Abstract
Background
In 2018, a large mumps epidemic coincided with an outbreak of diphtheria in refugee camps established in Bangladesh for the Rohingya people. These refugees did not receive a mumps-containing vaccine.
Methods
Cases of mumps were reported to the WHO's Early Warning, Alert and Response System (EWARS) during the Rohingya refugee crisis. The authors present amalgamated epidemiological data of a major, previously under-reported, mumps epidemic.
Results
In total, 19 215 mumps cases across a total of 218 facilities were reported to EWARS during 2018. The attack rate was 2.1% of the whole population. Of these cases, 7687 (40%) were in children aged <5 y. Mumps was more commonly seen among males than females.
Conclusion
Detailed reporting of outbreaks of all vaccine-preventable diseases is essential to ensure appropriate vaccination decisions can be made in future humanitarian crises.
Keywords: diptheria, mumps, refugee, Rohingya, under-reported, vaccination
Introduction
Since August 2017, over 740 000 Rohingya people have fled violence in Rakhine State, Myanmar and sought refuge in Cox's Bazar District in southern Bangladesh. Most have settled in Kutupalong Refugee Camp, which now has a population exceeding 914 000, including Rohingya refugees who fled from previous violence and a small number of the Bangladeshi host population.
Limiting vaccine-preventable diseases (VPDs) is a key public health intervention, especially in scenarios associated with displacement. VPDs with high morbidity and mortality are prioritised; however, it is important to consider vaccination against all VPDs, including those with low case fatality rates such as mumps.
Prior to arrival in Bangladesh, the Rohingya population had not received adequate vaccinations. A retrospective survey of vaccination coverage conducted by Médecins Sans Frontières (MSF) estimated measles vaccination coverage of less than 25% among children aged 6 to 59 mo at the start of the crisis.1
During the Rohingya crisis, two subsequent measles-rubella (MR) vaccination campaigns took place from September to November 2017. Oral cholera vaccination campaigns were implemented following a risk assessment and diphtheria, pertussis and tetanus vaccinations were administered following a diphtheria outbreak. No mumps-containing vaccine was given during the campaigns.
We provide the first description of a large mumps epidemic that occurred among Rohingya refugees in 2018. This outbreak was not included in the local weekly epidemiology bulletins created by the WHO2 and has not been documented in the literature. We discuss how vaccination decisions are made in acute humanitarian emergencies and how detailed reporting of all outbreaks, including those of low morbidity and mortality, is important to aid future vaccination decisions.
Materials and methods
Prior to publication, the authors obtained permission from the WHO and the Bangladesh Ministry of Health and Family Welfare (MoHFW) to access the amalgamated epidemiological data collected for all suspected mumps cases among the Rohingya refugees from December 2017 to December 2018.
Epidemiological data during the crisis were collected through the WHO's Early Warning, Alert and Response System (EWARS), a disease surveillance system commonly used in humanitarian settings, whereby users monitor a maximum of 12–14 selected diseases or health events. These conditions are chosen by consensus between the WHO, humanitarian organisations and the local ministry of health. Case definitions and thresholds for reporting and investigating alerts are prespecified for each condition.
In December 2017, EWARS was initiated in the Rohingya refugee camps through a partnership of the WHO and the Bangladesh MoHFW. Prespecified conditions for monitoring were selected.3 Mumps was not among these conditions.
EWARS depends on reporting by local healthcare workers, using either clinical, laboratory or epidemiological definitions for diagnosis. The mumps case definition used during the crisis was an ‘acute onset of unilateral or bilateral tender or self-limited swelling of the parotid or other salivary gland lasting ≥2 days without other apparent cause’. All cases were reported based on clinical suspicion. No confirmatory laboratory testing was undertaken.
Data were submitted to EWARS via an electronic case report form in real time with smartphone applications or at the end of each working day via laptop. Each case report documented the patient's gender, whether under or over 5-y-old, the patient's residence by camp number and the camp number of the reporting health facility.
Data for our study were analysed using Microsoft Excel version 1803 (Microsoft Corp., Redmond, WA, USA). Maps were generated using ArcGIS Pro version 2.2.0 (Esri, Aylesbury, UK) with files obtained from the Humanitarian Data Exchange.
Results
The first two suspected mumps cases were reported to EWARS on 17 January 2018 (Epidemiology (Epi) week 3). Both cases were male and aged >5 y. They were reported from a Ministry of Health Upazila health complex (Upazila being the local name for an administrative region). This facility was located on the outside border of the Kutupalong Refugee Camp, which acted as a secondary referral centre with inpatient beds available during the crisis.
