Abstract
Background
The aim of the study was to compare preservation of pulp vitality by indirect pulp treatment with calcium hydroxide, calcium silicate based cement (Biodentine) and Er,Cr:YSGG laser in permanent molars.
Materials and methods
30 patients were selected for this study as per the inclusion and exclusion criteria in the age group of 6–14 years and then randomly allocated to three groups A, B & C. In group A, after caries excavation, calcium hydroxide (Dycal) was placed at the floor. In group B, after caries excavation, calcium silicate based cement (Biodentine) was placed at the floor. In group C, after caries excavation, decontamination of the cavity was done with Er,Cr:YSGG laser. This was followed by placement of permanent restorative material in all the groups. Clinical and radiographic success was monitored at 3, 6 and months. Data analysis was performed using Statistical Package for the Social Science-21 (SPSS-21).
Results
At the end of 9 months, overall success rate of indirect pulp was 86.6%. There was no significant difference between the three groups. (p > 0.05)
Conclusion
The study showed that the success of indirect pulp treatment is independent of the type of liner used for pulp capping. Moreover, the study also shows that Er,Cr;YSGG laser can be effectively used for indirect pulp capping procedures.
Introduction
Dental caries is one of the most common global oral health problems in the world. Untreated caries can progress to involve pulpal tissue and lead to pain, infection and compromise quality of life. Management of deep carious and grossly decayed teeth is often challenging to the pediatric dentist. The principal objective of the management of deep carious lesion is to preserve the vitality of the teeth while causing as little trauma as possible to the pulp.This helps in providing protective resistance to masticatory forces compared with root canal filled teeth 1). In young patients, vital pulp therapy has higher success rate due to high healing capacity as compared to older patients 2). Various vital pulp therapies have been developed and used over the years including indirect pulp capping, direct pulp capping and pulpotomy procedures. Amongst these vital pulp therapy procedures, indirect pulp capping is one of the less invasive procedures and can be done easily in children and young adults. This procedure entails removal of demineralized carious tissue and a thin layer of affected dentin is left in situ in areas where further excavation may result in pulp exposure. This is followed by placement of a biocompatible material which stimulates healing of the dentin pulp complex and the tooth is then restored with an appropriate restorative material to prevent microleakage. Calcium hydroxide has been considered the “gold standard” of pulp capping materials for several decades due to excellent antibacterial properties and the ability to induce hard tissue formation 3). However it is highly soluble and subject to dissolution over time 4) and provides a poor seal 5). Another drawback associated with calcium hydroxide is the appearance of so-called “tunnel defects” in reparative dentin formed underneath calcium hydroxide pulp capings 6).
This has led to several other alternative materials being used for indirect pulp treatment. Amongst these, Mineral Trioxide Aggregate (MTA) has proven to be successful as indirect pulp capping agent. Biodentine (Septodont, USA) is relatively new calcium silicate based cement which has properties similar to that of MTA 7). Thus, Biodentine also is proposed to be effective as an indirect pulp capping agent 7).
With the advent of lasers, various procedures can be carried out with relative ease and amongst dental lasers, Er,Cr;YSGG lasers are particularly used for both hard tissue and soft tissue procedures. Er,Cr;YSGG lasers emit electromagnetic radiations in the medium infrared spectrum (2940 nm); interacting preferably with water and hydroxyl apatite, these lasers have an efficient ablation effect on both the soft tissues (gum and pulp) and the hard dental tissues and, more selectively, with the carious tissue rich in water 8). Use of Er,Cr;YSGG lasers compared with other types of lasers, has been proven to be useful in preparing cavities and removing caries, as well as in decontamination of the affected dentin 8). The necrotizing action chemically induced by the capping materials used in the conventional pulp capping procedures is replaced by the physical action of the laser.
There have been few studies on the use of calcium silicate based cement (Biodentine) and Er,Cr:YSGG laser for indirect pulp treatment. Thus this study was planned to compare the clinical performance of indirect pulp treatment using calcium hydroxide, calcium silicate based cement (Biodentine) and Er,Cr:YSGG laser.
The aim of the present study was to compare clinical and radiographic success of indirect pulp treatment or capping with calcium hydroxide, calcium silicate and Er,Cr:YSGG laser in permanent molars.
