Abstract
Background:
No previous study has compared the outcomes of repair for partial and complete proximal hamstring ruptures at various intervals after the injury.
Purpose:
The primary aim was to determine whether time from injury to surgery affected outcomes after primary repair of partial and complete proximal hamstring ruptures. The secondary aim was to assess patients’ experiences from initial evaluation to finding a treating surgeon.
Study Design:
Cohort study; Level of evidence, 3.
Methods:
Records from 2007 to 2016 from a single surgeon’s practice were reviewed. A total of 124 proximal hamstring repair procedures in 121 patients were identified. There were 92 patients who completed questionnaires: a custom survey, the standard Lower Extremity Functional Scale (LEFS), a custom LEFS, the standard Marx activity scale, a custom Marx activity scale, and the University of California Los Angeles (UCLA) activity score. Results were analyzed for partial and complete repair procedures performed at ≤3 weeks, ≤6 weeks, and >6 weeks after the injury.
Results:
The mean follow-up was 43 months (median, 38 months). Of 93 repair procedures reviewed, 51% (9/28 partial; 38/65 complete), 79% (16/28 partial; 57/65 complete), and 22% (12/28 partial; 8/65 complete) were performed at ≤3 weeks, ≤6 weeks, and >6 weeks, respectively. At those various intervals, no statistical difference was found in standard LEFS, custom LEFS, standard Marx, custom Marx, or UCLA scores. Female sex, older age, and body mass index >30 kg/m2 were negative predictors of outcome measures. When repaired >6 weeks after the injury, a greater percentage of patients reported weakness of the operative leg compared with the contralateral side (partial tears: 6.3% vs 25%, respectively; complete tears: 24.6% vs 50%, respectively) in addition to greater sitting intolerance (partial tears: 0% vs 25%, respectively; complete tears: 7.1% vs 12.5%, respectively). Patients repaired >6 weeks after the injury visited, on average, 2.6 practitioners before an evaluation by the treating surgeon compared with 1.6 treated surgically at ≤6 weeks (P = .008).
Conclusion:
Patients with proximal hamstring repair performed in the acute and chronic settings can expect successful outcomes but may experience more subjective weakness and difficulty with prolonged sitting when the repair is performed >6 weeks after the injury. Patients faced challenges in receiving the correct diagnosis and referral to an appropriate treating surgeon, emphasizing the need for an increased awareness of the injury.
Keywords: hamstring, proximal hamstring rupture, avulsion, repair timing
Proximal hamstring avulsion injuries typically occur with forced eccentric contraction of the hamstring with hip flexion and knee extension. In a cadaveric study, Miller et al20 observed that the proximal origin of the hamstring consists of a common tendon formed by the insertion of the semitendinosus and biceps femoris with a separate insertion of the semimembranosus laterally on the ischium. Injuries to the proximal hamstring can range from a partial avulsion of the tendon’s insertion to a complete rupture of the entire tendinous unit. Although there is awareness of acute proximal hamstring avulsions among orthopaedic surgeons, it is still a commonly missed injury, as it is often misdiagnosed as a hamstring strain.11 Additionally, magnetic resonance imaging (MRI) approval may be delayed by the patient's health insurance provider if nonoperative treatment is not attempted first. A delayed diagnosis can result in a chronic injury, which can present as persistent leg pain, difficulty with walking or running, cramping, sitting intolerance, or sciatic nerve symptoms.12,24
There appears to be no consensus regarding the exact definition of an acute injury; it is frequently reported as <4 weeks§ or <6 weeks3,21,25,27 and less frequently as <8 weeks12 or 12 weeks.24,29 Prior systematic reviews have compared repair outcomes of acute versus chronic proximal hamstring avulsions, with 2 studies defining an acute injury as ≤4 weeks14,28 and 1 study as ≤8 weeks.6 These studies demonstrated conflicting results when comparing return to sports, patient satisfaction, residual pain, subjective functional outcome scores, and strength.
The classification of a “complete” proximal hamstring rupture is also not clearly defined. Multiple studies have categorized a complete tear as a rupture of all 3 hamstring tendons or an avulsion of the conjoined tendon complex.11,13,16,21,26 Other studies have specified a complete tear as an avulsion of the semitendinosus, biceps femoris, and semimembranosus.5,8,19,24,27,29 The variation in tear type classification may affect results when comparing groups of patients, particularly with delayed repair, as partial tears can achieve good results in the chronic setting.1,17,29
The purpose of this study was to assess if time from injury to surgery at various time intervals affected postoperative outcomes after primary repair of partial and complete proximal hamstring ruptures. The secondary aim of the study was to investigate the patient process from initial evaluation to surgery to streamline the treatment of these injuries. We hypothesized that delayed surgical repair of proximal hamstring ruptures would result in lower subjective patient outcomes and that tears treated in the chronic setting were evaluated by more providers before the surgical consultation with the senior author (S.L.M.).
Methods
We performed retrospective review of a single sports medicine fellowship–trained orthopaedic surgeon’s (S.L.M.) practice between January 2007 and December 2016 to identify patients treated surgically for a proximal hamstring rupture. Institutional review board approval was obtained. Patients at least 6 months from surgery with a diagnosis of a proximal hamstring rupture on MRI were included. Exclusion criteria were patients aged <18 years or >75 years. Patients were mailed an initial screening packet at study initiation with an explanation of the study goals and the option to participate. The packet included a custom hamstring questionnaire, the standard Lower Extremity Functional Scale (LEFS),4 a custom LEFS,11 the standard Marx activity scale,18 a custom Marx activity scale,11 and the University of California Los Angeles (UCLA) activity score.2 The custom questionnaire was adapted from a prior study25 and included questions regarding demographics, subjective outcomes and patient satisfaction. Patients who did not return the completed packet within 4 weeks of mailing received a follow-up call for completion over the telephone. The length of follow-up in months was determined by the date on which the completed survey was received for each patient.
