Abstract
This research aims to explore the correlation between meteorological parameters and COVID-19 pandemic in New Jersey, United States. The authors employ extensive correlation analysis including Pearson correlation, Spearman correlation, Kendall’s rank correlation and auto regressive distributed lag (ARDL) to check the effects of meteorological parameters on the COVID new cases of New Jersey. In doing so, PM 2.5, air quality index, temperature (°C), humidity (%), health security index, human development index, and population density are considered as crucial meteorological and non-meteorological factors. This research work used the maximum available data of all variables from 1st March to 7th July 2020. Among the weather indicators, temperature (°C) was found to have a negative correlation, while humidity and air quality highlighted a positive correlation with daily new cases of COVID-19 in New Jersey. The empirical findings illustrated that there is a strong positive association of lagged humidity, air quality, PM 2.5, and previous infections with daily new cases. Similarly, the ARDL findings suggest that air quality, humidity and infections have lagged effects with the COVID-19 spread across New Jersey. The empirical conclusions of this research might serve as a key input to mitigate the rapid spread of COVID-19 across the United States.
Keywords: Coronavirus, temperature, humidity, air quality, New Jersey, United States
Abbreviations: COVID-19, Corona Virus Disease 2019; Aqi, Air Quality; US, United States; ARDL, Auto-regressive Distributed Lags; SARS-CoV-2, Corona Virus Disease 2019.
1. Introduction
A new type of pneumonia emerged in Wuhan, China at the end of 2019. It was named as coronavirus disease (COVID-19), which officially announced as a global pandemic on 20 February 2020 by World Health Organization (WHO), (Shahzad et al., 2020; Shakoor et al., 2020). This disease symptoms include fever, cough, and acute respiratory disorders like dyspnea, which can lead to pneumonia, acute respiratory syndrome, renal failure, and even death (Hemida and Ba Abduallah, 2020). According to the WHO data, a total of 23 million cases were confirmed with more 808,000 deaths all over the world until 23 August 2020 (WHO, 2020). The deadliest COVID-19 disease increases the risk of infection through the human to human contact (Wang et al. 2020; Chen et al., 2020) and can be able to transmit through the air (Mostafa et al. 2020). The recent literature examined that the contagion of viruses may be affected by several factors such as climatic conditions like temperature and humidity, air pollution, population density, use of masks, and quality of medical care (Iqbal et al., 2020; Kraemer et al., 2020).
Environmental factors influence the transmission rate and survival of epidemiological infectious diseases like coronavirus. Recently, some epidemiological and laboratory research work suggested that the temperature, air quality, and population density are the main outbreak factors for coronavirus disease (Dalziel et al., 2018; Guo et al., 2020; Ma et al., 2020; Tan et al., 2005; Tosepu et al., 2020; Yuan et al., 2006; Xie and Zhu, 2020). In the same line, previous studies reported that the climate and weather conditions affected the spatial distribution and timing of infections (Bedford et al., 2015; Sooryanarain and Elankumaran, 2015; Lemaitre et al., 2019). For example, evidence-based on weather parameters (e.g., temperature and humidity) help to spread the annual influenza epidemics in northern and southern hemispheres during the winter season (Tamerius et al., 2013; Bedford et al., 2015; Sooryanarain and Elankumaran, 2015).
The meteorological and weather parameters could influence the infection rate and disease spread via various channels. For instance, the temperature level, humidity, or air quality might increase or decrease the transmission rate, risk, and survival period of the virus in the air or on surfaces. Hence, the significance and sensitivity analysis of meteorological parameters on coronavirus's infection rate is essential to ensure the survival and safety of humans (Shahzad et al., 2020; Jahangiri et al. 2020).
In this regard, it was reported that some meteorological variables (temperature, humidity, and air) involve in contagion and affect the survival of the SARS virus (Yuan et al., 2006). Climate variables can also be a direct cause of biological interactions between SARS-CoV and humans. Such reasons and factors motivate the researcher to consider the related environmental factors as determinants of COVID-19. To this end, our study joins the strand of recent studies Ma et al., (2020); Shi et al., (2020); Xie and Zhu (2020) and Chen et al. (2020).
Furthermore, recent studies reported that COVID-19 correlates with extreme temperature and weather conditions (Oliveiros et al., 2020; Wang et al., 2020; Ahmadi et al., 2020). The retrospective studies show that the outbreak of severe acute respiratory syndrome (SARS) in 2003, in Guangdong ended with an increase in temperature (Wallis ve Nerlich, 2005). Temperature and its variations were documented to be effective on the spread of SARS (Tan, 2005). Some clinical examinations suggested that COVID-19 patients are probably similar to those of SARS and MERS (Fareed et al., 2020; Shi et al., 2020).
Currently, the United States is a highly affected country with 5.8 million total affected cases and 179,000 deaths. The topmost affected1 states of the United States were ranked as; New York, New Jersey, Massachusetts, California, Pennsylvania, Illinois, Michigan, Florida, and so on. This study focuses on COVID-19 concerning weather indicators in New Jersey, 2nd leading state in COVID-19 fatalities across all US states. In doing so, the authors examined the relationship between confirmed COVID-19 new cases and daily weather indicators in the state of New Jersey to provide beneficial results and implications. Earlier studies reported that the extreme weather conditions that accompany long-term climate change might also contribute to the spread of the West Nile virus in the United States and Europe (Epstein, 2001).
Notably, the theme and objective of this work join the strand of recent literature. More recently, the literature based on meteorological parameters suggested that population, temperature, and humidity significantly influence the COVID-19 spread in different regions of China and Turkey (Shi et al., 2020; Şahin, et al., 2020; Yongjian et al., 2020). On the contrary, Jahangiri et al., (2020) explored that there is no such scientific reason that increases the COVID-19 cases in moderate or cold climates than in warmer regions of Iran. There is still a paucity of research regarding COVID-19 and climate change. To provide useful implications and to take control of the spread of COVID-19, several studies have reported mixed findings regarding the determinants and causing factors of COVID-19. However, the effects of different environmental factors on the incidence of COVID-19 remain to be elucidated.
Currently, the situation is very alarming and dangerous for the United States, causing panic and fear in the population. This research's prime objective is to report new findings and solutions concerning the daily confirmed cases rate of COVID-19 and meteorological parameters (temperature, humidity, air quality index, and PM 2.5). An important contribution of this study is to highlight the lagged effects of meteorological parameters and role of non-meteorological for the daily new cases of COVID-19.
