Abstract
Background and Aim
We have previously reported improvement of clinical symptoms of genitourinary syndrome of menopause (GSM) at 3 and 6 months following three CO2 laser treatments. The current paper presents the results of long term follow up at 12, 15- and 18-months post laser treatment.
Methods
Twenty subjects (mean age 60.65 ± 6.34 years) who had completed the core study participated in follow-up. Subjects were evaluated at 12, 15, and 18 months following final laser therapy. An optional maintenance treatment was offered during Month 12 and Month 15 to those women who failed to increase their Vaginal Health Index Score (VHIS) by more than 34% from their individual baseline, or if the subject desired an additional treatment. At each study visit, VHIS and vulvovaginal atrophy (VVA) symptom severity were recorded. Sexual function was assessed using the Female Sexual Function Index (FSFI).
Results
Fifteen subjects were eligible for a single maintenance treatment (N = 2, at 12 months, and N = 13 at 15 Months). The mean VHIS (± standard deviation) remained significantly improved at 12 months following their last laser treatment (16.3 ± 4.5 vs. Baseline 12.4 ± 4.0; p < 0.05) and at the 15- and 18-months follow up visits as well (16.9 ± 4.6 and 17.1 ± 4.6, respectively; p < 0.05 compared to Baseline). Almost all VVA symptoms were significantly improved at 12 months following the third treatment compared to Baseline and this improvement was sustained at 15 and 18 months. At the 12 Months visit, the total FSFI score increased significantly (N = 15, 24.4 ± 6.9; p < 0.05), and at the 15- and 18-month follow-up visits, the total FSFI remained significantly higher than Baseline (22.2 ± 6.7, 25.8 ± 6.6).
Conclusion
Fractional CO2 laser treatments are effective in alleviating symptoms of VVA and sexual dysfunction in post-menopausal women, and that effects are sustained over the long-term.
Keywords: CO2 laser, vulvovaginal atrophy, menopause, sexual function
Introduction
In premenopausal women, estradiol levels fluctuate between 10 and 800 pg/mL over the menstrual cycle. Following menopause, the levels decrease to below 30 pg/mL, causing the vaginal wall to become thinner, prone to petechiae, pale, less elastic and dry. The vagina can narrow and shorten and the introitus may constrict. These changes underlie the genitourinary syndrome of menopause (GSM), formerly known as vulvovaginal atrophy, manifested clinically as a constellation of symptoms that include vaginal burning, dryness, itching, dyspareunia, and lower urinary dysfunction 1, 2). Furthermore, changes in the vaginal wall flora and pH leave post-menopausal women more prone to urinary-tract infections 3). GSM-associated symptoms can adversely affect women's sexual function and lower their quality of life 4), and while they affect 20% to 45% of midlife and older women, only a minority seek help 5).
In recent years, laser treatments, including fractional CO2 laser and erbium:YAG (Er:YAG), have emerged as effective and safe treatment options for GSM symptoms in post-menopausal women. Fractional CO2 laser treatments, usually consisting of three laser treatments provided in monthly intervals, have been shown to improve GSM symptoms at the completion of the treatment protocol or at 4 weeks following the final laser treatment 6–8).
Recently, a panel of experts has conducted a review of literature and extensive discussions on the available data concerning the effectiveness and safety of energy- based technologies for the treatment of GSM symptoms including reduction of vaginal laxity, improvement of sexual function and alleviation of stress urinary incontinence. The panel concluded that for patients with mild-to-moderate medical conditions, the treatments are safe, effective, and well tolerated 9).