Overall, 124 proximal hamstring repair procedures in 121 patients were initially included. Of the 124 repair procedures performed, 93 surveys were completed (75%) by 92 patients. A retrospective chart review was performed for patients who returned mailed questionnaires or completed the survey over the telephone. Demographic data, body mass index (BMI), imaging studies, and operative records were collected.
Tear Type
The type of tear (partial vs complete) and the amount of tear retraction were determined by a review of MRI scans by the senior author. MRI was performed at a variety of institutions; therefore, a standardized technique protocol was not followed. A complete tear involved a rupture of a common tendon of the semitendinosus, biceps femoris, and semimembranosus. A partial tear was defined as an avulsion of a common tendon with maintained insertion of some or all of the semimembranosus. The tear type was documented in the operative report.
Acute Versus Chronic Repair
The 2 acute time intervals, ≤3 weeks and ≤6 weeks, were chosen based on prior studies.∥ Groups were further categorized into partial or complete tears to distinguish if tear type influenced outcome measures in the acute and delayed settings.
Surgical Technique
The surgical technique has been previously described.20,25 Patients were in the prone position, with padding of bony prominences. A transverse incision was made at the gluteal crease with an L-shaped distal extension in cases of chronic, retracted tears or for improved exposure in patients with larger body habitus. The caudal edge of the gluteus maximus was identified and retracted proximally to visualize the hamstring sheath. The sheath was divided longitudinally and hematoma evacuated to expose the free end of the tendons. The sciatic nerve was identified in every case and protected throughout the procedure. If necessary in chronic injuries, sciatic nerve dissection was performed to visualize and free up the scarred tendon. The hamstring footprint on the ischial tuberosity was identified.
Between 1 and 4 double-loaded metal or all-suture anchors were used depending on the size of the hamstring tear and quality of the tissue. For complete tears, 3 anchors were typically used. After the proximal hamstring tissue was debrided and mobilized, 1 strand from the anterior and posterior anchors was passed through the tissue using a Krackow stitch, and the second strand from each anchor was passed in a modified Mason-Allen fashion. The third anchor sutures were passed as simple sutures. The suture from the running locking suture was used to reduce the tendon to the footprint on the tuberosity, and then, all sutures were tied. The tendon was approximated to the bony tuberosity footprint in all but 2 patients, in whom an allograft was required. For partial tears, 2 to 3 anchors were commonly used. One anchor was used infrequently in cases of poor tissue quality. In that scenario, 2 running locking sutures were utilized from the double-loaded anchor. The wound was closed in a layered fashion with absorbable suture (Dermabond; Ethicon) and covered with waterproof dressing. Bupivacaine was used at the end of the procedure for local analgesia.
All patients were placed in a locked, neutral hip orthosis to restrict hip flexion postoperatively. Patients maintained toe-touch weightbearing on crutches with the hip orthosis locked at 0° of flexion for 4 weeks. All patients were referred to physical therapy with the senior author’s rehabilitation protocol. Full weightbearing out of the brace and gentle hip and knee range of motion were initiated in the second month. Patients progressed to strengthening and nonimpact aerobic activities at 8 to 10 weeks, followed by a gradual return to physical activities. Patients generally returned to full activity without restrictions at 6 months after surgery.
Statistical Analysis
Statistical analysis was performed on the continuous and categorical variables by a biostatistician using SAS 9.4 software (SAS Institute). The Shapiro-Wilk test was used to determine the normality of continuous data. The Student t test and Wilcoxon test were used for normal and nonnormal distributions of quantitative variables, respectively. Categorical data were analyzed by the Pearson chi-square test. Additional regression analysis was performed to determine if patient variables exhibited an effect on outcome measures. These variables included age, sex, BMI, type of tear, amount of tear retraction, total number of practitioners seen before surgery, number of weeks from injury to surgery, injection or physical therapy before surgery, history of low back procedures, and duration of surgery. The threshold of significance was set at P < .05.
Results
Of the 92 patients (93 tears) who elected to participate in the study, 37 were male and 55 female (bilateral injury in 1 female), with a mean age of 50.6 years (range, 28-67 years). The mean follow-up was 43 months (median, 38 months). There were 56 right-sided tears and 37 left-sided tears. The most common mechanism of injury was a waterskiing-related accident (22/93), followed by a trip or slip during everyday activities (20/93). Injuries during other sports included running (9/93), tennis (6/93), baseball/softball (5/93), ice hockey (3/93), field hockey (2/93), skiing (2/93), and soccer (2/93). The remaining injuries were caused by trauma (5/93), an unknown event (3/93), or other physical activity/sport (14/93). Overall, there were 65 complete tears (70%) and 28 partial tears (30%). There were 2 patients with chronic tears, surgically treated at 18.6 and 36.1 weeks from the initial injury, that required allograft augmentation for repair. In 84 of the 93 cases (90.3%), the patients were satisfied with their surgery.