In the empirical analysis, the authors employ the three correlations tests such as Pearson correlation, Spearman correlation, and Kendall's rank correlation from and ARDL approach on the detailed dataset available up till July. Overall, the study reports new findings and conclusions in line with the objective of this work.
2. Environmental Quality in New Jersey
For the case of the United States, the COVID-19 disease has had high infection and transmission rate since its outbreak across all the states of country. In USA, the situation was very strange and surprising, unlike the neighboring countries (Canada, Mexico) or a few other developed nations. Among the states of the United States, New York, New Jersey, California, Florida and taxes are highly affected with higher transmission rate and fatalities due to COVID-19 spread. Up till July, the New Jersey state has witnessed more than 16000 deaths from COVID-19, while the infections and deaths are continuously increasing. New Jersey’s air continues to be among the most polluted in the US, with a large swath of the state receiving failing grades for smog. North Jersey City ranked as the 10th worst metropolitan area in the US for ozone levels. Centers for Disease Control estimates that 735,000 people lived in New Jersey state who suffer from asthma disease due to smog ingredients that can trigger asthma attacks. According to a report by the American Lung Association, they found 161,461 Pediatric asthma patients, 575,425 Adult asthma patients, 437,827 Chronic obstructive pulmonary disease patients, and 4,993 Lung cancer patients due to the environmental pollution in New Jersey state (New Jersey environment department report). New Jersey's smog levels were worse in 2016 because of record high temperatures. The state average temperature rises up to 55 degrees was the third warmest since 1895.
New Jersey (38°56′ N to 41°21′ N, 73°54′ W to 75°34′ W) has adverse environmental issues mainly due to economic activities. The implementation of mandatory lockdown in New Jersey to prevent COVID-19 transmission has resulted in a drastic reduction of environmental pollution by 60 percent. New Jersey's air continues to decline due to older diesel engines on trucks being retired or retrofitted along with the continued closing of coal-fired power plants. New Jersey State and federal government efforts in recent years have been introduced to buy back old high-emission vehicles, impose new restrictions on diesel truck emissions. Still, a considerable amount of air pollution gets blown into New Jersey from coal-burning power plants in the Midwest. The New Jersey administration is looking at rolling back fuel emission standards for cars and small trucks, which environmental advocates say will harm air quality. And it also wants to dismantle the clean power plan that restricts the amount of greenhouse gases that go into the atmosphere and contribute to global warming. Similar executive actions taken by governments worldwide have negative bearings on the economy, but air quality has drastically improved because of these actions (McKibbin and Fernando, 2020).
3. Materials and Methods
3.1. Data Specification
New Jersey is a state of the United States in North America, which is divided into 21 counties. In 2019, its total population was 8.882 million with an area of over 18,920 km2. The population density of New Jersey state is 455.8 residents per km2 (DB-City, 2020). Data are daily concentrations and collected from 1st March till 7th July for the year 2020. The authors have used the most extensive and latest available data.
Data for New Jersey state contain the daily confirmed new cases affected by COVID-19 (COVID); air quality measured as PM 2.5 (PM is proxy); Air quality (Aqi) is an index measuring the mature of air quality measured in percentage; temperature (temp) is measured in degree C°; and humidity (humidity) measured as a share of daily temperature. Data of the COVID-19 was collected from European Union database (European union, 2020).
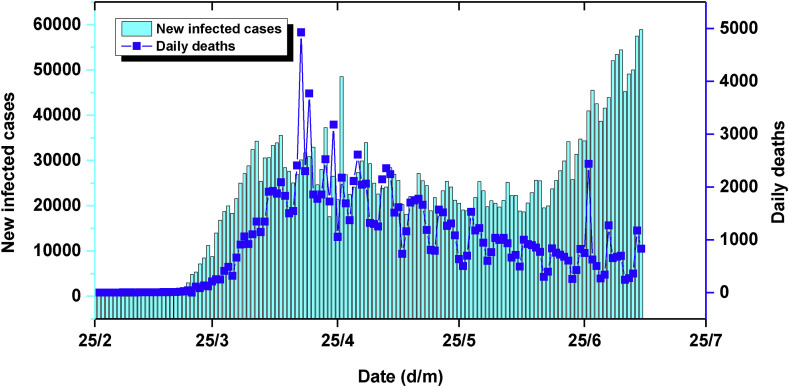
Data on air quality was obtained from United States Environmental Protection Agency database (EPA, 2020). The daily temperature and humidity were obtained from the website of time and data (https://www.timeanddate.com/). Figure 1 shows the tendency of number of confirmed cases and death in USA across time (1st March to 7th July). We observe that the first recorded cases were in the first week of March 2020. The tendency was very weak at the beginning, while in the last week of March 2020 the number of cases recorded increased sharply and exceeds 35000 cases in 11 April 2020. Compared to the number of people affected by the COVID-19 in USA, the number of deaths was low on average at the end of March, however, the number of deaths accelerated in April to reach approximately 5000 cases of death. In extension to empirical analysis, authors further added human development index, health security index, population density and median age as controlling factors. The data for health security index is accessed from center for health security database (https://www.ghsindex.org/), while the human development index data is available at https://globaldatalab.org/shdi/shdi/. Notably, the health security index represents overall health protection and security related rankings, while human development index shows the education and awareness level of population. The population density and median age data is available at the New Jersey government database (https://www.nj.gov/).
Figure 1.
USA COVID-19 Outlook
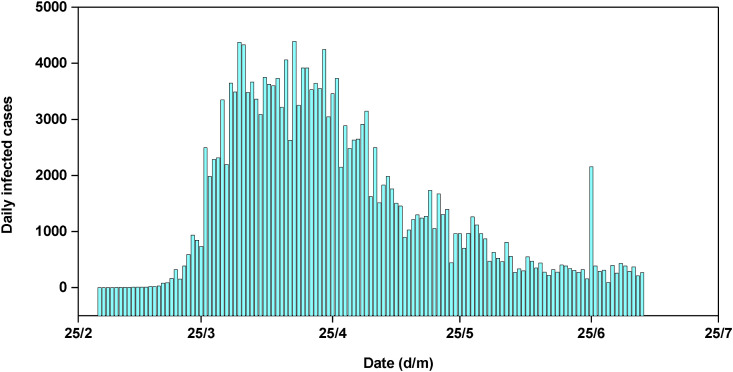
Figure 2 shows the daily new cases of COVID-19 in New Jersey state. The trend of daily confirmed cases in New Jersey has the same skeleton as that of the USA given that New Jersey begins to register confirmed cases in the second week of March (15 cases on 10 March 2020 with a temperature of 17°C and 37% of humidity). The maximum number of daily cases confirmed was 78467 cases on 17 April 2020 (the temperature was equal to 18°C and 59% of humidity).