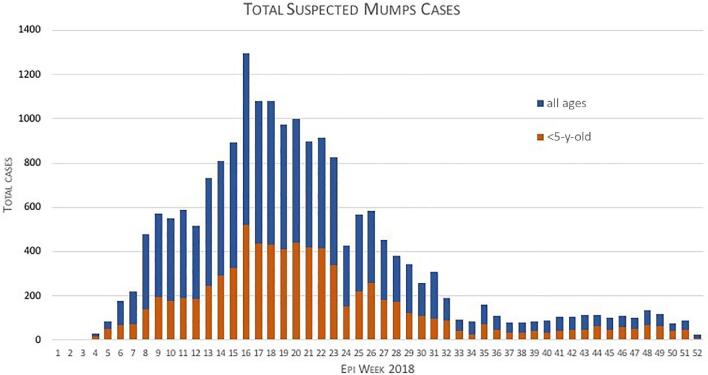
Case numbers escalated weekly producing a classic epidemic distribution (Figure 1). More than 500 weekly cases were reported consistently through Epi weeks 9–23. The peak of the outbreak was seen in Epi week 16 when 1292 cases were reported.
Figure 1.
Stacked bar chart depicting mumps case numbers reported to EWARS from 1 January 2018 (Epi week 1) to 31 December 2018.
In total, 19 215 cases were reported from January to December 2018, 7687 of which (40.0%) were in children aged <5 y. Mumps was more commonly seen among males than females and this was consistent for children aged <5 y (4146 males [53.9%] and 3541 females [46.1%]) and >5 y (5858 males [50.8%] and 5670 females [49.2%]).
Data regarding potential complications of mumps including meningitis, encephalitis, orchitis, oophoritis and pancreatitis were not available to the authors.
Given that the estimated population data released by the International Organisation for Migration in December 2018 totalled 909 207, this produces an estimated attack rate of 2.1%. Population data for children aged <5 y are not available.
Cases were reported from a total of 218 facilities, including those run by local government health facilities and international non-governmental organisations. MSF reported the majority of cases (13 627/19 215 [70.1%]).
Cases were reported from 92% of camps. The highest number of cases came from Camp 9, where 5401 cases were reported. Camp 15 reported 3047 cases and those in Camps 2W, 14 and 16 reported >1000 cases. Camps in existence prior to August 2017 (Kutupalong RC and Nayapara) reported far fewer cases (<10) (see Supplementary Data 2A and 2B).
Discussion
Our study provides the first description of a major mumps epidemic among Rohingya refugees. Cases were reported across multiple camps over multiple geographical locations, suggesting a high infectivity and high epidemic potential of mumps in a refugee crisis.
The hallmark feature of mumps virus infection is painful swelling of the parotid gland. Although generally benign and self-limiting, complications including aseptic meningitis, encephalitis, epidiymo orchitis and oophoritis can occur. Mumps can also cause spontaneous abortion in the first trimester of pregnancy, which is particularly relevant in a camp with a large population of women of childbearing age. This epidemic was not reported in the weekly epidemiology bulletin.2 While it can be understood that concurrent outbreaks of high morbidity and mortality diseases such as diphtheria, measles and acute jaundice syndrome were prioritised, it is nonetheless important that there is a record of this mumps epidemic as it has implications for planning in the current situation and subsequent acute humanitarian emergencies.
The WHO has a framework for vaccination decisions in acute humanitarian emergencies.4 The framework concentrates on three stages of decision-making: first, calculating the epidemiological risk posed by each VPD; second, considering vaccine properties; and third, prioritisation of vaccination alongside other public health interventions.
When considering epidemiological risk it is critical to search the literature for previous documented outbreaks of VPDs. A literature review of VPDs in refugees and internally displaced persons from 2000 to 2015 documented only 1 mumps outbreak report, whereas there were 16 articles for measles, 5 for polio and cholera and 1 for rubella.5 This mumps epidemic among Rohingya refugees, the largest ever recorded in a refugee population, has remained unreported in the literature until now.
During the health sector response to this crisis, Rohingya refugees received MR vaccine rather than measles-mumps-rubella (MMR). Despite its low case fatality rate, this large mumps epidemic increased pressure on already stretched curative health services. Combining this with the fact that targeting mumps can be opportunistically coupled with vaccinations against measles, consideration should be made for MMR vaccination in similar humanitarian crises in the future.