All Tears: Acute (≤3 Wk) vs Chronic (>3 Wk)
When an acute injury was defined as ≤3 weeks from the initial event, 47 were repaired in the acute setting, while 46 tears were considered subacute or chronic (delayed setting). There were no statistical differences in mean age or BMI at the time of surgery between the groups (Table 1). There were fewer female patients in the group that underwent delayed surgery ≤3 weeks after the initial injury compared to >3 weeks (male/female: 24/23 vs 13/33, respectively; P = .034). Additionally, fewer partial tears were repaired in the acute setting, ≤3 weeks, compared to delayed repair, >3 weeks (partial/complete: 9/38 vs 19/27, respectively; P = .025). A higher percentage of retracted tears >3 cm were treated in the acute setting, although this was not statistically significant (61.7% vs 41.3%, respectively; P = .08). Additionally, 10 of 12 severely retracted tears (>7 cm) were surgically treated in the acute setting. At follow-up, no statistical differences were found in subjective clinical outcome scores, perceived strength, functional limitations, or patient satisfaction. On average, patients who underwent delayed surgery were evaluated and/or treated by 1 additional health care provider before seeking a consultation with the senior author (1.4 vs 2.2, respectively; P < .001).
Table 1.
Outcomes for All Surgically Repaired Proximal Hamstring Rupturesa
| ≤3 Wk (n = 47) | >3 Wk (n = 46) | P | ≤6 Wk (n = 73) | >6 Wk (n = 20) | P | |
|---|---|---|---|---|---|---|
| Age at time of injury, y | 50.7 | 50.5 | .927 | 51.2 | 48.2 | .079 |
| Sex, male/female, n | 24/23 | 13/33 | .034 | 34/39 | 3/17 | .011 |
| Body mass index, kg/m2 | 25.9 | 24.7 | .126 | 25.6 | 24.2 | .049 |
| Tear type, partial/complete, n | 9/38 | 19/27 | .025 | 16/57 | 12/8 | .002 |
| VAS score for pain at time of injury | 8.4 | 8.1 | .427 | 8.2 | 8.5 | .960 |
| No. of practitioners seen before surgery | 1.4 | 2.2 | <.001 | 1.6 | 2.6 | .008 |
| Time from injury to surgery, wk | 2.0 | 41.2 | <.001 | 2.7 | 89.6 | <.001 |
| Surgical time, min | 67.8 | 68.4 | .700 | 65.5 | 77.3 | .189 |
| Follow-up, mo | 43.7 | 41.4 | .612 | 43.6 | 39.5 | .801 |
| VAS score for pain at rest | 0.6 | 0.6 | .726 | 0.6 | 0.8 | .808 |
| VAS score for pain with daily activities | 1.2 | 0.9 | .896 | 1.0 | 1.1 | .770 |
| VAS score for pain with strenuous exercise | 1.7 | 1.5 | .660 | 1.6 | 1.5 | .934 |
| Standard LEFS score | 73.3 | 74.2 | .427 | 73.9 | 73.4 | .674 |
| Custom LEFS score | 64.4 | 67.7 | .334 | 65.5 | 67.9 | .634 |
| Standard Marx score | 6.1 | 7.1 | .392 | 6.5 | 7.1 | .710 |
| Custom Marx score | 19.9 | 19.0 | .073 | 19.4 | 19.5 | .941 |
| UCLA score | 8.2 | 8.5 | .213 | 8.2 | 8.9 | .061 |
| No functional limitations, % | 53 | 67 | .231 | 60 | 60 | >.999 |
| Complete satisfaction with surgery, % | 87 | 93 | .599 | 90 | 90 | >.999 |
aData are presented as the mean unless otherwise indicated. Bolded P values indicate statistically significant differences between acute versus chronic repair. LEFS, Lower Extremity Functional Scale; UCLA, University of California, Los Angeles; VAS, visual analog scale.
Partial Tears: Acute (≤3 Wk) vs Chronic (>3 Wk)
When the 28 partial tears were independently examined, 9 were repaired ≤3 weeks from the injury, while 19 were repaired >3 weeks from the injury. There were no differences in age, BMI, sex, or tendon retraction between the acute and delayed groups (Table 2). The mean operative time for acute repair ≤3 weeks was significant longer compared to delayed repair >3 weeks (78.9 vs 59.3 minutes, respectively; P = .022). There were no statistical differences in subjective clinical outcome scores, perceived strength, functional limitations, patient satisfaction, or number of practitioners seen before surgery between the 2 groups. None of the 9 (0%) patients in the acute repair group reported sitting intolerance on the standard LEFS, compared with 3 of 19 (15.8%) in the delayed repair group.
Table 2.