Figure 2.
Daily New Cases of COVID-19 in New Jersey
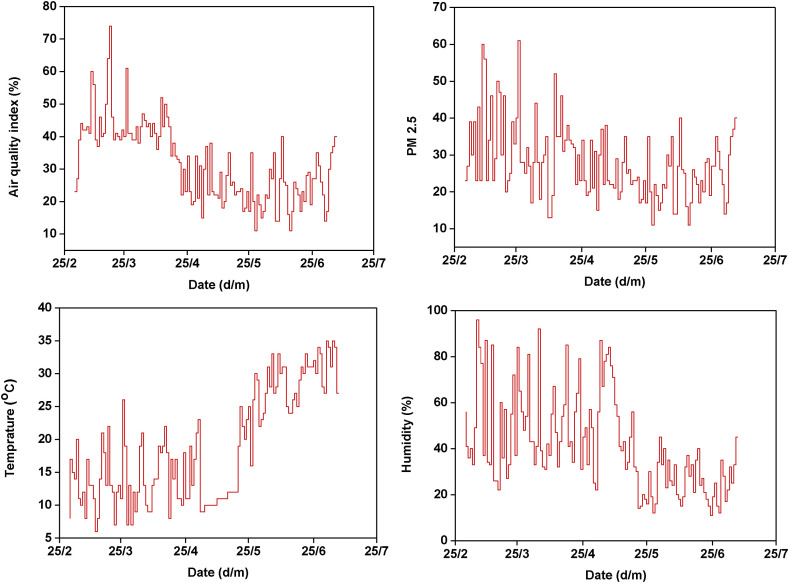
Figure 3 illustrates the temperature (°C), air quality, PM2.5 and humidity variation in New Jersey across the selected period. According to the graph presented in figure 3, we can see that the curve has an upward trend with breakpoint points, causing approximately seasonal effects. The highest temperature value was 26°C on 27 March 2020 (corresponding to an advanced level of daily confirmed cases with 8825) while the lowest level of temperature was 1°C on 22 February 2020 (there are no COVID-19 confirmed cases in that date).
Figure 3.
Trends in environmental indicators in New Jersey during the study period
Figure 3 indicates that the curve is practically stationary with upward and downward tendencies. It suggests that the highest humidity level attains the share of more than 90 percent in the March and April days. While, as per the COVID-19 statistics, the infection rate was high during the mentioned period. Overall, we observe considerable fluctuations in temperature, humidity, and air quality index during the studied period.
3.2. Estimation Strategy
Given that the data was not normally distributed due to the sudden peaks and decline, the empirical analysis use three correlations tests such as Pearson correlation, Spearman correlation and Kendall’s rank correlation. Further, Table 1 presents some descriptive statistics of our analysis variables under investigation. According to these statistics, it is clear that the daily number of cases affected by COVID-19 was so higher to attaint an average of 11277.46 people. The biggest number of cases was equal to 78467 on 17 April 2020. Mature indicator of air quality attaint an average of 46 aqi and it touch a maximum level of 82 aqi on 24 March 2020. Regarding air quality, with an average of 38, the temperature was in lowest minimum of 1°C and the highest maximum temperature was reached 26°C (air quality and aqi has the same level with the maximum temperature degree).
Table 1.
Descriptive Statistics.
| Variables | Obs | Mean | Std.Dev. | Min | Max | p1 | p99 | Skew. | Kurt. |
|---|---|---|---|---|---|---|---|---|---|
| COVID-19 | 129 | 1429.519 | 1368.317 | 0 | 4391 | 0 | 4372 | .725 | 2.085 |
| Air Quality | 129 | 31.752 | 11.867 | 11 | 74 | 11 | 64 | .606 | 3.362 |
| PM2.5 | 129 | 27.798 | 9.856 | 11 | 61 | 11 | 60 | .964 | 4.092 |
| Temperature | 129 | 18.806 | 8.417 | 6 | 35 | 7 | 35 | .378 | 1.776 |
| Humidity | 129 | 41.62 | 20.664 | 11 | 96 | 12 | 92 | .801 | 2.847 |
| Log COVID | 125 | 6.48 | 1.774 | .693 | 8.387 | .693 | 8.383 | -1.491 | 5.068 |
| Log Air Quality | 129 | 3.386 | .387 | 2.398 | 4.304 | 2.398 | 4.159 | -.258 | 2.483 |
| Log PM2.5 | 129 | 3.265 | .347 | 2.398 | 4.111 | 2.398 | 4.094 | -.018 | 2.892 |
| Log Humidity | 129 | 3.605 | .509 | 2.398 | 4.564 | 2.485 | 4.522 | -.163 | 2.445 |
| Log Temperature | 129 | 2.829 | .469 | 1.792 | 3.555 | 1.946 | 3.555 | -.095 | 1.785 |
The Pearson of coefficient correlation is considered for our case in order to measure the degree of linear relationship between two variables. It is known as the best technique of measuring the relationship between variables of interest because it is based on the method of covariance. It gives information about the magnitude of links between the variables and also gives the direction of this association. The computed correlation value should be between -1 and 1, indicating a strong negative correlation or strong positive correlation, respectively.
The formula of the Pearson coefficient correlation is given as follow:
| (1) |
The equation (1) illustrate the Pearson coefficient correlation estimation formula. This estimated coefficient defines the ratio of the covariance () by the product of the standard deviations ().
Using a monotonic function, the rank correlation coefficient () developed by Spearman controls the correlation between the variables. Due to the non-normality of the data, it is well to uses that correlation coefficient in the present analysis (Şahin, 2020). The Spearman's correlation assesses monotonic associations. If there are no repeated data values, a perfect Spearman correlation of +1 or −1 take place when each of the variables is a perfect monotone function of the other.
The coefficient can be defined as follows:
| (2) |
In equation (2) Where denotes the number of the data; indicates the difference in the rank of the element of each random series used. The sign of the Spearman correlation indicates the direction of relationship between the independent and the independent variables. If the dependent variable tends to increase when the independent variable increases, then the spearman correlation coefficient is positive. However, if the dependent variable tends to decrease when the independent increases, then the spearman correlation coefficient is negative. If there is no tendency to increase or decrease for the dependent variable when the independent increases, then the spearman correlation coefficient is equal to zero.