Methodology
The present study was a longitudinal experimental study carried out in Department of Pedodontics and Preventive Dentistry, Maulana Azad Institute of Dental Sciences, after obtaining prior approval from the Institutional Ethical Committee. Study population comprised of 30 children aged 6–14 years, who visited the Outpatient Department of Pedodontics and Preventive Dentistry, at Maulana Azad Institute of Dental Sciences, New Delhi. The sample size was estimated based on the previous literature findings 9) and by consulting a biostatistician as per the formula given below:
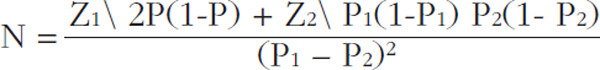 |
Z1 = 1.96 (standard normal variate for power)
Z2 = 0.84 (standard normal variate for level of significance)
 |
P1 = Proportion in cases (1.68)
P2 = Proportion in control (2.04)
The inclusion and exclusion criteria were as follows:
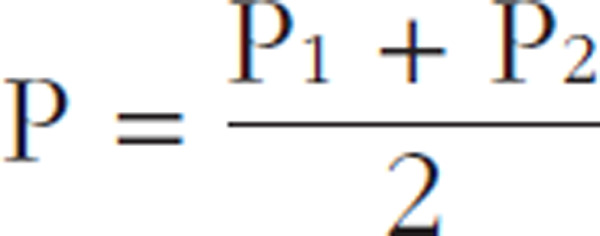
The details of the study procedure and the purpose of the study were explained to the parents and written informed consent was obtained from them. Randomization was done using a single sequence of random assignment for group allocation. These patients were then randomly allocated to three groups A, B & C as given in Figure 1.
Fig. 1:
Methodology flow chart
Inclusion criteria
Pediatric patients aged 6–14 years.
Deep carious lesion present in permanent molars with normal appearance of gingiva.
Absence of clinical signs and symptoms of pulpal exposure such as spontaneous pain, tenderness, swelling, fistula, abscess formation, abnormal tooth mobility.
Radiographically, carious lesion involving more than two-third thickness of dentin not involving pulp.
Absence of radiographic signs and symptoms of pulpal degeneration such as thickening of periodontal spaces, interradicular or periapical radiolucencies, internal or external root resorption
Positive parental informed consent
Exclusion criteria
Children with special health care needs that may not be able to cooperate.
Medically compromised children
Presence of clinical signs and symptoms of pulpal exposure such as spontaneous pain, tenderness, swelling, fistula, abscess formation, abnormal tooth mobility.
Presence of radiographic signs and symptoms of pulpal degeneration such as thickening of periodontal spaces, interradicular or periapical radiolucencies, internal or external root resorption
-
Mobility of teeth
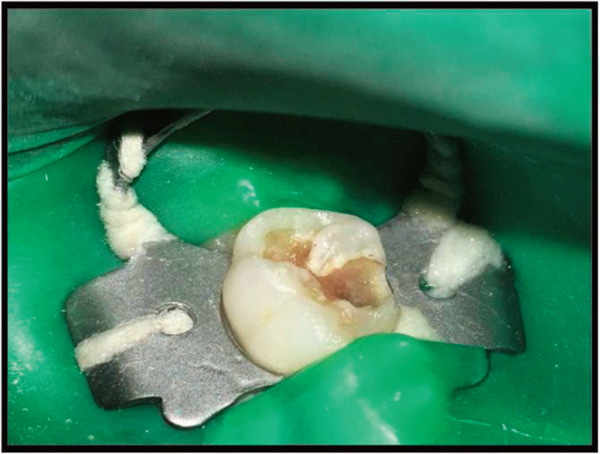
The tooth was anesthetized using local anesthesia and isolated using rubber dam. After caries removal using carbide burs (No 245; MANI, JAPAN) at low speed 10), the teeth were treated as follows:
In Group A, Calcium hydroxide-based liner (Dycal) was mixed as per the manufacturer's instructions and carried into the cavity and uniformly placed over the floor of cavity. In Group B, Biodentine was mixed according to the manufacturer's instructions and carried into the cavity and uniformly placed over the floor of cavity. In Group C, the bottom of the cavity was further radiated at 75–100 mJ (1–1.5 Watt) for 60 sec using Er, Cr: YSGG laser (Water-lase iPlus, BioLase) to ensure complete decontamination. In all the three groups, composite resin restoration (Z 100, 3M) was placed as the final restorative material as per manufacturer's instructions.