Outcomes for Surgically Repaired Partial Proximal Hamstring Rupturesa
| ≤3 Wk (n = 9) | >3 Wk (n = 19) | P | ≤6 Wk (n = 16) | >6 Wk (n = 12) | P | |
|---|---|---|---|---|---|---|
| Age at time of injury, y | 46.6 | 48.3 | .700 | 48.9 | 46.2 | .406 |
| Sex, male/female, n | 4/5 | 16/3 | .068 | 8/8 | 0/12 | .008 |
| Body mass index, kg/m2 | 24.9 | 22.2 | .268 | 24.0 | 21.9 | .109 |
| VAS score for pain at time of injury | 8.9 | 7.6 | .127 | 8.1 | 7.8 | .453 |
| No. of practitioners seen before surgery | 1.2 | 2.4 | .234 | 1.5 | 2.8 | .034 |
| Time from injury to surgery, wk | 1.7 | 86.6 | <.001 | 2.6 | 134.9 | <.001 |
| Surgical time, min | 78.9 | 59.3 | .022 | 68.3 | 62.1 | .501 |
| Follow-up, mo | 44.3 | 34.7 | .507 | 36.7 | 39.2 | .403 |
| VAS score for pain at rest | 0.0 | 0.2 | .144 | 0.1 | 0.3 | .168 |
| VAS score for pain with daily activities | 0.6 | 0.6 | .891 | 0.5 | 0.8 | .586 |
| VAS score for pain with strenuous exercise | 1.0 | 1.2 | .437 | 1.0 | 1.3 | .261 |
| Standard LEFS score | 76.4 | 76.3 | .980 | 76.5 | 76.1 | .507 |
| Custom LEFS score | 64.8 | 71.7 | .378 | 66.8 | 73.0 | .419 |
| Standard Marx score | 6.6 | 7.7 | .639 | 6.1 | 9.1 | .107 |
| Custom Marx score | 20.0 | 19.0 | .491 | 18.8 | 20.0 | .750 |
| UCLA score | 8.1 | 9.0 | .111 | 8.1 | 9.4 | .014 |
| No functional limitations, % | 67 | 79 | .414 | 81 | 67 | .354 |
| Complete satisfaction with surgery, % | 100 | 95 | >.999 | 100 | 92 | .429 |
aData are presented as the mean unless otherwise indicated. Bolded P values indicate statistically significant differences between acute versus chronic repair. LEFS, Lower Extremity Functional Scale; UCLA, University of California, Los Angeles; VAS, visual analog scale.
Complete Tears: Acute (≤3 Wk) vs Chronic (>3 Wk)
Of the 65 complete tears, 38 were surgically repaired in the acute setting and 27 had delayed repair. There were no statistical differences in age, BMI, sex, or tendon retraction (Table 3). When comparing outcome measures, the mean custom Marx score was significantly higher with acute repair of complete tears (19.9 vs 19.0, respectively; P = .041). No statistical differences were found in the other subjective clinical outcome scores, perceived strength, functional limitations, or patient satisfaction with surgery. Sitting intolerance was reported in 4 of 37 (10.8%) patients in the acute repair group and 1 of 27 (3.7%) in the delayed repair group. Although the mean duration of surgery was shorter in the acute repair group compared to the delayed repair group, it was not statistically significant (65.0 vs 74.7 minutes, respectively; P = .266). In comparison to tears repaired ≤3 weeks following injury, patients with complete tears surgically repaired >3 weeks after the initial injury saw, on average, more health care providers before the evaluation by the treating surgeon (1.4 vs 2.1, respectively; P = .018).
Table 3.
Outcomes for Surgically Repaired Complete Proximal Hamstring Rupturesa
| ≤3 Wk (n = 38) | >3 Wk (n = 27) | P | ≤6 Wk (n = 57) | >6 Wk (n = 8) | P | |
|---|---|---|---|---|---|---|
| Age at time of injury, y | 51.6 | 52.0 | .834 | 51.9 | 51.2 | .787 |
| Sex, male/female, n | 19/19 | 10/17 | .324 | 26/31 | 3/5 | .723 |
| Body mass index, kg/m2 | 26.1 | 26.6 | .849 | 26.1 | 27.8 | .784 |
| VAS score for pain at time of injury | 8.2 | 8.5 | .640 | 8.2 | 9.6 | .117 |
| No. of practitioners seen before surgery | 1.4 | 2.1 | .018 | 1.6 | 2.3 | .360 |
| Time from injury to surgery, wk | 2.0 | 9.3 | <.001 | 2.7 | 21.6 | <.001 |
| Surgical time, min | 65.0 | 74.7 | .266 | 64.7 | 100.0 | .004 |
| Follow-up, mo | 43.5 | 46.2 | .968 | 45.6 | 39.9 | .632 |
| VAS score for pain at rest | 0.8 | 0.8 | .715 | 0.7 | 1.5 | .601 |
| VAS score for pain with daily activities | 1.3 | 1.2 | .994 | 1.2 | 1.6 | .670 |
| VAS score for pain with strenuous exercise | 1.9 | 1.6 | .526 | 1.8 | 1.6 | .737 |
| Standard LEFS score | 72.5 | 72.7 | .515 | 73.1 | 69.4 | .627 |
| Custom LEFS score | 64.2 | 64.8 | .875 | 65.1 | 60.1 | .404 |
| Standard Marx score | 6.0 | 6.6 | .676 | 6.6 | 4.0 | .176 |
| Custom Marx score | 19.9 | 19.0 | .041 | 19.6 | 18.8 | .216 |
| UCLA score | 8.2 | 8.2 | .800 | 8.2 | 8.0 | .959 |
| No functional limitations, % | 50 | 59 | .711 | 54 | 50 | .611 |
| Complete satisfaction with surgery, % | 84 | 93 | .818 | 88 | 87 | >.999 |
aData are presented as the mean unless otherwise indicated. Bolded P values indicate statistically significant differences between acute versus chronic repair. LEFS, Lower Extremity Functional Scale; UCLA, University of California, Los Angeles; VAS, visual analog scale.