Kendall’s rank correlation is a non-parametric test considered as an alternative to Pearson’s correlation (parametric) to evaluate the degree of relationship based on the pairs of observations. The use of Kendall’s rank correlation is to check for the similarities in the ordering of the data when it is ranked by quantities (towards data science, 2020). The other kinds of correlation coefficients use the observations as the basis of the correlation, while the coefficient of Kendall correlation uses pairs of observations and controls the strength of relationship based on the patter on concordance and discordance between the pairs. The value of Kendall rank correlation is given by the following formula:
| (3) |
In equation (3), Where denotes the number of concordant (ordered in the same way); indicates the number of discordant (ordered in different way) and indicates the number of observations (statistics solutions, 2020). In fact, the estimated correlation coefficient of Kendall is frequently smaller values than those of Spearman and the probability values are more accurate with smaller sample sizes. The main reason for three correlation techniques is just to check if the results are consistent and not spurious.
Lastly, the authors utilize the Auto-regressive Distributed Lag (ARDL) model approach. The main reason to apply the ARDL method is to check the lagged effects of variables. Notably, the ARDL model is employed in two equations as without lag of covariates in equation 1 and with two days lag (t-2) for lag of covaraites. The ARDL method is considered as widely used time-series technique to check the lagged effects of any factors. During the COVID-19 crisis, the researcher’s argued that the there is 2 to 15 days time for transmission and infection (Ma et al., 2020; Hemida and Ba Abduallah, 2020; Wu et al., 2020). Due to this reason, this study further unveils the temporal lagged effects of studied indicators with COVID-19 spread. The ARDL findings provide robust and consistent results on short time data e.g from 90 to 150 oberserbations. In the recent literture, Wu et al., (2020) also employed similar data and empirical strategy.
4. Empirical Results and Discussion
4.1. Empirical results
The results from Pearson correlation tests are reported in Table 2 and show that the correlation between the numbers of confirmed COVID-19 cases and air quality (PM 2.5) is positive and significant (r = 0.1797). On the contrary, temperature has highlighted negative effects on COVID-19 new cases. The empirical finding is in line with the recent research works and argue that temprature might reduce the daily new infections of COVID-19. Such finding is not surprsing and in line with the scientific reasons. The empircal findings are in line with the conclusions of Ma et al., (2020); Shi et al., (2020) and Shahzad et al., (2020) for the case of China. The negative finding justifies that COVID-19 virus might be less stable and less active in high temperature areas.
Table 2.
Pairwise correlation analysis (Pearson correlation).
| Variables | COVID | Air Quality | PM 2.5 | Temperature | Humidity |
|---|---|---|---|---|---|
| COVID | 1.0000 | ||||
| Air Quality | 0.1797* | 1.0000 | |||
| PM 2.5 | 0.0406* | 0.7555* | 1.0000 | ||
| Temperature | -0.3969* | -0.3359* | -0.1208 | 1.0000 | |
| Humidity | 0.2782* | 0.3286* | 0.2883* | -0.6495* | 1.0000 |
Note: * shows significance at the 5% level.
The recent literature has highlighted that under the conditional experiment conditions, the stability of COVID-19 virus is similar to SARS-CoV. Recently, Chan et al., (2011) reported that if temperature ranges from 20 to 25 °C, with humidity of 40%–50%, the SARS-CoV can remain active for up to 4 to 5 days on surfaces. On the contrary, the stability period of SARS-CoV reduce if the temperature and humidity increase. During the studied period the temperature and humidity of New Jersey are increasing, which might be the reason for negative association between temperature and daily new cases. Although the rise in temperature and humidity in New Jersey is due to seasonal fluctuation, while the COVID-19 new cases in New Jersey are also increasing. One more possible explanation for the temperature can be attributed to the immune system of local residents, which is also linked with weather, food and daily routine life of people. The findings of this research are in line with the study of Wu et al., (2020) for the case of panel study on 166 countries. The correlations between air quality index and PM 2.5 are positive. While, the correlation between temperature and COVID-19 is observed negative and statistically significant. However, there is a positive correlation between air quality, humidity and PM 2.5 with COVID-19 new cases.
Table 3 reports the results from the Spearman correlation analysis of Spearman non-parametric tests. The findings indicate the existence of strong positive correlations between COVID-19 and air quality and between COVID-19 and humidity (rs = 0.0785; p<0.05) and (rs = 0.2741; p<0.05), respectively), while the relationship between COVID-19 and temperature is found to be statistically significant and negative (rs = - 0.3237; p<0.05). The spearman correlations between air quality index and PM 2.5 and between PM 2.5 and humidity are strongly proved to be positive and statistically significant at a 1% level of significance (rs = 0.7567; p<0.05) and (rs = 0.2612; p<0.05). The Spearman correlation between air quality index (positive) and the temperature is strongly negative and statistically significant at the 5% significance level (rs = - 0.3185; p<0.05). Overall, the Pearson and Spearman correlation findings report consistent estimates. The estimates of air quality are contrary to the claims of Bashir et al., (2020), who reported inverse impacts of air quality and PM 2.5 with daily new cases and mortality rate in California.
Table 3.
Pairwise correlation analysis (Spearman Correlation).
| Variables | COVID | Air Quality | PM 2.5 | Temperature | Humidity |
|---|---|---|---|---|---|
| COVID | 1 | ||||
| Air Quality | 0.0785* | 1 | |||
| PM 2.5 | 0.0251 | 0.7567* | 1 | ||
| Temperature | -0.3237* | -0.3185* | -0.1313 | 1 | |
| Humidity | 0.2741* | 0.3596* | 0.2612* | -0.6955* | 1 |
Note: * shows significance at the 5% level.
Table 4 reports the results from Kendall's rank correlation. According to these results, we remark that there is practically similar interaction between variables, as mentioned by Spearman rank correlation. In fact, negative significant association are recorded between COVID-19 and temperature and the relationship between COVID-19 and humidity is found to be statistically significant and positive. Two strong positive correlations have verified air quality index and PM 2.5 and between air quality index and humidity at mixed significance levels of 1% and 5%, respectively (τ = 0.6645) and (τ = 0.2419). Finally, Kendall’s rank revealed robust positive correlation of air quality, PM 2.5 and humidity with COVID-19 daily new cases at the 5% significant level.
Table 4.
Pairwise correlation analysis (Kendall’s rank correlation).
| Variables | COVID | Air Quality | PM 2.5 | Temperature | Humidity |
|---|---|---|---|---|---|
| COVID | 0.9981 | ||||
| Air Quality | 0.0648 | 0.9721 | |||
| PM 2.5 | -0.0071 | 0.6645* | 0.9633 | ||
| Temperature | -0.2249* | -0.1932* | -0.0822 | 0.9605 | |
| Humidity | 0.1703* | 0.2419* | 0.1774* | -0.4990* | 0.9823 |
Note: * shows significance at the 5% level.
