants had never heard of ADHD (versus no white participants), 22.0% of Latino-LEP participants had never heard of cerebral palsy (versus 5.2% of white participants), and 21.8% had never heard of cleft lip or palate (versus 2.6% of white participants). As Figure 1 shows, non-white participants were over represented in the population of people who “didn’t know much about” or had “never heard of” common DDs. Significantly more non-white participants reported that they had never heard of one or more of the common DDs compared to white participants (72% versus 52.3%, P < .001).
Figure 1. Frequency of reported knowledge about developmental disabilities by parent ethnicity/language.
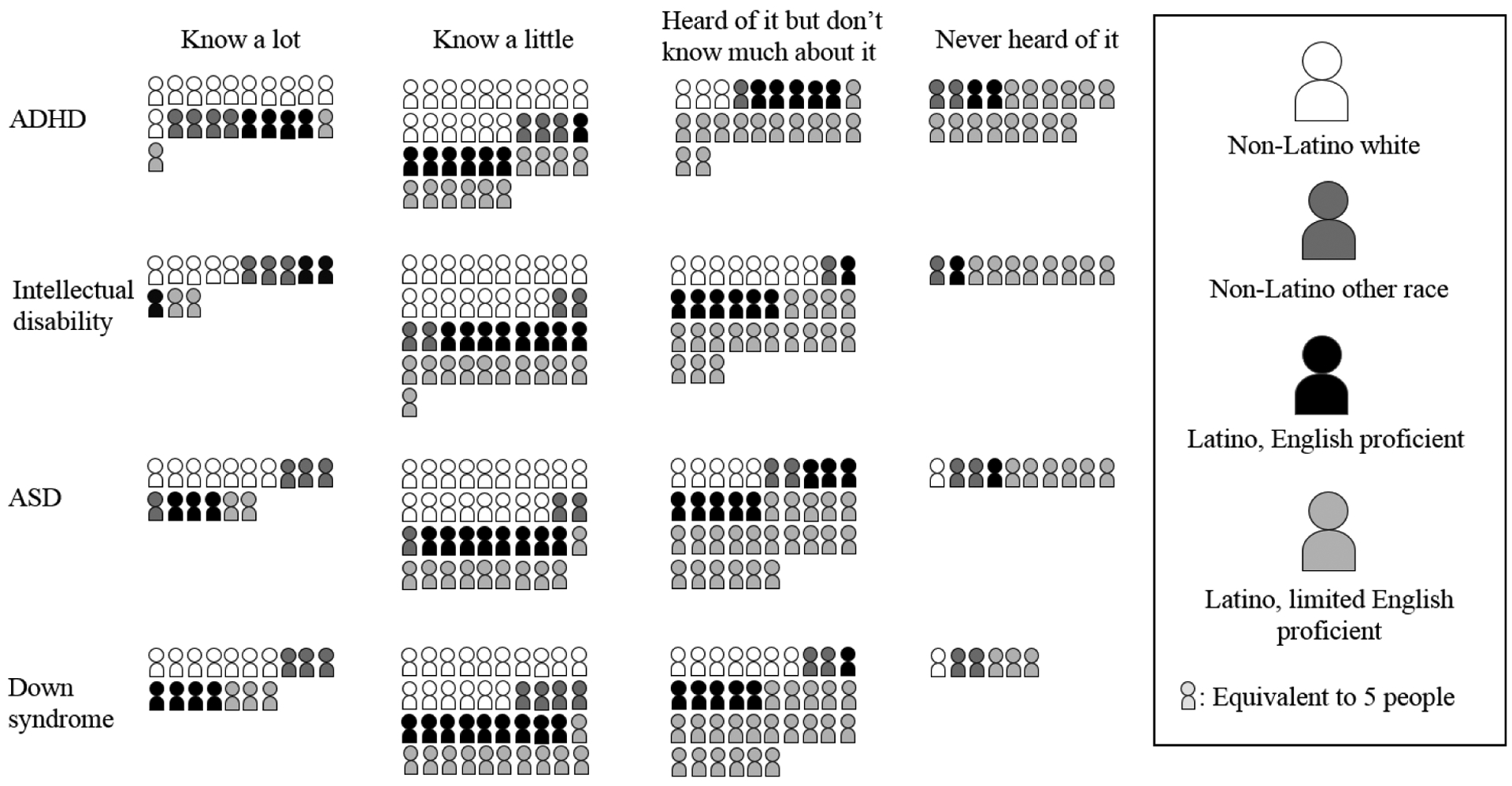
Note: Figure rounds values to the nearest five individuals.