The subjects in all the three groups were evaluated immediately after the procedure, at 3 months, 6 months and 9 months using following criteria: (1) absence of spontaneous pain and/or sensitivity to pressure; (2) absence of sinus, fistula, edema, and/or abnormal mobility; (3) absence of radiolucencies at the interradicular and/or periapical regions; (4) absence of internal or external root resorption. The data was compiled and data analysis was performed using Statistical Package for the Social Science-21 (SPSS-21). The data was analyzed on the basis of categorical scores given to clinical and radiographic analysis of the three groups using chi-square (χ2) analysis and p-values < 0.05 were considered statistically significant.
Results
As shown in Table 1, at the end of 3 months, there were no signs of clinical or radiographic failure in all the three groups. At the end of 6 months, there was one failure in the Er, Cr: YSGG group with loss of vitality, presence of sponataneous pain and periapical lesion. In the Biodentine group, one subject reported with abscess and another subject exhibited signs of root resorption at the end of nine month, another subject in the Er, Cr: YSGG group presented with spontaneous pain and periapical pathology evident on radiograph while in the calcium hydroxide group, one subject presented with acute pain. The success rate amongst the groups was compared using chisquare test as shown in Table 2.
Table 1: Clinical and radiographic evaluation of Group A,B,C after 9 months.
| Group A | Group B | Group C | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| CALCIUM HYDROXIDE | BIODENTINE | Er, Cr:YSGG laser | ||||||||||
| VITALITY | CLINICAL | RADIO GRAPHIC |
VITALITY | CLINICAL | RADIO GRAPHIC |
VITALITY | CLINICAL | RADIO GRAPHIC |
||||
| PERIAPICAL LESION | PATHOLOGIC RESORPTION | PERIAPICAL LESION | PATHOLOGIC RESORPTION | PERI APICAL LESION | PATHOLOGIC RESORPTION | |||||||
| 3 months | 0/10 | 0/10 | 0/10 | 0/10 | 0/10 | 0/10 | 0/10 | 0/10 | 0/10 | 0/10 | 0/10 | 0/10 |
| 6 months | 0/10 | 0/10 | 0/10 | 0/10 | 0/10 | 0/10 | 0/10 | 0/10 | 1/10 | 1/10 | 1/10 | 0/10 |
| 9 months | 0/10 | 1/10 | 0/10 | 0/10 | 1/10 | 0/10 | 2/10 | 0/10 | 1/9 | 1/9 | 1/9 | 0/9 |
| TOTAL | 0/10 | 1/10 | 0/10 | 0/10 | 1/10 | 0/10 | 2/10 | 0/10 | 1/10 | 2/10 | 2/10 | 0/10 |
| Total failures | 1/10 | 2/10 | 2/10 | |||||||||
Table 2: Comparative evaluation after 9 months using chi square test (χ2).
| Successful cases at the end of 9 months | Failed cases at the end of 9 months | Chi square value (χ2) | p-value | |
|---|---|---|---|---|
| Group A Calcium hydroxide | 9 | 1 | 0.48 | 0.79 |
| Group B Calcium silicate based cement (Biodentine) | 8 | 2 | ||
| Group C Er,Cr;YSGG laser | 8 | 2 | ||
Chi square value (χ2) was 0.48 and the p-value at the end of 9 months was 0.79
The difference between the three groups was not statistically significant as p > 0.05.
Discussion
The main objective of the indirect pulp treatment is to maintain the vitality of teeth with reversible pulp injury. The rationale for this treatment modality is based on the observation that reduction in bacterial counts can help in utilizing the healing potential of odontoblasts which results in deposition of tertiary dentin matrix or sclerotic dentin 11). This is mediated by the activation of endogenous signaling molecules, such as TGF-βs, which are present at the dentinal matrix and are solubilized by various agents used for indirect pulp treatment.