It is important to go through an econometric regression and check for which of the analysis variables can impact the daily COVID-19 new cases. To this end, the analysis considers the ARDL method. The results from the ARDL regressions are reported in Table 5 . Based on the ARDL approach, the results suggest that the daily lagged coefficient of COVID-19 affects positively the actual value of the confirmed number of cases affected by the COVID-19. Thus, a 1% increase in the daily lagged value of COVID-19 confirmed number of cases will contribute to increasing the present number of cases with 0.44%. The ARDL model is applied with meterological and non-meterological factors as reported in table 5 and 6 . Notably, the researchers employed the ARDL methodology with lag of COVID-19 new cases in equation 1 and with two days lags of covariates. It is important to mention here that due to limited data availability three or more days lags could not be performed in empirical analysis.
Table 5.
ARDL Empirics for New Jersey.
| Variables | Eq-1 (auto-lags of covariates) |
Eq-2 (lag of 2 days for co-variates) |
||
|---|---|---|---|---|
| Coefficient | t-statistics | Coefficient | t-statistics | |
| Log COVID (t-1) | 0.4448*** | 5.5000 | 0.4192*** | 5.120 |
| Log COVID (t-2) | 0.4645*** | 5.9600 | 0.4884*** | 6.2100 |
| Log Air Quality | 0.3101* | 1.7900 | 4.0986* | 1.7100 |
| Log PM 2.5 | -0.1895 | -1.0200 | 3.0304* | -1.1900 |
| Log Temperature | -0.2243** | -1.8900 | -3.3984** | -2.0700 |
| Log Humidity | -0.1215 | -1.1100 | 2.2824* | -1.4900 |
| Constant | 1.2930** | 1.7300 | 1.9413** | 2.2300 |
| Error correction term | -.09068*** | -3.5300 | -0.0923*** | -4.0100 |
| F-Statistic | 233.86 | - | 171.43 | - |
| Adj R-squared | 0.920 | - | 0.362 | - |
| F-bound test | 4.853*** | - | 6.136*** | - |
| t-test | -3.532*** | - | -4.013*** | - |
Notes: The symbols *, **, and *** denote the significance level at 10%, 5%, and 1%, respectively. The ARDL (auto logs) model is estimated with auto lags which estimates the effects of same day. While, ARDL 2 days lags equation reports the estimates of t-2 for all co-variates. The bound tests show that model is stable.
Table 6.
ARDL Empirics robustness check with Non-meteorological.
| Variables | ARDL (Eq-1) |
ARDL (Eq-2) |
||
|---|---|---|---|---|
| Coefficient | t-statistics | Coefficient | t-statistics | |
| Log Air Quality | 2.0844* | 1.4000 | 3.9163** | 1.8000 |
| Log Temperature | -2.8457** | -1.8900 | -3.5353* | -1.7300 |
| Log Humidity | -1.6274 | -1.9100 | -2.8477 | -1.3700 |
| Human development index | -10.3996 | -0.2600 | - | |
| Health security index | -0.2699* | -0.8400 | - | - |
| Population density | - | - | -8.3350* | -0.2700 |
| Median age | 5.6963** | 2.2000 | ||
| Constant | 4.1000** | 4.0110 | 102.0041** | 0.4100 |
| Error correction term | -0.0887*** | -3.4400 | -0.0906** | -3.3300 |
| F-Statistic | 198.35 | - | 55.35 | - |
| Adj R-squared | 0.9201 | - | 0.3351 | - |
| F-bound test | 3.972** | - | 3.542*** | - |
| t-test | -3.442** | - | -3.330** | - |
Notes: The symbols *, **, and *** denote the significance level at 10%, 5%, and 1% respectively. The ARDL eq-1 is estimated with human development index, and health security index as control variables. While, equation 2 is estimated with population density and median age of people. The bound tests show that model is stable.
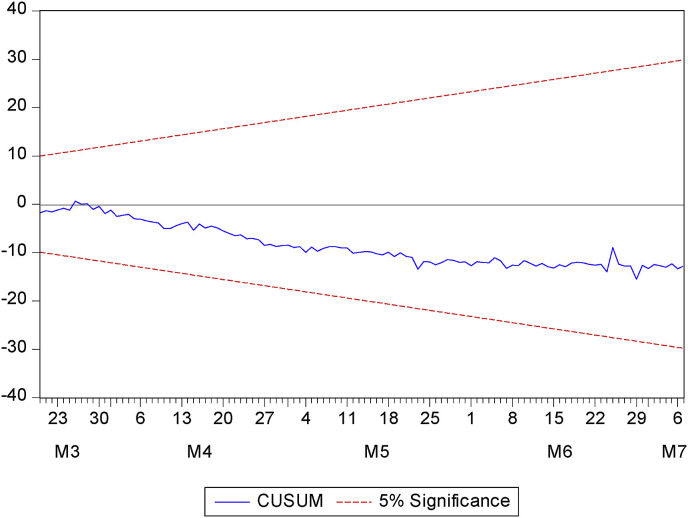
Based on the ARDL approach, the results suggest that the daily lagged coefficient of COVID-19 affects positively the actual value of the confirmed number of cases affected by the COVID-19. Thus, a 1% increase in the daily lagged value of COVID-19 confirmed number of cases will contribute to increasing the present number of cases with 0.44%. Table 5 the results show that PM 2.5, air quality index and humidity values are positive. Notably, PM 2.5, air quality index and humidity each percent increase, resulting in an increase of 3.03%, 0.31% and 2.28% in COVID-19 cases, respectively. In a recent study, Shakoor et al., (2020) also concluded positive association between PM1.0 and COVID-19 in the United States and China. More specifically, temperature shows negative effects on daily new cases. This shows us that the temperature is decisive in the number of COVID 19 cases. Every one percent increase in average temperature is associated with an average decrease in the number of COVID-19 cases of 0.22% and 3.39%, according to ARDL results. The estimates mention that temperature has negative association without lag and with two days lag (t-2) on the COVID-19 new cases. One of the important contributions of this study is to unveil the lagged effects of meteorological indicators on the COVID-19 spread in New Jersey. In the recent literature, Zhang et al., (2020) and Wu et al., (2020) also reported lagged effects of air quality and temperature on COVID-19 for their studies on Chinese cities and 166 countries respectively. The findings of lagged impacts of temperature, air quality and COVID-19 on daily new cases validate the claims of health scientists regarding the incubation period of SARS-CoV-2. Figure 4 illustrate the cumulative sum control chart (CUSUM), which is used to check the validity of ARDL model. Notably, the CUSUM plot shows the validity of ARDL model.