As with any emerging medical field, data is still needed regarding the long-term efficacy and safety of these treatments 10, 11), accordingly, some studies assessing the effects of laser therapy in GSM for longer than 3 months have been published. Samuels and colleagues have shown that at 12 months of follow-up, the vaginal health improvement achieved after 3 fractional CO2 treatments was maintained 12, 13).I have previously reported the results of a prospective study in 28 healthy post-menopausal women with VVA-related symptoms that were treated with fractional CO2 laser 3 times, in 4-week intervals 14). In the study, the mean vaginal health index score (VHIS) was significantly improved (13.89 ± 4.25 vs. Baseline 11.93 ± 3.82; p < 0.05) one month following the initial laser treatment and further improved at 3 and 6 months following all three laser treatments (16.43 ± 4.20 and 17.46 ± 4.07, respectively). Almost all VVA symptoms were significantly improved at the first visit following initial treatment. Further significant improvement in VVA symptoms was noted at 3 and 6 months. Following laser therapy, the Female Sexual Function Index (FSFI) score increased significantly (22.36 ± 10.40 vs. Baseline 13.78 ± 7.70; p < 0.05) and remained significantly higher than baseline at the 3- and 6-month follow-up visits.
The current paper presents the results of 12, 15 and 18 months of follow-up post third laser treatment, conducted in 20 of the above-mentioned core study.
Materials and Methods
Study Design
This was a follow-up study of a prospective trial of postmenopausal women presenting with VVA-related symptoms. The follow-up was conducted between June 2017 and April 2018 at the Center of Women's Health and Wellness, Lawrenceville, New Jersey USA. The protocol was approved by Schulman Institutional Review Board. Specific written informed consent to participate in the follow- up was obtained from all subjects.
Study Population
The follow-up was conducted on 20 patients out of the 28 who have completed the core study. None of the subjects who declined to participate in the follow-up was due to safety reasons. All 20 women completed the follow- up study.
Main inclusion criteria for the core study, as previously reported 14), were: sexual activity or desire for sexual activity, menopausal status, and one or more VVA-related symptoms (e.g. dryness, itching, burning, dysuria or dyspareunia). Women that had VHI scores below 5 (Gloria Bachmann's Vaginal Health Index (VHI) 15), systemic steroid or hormonal use in previous three months, active genital infection, recurrent urinary tract infections, abnormal Pap smears, or pelvic organ prolapse (POP) > II, were excluded.
Study Protocol and Procedure
Subjects were seen at three visits at 12, 15, and 18 months following the third laser and final treatment of the core study (14, 17, and 20 months after Baseline). The protocol included optional maintenance treatments at the Month 12 and Month 15 visits in cases in which: 1) individual patient score of VHIS at the time of the FU visit was less than 34% increase from the individual baseline or 2) subject desired additional treatment.
Subjects were asked to refrain from using vaginal lubricants seven days prior to treatment. The treatment of the vaginal canal, when applicable, was provided by the FemTouch™ handpiece of the Lumenis AcuPulse™ system. The FemTouch™ handpiece was inserted into the vagina and the fractional CO2 laser energy was transmitted through the handpiece along the vaginal canal in a retrograde manner. Treatment settings were determined by the physician, based on the degree of vaginal atrophy and varied at 7.5, 10 or 12.5 mJ.
Following treatment, subjects were instructed to avoid heat exposure in the treated area and refrain from sexual activity up to 72 hours. Subjects were asked to document the timing of resumed sexual activity after the procedure.
Data Collection
Demographic data and medical history data collected during the core study were verified and updated. At each study visit, vaginal health was assessed by the investigator and a VHIS consisting of five vaginal parameters: Elasticity, Secretion/fluid volume, Vaginal pH, Integrity of the epithelium, and Lubrication/moisture of the vaginal wall, was recorded. VVA symptom severity was self-evaluated by study participants on a 10cm visual analogue scale (VAS).
Subjects were asked to rate treatment discomfort / pain immediately after treatment in the following categories: insertion of the probe into the vagina, movement of the probe inside the vagina and laser irradiation inside the vagina. The rating was based on a pain VAS where the extreme left indicates “no pain” and extreme right indicates “intolerable pain”.
The FSFI, a questionnaire designed to measure sexual functioning in women with a specific focus on sexual arousal, orgasm, satisfaction, and pain during the 4 weeks preceding study visit 16) was collected at each visit. In addition, “sexual downtime”, defined as the period of time following the procedure during which the subject could not have sexual intercourse, was reported by the subjects at treatment visits following procedures.