All Tears: Acute (≤6 Wk) vs Chronic (>6 Wk)
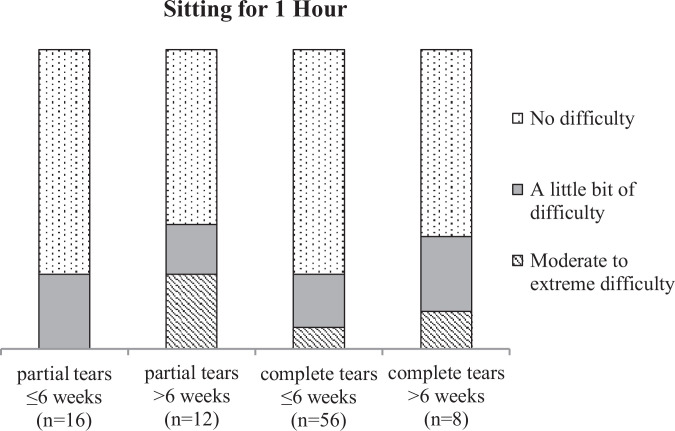
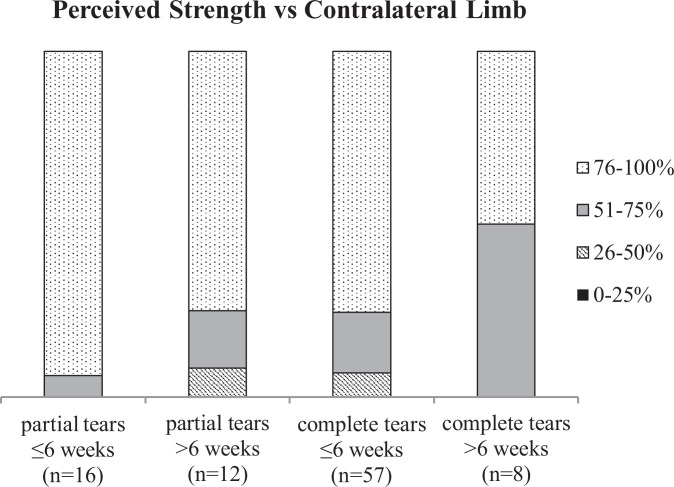
When the definition of an acute tear was changed to ≤6 weeks, 73 tears were treated acutely compared with 20 in the delayed setting. There was no difference in mean age between the groups (P = .079) (Table 1). The acute repair group, in comparison to the delayed repair group, had a significantly larger ratio of male patients (male/female: 34/39 vs 3/17, respectively; P = .011), higher BMI (25.6 vs 24.2 kg/m2, respectively; P = .049), lower percentage of partial tears (partial/complete: 16/57 vs 12/8, respective; P = .002), and saw approximately 1 fewer medial provider before receiving surgical treatment (1.6 vs 2.6, respectively; P = .008). There was a significant difference in the amount of tendon retraction between the 2 groups: the acute repair group had a higher percentage of retracted tears (>3 cm) compared with the delayed repair group (56.2% vs 35.0%, respectively; P = .042). Furthermore, 11 of 12 severely retracted tears (>7 cm) were surgically treated in the acute setting. The mean operative time was shorter in the acute repair group, but it was not statistically significant (65.5 vs 77.3 minutes, respectively; P = .189). No statistical differences were found in subjective clinical outcome scores, functional limitations, or patient satisfaction after surgery. Additionally, 4 of 72 (6%) patients treated in the acute setting and 4 of 20 (20%) treated in the delayed setting reported moderate to extreme difficulty with sitting for longer than 1 hour. Near or full strength of the surgical leg compared with the contralateral leg was subjectively noted in 58 of 73 (79.5%) patients in the acute repair group and 13 of 20 (65%) in the delayed repair group (P = .275).
Partial Tears: Acute (≤6 Wk) vs Chronic (>6 Wk)
Overall, 16 partial tears were categorized as acute and 12 were categorized as chronic. There was no statistical difference in age, BMI, or tendon retraction (Table 2). There was a higher ratio of male patients in the acute repair group compared to the delayed repair group (male/female: 8/8 vs 0/12, respectively; P = .008). Compared to partial tears that underwent repair ≤6 weeks after initial injury, those repaired in the delayed setting saw, on average, 1 more medical professional before undergoing surgery (1.5 vs 2.8, respectively; P = .034). Patients with partial tears treated ≤6 weeks from the injury had a lower mean UCLA score (8.1 vs 9.4 respectively; P = .014). No statistical differences were found in the other subjective clinical outcome scores, operative time, functional limitations, or patient satisfaction after surgery. Moreover, 0 of 16 (0%) patients reported moderate to severe sitting intolerance with acute repair, versus 3 of 12 patients (25%) with delayed repair (Figure 1). Furthermore, 15 of 16 (93.8%) patients who underwent acute repair and 9 of 12 (75%) in the chronic setting reported near or full strength in the operative versus the contralateral limb (P = .285) (Figure 2).
Figure 1.
Patient-reported difficulty with sitting for 1 hour after repair of proximal hamstring ruptures.
Figure 2.
Subjective percentage of strength in operative compared with contralateral limb.
Complete Tears: Acute (≤6 Wk) vs Chronic (>6 Wk)
Of the 65 complete tears, 57 underwent acute repair and 8 underwent delayed repair. There were no statistical differences in age, BMI, sex, or tendon retraction (Table 3). Additionally, no statistical differences were found when comparing subjective clinical outcome scores, functional limitations, or patient satisfaction. Moderate to extreme difficulty with sitting for longer than 1 hour was reported in 4 (7.1%) patients treated in the acute setting and 1 (12.5%) patient treated in the chronic setting (Figure 1). Although not statistically significant (P = .202), 43 of 57 (75.4%) patients in the acute group and 4 of 8 (50%) patients in the chronic group felt that their surgical limb demonstrated near or full strength compared with the contralateral limb (Figure 2). Surgical time was significantly shorter in complete tears undergoing acute repair (64.7 vs 100.0 minutes, respectively; P = .004). Patients with complete tears in the delayed repair group saw fewer health care providers before surgery, but it was not found to be statistically significant (1.6 vs 2.3, respectively; P = .360).