Figure 4.
CUSUM stability model of ARDL findings
The results from the ARDL regressions for non-meteorological indicators is reported in Table 6. In Table 6, we included human development index, health secutrity index, population density and median age as robustness controls. According to the findings, air quality and temperature are positive and negative, respectively. The results revealed that a 1°C increase in temperature was associated with a 2.84% reduction in daily new cases. Notably, a 1 percent increase in air pollution reveals that it is associated with an increase of 2.08% in new daily cases. Further, a 1% increase in health security index and population density, resulting in a decrease of 0.26% and 8.33% in daily new cases, respectively. Median age each percent increase is associated with an average increase in the number of COVID-19 cases of 5.69%. The findings of non-meteorological indicators allow us to draw the narrative that effective health policies, safety measures, education quality and awareness and age of population might be important variables to reduce such pandemics and diseases crisis. Based on such findings, the authors further argue that United States can reforms policies keep in view the health protection, health safety, education, and age groups of population across different states to reduce the rapid COVID-19 transmission.
4.2. Discussion of Findings
The ARDL results show that only air quality and temperature led to affect the daily number of confirmed cases (COVID-19). In fact, at mixed levels of statistical significance levels (1% and 5%), PM 2.5 (resp. temperature) affects positively (resp. negatively) COVID-19. Notably, the lagged findings validate recent research arguments and state that the incubation period might exist between the previous infections, air quality, humidity, and daily new cases of COVID-19. While shaping the policies and regulations for traveling, the incubation period might be considered necessary (Xie and Zhu 2020). Due to this reason, some countries which regulated the traveling with quarantine and smart lockdown measures have successfully controlled the COVID-19 crisis. Such findings can be regarded as a contribution to literature, and it might help to draw new implications to control disease spread in New Jersey. Thus, the intoxication and weather factors could be considered as determining features of COVID-19.
Overall, the results might be due to the fact that the moisture in the exhaled bioaerosols evaporates quickly in low humid areas, forming droplet nuclei that might remain in the air and surface for longer time. Consequently, it can increase the virus transmission. Similalry, the cold weather or low temprature hinders the natural immunity of humans. The low temprature due to rains or winter decrease the blood supply and thus slow down the provision of immune cells to the nasal mucosa (Wu et al., 2020; Shahzad et al., 2020). Overall, the empirical conclusions endorse the findings of Tosepu et al., (2020); and Şahin (2020); Ma et al., (2020); Fareed et al. (2020); Wu et al. (2020); and Chen et al. (2020), and argue that future research can guide about the role of meteorological parameters and COVID-19 disease.
As a final discussion, the three statistical correlations have proved a strong association between the variable COVID-19, air quality index, PM 2.5, and humidity for the New Jersey. In fact, COVID-19 has proved a strong positive correlation with air quality index, PM 2.5 and humidity. This finding can be traduced by the fact that an increase in any one of these weather indicators will affect the number of confirmed cases affected by COVID-19. The findings can provide evidence that air pollution is an important factor in COVID-19 infection. As shown in the literature, air pollution is closely related to other microbes' respiratory tract infections (Horne et al. 2018; Mehta et al., 2013).
The results found that temperature (negative) and humidity (positive) related to COVID-19. This correlation is compatible with previous studies (SARS) (Tan et al., 2005; Yuan et al. 2006). In addition, the humidity and air quality can also be said to be the environmental driving force of the COVID-19 outbreak in China (Shi et al. 2020). This is due to the fact that COVID-19 is sensitive to heat and makes it difficult to survive, not to mention useful factors for virus transmission, such as high temperature, crowding indoors and poor ventilation on cold days (Bunker et al., 2016).
On the contrary, in our study the temperature shows negative effects with COVID-19, while the daily new cases are still increasing. Such findings enable us to consider that temperature may not be an effective variable in the COVID-19 spread. The rise in temperature level is due to seasonal reasons, and it may not be the only determinant of COVID-19 in New Jersey. Such findings are in contrast with the conclusions of Tosepu et al., (2020) and Ma et al., (2020) for their studies on Indonesia and China. The results of this study are inconsistent with the findings of Ahmadi et al., (2020) for the case of Iran. Their study reported that humidity, temperature and wind are closely associated with COVID-19 new infections across different cities of Iran.
The results obtained are consistent with previous literature stating that short-term exposure to air pollution can increase the spread and infection of the coronavirus (Zhang et al. 2020; Shakoor et al., 2020). According to the results, a good global health safety score in New jersey has a positive effect on the daily number of cases. Countries differ widely in their capacity to prevent, detect and respond to outbreaks. The New Jersey sample analyzed has strong operational preparedness capacities, suggesting that an effective response to potential health emergencies, including COVID-19, is possible. Capacity building and cooperation between countries is needed to strengthen global preparedness for epidemic control (Kandel et al. 2020). This study also includes variables that reflect medical conditions, population aging, and population density to reduce confounding bias. The empirics mention that health safety measures and health security precautions might be effective tool to mitigate COVID-19 spread. On the contrary, the study observes positive effects of median age with daily new infections.
Overall, different US states have different environment and weather conditions. Similarly, the situation of COVID-19 across all US states is different, which is related to environment and climate change via various channels. Hence, the policymakers and health scientists can work on combined and synchronized policies to combat such epidemics and fight against climate change issues. It is important to mention here that the analysis is based on New Jersey as a single state due to limited available data. Environmental conditions and weather factors may not be very different across the 21 counties of state; hence the findings can be considered for New Jersey. However, future research might consider the county-level data of COVID-19 and meteorological parameters with the incorporation of population density, urban population, etc.
It is important to mention here that the current study has a few limitations. One caveat of this research is that the study mainly focused on meteorological parameters and could not consider population density, inter-city movement, and masks in the empirical analysis. In the same line, future research can focus on county-level analysis, city-level analysis, and comparative analysis of different states to provide more useful insights regarding the determinants of COVID-19 spread.