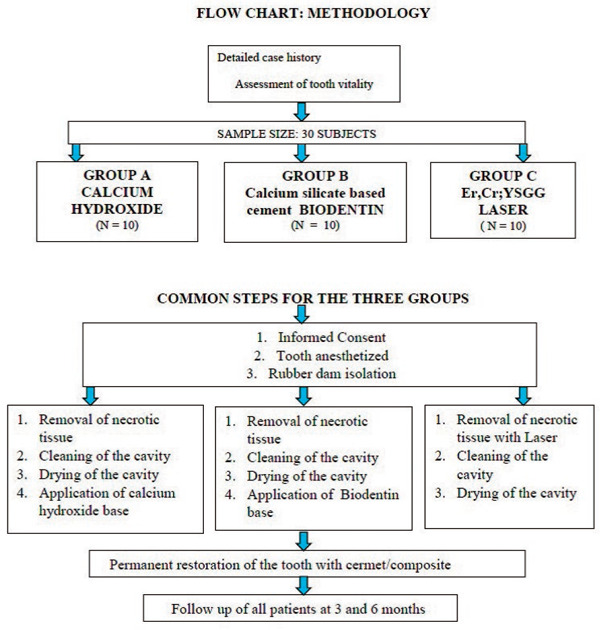
The present study was conducted to determine clinical and radiographic success of indirect pulp capping using calcium hydroxide, Biodentine and Er, Cr: YSGG laser. Adequate isolation is the most critical aspect of any restorative procedure. All the steps were performed under rubber dam isolation, as rubber dam provides the most controllable isolation. It prevents accidental swallowing or aspiration of instruments or materials 12). Rubber dam also improves access to the operative field by restraining the tongue and retracting the gingival papilla. It permits treatment to proceed in a more relaxed environment, eliminating the need for constant monitoring of isolation or frequent exchange of cotton rolls 13). A study conducted by Eidelman E (1983) concluded that retention of restorative materials were higher with rubber dam than without rubber dam 14). Another study conducted by Wang Y(2016) indicated that dental restorations had a significantly higher survival rate in cases done under rubber dam isolation compared to isolation with cotton rolls 15).
Following a pulp treatment procedure, bacterial leakage through the final restoration is considered to be more detrimental to outcome than bacterial contamination at the time of the treatment 16). This finding underlines the need for a good seal in the final restoration after the completion of the pulp treatment. Restorations with well-sealed margins are necessary for the prevention of pulp pathologies. So the cavities were sealed with permanent restorative material to avoid bacterial contamination.
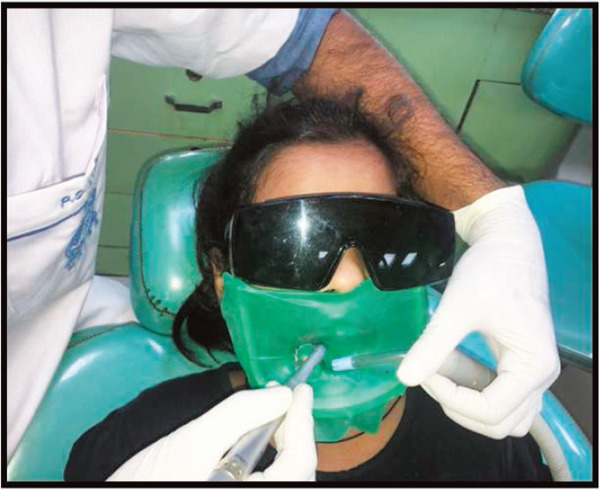
Fig. 2:
isolation of tooth using rubber dam
Fig. 3:
Decontamination using Er, Cr: YSGG laser
The follow up was conducted at 3, 6 and 9 months. In our study, the overall success of the IPC procedure was 86.66%. This result of our present study is similar to results obtained in previous studies on indirect pulp treatment. Bjørndal L, Thylstrup A (1998) 17) conducted a study on stepwise excavation of deep carious lesions and restoring them with the help of indirect pulp capping agents in permanent teeth. Ninety four teeth with deep carious lesions were chosen for the study and only five cases resulted in pulp exposure during the final excavation. After nine month follow up, the overall success of indirect pulp treatment was 85%. Another study was conducted by Falster CA et al (2001) to determine the success of indirect pulp treatment. Indirect pulp treatment with and without calcium hydroxide liner was done on 48 permanent molars and the overall success rate was 83% after 2 year follow up 18). Studies conducted by Beetke et al 19) (2000) reported a success rate of 84% at the end of 9 months when indirect pulp treatment was done in permanent molars with calcium hydroxide as the liner. Another study conducted by Nordstrom et al (1974) 20) reported a success rate of 85% when indirect pulp capping was done with calcium hydroxide in permanent molars.