A key consideration in any vaccination campaign is cost. MR vaccines are cheaper than MMR vaccines. An economic cost analysis comparing the cost of an MR vs an MMR vaccination campaign with the cost of managing 19 215 cases and potential complications of mumps is an area for further research.
An important confounding factor unique to this crisis was that the mumps epidemic coincided with an ongoing diphtheria outbreak. The most commonly reported symptoms of diphtheria were fever, sore throat and difficulty in swallowing. These symptoms were also commonly reported by patients with mumps, leading to large case numbers being referred as suspected diphtheria. This led to patients with mumps waiting in isolation facilities alongside probable diphtheria cases. Given the similarities in case presentation it is believed that patients diagnosed with suspected diphtheria may in fact have had mumps, and indeed some patients diagnosed with suspected mumps may have had, or become infected with, diphtheria. This strengthens the argument for including mumps in vaccination campaigns targeting vulnerable populations with previously low immunisation rates. It also raises the question as to why vaccination against diphtheria was not also prioritised. This is another issue requiring further research.
Our study has limitations. First, all cases reported in this mumps epidemic were diagnosed upon clinical suspicion. No confirmatory testing for mumps was undertaken. Second, when implementing EWARS, users must set a locally appropriate threshold for reporting and investigating an alert. As the authors did not work alongside the local epidemiology team the thresholds set for mumps are not known in this paper.
Conclusions
This previously unreported mumps epidemic among Rohingya refugees is the largest ever recorded in a refugee population. The mumps epidemic coincided with an outbreak of diphtheria. Clinical similarities between mumps and diphtheria may have led to inappropriate case management and placed individuals at increased risk of acquiring either mumps or diphtheria. Detailed reporting of outbreaks of all VPDs, including diseases of low morbidity and mortality, is essential to ensure appropriate vaccination decisions can be made in future humanitarian crises.
Supplementary Material
Acknowledgements
Great thanks to Jessy Hampton for her time creating the maps shown in the Supplementary data.
Contributor Information
Luke Mair, Department of Clinical Sciences, Liverpool School of Tropical Medicine, Liverpool, UK; Tropical and Infectious Diseases Unit, Liverpool University Hospitals NHS Foundation Trust, Liverpool, UK; Infectious Diseases Department, Sheffield Teaching Hospitals, Sheffield, UK.
Pryanka Relan, Department of Emergency Medicine, Mount Sinai Health System, New York, NY, USA.
David Oliver Hamilton, Critical Care Department, Liverpool University Hospitals NHS Foundation Trust, Liverpool, UK.
Abdullah Al-Noman, Department of Maternal & Child Health, National Institute of Preventive and Social Medicine (NIPSOM), Dhaka, Bangladesh.
Timothy O'Dempsey, Department of Clinical Sciences, Liverpool School of Tropical Medicine, Liverpool, UK.
Authors’ contributions
LM and PR conceived the study. TOD provided supervision throughout. All authors were involved in study implementation. DOH acted as liaison with the local Ministry of Health and AAN as liaison with the WHO in the collection and obtaining of data. LM and PR analysed and presented the data. LM, PR and DOH wrote the manuscript. All authors edited the manuscript. All of the authors have reviewed and approved the final version of the manuscript.
Funding
No funding was received.
Competing interests
None declared.
Ethical approval
Not required.
References
- 1. Grellety E, Falq G. Retrospective mortality, nutrition and measles vaccination coverage survey in Balukhali 2 and Tasnimarkhola camps. 2017. Epicentre Médecins Sans Frontières. https://www.msf.org/sites/msf.org/files/report-rohingyas-emergency-17-vf1.pdf [accessed September 2019]. [Google Scholar]
- 2. World Health Organisation Bangladesh. Rohingya Crisis. Weekly Epidemiology Bulletin. http://www.searo.who.int/mediacentre/emergencies/bangladesh-myanmar/en/ [accessed December 2019].
- 3. Karo B, Haskew C, Khan AS, et al. World Health Organization Early Warning, Alert and Response System in the Rohingya crisis, Bangladesh, 2017-2018. Emerg Infect Dis. 2018;11:2074–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. World Health Organisation Vaccination in acute humanitarian emergencies: a framework for decision making. Department for Immunisation Vaccines and Biologicals. 2013. WHO/IVB/13.07. [Google Scholar]
- 5. Lam E, Mccarthy A, Brennan M. Vaccine-preventable diseases in humanitarian emergencies among refugee and internally-displaced populations. Hum Vacc Immunother. 2015;11:2627–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.