The subject's overall satisfaction level with the treatment procedure and outcome were assessed after each treatment, using a 5-point Likert scale where 0 represents “very dissatisfied” and 4 represents “very satisfied”.
Statistical Analysis
All statistical analyses were performed using SAS® version 9.4 (SAS Institute, Cary NC, USA) software. Statistical tests performed were two-sided. The level of significance is 0.05. All p-values are nominal.
Descriptive statistics (frequency – count and proportion, mean, standard deviation, minimum, median and maximum) are presented for the background variables and study variables.
The Baseline for assessments of change in the follow-up study was the Baseline of the core study, prior to any laser treatment. The changes from baseline in the VHIS, subject assessment of VVA symptoms and FSFI were evaluated using repeated measures analysis of variance models, where the changes were modelled (individually) as a function of respective baseline values and visit number (categorical).
No sample size calculation was performed for the follow-up study.
Results
Demographic and Baseline Characteristics of Study Population
20 of the 28 women who completed the core study agreed to participate in the follow-up study, and all of them completed 18 months of follow-up (counted from the third treatment of the core study). Demographic and other baseline characteristics are presented in Table 1.
Table 1: Demographic Characteristics of The Study Population.
| Characteristic | N = 20 |
|---|---|
| Age (years) | 60.65 ± 6.34 |
| Mean body mass index (kg/m2) | 26.12 ± 4.75 |
| Previous Vaginal Deliveries | 60% (12/20) |
| Time Since Last Spontaneous Menstrual Bleeding (months) | 106.15 ± 66.94 |
Data are presented as mean ± standard deviation (continuous variables) or % (n/N) (categorical variables).
Maintenance Treatments
In total, 15 subjects were eligible for a maintenance treatment; 14 subjects based on visit VHIS that was less than 34% increase from her individual Baseline and 1 subject based on her elective desire for an additional treatment. At the 12-months visit, treatment was provided to 2 subjects and at the 15-months visit, to an additional 13 subjects. Each of the 15 subjects received a single maintenance treatment. The energy and density were selected based on the VHIS evaluated at the visit. The treatment settings were:
Energy [10 mJ] and density 10% - provided to 12 subjects.
Energy [12.5 mJ] and density of 10%- provided to 3 subjects.
Subject assessment of procedure-related pain and discomfort showed low pain scores, the maximal mean score was 3.1 ± 3.2, for movement of the probe. In fact, the majority of women felt no discomfort following the procedure. Adverse events (AE) reported during the study were of mild to moderate severity and were all unrelated to the procedure. One severe event of ‘fracture in right ulnar’ was reported and classified as unrelated to the procedure.
The majority of women felt no discomfort at all, following the procedure. Those that reported any discomfort, reported alleviation within2 weeks after the procedure or less.
Change from Baseline in VHIS and VVA Symptoms
For the twenty subjects in this follow-up study, the mean VHI (± standard deviation) was significantly improved at 12 months after the third laser treatment (16.3 ± 4.5 vs. Baseline 12.4 ± 4.0; p < 0.05) (Table 2). Additionally, this score remained significantly improved at the 15- and 18-months follow up visits (16.9 ± 4.6 and 17.1 ± 4.6, respectively; p < 0.05.) (Figure 1).
Table 2: VHI Score and VVA Symptoms.
| Baseline | 12MFUb | 15MFUc | 18MFU | |
|---|---|---|---|---|
| VHIS | 12.4 ± 4.0* | 16.3 ± 4.5* | 16.9 ± 4.6* | 17.1 ± 4.6* |
| Vaginal itchinga | 1.2 ± 2.0* | 0.8 ± 1.2* | 0.6 ± 1.1* | 0.4 ± 0.6* |
| Vaginal burninga | 1.8 ± 2.6* | 0.6 ± 0.9* | 0.6 ± 0.9* | 0.4 ± 0.7* |
| Vaginal drynessa | 4.7 ± 3.1* | 2.3 ± 2.2* | 2.0 ± 2.0* | 1.5 ± 1.6* |
| Dyspareunia (Pain during intercourse)a | 5.8 ± 3.4* | 2.9 ± 2.8* | 3.0 ± 2.6* | 2.0 ± 2.4* |
| Dysuria (Pain/stinging during urination)a | 1.3 ± 2.4* | 0.6 ± 1.2* | 0.5 ± 0.8* | 0.2 ± 0.4* |
Data is presented as mean ± standard deviation.