Fig. 4a:
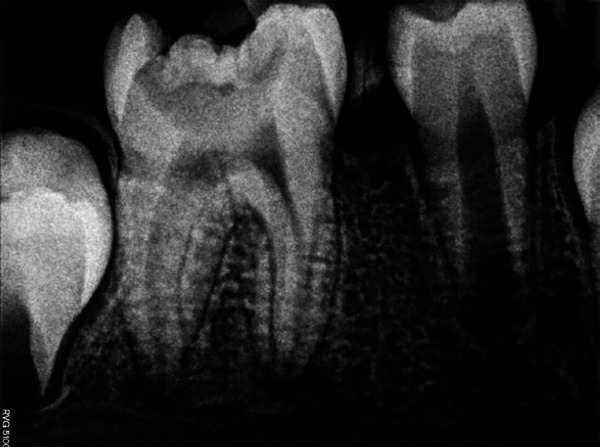
Preoperative radiograph
Fig. 4b:

Immediate post-operative radiograph
Fig. 4c:

3 month follow-up radiograph
Fig. 4d:

6 month follow-up radiograph
Fig. 4e:

9 month follow-up radiograph
The overall success rate at the end of 3 months was 100% which reduced to 96.6% at the end of 6 months and 86.6% at the end of 9 months among all the three groups. This result was also similar to a study conducted by Nirschl et al (1983) in which the success rates of indirect pulp capping were 100%, 97% and 85% after 3, 6, 9 months respectively 21). Another study conducted by Straffon LH et al (1986) conducted a study on indirect pulp treatment on permanent molars and reported a success rate of 99%, 90% and 82% at the end of 3, 6, 9 months respectively 22). The decrease in success rate after long term follow may be due to improper case selection, inadequate caries removal, poor manipulation techniques which may lead to poor strength of the restorative materials.
After 9 months, 90% success rate of indirect pulp treatment was found in calcium hydroxide group. The good clinical success rates of IPT are related to the thickness of the newly formed dentine. In a study using calcium hydroxide as indirect pulp capping agent, Stanley et al (2001) showed that dentine bridge is formed by 3 months and the thickness of dentin bridge can reach upto 0.5 mm after 6 months 23). Kerkhove et al (1967) conducted a study to determine the success of indirect pulp treatment using calcium hydroxide. Indirect pulp treatment was done on 56 permanent teeth and the success rate of indirect pulp treatment was 89%. 24) Clinical studies have effectively proved the success of calcium hydroxide compounds as IPC agents. Various studies have also described reparative dentin formation when calcium hydroxide was used for IPT 25, 26). However, in long-term clinical studies of pulp capping with calcium hydroxide-based materials, failure rates increased with follow-up time 27). In addition, an increased frequency of inflammatory cells and localized areas of pulp necrosis have also been reported 28).Similar findings were found in our study where one failure was reported in teeth treated after 9 months . This could be due to known disadvantages of gradual disintegration and tunnel defects in the newly formed dentin 29).