Partial Versus Complete Tears
Compared with complete tears, patients with partial tears were significantly younger (47.7 vs 51.8 years, respectively; P = .049) and had a lower BMI (23.1 vs 26.3 kg/m2, respectively P < .001) (Table 4). A higher percentage of partial tears had little to no tendon retraction compared with complete tears (P = .002). The mean time from injury to surgery was significantly longer in partial tears compared with complete tears (59.3 vs 5.0 weeks, respectively; P = .019). Although patients with partial tears generally scored higher on outcome measures than those with complete tears after surgical repair, only leg pain at rest was statistically significant (0.1 vs 0.8, respectively; P = .035). No significant differences were found in the remaining subjective clinical outcome scores, number of practitioners seen before surgery, or operative time. Additionally, 3 of 28 (10.7%) patients with surgically repaired partial tears and 5 of 64 (7.8%) with complete tears reported moderate to extreme difficulty with sitting for longer than 1 hour. Near or full strength of the surgical leg compared with the contralateral side was subjectively noted in 24 of 28 (85.7%) patients in the partial tear group and 47 of 65 (72.3%) in the complete tear group (P = .163). Patients with partial tears had a higher rate of satisfaction after surgery, with 96.4% satisfied compared with 87.7% of patients with complete tears, although it was not statistically significant (P = .600). A significantly higher percentage of patients with complete tears noted subjective functional limitations on the custom questionnaire (P = .044).
Table 4.
Outcomes for Surgically Repaired Partial and Complete Proximal Hamstring Rupturesa
| Partial (n = 28) | Complete (n = 65) | P | |
|---|---|---|---|
| Age at time of injury, y | 47.7 | 51.8 | .049 |
| Sex, male/female, n | 8/20 | 29/36 | .172 |
| Body mass index, kg/m2 | 23.1 | 26.3 | <.001 |
| VAS score for pain at time of injury | 8.0 | 8.4 | .059 |
| No. of practitioners seen before surgery | 2.0 | 1.7 | .138 |
| Time from injury to surgery, wk | 59.3 | 5.0 | .019 |
| Surgical time, min | 65.6 | 69.2 | .547 |
| VAS score for pain at rest | 0.1 | 0.8 | .035 |
| VAS score for pain with daily activities | 0.6 | 1.2 | .369 |
| VAS score for pain with strenuous exercise | 1.1 | 1.8 | .399 |
| Standard LEFS score | 76.3 | 72.6 | .546 |
| Custom LEFS score | 69.5 | 64.5 | .146 |
| Standard Marx score | 7.4 | 6.3 | .336 |
| Custom Marx score | 19.3 | 19.5 | .211 |
| UCLA score | 8.7 | 8.2 | .221 |
| No functional limitations, % | 75 | 54 | .044 |
| Complete satisfaction with surgery, % | 96 | 88 | .600 |
aData are presented as the mean unless otherwise indicated. Bolded P values indicate statistically significant differences between groups. LEFS, Lower Extremity Functional Scale; UCLA, University of California, Los Angeles; VAS, visual analog scale.
Outcome Measures
Patient variables including age, sex, BMI, tear type, and time to surgery were used in regression models to evaluate the effect on outcome measures. Other variables from chart data and the custom questionnaire were excluded from the models, as they were not found to strongly influence outcomes. Regression models for outcome measures including the custom Marx activity scale, leg pain at rest, leg pain with daily activities, leg pain with strenuous activities, perceived leg strength, and satisfaction with surgery were not included, as the data were not evenly distributed and a correlation could not be performed. Female sex was a negative predictor of standard LEFS (β = –4.12 [95% CI, –8.19 to –0.04]; R 2 = 0.14), custom LEFS (β = –7.25 [95% CI, –14.08 to –0.41]; R 2 = 0.17), standard Marx (adjusted odds ratio [aOR], 4.64 [95% CI, 1.40 to 15.33]), and UCLA (β = –1.29 [95% CI, –2.03 to –0.56]; R 2 = 0.29) scores. Increasing age was also a negative predictor of custom LEFS (β = –2.40 [95% CI, –4.25 to –0.54]; R 2 = 0.17), standard Marx (aOR, 1.39 [95% CI, 1.01 to 1.90]), and UCLA (β = –0.30 [95% CI, –0.50 to –0.10]; R 2 = 0.29) scores. Elevated BMI was associated with lower standard LEFS (β = –6.09 [95% CI, –11.72 to –0.46]; R 2 = 0.14), custom LEFS (β = –12.05 [95% CI, –21.49 to –2.60]; R 2 = 0.17), standard Marx (aOR, 2.42 [95% CI, 1.26 to 4.64]), and UCLA (β = –2.18 [95% CI, –3.19 to –1.17]; R 2 = 0.29) scores. Tear type (complete vs partial) did not have a significant effect on standard LEFS, custom LEFS, standard Marx, or UCLA scores. Delaying surgery for ≥3 weeks was associated with a higher standard Marx score (aOR, 0.30 [95% CI, 0.10-0.85]). Timing of surgery did not have an effect on standard LEFS, custom LEFS, or UCLA scores in the regression models.
