The majority of emerging infectious diseases are zoonotic, originating from domesticated animals and wildlife.1 The Covid-19 pandemic is also a zoonosis, with current evidence suggesting that the causative agent – human severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) – is closely related to coronaviruses circulating in bats.2 It is therefore important to determine whether changes in human behaviour are increasing the risk of infectious diseases spilling over from wildlife populations into people.
One factor that affects the risk of emerging infectious diseases is mammalian biodiversity, or the number of different species of mammals, in a given area. Where there are many different mammalian species in one location there are also likely to be many different viruses circulating, leading to the suggestion that the risk of zoonosis inevitably increases in areas of high biodiversity.1 However, the link between biodiversity and the risk of emerging zoonotic disease is complex, and some argue that decreasing biodiversity can also lead to an increased risk. An example of this increased risk, known as the dilution effect,3 occurs when animals are forced into close proximity as a consequence of loss of biodiversity and habitat, resulting in viruses being more easily transmitted from one susceptible host to another.
It is widely accepted that the risk of emerging infectious diseases is greatest where human activity leads to new interactions with animals and their diseases. For example, habitat change resulting from logging and urban expansion not only decreases biodiversity but also brings people into close contact with a greater diversity of animals that might be carrying diseases with zoonotic potential. Also, the modern global economy encourages travel between large urban centres and remote regions, further increasing the risk of severe national and global disease outbreaks.
One method of identifying and managing the risk of emerging infectious diseases is to collect samples from animals to identify any diseases that they might be carrying. This is especially relevant to coronaviruses as several human and animal diseases, such as severe acute respiratory syndrome and Middle East respiratory syndrome coronaviruses in people and swine acute diarrhoea syndrome coronavirus in pigs, are closely related to coronaviruses found in horseshoe bats.
What you need to know.
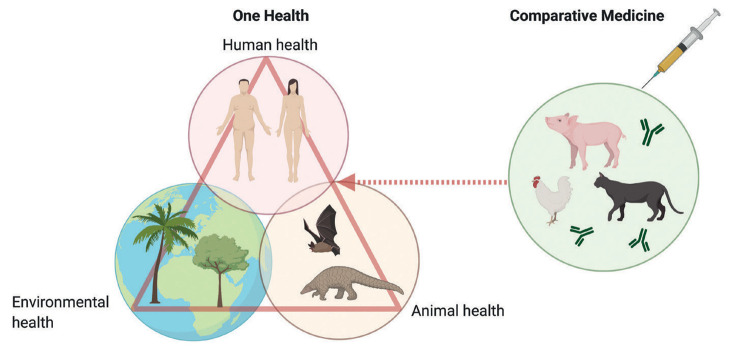
A ‘One Health’ approach identifies the intimate connections between the health of people, animals and our shared environment. The emergence of infectious diseases such as Covid-19 reminds us of the importance of identifying and understanding these connections to control and prevent disease.
Recent data have suggested that severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) likely originated in horseshoe bats, indicating that wider sampling and investigation of animal pathogens could assist the prediction of emerging infectious diseases.
However, it is equally important to adopt a comparative medicine approach, recognising and effectively using the knowledge of coronavirus biology that has accumulated for related veterinary viruses.
Research into animal coronaviruses has led to several successful veterinary vaccines and provides a better understanding of the potential challenges facing research efforts to develop safe, effective vaccines against SARS-CoV-2.
China has a rich and diverse bat population, and a robust surveillance system has been developed that allows the identification of bat coronaviruses. Surveillance studies were used recently to build a picture of how coronaviruses evolved in Chinese bat populations and identify the key bat species and geographical locations driving virus diversity in China.4 This study concluded that SARS-CoV-2 is likely to have originated in horseshoe bats in Yunnan province, China, a region close to borders with Myanmar and Laos – countries that also carry large bat populations. The study also found that the stable presence of bats and other mammals in southwestern and southern China over a long period makes these regions hot spots of coronavirus diversity, as well as areas of high risk for the emergence of bat-borne coronaviruses with zoonotic potential. This risk is further amplified as the human populations of these regions are rapidly growing and becoming increasingly urbanised, with more poultry and livestock farming bringing bats, domesticated animals and people into close proximity.