The success rate of indirect pulp treatment in calcium silicate based cement (Biodentine) group was 80%. This data also corroborates with the results of previous studies. Hashim et al (2015) 30) conducted a study to assess the effectiveness of calcium silicate cement (Biodentine) versus glass ionomer cement (GIC; controlgroup) as indirect pulp capping materials. Seventy-two indirect pulp treatments (36 Biodentine and 36 Fuji IX) were placed in 53 patients who had signs and symptoms of reversible pulpitis. Subjects were evaluated clinically and radiographically for the success of indirect pulp treatment and the evaluation criteria were based on AAPD guidelines. The clinical success rates for Biodentine was 83%. Another study was conducted by George V, Janardhanan S (2015) to determine the clinical and radiographic evaluation of indirect pulp treatment with MTA and calcium hydroxide in primary teeth 9). Forty primary molars were divided into two groups of 20 teeth each for MTA and Dycal and indirect pulp treatment was done. A statistically significant increase in dentin thickness with both MTA and Dycal was found in their study. The high success rate in Biodentine group may be attributed to the excellent properties of Biodentine as a dentine substitute. Biodentine can stimulate odontoblastic activity and reparative dentin formation, by induction of cell differentiation which makes it perfectly biocompatible and capable of inducing the apposition of the reactionary dentin. Comparing with MTA, the total preparation, placement, and setting approximately take 12 min which makes Biodentine more user-friendly for pulp capping procedures 31). Biodentine does not contain calcium hydroxide, but after hardening, calcium oxide is formed that reacts with tissue fluids to form calcium hydroxide. This induces fibronectin secretion by pulp cells adjacent to the necrotic layer under the capping material. The secreted layer further forms collagen fibrils which undergo reorganization forming reparative dentin tissue. Thus, Biodentine can stimulate reparative dentin formation 32). Biodentine has excellent biocompatibility, physical properties and bonding to the dental hard tissues. Calcium hydroxide ions are released from the cement during the setting phase of Biodentine results in a pH of about 12.5 that may cause the basification of the surroundings. This high pH inhibits the augmentation of micro organisms and can disinfect the dentin. Biodentine can adhere to tooth surface by micromechanical adhesion. It is also recommended that there might a possible ion exchange contributing to further adhesion of the cement giving terrific resistance to microleakage and bacterial infiltration. There were two failures in Biodentine group after 9 month follow up. This might have occurred due to poor case selection or improper manipulation of Biodentine and permanent restorative material.
In Er,Cr:YSGG group, the success rate of indirect pulp treatment was 80%. A study was conducted by Olivi G et al (2007) to verify the effectiveness of laser combined with a self-hardening calcium hydroxide base in pulp capping procedures performed on permanent teeth affected by caries 33). A total of 34 subjects were divided into three groups. Group 1 were treated with traditional rotating instruments and pulp capping with self-hardening calcium hydroxide, Group 2 were treated with Er,Cr:YSGG laser and Group 3 were treated with Erbium: YAG laser. When preparation was complete, the bottom of the cavity was further radiated at 75–100 mJ (1–1.5 Watt) for 60 sec to ensure complete decontamination. Traditional technique group showed a success of 63%; Er,Cr:YSGG laser-assisted technique showed a success rate of 80% and Erbium:YAG lasers laser-assisted technique showed a success rate of 75% (adult control group 70%). Our result was in accordance with the results of above mentioned study. The results also show that indirect pulp treatment can also be done without the placement of a liner. The purpose of liner is to act as a bactericidal agent and to provide a sterile field. Due to the decontamination property of Er,Cr:YSGG laser, the bactericidal action is achieved and thus Er,Cr:YSGG can be effectively used for indirect pulp capping procedures. Two failures were seen in this group also. This might have occurred due to poor case selection or improper manipulation of the permanent restorative material. Incomplete decontamination with laser may also result in failure of indirect pulp treatment 34).
The present study demonstrates that clinical outcome was independent of the application of type of base used. These findings suggest that, once the grossly decayed dentin is removed and good interfacial seal is provided, the healing and self-repair processes of the dentin- pulp complex are independent from the application of an inducer of mineralization such as calcium hydroxide. Moreover the decontamination effect of the laser and apparent closure of dentinal tubules due to its biostimulant effect has led to high percentage of success in laser group 35).
Our study shows that indirect pulp treatment is an effective method for management of deep carious lesion and we have obtained an overall success rate of 86.6%. There was no statistical difference between the different materials used for indirect pulp treatment (p-value > 0.5). However, our study had limited sample size with short term follow up. Studies with longer follow up and larger sample size are required to obtain ideal results.
Conclusion
In the present study, indirect pulp treatment using calcium hydroxide, calcium silicate based cement (Biodentine) and Er,Cr:YSGG laser showed high clinical and radiographic success (86.6%).
Clinically and radiographically, there was no statistically significant difference between teeth treated with calcium hydroxide, calcium silicate based cement (Biodentine), and Er,Cr:YSGG laser.
The results shows that Calcium silicate based cement (Biodentine) can be used successfully in indirect pulp treatment and no chemical liner may be required if adequate decontamination can be achieved as in case of Er,Cr:YSGG laser
Indirect pulp treatment procedures done in the present study have given successful results with different types of pulp capping agents. However, the follow up duration of the present study was 9 months with limited sample size. It is suggested that more studies with longer follow up be carried out in order to establish a standard protocol for the management of deep carious lesions with indirect pulp treatment.