Personal experience with DDs.
Of the DDs queried, participants were most likely to know someone with ADHD (33.6%) or ASD (28.6%). Knowing someone with a DD varied by ethnicity/language: for instance, 63.9% of white participants knew someone with ADHD compared with only 5.8% of Latino-LEP participants, and 43.9% of white participants knew someone with ASD compared with 16.2% of Latino-LEP participants (Supplemental Table 2). After adjusting for education, other socio-demographic factors and mode of survey administration, Latino-LEP participants remained least likely to know someone with all DDs except Down syndrome and Rett syndrome (Table 3).
Table 3.
Logistic regression results: Adjusted odds ratios (95% confidence intervals) of having personal experience (family member or friend) with selected developmental disabilities by race/ethnicity and language (N=539)
| Adjusted Odds Ratio (95% Confidence Interval) for Selected Disabilities by Group | ||||||||
|---|---|---|---|---|---|---|---|---|
| ADHD | Intellectual disability | Autism spectrum disorder | Rett syndrome | Cleft lip/palate | Cerebral palsy | Down syndrome | None of the above | |
| Racial/Ethnic/Language Group | Insufficient observations | |||||||
| Non-Latino, white, English proficient (n = 155) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | |
| Non-Latino, other race, English proficient (n = 55) | 0.39 (0.19 – 0.81) | 0.96 (0.42 – 2.20) | 0.94 (0.48 – 1.85) | 1.54 (0.63 – 3.79) | 0.81 (0.28 – 2.33) | 1.15 (0.48 – 2.75) | 1.24 (0.58 – 2.64) | |
| Latino, English proficient (n = 100) | 0.52 (0.29 – 0.93) | 0.52 (0.24 – 1.15) | 0.61 (0.34 – 1.07) | 0.95 (0.43 – 2,14) | 0.19 (0.05 – 0.69) | 1.50 (0.77 – 2.94) | 1.28 (0.70 – 2.34) | |
| Latino, limited English proficiency (n = 191) | 0.05 (0.02 – 0.12)b | 0.22 (0.07 – 0.63)a | 0.26 (0.15 – 0.46) b | 0.55 (0.21 – 1.46) | 0.10 (0.03 – 0.34) b | 0.77 (0.40 – 1.48) | 4.31 (2.51 – 7.40) b | |
Abbreviation: ADHD, attention deficit hyperactivity disorder.
Logistic regression model adjusted for parent ethnicity, race, and English proficiency, age, gender, education, mode of survey administration, and location of WIC agency. Bold values are significant at p<0.05.
p<0.01;
p<0.001
Advice-seeking.
When asked where they would seek advice about developmental and behavioral concerns, participants most frequently identified a doctor (85%), a partner (48.2%), and WIC (33.4%). Responses did not vary significantly by ethnicity/language.
DISCUSSION
This study investigated knowledge and familiarity about DDs and their early signs among low-income families according to race/ethnicity and English proficiency. Our first finding was that all racial/ethnic minority parents, and particularly other race and Latino-LEP parents, were less familiar with early signs of several common DDs than white parents. Our second finding was that all racial/ethnic minority parents, and particularly Latino-LEP parents, self-reported less knowledge about several common DDs compared to white parents. Our third finding was that all racial/ethnic minority parents, particularly Latino-LEP parents, were less likely than white parents to report having a friend or family member with common DDs. Overall, the study suggests that even in a uniformly low-income sample, parent familiarity, knowledge, and personal experience with DDs varies according to race/ethnicity and language, and these differences persist even after adjusting for parent education. In contrast, there were no ethnic/language differences in advice-seeking behaviors.
Findings about specific DDs were also notable. Of the DDs we asked about, ADHD is the most prevalent.1 Parents in this study knew more about ADHD than any other DD, and were more likely to know someone with ADHD than any other DD. However, some of the largest racial/ethnic disparities in knowledge and familiarity were found for ADHD. For instance, a majority of white parents knew someone with ADHD and knew at least “a little” about it, compared to <10% of Latino-LEP parents. Less pronounced race/ethnicity and language-based disparities also existed in parent knowledge about other DDs such as ASD and intellectual disability, even after controlling for factors such as parental education. These results suggest that factors beyond income and educational attainment, such as access to information, cultural beliefs, or families’ social networks, may play critical roles in DD awareness.