5. Concluding Remarks
The Coronavirus (COVID-19) has become a pandemic, and it rapidly affecting all humans beyond race, religion, and age groups. The rapid death rate due to COVID-19 across several developed countries has become a major challenge for researchers, health scientists, policymakers etc. In present study meteorological and non-meteorological factors are highlighted as important factors in determining the rapid spread of COVID-19 in New Jersey. This research unveils interesting and mixed outcomes on the correlation between temperature, air quality, PM2.5, humidity and COVID-19 in New Jersey, United States. Overall, we find that air quality, humidity and previous COVID-19 cases might induce further spread in United States. The correlation findings strongly support the literature and argues that air quality, humidity have direct and lagged effects (0 to 2 days) with the COVID-19 spread in New Jersey. The empirical conclusions are supported by rising number of new cases and deaths across different states of United States. Interestingly, the results further suggest that temperature may not be the real determinant of rapid virus spread in New Jersey. This result justifies that humidity, air quality and temperature are important factors regarding the COVID-19 transmission in New Jersey. Overall, the study offers novel findings and argues that New Jersey state might need reformed policies to combat the virus spread. Based on estimates of non-meteorological indicators the authors further argue that United States can reforms policies keep in view the health protection and safety measures, education quality, and age groups of population across different states to mitigate the rapid COVID-19 transmission.
Although, the data and estimates show significant impacts of humidity, and air quality on COVID-19 in United States, this work has still had some limitations. In a study published Monday(May 18) in Science, Rachel Baker, of the University of Princeton (New Jersey), and his colleagues estimate that the climate seems to modulate the rate of transmission of the virus well: like that responsible for the influenza, but also like the coronaviruses involved in winter colds, SARS-CoV-2 appears to be less active when temperatures and humidity rise. However, this climatic sensitivity has little effect. According to the epidemiological modeling of some researchers, the transmission of the virus is primarily guided by the immunity of the population. Despite very different climatic conditions, the modeling does not show any significant difference in epidemic spread.
For instance, there are several factors need to be investigated related to the COVID-19 virus such as virus resistance, population, urban density, mobility, hygiene, use of masks and sanitizers etc. The future research might evolve around COVID-19 and guide us further about the pandemic, its solutions and causes etc.
Credit author statement
Buhari Doğan: Conceptualization, Data curation, editing. Mehdi Ben Jebli: Methodology, results and discussion. Khurram Shahzad: Introduction writing, data collection, reviewing. Taimoor Hassan Farooq: Figures, revision, suggestions, and, Supervision. Umer Shahzad: Abstract, conclusion, revision, Supervision, and, editing.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgment and Funding
The datasets used during the current study are available on request. We are grateful to editor and anonymous referee's for valuable comments and helpful suggestions.
This work was supported by National Natural Science Foundation of China: [Grant Numbers 71503001, 71974001]; Provincial Natural Science Research Project in Anhui Province: [Grant Number KJ2019A0649].
Footnotes
The facts of United States are available at https://www.theguardian.com/world/ng-interactive/2020/apr/20/coronavirus-map-of-the-us-latest-cases-state-by-state, which are changing continuously.
References
- Ahmadi, M., A. Sharifi, S. Dorosti, et al., 2020. Investigation of effective climatology parameters on COVID-19 outbreak in Iran, Science of the Total Environment, https://doi.org/10.1016/j.scitotenv.2020.138705. [DOI] [PMC free article] [PubMed]
- Bashir M.F., MA B.J., Bilal, Komal B., Bashir M.A., Farooq T.H., Iqbal N., Bashir M. Correlation between environmental pollution indicators and COVID-19 pandemic: A brief study in Californian context. Environ. Res. 2020;187:109652. doi: 10.1016/j.envres.2020.109652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bedford T., Riley S., Barr I.G., et al. Global circulation patterns of seasonal influenza viruses vary with antigenic drift. NATURE. 2015;523:217–220. doi: 10.1038/nature14460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bunker A., Wildenhain J., Vandenbergh A., Henschke N., Rocklöv J., Hajat S., Sauerborn R. Effects of Air Temperature on Climate-Sensitive Mortality and Morbidity Outcomes in the Elderly; a Systematic Review and Meta-analysis of Epidemiological Evidence. Ebiomedicine. 2016;6:258–268. doi: 10.1016/j.ebiom.2016.02.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan K.H., Peiris J.S.M., Lam S.Y., Poon L.L.M., Yuen K.Y., Seto W.H. The effects of temperature and relative humidity on the viability of the SARS coronavirus. Adv. Virol. 2011 doi: 10.1155/2011/734690. 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen B., Liang H., Yuan X., Hu Y., Xu M., Zhao Y., et al. Roles of meteorological conditions in COVID-19 transmission on a worldwide scale. medRxiv. 2020 [Google Scholar]
- Dalziel B.D., Kissler S., Gog J.R., Viboud C., Bjørnstad O.N., Metcalf C.J.E., et al. Urbanization and humidity shape the intensity of influenza epidemics in US cities. Science. 2018;362:75–79. doi: 10.1126/science.aat6030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epstein P.R. West Nile virus and the climate. J. Urban Health. 2001;78:367–371. doi: 10.1093/jurban/78.2.367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- EPA, 2020. Outdoor Air Quality Data. Accessed at: https://www.epa.gov/outdoor-air-quality-data/download-daily-data.
- European union, 2020. European union Coronavirus database 2, number of cases. Accessed at: https://www.ecdc.europa.eu/sites/default/files/documents/COVID-19-geographic-disbtribution-worldwide.xlsx.