References
- 1: Mathewson RJ, Primosch RE: Pulp treatment. In Fundamentals of Pediatric Dentistry, 3rd Ed. Mathewson RJ, Primosch RE; Chicago: Quintessence, 1995. 155-8. [Google Scholar]
- 2: McDonald RE, Avery DR: Treatment of deep caries, vital pulp exposure, and pulpless teeth. In McDonald RE, Avery DR. Eds. Dentistry for the child and adolescent, 6th Ed. St. Louis: CV Mosby Co, 1994. 189-92. [Google Scholar]
- 3: Coolidge ED. The treatment of deep dental caries. Ill Dent J. 1931;1:363-373. [Google Scholar]
- 4: King JB, Crawford JJ, Lindahl RI. Indirect pulp capping: A bacteriologic study of deep carious dentin in human teeth. Oral Surg Oral Med Oral Pathol. 1965;20:663-673. [DOI] [PubMed] [Google Scholar]
- 5: Dimaggio JJ, Hawes RR. Continued evaluation of direct and indirect pulp capping [abstract]. IADR. 1963. Abstract 38 [Google Scholar]
- 6: Zerosi C. Continued appraisal of the literature on deep carious lesions. Int Dent J. 1970;20:297-07 [PubMed] [Google Scholar]
- 7: Nowicka A, Lipski M, Parafiniuk M, Sporniak-Tutak K, Lichota D, Kosierkiewicz A, et al. Response of human dental pulp capped with Biodentine and mineral trioxide aggregate. J Endod 2013;39:743-7. [DOI] [PubMed] [Google Scholar]
- 8: Olivi G, Genovese MD. Erbium chromium laser in pulp capping treatment. J Oral Laser App. 2006; 6(4): 291-95. [Google Scholar]
- 9: George V, Janardhanan SK, Kumaran P, Xavier AM. Clinical and radiographic evaluation of indirect pulp treatment with MTA and calcium hydroxide. J Indian Soc Pedod Prev Dent 2015;33:104-10 [DOI] [PubMed] [Google Scholar]
- 10: Venkatesh N, Kavyashree B, Amitha HA. Comparative Assessment Of Success Rate Of Indirect Pulp Treatment With 2% Chlorhexidine Gluconate Disinfecting Solution, Calcium Hydroxide And Resin Modified Glass Ionomer Liner In Primary Teeth - A Prospective Study. IOSR Journal of Dental and Medical Sciences. 2016;15(2) 45-53 [Google Scholar]
- 11: Massler M. Therapy conducive to healing of human pulp. Oral Surg Oral Med Oral Pathol. 1972; 34:122-30. [DOI] [PubMed] [Google Scholar]
- 12: Barros de Campos PR, Maia RR, Rodrigues de Menezes L, Barbosa IF, Carneiro da Cunha A, da Silveira Pereira GD. Rubber dam isolation--key to success in diastema closure technique with direct composite resin. Int J Esthet Dent. 2015. Winter; 10(4): 564-74 [PubMed] [Google Scholar]
- 13: Karaouzas L, Kim YE, Boynton JR., Jr Rubber dam isolation in pediatric patients: a review. J Mich Dent Assoc. 2012. January;94(1):34-7 [PubMed] [Google Scholar]
- 14: Eidelman E, Fuks AB, Chosak A. The retention of fissure sealants: rubber dam or cotton rolls in private practice. J Dent for Children 1983; 259-61 [PubMed] [Google Scholar]
- 15: Wang Y, Li C, Yuan H, Wong MC, Zou J, Shi Z, Zhou X. Rubber dam isolation for restorative treatment in dental patients. J Dent for Children 2000; 45-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16: Briso ALF, Rahal V, Mestrener SR, et al. Biological response of pulps submitted to different capping materials. Braz Oral Res 2006. 20: 219-225. [DOI] [PubMed] [Google Scholar]
- 17: Bjørndal L, Thylstrup A: A practice-based study on stepwise excavation of deep carious lesions in permanent teeth: a 1-year follow-up study. Community Dent Oral Epidemiol 1998; 26: 122-8 [DOI] [PubMed] [Google Scholar]
- 18: Caline A, Falster, Araujo Fernando B., Lloyd H., Straffon, Jacques E. Nor, Indirect pulp treatment: in vivo outcomes of an adhesive resin system vs calcium hydroxide for protection of the dentin-pulp complex, Pediatr Dent 2002; 24:241-8 [PubMed] [Google Scholar]