These study findings point to a need to improve the quality of information given to language and ethnic minority families. One strategy could involve offering culturally-specific information about child development and DDs in multiple languages, at a low reading level, and/or in non-print form. Encouraging developmental monitoring (e.g., milestones) and promotion (e.g., reading, singing) in racial/ethnic minority communities may also engender greater understanding of typical developmental trajectories and of deviation from these norms. Parents need to know that their early developmental concerns are important and can be a strong indicator of their child’s developmental status. Parents also need to know that even when a child’s developmental difference does not meet a clinical threshold for DD, it should be actively monitored and addressed. Information on these topics could be distributed through community agencies or safety-net providers (e.g., WIC, Head Start), via social networks, or through traditional media channels (e.g., Spanish-language television or radio). The CDC’s Learn the Signs Act Early campaign32 provides good examples of parent-friendly information on developmental promotion and monitoring in multiple formats.
Health care providers should use study findings to act on DD knowledge needs among low-income families, especially for racial/ethnic minorities or those with LEP. Since all families sought out health care providers as the top information source, front line health care providers are important in reducing DD disparities. Study findings underscore American Academy of Pediatrics recommendations that primary care providers perform proactive developmental surveillance and screening, and not wait for parents to raise concerns. Likewise, when relying on parent reports of a child’s development, providers should be aware that cultural background, knowledge, and familiarity with DDs may affect what parents say. Providers should perform proactive outreach to ensure that racial/ethnic and language minority families seek routine preventive care, where screening and surveillance may take place. Finally, one reason that racial/ethnic minority and limited English proficient families may know less about DDs could be that providers offer these families less and/or lower-quality information about DDs. Providers should be vigilant in counseling families about child development regardless of cultural background or social class. More research is needed to assess which strategies are most effective in enhancing information transfer to parents.
Study strengths include its multicenter design, community-based sampling, and high response rate. Limitations include insufficient representation of races/ethnicities other than Latinos and non-Latino whites. We grouped other race/ethnicities into an “other” category to conserve statistical power; this group consisted of mostly African American and Asian families. We recognize that this group may be heterogeneous in DD familiarity and knowledge. Study findings that “other race” parents had the lowest familiarity with child development items suggest that these parents may have specific needs that are going unaddressed; this is also an area that needs additional investigation. Likewise, survey administration in English and Spanish may have excluded perspectives of limited English proficient parents who speak other languages, who may experience even greater disparities in quality of developmental care.34
Another limitation of this study is that all participants resided in Oregon, where most Latinos are of Mexican origin, and all participants used WIC services, so they may not be representative of U.S. low-income families more generally. Several survey items only asked about certain DDs; caution should be advised in over-generalizing at all developmental conditions. Additional limitations include that the survey’s measure of developmental milestones was not validated against a more comprehensive battery of parent development knowledge. Such a validation was not possible because we could find no comprehensive existing measure appropriate to the study population. In order to mitigate this limitation, we adapted survey items from previously validated instruments, and we conducted extensive cognitive testing. To be cautious, we conducted only relative comparisons, and we draw no conclusions on what level of DD familiarity is “adequate” or “strong.” Nonetheless, parent-child interactions may vary by culture, and the measure may not account for cultural differences in parent-child interactions and child behaviors. The measure may also have been subject to positivity bias, especially when orally administered, because parents may have not wanted to seem “uncaring” about the hypothetical child. For the child development outcomes, this may lead to increased reporting of “yes, concerned,” for milestones where the appropriate answer was “no, not concerned.” We accounted for this limitation by adjusting for survey mode in analyses, but residual confounding could remain. Likewise, the survey may have overestimated child development and DD familiarity, since parents may hesitate to acknowledge lack of familiarity. Finally, the study is cross-sectional and does not link parent beliefs or familiarity with delays in access to DDs services, although other studies have done so.12,36 Other factors not assessed (e.g., presence of medical home), may also be important.
In summary, in this low-income sample of families participating in WIC, racial/ethnic minority and limited English proficient families had less familiarity, self-reported knowledge, and personal experience with several common DDs and their early signs compared to non-Latino white, English proficient families. Advice-seeking behaviors did not differ by ethnicity/language group. Attempts to increase familiarity with DDs and improve information delivery in racial/ethnic minority communities may allow families to recognize early signs of DDs and seek care, which may ultimately help reduce health disparities.