Number and Type of Practitioners
A total of 56 of 93 (60%) proximal hamstring tears in the study were initially evaluated by an emergency room, urgent care, or primary care provider (Table 5). The majority of partial tears (36%) in both the ≤6-week acute and >6-week chronic settings were initially evaluated by a primary care provider. Complete tears were typically first evaluated by an emergency room provider (42%). An initial evaluation by a nonoperative sports practitioner or other orthopaedic surgeon occurred in 29 of 93 (31%) patients. This percentage was higher among all tears treated chronically. Additionally, 7 of the 93 (8%) patients were initially evaluated by the senior author. Of these 7 patients, 6 were acutely treated (3 partial; 3 complete), and 1 partial tear was repaired >6 weeks after the initial injury. Compared to patients treated in the acute setting, patients with tears treated >6 weeks from the initial injury, saw significantly more practitioners before an evaluation by the treating surgeon (1.6 vs 2.6, respectively; P = .008). This trend persisted when chronic tears were subcategorized into partial and complete tears, although it was not statistically significant among complete tears (partial: 1.5 vs 2.8, respectively [P = .034]; complete: 1.6 vs 2.3, respectively [P = .36]).
Table 5.
Time to Evaluation and Type of Medical Providers Seena
|
|
Total (N = 93) | All Tears | Partial Tears | Complete Tears | |||
|---|---|---|---|---|---|---|---|
| ≤6 Wk (n = 73) | >6 Wk (n = 20) | ≤6 Wk (n = 16) | >6 Wk (n = 12) | ≤6 Wk (n = 57) | >6 Wk (n = 8) | ||
| Time from injury to seeing medical professional, d | 1.8 | 1.4 | 3.4 | 1.4 | 4.1 | 1.4 | 2.4 |
| Initial practitioner seen, n (%) | |||||||
| Emergency room | 31 (33) | 26 (36) | 5 (25) | 3 (19) | 1 (8) | 23 (40) | 4 (50) |
| Urgent care | 6 (7) | 5 (7) | 1 (5) | 1 (6) | 1 (8) | 4 (7) | 0 (0) |
| Primary care | 19 (20) | 15 (21) | 4 (20) | 7 (44) | 3 (25) | 8 (14) | 1 (13) |
| Nonoperative sports | 9 (10) | 5 (7) | 4 (20) | 0 (0) | 3 (25) | 5 (9) | 1 (13) |
| Other orthopaedic surgeon | 20 (22) | 15 (21) | 5 (25) | 2 (13) | 3 (25) | 13 (23) | 2 (25) |
| Senior author (S.L.M.) | 7 (8) | 6 (8) | 1 (5) | 3 (19) | 1 (8) | 3 (5) | 0 (0) |
| Unknown | 1 (1) | 1 (1) | 0 (0) | 0 (0) | 0 (0) | 1 (2) | 0 (0) |
| No. of practitioners seen before surgery | 1.8 | 1.6 | 2.5 | 1.5 | 2.7 | 1.6 | 2.2 |
| Time from injury to evaluation by senior author, wk | 19.5 | 2.0 | 83.3 | 1.8 | 126.0 | 2.0 | 19.3 |
aData are presented as the mean unless otherwise indicated.
Discussion
To our knowledge, this is the first study to compare acute and chronic proximal hamstring repair at various time intervals for both partial and complete tears. When all proximal hamstring tears were analyzed, no significant differences were observed across all outcome measures between tears repaired acutely ≤3 weeks and ≤6 weeks from the initial injury compared with chronic injuries repaired >3 weeks and >6 weeks from the injury. Additionally, patient satisfaction was high across all tear groups repaired in both the acute and delayed settings. Cohen et al11 reported similar findings when comparing surgical repair ≤4 weeks and >4 weeks from the initial injury in patients with a mixture of complete and partial proximal hamstring ruptures. The authors, however, did note that patients who underwent acute repair had a significantly higher custom Marx score (20.0 vs 18.7, respectively; P = .001). When our study population was separated into partial and complete tear groups, patients with complete tears repaired ≤3 weeks from the injury also had a significantly higher mean custom Marx score (19.9 vs 19.0, respectively; P = .041). Although this trend was also observed with complete tears repaired ≤6 weeks from the injury, it was not statistically significant (19.6 vs 18.8, respectively; P = .216). It is important to note that the custom Marx activity scale was created by Cohen et al11 and is not a validated outcome measure. We are unable to determine if the statistically significant higher custom Marx score in complete tears repaired ≤3 weeks is clinically significant.
In general, patients with partial tears had better outcome scores compared with those with complete tears, although this was not statistically significant, with the exception of leg pain at rest (P = .035) and functional limitations (P = .044). Barnett et al3 found that patients with partial hamstring injuries had significantly greater preoperative hamstring strength and postoperative quadriceps strength compared with those with complete ruptures. Despite these objective differences, they found that patients with complete tears reported significantly higher scores on a subjective assessment. In our study, a higher percentage of patients with partial tears reported near or full strength after surgical repair compared with patients with complete tears, although it was not statistically significant. Additionally, partial tears were repaired after a mean of 59.3 weeks from the initial injury compared with 5.0 weeks for complete repair (P = .019).
Surprisingly, when comparing partial repair performed ≤6 weeks with that performed >6 weeks after the initial injury, patients who underwent delayed repair had a significantly higher mean UCLA score (P = .014). This was a general trend among the chronically repaired partial tears across various outcome measures, although the results were not statistically significant. This may be the result of surgeon selection bias. When looking at the amount of tendon retraction associated with the tear at the time of MRI, there was a noticeable difference between those treated at ≤6 weeks compared with those repaired at >6 weeks, with a significantly higher percentage of severely retracted tears (>7 cm) treated in the acute setting (P = .042). A similar trend existed within the ≤3-week and >3-week treatment groups, although it was not statistically significant (P = .08). This bias is likely based on prior recommendations that proximal hamstring ruptures with retraction >2 cm should be treated in the acute setting.10,11,29 Wood et al29 noted that surgical repair of retracted tears >6 weeks from the injury may result in increased difficulty in reattaching the tendon to the ischium in addition to tethering of the tendon edge to adjacent tissue and the sciatic nerve. Compared to patients treated ≤6 weeks, complete tears repaired >6 weeks from the injury resulted in a significantly longer operative time (64.7 vs 100 minutes, respectively; P = .004).