- 19: Beetke E, Wenzel B, Lau B, Kienengräber V. Zur direkten Ü berkappung der artifiziell freigelegten Pulpa bei Caries profunda. Stomatol DDR 1990;40:246-9. [PubMed] [Google Scholar]
- 20: Nordstrom DO, Wei SH, Johnson R: Use of stannous fluoride for indirect pulp capping. JADA 1974;88:997-03. [DOI] [PubMed] [Google Scholar]
- 21: Nirschl RF, Avery DR: Evaluation of a new pulp capping agent in indirect pulp therapy. ASDC J Dent Child 1983;50:25-30. [PubMed] [Google Scholar]
- 22: Straffon LH, Corpron RL, Bruner FW, Daprai F. Twenty-fourmonth clinical trial of visible-light activated cavity liner in young permanent teeth. ASDC J Dent Child.1991;58:124-8. [PubMed] [Google Scholar]
- 23: Stanley HR, White CL, McCray L. The rate of tertiary (reparative) dentine formation in the human tooth. Oral Surg Oral Med Oral Pathol 1966;21:180-9 [DOI] [PubMed] [Google Scholar]
- 24: Kerkhove BC, Jr., Herman SC, Klein AI, McDonald RE: A clinical and television densitometric evaluation of the indirect pulp capping technique. Dent Child. 1966; 34:164-6. [PubMed] [Google Scholar]
- 25: Tran XV, Gorin C, Willig C, Baroukh B, Pellat B, Decup F, et al. Effect of a calcium-silicate based restorative cement on pulp repair. J Dent Res 2012;91:1166-71. [DOI] [PubMed] [Google Scholar]
- 26: Leye Benoist F, Gaye Ndiaye F, Kane AW, Benoist HM, Farge P. Evaluation of mineral trioxide aggregate (MTA) versus calcium hydroxide cement (Dycal) in the formation of a dentine bridge: A randomised controlled trial. Int Dent J 2012;62:33-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27: Olsson H, Petersson K, Rohlin M. Formation of a hard tissue barrier after pulp cappings in humans. A systematic review. Int Endod Journal 2006;39:429-42 [DOI] [PubMed] [Google Scholar]
- 28: Accorinte ML, Loguercio AD, Reis A, Carneiro E, Grande RH, Murata SS, et al. Response of human dental pulp capped with MTA and calcium hydroxide powder. Oper Dent 2008;33: 488-95. [DOI] [PubMed] [Google Scholar]
- 29: Smith AJ. Pulpal responses to caries and dental repair. Caries Res 2002. 36: 223-32. [DOI] [PubMed] [Google Scholar]
- 30: Hashem D, Mannocci F, Patel S, Manoharan A, Brown JE, Watson TF, Banerjee A. Clinical and radiographic assessment of the efficacy of calcium silicate indirect pulp capping: a randomized controlled clinical trial. J Dent Res. 2015. April;94(4):562-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31: Laurent P, Camps J, About I. Biodentine (TM) induces TGF-α1 release from human pulp cells and early dental pulp mineralization. Int Endod Journal 2012;45:439-48. [DOI] [PubMed] [Google Scholar]
- 32: Camilleri J. Hydration characteristics of Biodentine and Theracal used as pulp capping materials. Dent Mater 2014;30:709-15 [DOI] [PubMed] [Google Scholar]
- 33: Olivi G, Genovese MD, Maturo P, Docimo R. Pulp capping: advantages of using laser technology. Eur J Paediatr Dent. 2007. June;8(2):89-95. [PubMed] [Google Scholar]
- 34: Marques NC, Neto NL, Rodini CD, Fernandes AP, Sakai VT, Machado MA. Low-level laser therapy as an alternative for pulpotomy in human primary teeth. Lasers Med Science. 2014;22(2) 125-43 [DOI] [PubMed] [Google Scholar]
- 35: Saegusa H, Watanabe S, Anjo T, Ebihara A, Suda H. (2010) Safety of laser use under the dental microscope. Aust Endod Journal 36, 6-11. [DOI] [PubMed] [Google Scholar]