Supplementary Material
Acknowledgements:
This project was funded by grant K23MH095828 from the National Institute of Mental Health (PI = Zuckerman). We acknowledge all of the Oregon WIC staff who assisted with survey data collection. We also acknowledge Max Perelman, MD for his assistance with data collection and entry, Shon Tyler, B.S. for his assistance with data entry, and Christina Nicolaidis MD MPH, for her guidance on project management. Portions of this study were presented as an abstract at the International Meeting for Autism Research, San Francisco, CA, May 10-13, 2017.
REFERENCES
- 1.Houtrow AJ, Larson K, Olson LM, Newacheck PW, Halfon N. Changing trends of childhood disability, 2001–2011. Pediatr. 2014:530–538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hardoff D, Jaffe M, Cohen A, Jonas R, Lerrer-Amisar D, Tirosh E. Emotional and behavioral outcomes among adolescents with mild developmental deficits in early childhood. J Adolesc Health. 2005;36(1):70 e14–79. [DOI] [PubMed] [Google Scholar]
- 3.Powers RL, Marks DJ, Miller CJ, Newcorn JH, Halperin JM. Stimulant treatment in children with attention-deficit/hyperactivity disorder moderates adolescent academic outcome. J Child Adol Psychopharm. 2008;18(5):449–459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sutton PS, Darmstadt GL. Preterm birth and neurodevelopment: a review of outcomes and recommendations for early identification and cost-effective interventions. J Trop Pediatr. 2013;59(4):258–265. [DOI] [PubMed] [Google Scholar]
- 5.Magana S, Parish SL, Rose RA, Timberlake M, Swaine JG. Racial and ethnic disparities in quality of health care among children with autism and other developmental disabilities. Intellect Dev Disabil. 2012;50(4):287–299. [DOI] [PubMed] [Google Scholar]
- 6.Parish S, Magana S, Rose R, Timberlake M, Swaine JG. Health care of Latino children with autism and other developmental disabilities: quality of provider interaction mediates utilization. Am J Intellect Dev Disabil. 2012;117(4):304–315. [DOI] [PubMed] [Google Scholar]
- 7.Morgan PL, Hillemeier MM, Farkas G, Maczuga S. Racial/ethnic disparities in ADHD diagnosis by kindergarten entry. J Child Psychol Psychiatry. 2014;55(8):905–913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Coker TR, Elliott MN, Toomey SL, et al. Racial and ethnic disparities in ADHD diagnosis and treatment. Pediatr. 2016:e20160407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zuckerman KE, Mattox K, Baghaee A, Batbayar O, Donelan K, Bethell C. Pediatrician identification of Latino children at risk for autism spectrum disorder. Pediatr. 2013;132(3):445–453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jimenez ME, Fiks AG, Shah LR, et al. Factors associated with early intervention referral and evaluation: a mixed methods analysis. Acad Pediatr. 2014;14(3):315–323. [DOI] [PubMed] [Google Scholar]
- 11.Travers JC, Krezmien MP, Mulcahy C, Tincani M. Racial disparity in administrative autism identification across the United States during 2000 and 2007. J Spec Educ. 2012. [Google Scholar]
- 12.Zuckerman KE, Lindly OJ, Sinche BK. Parental concerns, provider response, and timeliness of autism spectrum disorder diagnosis. J Pediatr. 2015;166(6):1431–1439.e1431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bornstein MH, Cote LR, Haynes OM, Hahn CS, Park Y. Parenting knowledge: experiential and sociodemographic factors in European American mothers of young children. Dev Psychol. 2010;46(6):1677–1693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bornstein MH, Cote LR. “Who is sitting across from me?” Immigrant mothers’ knowledge of parenting and children’s development. Pediatr. 2004;114(5):e557–564. [DOI] [PubMed] [Google Scholar]
- 15.Pachter LM, Dworkin PH. Maternal expectations about normal child development in 4 cultural groups. Arch Ped Adol Med. 1997;151(11):1144–1150. [DOI] [PubMed] [Google Scholar]
- 16.Ratto AB, Reznick JS, Turner-Brown L. Cultural effects on the diagnosis of autism spectrum disorder among Latinos. Focus Autism Other Dev Disabil. 2015. [Google Scholar]