Data is measured on a VAS scale (range 0–10).
2 subjects were treated at the 12MFU visit;
13 subjects were treated at the 15MFU visit;
Significant change from baseline (p < 0.05) according to SAS Mixed model
MFU: months of follow-up after the third laser treatment.
Fig. 1:
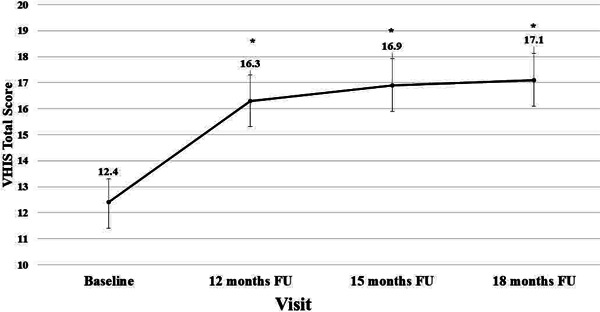
Data is presented as mean ± standard error.
*Significantly different from baseline, p < 0.05.
Figure 1: VHIS During the Long-Term Follow-Up
-Attached As a Separate File-
VHIS improvement was noted in subjects who received maintenance treatments as well as those who did not, with no significant difference between the two groups (Table 3).
Table 3: Adjusted Mean (± standard error) Change from Baseline of VHIS total by visit.
| 12MFUa | 15MFUb | 18MFU | |
|---|---|---|---|
| Treated subjects (N = 15) |
3.2 ± 0.8* | 3.4 ± 0.8* | 4.0 ± 0.8* |
| Not treated subjects (N = 5) |
5.7 ± 1.3* | 7.5 ± 1.3* | 6.5 ± 1.3* |
Significantly change from baseline (p < 0.05) according to SAS Mixed model
2 subjects were treated at this visit;
13 subjects were treated at this visit
VAS scoring of VVA symptoms by visit is presented in Table 2 and Figure 2. VVA symptoms such as vaginal burning, vaginal dryness and dyspareunia were significantly improved at the 12, 15 and 18 months follow up visits. At the 12 Months visit, significant improvements were noted in vaginal burning, vaginal dryness, dyspareunia and dysuria. Vaginal itching also improved, and this improvement was sustained at the 18 months follow-up visit.
Fig. 2:
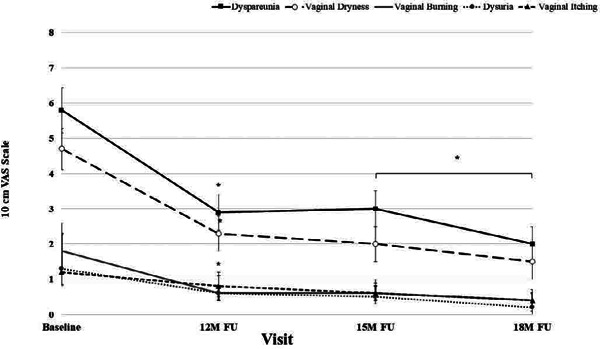
Data measured on a VAS scale (range 0–10), is presented as mean ± standard error.
*Significantly different from baseline, p <0.05.
Figure 2: VVA Symptoms
-Attached As a Separate File-
Sexual Function (FSFI) and Sexual Downtime
The effects of CO2 laser treatment on VVA symptoms was also measured with the FSFI. 15 of the 20 follow-up study subjects provided FSFI information, of which 11 had a maintenance treatment during the follow-up. The mean Baseline score of FSFI (± SD) was 16.2 ± 7.9 (Table 4). At the 12 Months visit, the total FSFI score increased significantly (24.4 ± 6.9; p < 0.05), and at the 15- and 18-month follow-up visits, the total FSFI remained significantly higher than Baseline (22.2 ± 6.7, 25.8 ± 6.6). Similarly, increases in all FSFI sub-domains from Baseline remained statistically significant during the follow-up visits excluding ‘Arousal at month 15’. However, by month 18, a significant improvement was noted in this symptom as well.