- Fareed Z., Iqbal N., Shahzad F., Shah S.G.M., Zulfiqar B., Shahzad K., Hashmi S.H., Shahzad U. Co-variance nexus between COVID-19 mortality, humidity, and air quality index in Wuhan, China: New insights from partial and multiple wavelet coherence. Air Qual. Atmos. Heal. 2020;13:673–682. doi: 10.1007/s11869-020-00847-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo, X.-J., Zhang, H., Zeng, Y.-P., 2020. Transmissibility of COVID-19 and Its Association with Temperature and Humidity. DOI:10.21203/rs.3.rs-17715/v1. [DOI] [PMC free article] [PubMed]
- Hemida M.G., Ba Abduallah M.M. The SARS-CoV-2 outbreak from a one health perspective. One Heal. 2020:100127. doi: 10.1016/j.onehlt.2020.100127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iqbal N., Fareed Z., Shahzad F., He X., Shahzad U., Lina M. The nexus between COVID-19, temperature and exchange rate in Wuhan city: New findings from partial and multiple wavelet coherence. Sci. Total Environ. 2020;729:138916. doi: 10.1016/j.scitotenv.2020.138916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horne B.D., Joy E.A., Hofmann M.G., Gesteland P.H., Cannon J.B., Lefler J.S., Blagev D.P., Korgenski E.K., Torosyan N., Hansen G.I. Short-term elevation of fine particulate matter air pollution and acute lower respiratory infection. Am. J. Respir. Crit. Care Med. 2018;198:759–766. doi: 10.1164/rccm.201709-1883OC. [DOI] [PubMed] [Google Scholar]
- Jahangiri M., Jahangiri M., Najafgholipour M. The sensitivity and specificity analyses of ambient temperature and population size on the transmission rate of the novel coronavirus (COVID-19) in different provinces of Iran. Sci. Total Environ. 2020;728:138872. doi: 10.1016/j.scitotenv.2020.138872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kandel N., Chungong S., Omaar A., Xing J. Health security capacities in the context of COVID-19 outbreak: an analysis of International Health Regulations annual report data from 182 countries. The Lancet. 2020 doi: 10.1016/s0140-6736(20)30553-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kraemer M.U., Yang C.-H., Gutierrez B., Wu C.-H., Klein B., Pigott D.M., du Plessis L., Faria N.R., Li R., Hanage W.P. The effect of human mobility and control measures on the COVID-19 epidemic in China. Science. 2020 doi: 10.1126/science.abb4218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lemaitre J., Pasetto D., Perez-Saez J., et al. Rainfall as a driver of epidemic cholera: comparative model assessments of the effect of intra-seasonal precipitation events. Acta Trop. 2019;190:235–243. doi: 10.1016/j.actatropica.2018.11.013. [DOI] [PubMed] [Google Scholar]
- Ma Y., Zhao Y., Liu J., et al. Effects of temperature variation and humidity on the death of COVID-19 in Wuhan, China. Science of the Total Environment. 2020 doi: 10.1016/j.scitotenv.2020.138226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKibbin, W.J., Fernando, R., 2020. The Global Macroeconomic Impacts of COVID-19: Seven Scenarios. CAMA Working Paper No. 19/2020.
- Mehta S., Shin H., Burnett R., North T., Cohen A.J. Ambient particulate air pollution and acute lower respiratory infections: a systematic review and implications for estimating the global burden of disease. Air Quality, Atmosphere & Health. 2013;6:69–83. doi: 10.1007/s11869-011-0146-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- New Jersey Environment department report. Available at: https://www.northjersey.com/story/news/environment/2018/04/18/new-jerseys-air-among-worst-nation/521041002/..
- Oliveiros B., Caramelo L., Ferreira N.C., Caramelo F. Role of temperature and humidity in the modulation of the doubling time of COVID-19 cases. medRxiv. 2020 doi: 10.1101/2020.03.05.20031872. [DOI] [Google Scholar]
- Şahin M. Impact of weather on COVID-19 pandemic in Turkey. Sci. Total Environ. 2020:138810. doi: 10.1016/j.scitotenv.2020.138810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi P., Dong Y., Yanc H., Zhao C., Li X., Liu W., Hea M., Tang S., Xi S. Impact of temperature on the dynamics of the COVID-19 outbreak in China. Sci. Total Environ. 2020;728:138890. doi: 10.1016/j.scitotenv.2020.138890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shakoor A., Chen X., Farooq T.H. Fluctuations in environmental pollutants and air quality during the lockdown in the USA and China:two sides of COVID-19 pandemic. Air Qual. Atmos. Heal. 2020 doi: 10.1007/s11869-020-00888-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shahzad F., Shahzad U., Fareed Z., Iqbal N., Hashmi S.H., Ahmad F. Asymmetric nexus between temperature and COVID-19 in the top ten affected provinces of China: A current application of quantile-on-quantile approach. Sci. Total Environ. 2020;736:139115. doi: 10.1016/j.scitotenv.2020.139115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sooryanarain H., Elankumaran S. Environmental role in influenza virus outbreaks. Annu. Rev. Anim. Biosci. 2015;3:347–373. doi: 10.1146/annurev-animal-022114-111017. [DOI] [PubMed] [Google Scholar]
- Tamerius J.D., Shaman J., Alonso W.J., et al. Environmental predictors of seasonal influenza epidemics across temperate and tropical climates. PLoS Pathog. 2013;9 doi: 10.1371/journal.ppat.1003194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tan J. An initial investigation of the association between the SARS outbreak and weather: with the view of the environmental temperature and its variation. Journal of Epidemiology & Community Health. 2005;59(3):186–192. doi: 10.1136/jech.2004.020180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tosepu R., Gunawan J., Effendy D.S., Lestari H., Bahar H., Asfian P. Correlation between weather and Covid-19 pandemic in Jakarta, Indonesia. Sci. Total Environ. 2020;725:138436. doi: 10.1016/j.scitotenv.2020.138436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wallis P., Nerlich B. Disease metaphors in new epidemics: the UK media framing of the 2003 SARS epidemic. Soc Sci Med. 2005;60(11):2629–2639. doi: 10.1016/j.socscimed.2004.11.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang M., Jiang A., Gong L., Luo L., Guo W., Li C., Zheng J., Li C., Yang B., Zeng J. Temperature significant change COVID-19 transmission in 429 cities. medRxiv. 2020 doi: 10.1101/2020.02.22.20025791. [DOI] [Google Scholar]
- World Health Organization (WHO) 2020. Coronavirus disease 2019 (COVID-19) Situation Report-132. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports.
- Wu Y., Jing W., Liu J., Ma Q., Yuan J., Wang Y., Du M., Liu M. Effects of temperature and humidity on the daily new cases and new deaths of COVID-19 in 166 countries. Sci. Total Environ. 2020;729:1–7. doi: 10.1016/j.scitotenv.2020.139051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yongjian Z., Jingu X., Fengming H., et al. Association between short-term exposure to air pollution and COVID-19 infection: Evidence from China. Science of the Total Environment. 2020 doi: 10.1016/j.scitotenv.2020.138704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuan J., Yun H., Lan W., Wang W., Sullivan S.G., Jia S., et al. A climatologic investigation of the SARS-CoV outbreak in Beijing, China. Am. J. Infect. Control. 2006;34:234–236. doi: 10.1016/j.ajic.2005.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xie J., Zhu Y. Association between ambient temperature and COVID-19 infection in 122 cities from China. Sci. Total Environ. 2020:138201. doi: 10.1016/j.scitotenv.2020.138201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Z., Xue T., Jin X. Effects of meteorological conditions and air pollution on COVID-19 transmission: Evidence from 219 Chinese cities. Sci. Total Environ. 2020;741:140244. doi: 10.1016/j.scitotenv.2020.140244. [DOI] [PMC free article] [PubMed] [Google Scholar]