- 17.Zuckerman KE, Lindly O, Reyes N, et al. Disparities in diagnosis and treatment of autism in Latino and non-Latino white families. Pediatr. 2017;139(5):1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Burkett K, Morris E, Manning-Courtney P, Anthony J, Shambley-Ebron D. African American families on autism diagnosis and treatment: The influence of culture. J Autism Dev Disord. 2015;45(10):3244–3254. [DOI] [PubMed] [Google Scholar]
- 19.Bussing R, Schoenberg NE, Rogers KM, Zima BT, Angus S. Explanatory models of ADHD: Do they differ by ethnicity, child gender, or treatment status? J Emot Behav Dis. 1998;6(4):233–242. [Google Scholar]
- 20.Liu Ka‐Yuet, King Marissa, Bearman Peter S.. Social influence and the autism epidemic. Am J Sociol. 2010;115(5):1387–1434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bussing R, Zima BT, Gary FA, Garvan CW. Barriers to detection, help-seeking, and service use for children with ADHD symptoms. J Behav Health Serv Res. 2003;30(2):176–189. [DOI] [PubMed] [Google Scholar]
- 22.Bussing R, Schoenberg NE, Perwien AR. Knowledge and information about ADHD: evidence of cultural differences among African-American and white parents. Soc Sci Med. 1998;46(7):919–928. [DOI] [PubMed] [Google Scholar]
- 23.Huang K-Y, O’Brien Caughy M, Genevro JL, Miller TL. Maternal knowledge of child development and quality of parenting among White, African-American and Hispanic mothers. J Appl Dev Psychol. 2005;26(2):149–170. [Google Scholar]
- 24.Durkin MS, Maenner MJ, Baio J, et al. Autism spectrum disorder among US children (2002–2010): Socioeconomic, racial, and ethnic disparities. Am J Public Health. 2017;107(11):1818–1826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Froehlich TE, Lanphear BP, Epstein JN, Barbaresi WJ, Katusic SK, Kahn RS. Prevalence, recognition, and treatment of attention-deficit/hyperactivity disorder in a national sample of US children. Arch Ped Adol Med. 2007;161(9):857–864. [DOI] [PubMed] [Google Scholar]
- 26.Flores G, Abreu M, Tomany-Korman SC. Limited English proficiency, primary language at home, and disparities in children’s health care: how language barriers are measured matters. Pub Health Rep. 2005;120(4):418–430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Thorn B, Tadler C, Huret N, et al. WIC participant and program characteristics 2014. Alexandria, VA2015. [Google Scholar]
- 28.American Association for Public Opinion Research. Response Rate - An Overview. http://www.aapor.org/Education-Resources/For-Researchers/Poll-Survey-FAQ/Response-Rates-An-Overview.aspx, Accessed June 2018.
- 29.Townsend MS, Sylva K, Martin A, Metz D, Wooten-Swanson P. Improving readability of an evaluation tool for low-income clients using visual information processing theories. J Nut Educ Behav. 2008;40(3):181–186. [DOI] [PubMed] [Google Scholar]
- 30.Squires J Ages and Stages Questionnaire. Third ed. Baltimore, MD: Brookes Publishing Co.; 2012. [Google Scholar]
- 31.Robins DL, Casagrande K, Barton M, Chen C-MA, Dumont-Mathieu T, Fein D. Validation of the Modified Checklist for Autism in Toddlers, Revised with Follow-up (M-CHAT-R/F). Pediatr. 2014;133(1):37–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Centers for Disease Control and Prevention. Learn the signs. Act early. http://www.cdc.gov/ncbddd/actearly/index.html. Accessed June 2018.
- 33.Vickstrom ER, Shin HB, Collazo SG, Bauman KJ. How well—still good? Assessing the validity of the American Community Survey English-ability question. SEHSD Working Paper 2015; https://www.census.gov/content/dam/Census/library/working-papers/2015/demo/SEHSD-WP2015-18.pdf. Accessed August, 2017. [Google Scholar]
- 34.Knuti Rodrigues K, Hambidge SJ, Dickinson M, Richardson DB, Davidson AJ. Developmental screening disparities for languages other than English and Spanish. Acad Pediatr. 2016;16(7):653–659. [DOI] [PubMed] [Google Scholar]
- 35.Sentell T, Braun KL. Low health literacy, limited English proficiency, and health status in Asians, Latinos, and other racial/ethnic groups in California. J Health Comm. 2012;17 Suppl 3:82–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zuckerman KE, Lindly OJ, Sinche BK, Nicolaidis C. Parent health beliefs, social determinants of health, and child health services utilization among U.S. school-age children with autism. J Dev Behav Pediatr. 2015;36(3):146–157. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