Table 4: FSFI Total and Domain Scores.
| Baseline | 12MFUa | 15MFUb | 18MFU | |
|---|---|---|---|---|
| Total Score | 16.2 ± 7.9* | 24.4 ± 6.9* | 22.2 ± 6.7* | 25.8 ± 6.6* |
| Desire | 2.7 ± 1.2* | 3.4 ± 1.0* | 3.4 ± 0.8* | 3.5 ± 1.1* |
| Arousal | 3.0 ± 1.4* | 4.2 ± 1.2* | 3.6 ± 1.6 | 4.4 ± 1.2* |
| Lubrication | 2.3 ± 1.6* | 4.2 ± 1.2* | 3.7 ± 1.4* | 4.4 ± 1.3* |
| Orgasm | 3.0 ± 2.0* | 4.4 ± 1.5* | 3.9 ± 1.7* | 4.7 ± 1.2* |
| Satisfaction | 3.2 ± 1.8* | 4.4 ± 1.3* | 4.2 ± 1.0* | 4.8 ± 1.3* |
| Pain | 2.1 ± 1.3* | 3.8 ± 1.5* | 3.3 ± 1.6* | 4.0 ± 1.6* |
Data is presented as mean ± standard deviation;
2 subjects were treated at this visit;
9 subjects were treated at this visit;
P < 0.05
At the Month 18 visit, 90% of patients (18 patients) were satisfied with the procedure, one patient was dissatisfied and the other very dissatisfied.
Discussion
As was the case for the core study, the present study was a relatively small study, with no control group. However, results were consistent across study participants lending them credibility. Selection-bias is a concern with any long-term follow-up. It may be claimed that subjects who are satisfied with their results are more inclined to volunteer to participate in study extensions. However, in this specific case, an opposing view may also by applicable, as subjects who wanted additional treatments due to un sustained satisfaction with results of the first treatment series may also be motivated to participate in the follow-up. Thus, it is unclear in what direction selection-bias affected the results, if at all.
The core study was a prospective, open-label single- arm study in 28 healthy post-menopausal women with VVA-related symptoms that were treated with 3 fractional CO2 laser treatments. In the study, a significant improvement in VHIS was detected early and sustained at 3 and 6 months following the third treatment 14). The current is a follow-up study that recruited 20 of the 28 participants of the core study and included visits at 12, 15 and 18 months following the third laser treatment of the core study. During the current study, 15 of the 20 participants received maintenance treatments. Here, a sustained statistically-significant improvement of VHIS from Baseline was observed. The patient-reported assessment of VVA symptoms showed an improvement during the core study, and this improvement was also sustained over the long-term follow-up reported here. Finally, the improvement in sexual function observed during the core study was sustained over the long-term evaluated here.
These results are in-line with the mode of action of fractional CO2 lasers, which is based on remodeling of the vaginal connective tissue without causing damage to surrounding tissue. Rather than a superficial short-term symptom-alleviation, it seems like the CO2 laser treatment leads to profound regenerative effects of the vaginal wall. A preclinical study in a porcine model 17) showed that treatment with a microablative fractional CO2 laser caused slight thermal denaturation in the vaginal mucosa without excessive hemorrhaging, vesicle formation or erythema that recovered 30 days following treatment. The energy supplied caused superficial ablation of the epithelium, contraction of collagen and neocollagenesis. By Day 30, clear regenerative effects were observed, treated areas showed an increase in collagen and elastic fibers on the lamina propria, as well as neovascularization. Over-expression of HSP70 was observed, suggested by the authors as the underlying trigger of neocollagenesis, as HSPs are known to play key roles in the coordinated expression of growth factors that supports cellular activities including cell proliferation and stimulation of cellular metabolism. A histological examination of a punch biopsy from a post-menopausal woman treated once with CO2 fractional laser, showed that the onset of structural changes in the epithelium and connective tissues of the vaginal wall was already evident immediately following treatment 18). The structural changes included, among others, vasculogenesis, formation of papillae and neocollagenesis in the connective tissues and thickening and desquamation of cells in the epithelium at the mucosal surface. These findings shed new light on the timeline of the process leading to the thicker epithelium, new vascularized papillae and connective tissue with evidence of new formation of thin collagen fibers and fibroblasts supporting renewal of the extracellular matrix, which were previously observed in women following a series of CO2 laser treatments 19–21).