The emergence of Covid-19 illustrates the intimate connections between the health of people, animals and our shared environment and highlights the importance of a One Health approach. Comparative medicine complements a One Health approach, having an important role in the prevention and control of emerging infectious diseases such as Covid-19 by contributing to an improved understanding of coronavirus biology, the pathogenesis of coronavirus infections and the optimisation of coronavirus vaccination strategies.
A recent study indicated that SARS-CoV-2 could have emerged directly from bats. It was postulated that SARS-CoV-2 did not require significant adaptation to spread among people, which could be an example of a direct spillover of a coronavirus into people.5 The ability of the virus to readily infect people, and other mammals, might have arisen as a consequence of ancient evolutionary events as the virus evolved to infect different host bat species. It is generally accepted that wider sampling and virus discovery in locations with high coronavirus diversity will be necessary to identify viruses with zoonotic potential, which could help to prevent future outbreaks.
An additional risk factor for emerging infectious diseases is the illegal animal trade, as well as cultural traditions that lead to the consumption of wildlife. These practices can bring people into close contact with animal species that would not normally be encountered, or lead to the hunting of animals in areas of high biodiversity. Increased policing of the illegal exotic animal trade could decrease risk, as could changing the way in which wild animals are captured or hunted for meat. If farming methods for such animals can be introduced and regulated in a way that increases biosecurity (broadly, the control of infections entering or exiting a farm), then it might be possible to minimise the risk of emerging diseases while also respecting cultural traditions.
Have vaccines been developed for animal coronaviruses?
Coronaviruses infect a wide variety of mammals and birds and are commonly associated with enteric and respiratory illnesses. Effective veterinary coronavirus vaccines have been developed against several animal coronaviruses that cause economically and clinically important diseases of domestic animals such as pigs, chickens, dogs and cats. However, some of these vaccines have only short-term efficacy because of the emergence of new virus variants.
Coronaviruses are divided into four groups – alpha, beta, delta and gamma– and vaccines have been developed against coronaviruses belonging to each of these groups. Veterinary coronavirus vaccines that are commercially available in the UK include vaccines against infectious bronchitis virus infection (gammacoronavirus) in poultry, canine enteric coronavirus infection (alphacoronavirus) in dogs, porcine epidemic diarrhoea virus and transmissible gastroenteritis virus (alphacoronavirus) infection in pigs and bovine coronavirus virus (betacoronavirus) infection that causes shipping fever in young calves.
It might be significant that the majority of licensed veterinary vaccines have been developed to protect against alphacoronaviruses, whereas SARS-CoV-2 is a betacoronavirus. It will be important to establish what knowledge gained from the development of these vaccines is applicable to betacoronaviruses and to recognise that the development of a Covid-19 vaccine may present unforeseen hurdles and challenges. It is notable that many attempts have been made to develop feline coronavirus (FCoV) (alphacoronavirus) vaccines, most of which failed. Understanding why some experimental vaccines failed to protect cats from FCoV infection could have comparative value, informing the development of Covid-19 vaccines.