The results of the current follow-up study are in-line with observations previously made with fractional CO2 laser treatments of post-menopausal women with VVA or genitourinary syndrome of menopause (GSM)-related symptoms
In accordance with previous findings 22), fractional CO2 laser therapy was found to be safe and well-tolerated in our study, with minimal AEs reported, all unrelated to laser treatment.
In conclusion, the results suggest that fractional CO2 laser treatments are safe, well-tolerated and effective in alleviating symptoms of VVA and sexual dysfunction in post-menopausal women, and that effects are sustained over the long-term. Further clinical studies that are well-controlled are needed to evaluate the long-term efficacy and safety of fractional CO2 laser treatment.
References
- 1: Heiman JR, Rupp H, Janssen E, Newhouse SK, Brauer M, Laan E. 2011. Sexual desire, sexual arousal and hormonal differences in premenopausal US and Dutch women with and without low sexual desire. Hormones and behavior. 59:772-779. [DOI] [PubMed] [Google Scholar]
- 2: Gandhi J, Chen A, Dagur G, Suh Y, Smith N, Cali B, Khan SA. 2016. Genitourinary syndrome of menopause: an overview of clinical manifestations, pathophysiology, etiology, evaluation, and management. American journal of obstetrics and gynecology. 215:704-711. [DOI] [PubMed] [Google Scholar]
- 3: Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, van Kerrebroeck P, Victor A, Wein A. 2002. The standardisation of terminology of lower urinary tract function: report from the Standardisation Sub-committee of the International Continence Society. American journal of obstetrics and gynecology. 1:116-126 [DOI] [PubMed] [Google Scholar]
- 4: Kim H-K, Kang S-Y, Chung Y-J, Kim J-H, Kim M-R. 2015. The Recent Review of the Genitourinary Syndrome of Menopause. J Menopausal Med. 21:65-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5: Nappi RE, Palacios S. 2014. Impact of vulvovaginal atrophy on sexual health and quality of life at postmenopause. Climacteric. 17:3-9. [DOI] [PubMed] [Google Scholar]
- 6: Athanasiou S, Pitsouni E, Antonopoulou S, Zacharakis D, Salvatore S, Falagas ME, Grigoriadis T. 2016. The effect of microablative fractional CO2 laser on vaginal flora of postmenopausal women. Climacteric. 19:512-518. [DOI] [PubMed] [Google Scholar]
- 7: Pieralli A, Fallani MG, Becorpi A, Bianchi C, Corioni S, Longinotti M, Tredici Z, Guaschino S. 2016. Fractional CO2 laser for vulvovaginal atrophy (VVA) dyspareunia relief in breast cancer survivors. Archives of gynecology and obstetrics. 294:841-846. [DOI] [PubMed] [Google Scholar]
- 8: Pitsouni E, Grigoriadis T, Tsiveleka A, Zacharakis D, Salvatore S, Athanasiou S. 2016. Microablative fractional CO2-laser therapy and the genitourinary syndrome of menopause: An observational study. Maturitas. 94:131-136. [DOI] [PubMed] [Google Scholar]
- 9: Gold M, Andriessen A, Bader A, Alinsod R, French ES, Guerette N, Kolodchenko Y, Krychman M, Murrmann S, Samuels J. 2018. Review and clinical experience exploring evidence, clinical efficacy, and safety regarding nonsurgical treatment of feminine rejuvenation. J Cosmet Dermatol. 17:289-297. [DOI] [PubMed] [Google Scholar]
- 10: Arunkalaivanan A, Kaur H, Onuma O. 2017. Laser therapy as a treatment modality for genitourinary syndrome of menopause: a critical appraisal of evidence. Int Urogynecol J. 28:681-685. [DOI] [PubMed] [Google Scholar]
- 11: Streicher LF. 2018. Vulvar and vaginal fractional CO2 laser treatments for genitourinary syndrome of menopause. Menopause. 25:571- 573. [DOI] [PubMed] [Google Scholar]
- 12: Behnia-Willison F, Sarraf S, Miller J, Mohamadi B, Care AS, Lam A, Willison N, Behnia L, Salvatore S. 2017. Safety and long-term efficacy of fractional CO2 laser treatment in women suffering from genitourinary syndrome of menopause. European Journal of Obstetrics and Gynecology and Reproductive Biology. 213:39-44. [DOI] [PubMed] [Google Scholar]
- 13: Samuels JB, Garcia MA. 2018. Treatment to External Labia and Vaginal Canal With CO2 Laser for Symptoms of Vulvovaginal Atrophy in Postmenopausal Women. Aesthet Surg J. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14: Eder SE. 2018. Early effect of fractional CO2 laser treatment in Post-menopausal women with vaginal atrophy. Laser Ther. 27:41-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15: Bachmann GA, Notevolitz M, Kelly SL. 1992. Long-term non-hormonal treatment of vaginal dryness. Clin Pract Sex 8:3-8 [Google Scholar]
- 16: Rosen R. 2000. The Female Sexual Function Index (FSFI): a multidimensional self-report instrument for the assessment of female sexual function. Journal of Sex & Marital Therapy. 26:191-208. [DOI] [PubMed] [Google Scholar]
- 17: Kwon T-R, Kim JH, Seok J, Kim JM, Bak D-H, Choi M-J, Mun SK, Kim CW, Ahn S, Kim BJ. 2018. Fractional CO2 laser treatment for vaginal laxity: A preclinical study. Lasers Surg Med. September;50(9):940-947 [DOI] [PubMed] [Google Scholar]
- 18: Salvatore S, França K, Lotti T, Parma M, Palmieri S, Candiani M, D'Este E, Viglio S, Cornaglia AI, Farina A, et al. 2018. Early Regenerative Modifications of Human Postmenopausal Atrophic Vaginal Mucosa Following Fractional CO2 Laser Treatment. Open Access Maced J Med Sci. 6:6-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19: Salvatore S, Nappi RE, Zerbinati N, Calligaro A, Ferrero S, Origoni M, Candiani M, Leone Roberti, Maggiore U. 2014. A 12-week treatment with fractional CO2 laser for vulvovaginal atrophy: a pilot study. Climacteric. 17:363-369. [DOI] [PubMed] [Google Scholar]
- 20: Perino A, Calligaro A, Forlani F, Tiberio C, Cucinella G, Svelato A, Saitta S, Calagna G. 2015. Vulvo-vaginal atrophy: a new treatment modality using thermo-ablative fractional CO2 laser. Maturitas. 80:296-301. [DOI] [PubMed] [Google Scholar]
- 21: Zerbinati N, Serati M, Origoni M, Candiani M, Iannitti T, Salvatore S, Marotta F, Calligaro A. 2015. Microscopic and ultrastructural modifications of postmenopausal atrophic vaginal mucosa after fractional carbon dioxide laser treatment. Lasers in medical science. 30:429-436. [DOI] [PubMed] [Google Scholar]
- 22: Pagano I, Gieri S, Nocera F, Scibilia G, Fraggetta F, Galia A, Gioè M, Pecorino B, Scollo P. 2017. Evaluation of the CO2 Laser Therapy on Vulvo-Vaginal Atrophy (VVA) in Oncological Patients: Preliminary Results. J Cancer Ther. 8:452-463. [Google Scholar]