The challenges of developing an FCoV vaccine
Most cats infected with FCoV remain healthy or develop only mild enteritis. However, a small proportion will develop feline infectious peritonitis (FIP) – a disease with a very poor prognosis. The virulence of the virus, the viral load and the cat’s immune response are factors that determine whether FIP will develop in infected cats, although the role of antibodies in preventing cats from developing FIP is unclear.6
In experimental studies, it was found that some FCoV vaccine candidates induced antibodies that neutralised the virus while others bound to the virus and increased viral uptake. This phenomenon, known as antibody-dependent enhancement of infection,7 apparently amplified rather than prevented disease.8 Although cats that developed antibodies following vaccination were more likely than unvaccinated cats to develop FIP after being experimentally infected with the virus,9 antibody-positive cats that had been naturally exposed to the virus did not show enhanced disease.10 This difference could have been related to the higher doses of virus to which cats were exposed in experimental infections compared with natural infections. Alternatively, the difference could be related to the virus being administered experimentally by injection, whereas, in natural field infections, cats are exposed to the virus at mucosal surfaces.10
There is currently one FCoV vaccine that is available commercially in the USA and some European countries. This vaccine is administered intranasally and contains an attenuated virus that replicates efficiently at mucosal surfaces in the upper respiratory tract but cannot replicate at the higher temperatures within the lower respiratory tract. The attenuated virus stimulates an effective immune response that does not lead to antibody-dependent enhancement and avoids the risk of severe disease caused by virus replication in the lower respiratory tract. The vaccine is not recommended for use in antibody-positive cats since such cats will either have natural immunity or will already be incubating FCoV.11 However, intranasal vaccination of antibody-negative kittens has been shown to be safe and effective.11
How could a One Health approach prevent emerging infections?
There are no simple solutions for preventing emerging disease outbreaks, but it might be possible to predict the likelihood of the emergence of new infections such as SARS-CoV-2 using surveillance systems to identify viruses circulating in wild and domestic animals. Ideally, surveillance would be combined with the restoration of animal habitats, encouraging animals to forage in areas free from human interference. Community engagement and government policies could also be implemented to control human behaviours that increase the risk of human exposure to animal pathogens.
It might also be possible to mitigate the risk of emerging infections through research and the development of vaccines and other disease control strategies for wild and domestic animal populations, which ultimately would also lead to improvements in human health. This is most likely to be achieved by taking a broad approach to One Health that encompasses comparative medicine to have the greatest impact on the health of people, animals and the environment.
Acknowledgements
We thank Diane Addie and Russell Brown for useful discussions during the preparation of this article.
References
- 1.Allen T, Murray KA, Zambrana-Torrelio C, et al. Global hotspots and correlates of emerging zoonotic diseases. Nat Commun 2017; doi: 10.1038/s41467-017-00923-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhou P, Yang X, Wang X, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature 2020:579:270–3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schmidt KA, Ostfeld RS. Biodiversity and the dilution effect in disease ecology. Ecology 2001;82:609–19 [Google Scholar]
- 4.Latinne A, Hu B, Olival KJ, et al. Origin and cross-species transmission of bat coronaviruses in China. bioRxiv 2020; doi: 10.1101/2020.05.31.116061 [preprint] [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 5.MacLean OA, Lytras S, Singer JB, et al. Evidence of significant natural selection in the evolution of SARS-CoV-2 in bats, not humans. bioRxiv 2020; doi: 10.1101/2020.05.28.122366 [preprint] [DOI] [Google Scholar]
- 6.European Advisory Board on Cat Diseases. Feline infectious peritonitis. www.abcdcatsvets.org/feline-infectious-peritonitis (accessed 1 July 2020) [DOI] [PMC free article] [PubMed]
- 7.Takano T, Kawakami C, Yamada S, et al. Antibody-dependent enhancement occurs upon re-infection with the identical serotype virus in feline infectious peritonitis virus infection. J Vet Med Sci 2008;70:1315–21 [DOI] [PubMed] [Google Scholar]
- 8.Vennema H, de Groot RJ, Harbour DA, et al. Early death after feline infectious peritonitis virus challenge due to recombinant vaccinia virus immunization. J Virol 1990;64:1407–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Olsen CW. A review of feline infectious peritonitis virus: molecular biology, immunopathogenesis, clinical aspects and vaccination. Vet Microbiol 1993;36:1–37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Addie DD, Toth S, Murray GD, et al. Risk of feline infectious peritonitis in cats naturally infected with feline coronavirus. Am J Vet Res 1995;56:429–34 [PubMed] [Google Scholar]
- 11.Fehr D, Holznagel E, Bolla S, et al. Placebo-controlled evaluation of a modified life virus vaccine against feline infectious peritonitis: safety and efficacy under field conditions. Vaccine 1997;15:1101–9 [DOI] [PMC free article] [PubMed] [Google Scholar]