When subdividing the partial tears into acute and chronic time intervals, those surgically repaired ≤3 weeks from the injury had a significantly longer surgical time compared with those repaired at >3 weeks (78.9 vs 59.3, respectively; P = .022). This trend was not observed when comparing partial tears treated at ≤6 weeks versus >6 weeks. This finding may be owing to a number of factors including the amount of retraction, patient body habitus, soft tissue edema, and local hemorrhage. Moreover, 17 of 28 (60.7%) partial tears had retraction ≤3 cm on MRI. Of the 11 partial tears that demonstrated retraction >3 cm, 9 of 11 (81.8%) were treated ≤6 weeks of the injury. These findings suggest that physician bias may exist in surgical timing for both partial and complete tears with a large amount of tendon retraction. A minimally retracted tear is considered technically easier to repair compared with a retracted tear, even if performed in the chronic setting. The amount of tendon retraction is an important consideration when counseling patients regarding the timing of surgical treatment.
No statistical differences were found in outcome measures comparing complete tears repaired acutely ≤6 weeks from the injury versus chronic repair at >6 weeks. This is similar to a recent systematic review that found no statistical difference in standard LEFS and Marx scores when comparing acute tears treated at <2 months versus delayed repair.6 Overall, those authors reported no to minimal difference in outcomes between acute and chronic repair in terms of return to sports, patient satisfaction, hamstring strength, or pain, although they noted that a significantly higher percentage of patients in the chronic repair group reported sitting pain. This is similar to our study, in which 7.1% of patients treated ≤6 weeks from the injury and 12.5% treated at >6 weeks reported moderate to severe sitting intolerance after 1 hour. Prior studies have also observed pain with prolonged sitting for both partial and complete tears with varying chronicity treated surgically.3,5,7,9,11 Bodendorfer et al6 reported that patients who underwent acute repair performed better on strength testing. Although objective strength testing was not performed in our study, a higher percentage of patients with acutely repaired complete tears reported near to full strength of their operative leg compared with the contralateral side, although this was not statistically significant.
Of the 8 complete tears treated >6 weeks from the injury, 2 cases required allograft augmentation. These tears were repaired at 18.6 and 36.1 weeks, after the initial injury. Patients with allograft repair were included in the analysis because a prior study by Folsom and Larson13 reported high patient satisfaction and return-to-sports rates, which were comparable with acute repair. Both patients in our study were satisfied with the surgery, although the patient who underwent repair at 36.1 weeks was not able to return to the same level of sports. Additionally, it is important to be aware of and discuss the possibility of allograft augmentation in complete tears surgically repaired >6 weeks after the injury. In all complete, retracted tears treated in the chronic setting, the senior author was prepared to perform allograft augmentation if primary repair was not possible.
Few studies have examined the number of medical providers seen by patients with a proximal hamstring rupture.11,29 Cohen et al11 found that 37% of patients were misdiagnosed or treated unsuccessfully by more than 1 practitioner before an evaluation by the senior author. The authors noted that the majority of these patients were initially diagnosed with a hamstring strain without an MRI scan, as a proximal hamstring avulsion was not considered part of the differential diagnosis. Wood et al29 found that all patients with a chronic proximal hamstring rupture in their study had seen at least 1 medical provider who originally misdiagnosed the injury or underestimated the clinical importance of a proximal avulsion.
Our findings also highlight the importance of this issue, as patients with chronic tears saw roughly 1 additional health practitioner before a surgical consultation with the senior author, which occurred, on average, 83.3 weeks after the initial injury. The most surprising finding was that a higher percentage of tears treated chronically were initially evaluated by a nonoperative sports practitioner or other orthopaedic surgeon. This may not have clinical importance among partial tears unless significant retraction is present. Complete tears with retraction, however, become technically more challenging when treated in the chronic setting. As previously mentioned, compared to acute repair, complete hamstring avulsions treated >6 weeks from initial injury required, on average, longer operative time (64.7 vs 100.0 minutes, respectively; P −[c/u] .004) This is important because there are risks related to prolonged time under anesthesia in addition to the added cost per minute in the operating room. These findings emphasize the need for improved education regarding proximal hamstring injuries within the medical community and early referral to a treating surgeon. This applies to emergency room, urgent care, and primary care practitioners in the acute setting in addition to nonoperative sports providers and orthopaedic surgeons, who are often responsible for confirming the diagnosis and dictating treatment.
There are several weaknesses in this study, including the retrospective design and absence of objective functional assessments. The use of postoperative questionnaires in long-term follow-up may have introduced recall bias. Because of the retrospective nature of the study, we did not have preoperative subjective measures or a nonoperative control group for comparison. Additionally, our study did not include objective measures at presentation or at follow-up. Future research is needed to determine if timing of surgery has an effect on range of motion, strength, endurance, and flexibility. Another limitation of our study is the small sample size and lack of sex heterogeneity among partial tears, with more female patients in the chronic repair group. The amount of tear retraction may have been a confounding variable, as surgeon bias may have led to more acute repair procedures of both partial and complete tears with a large amount of retraction on MRI. The tendency to treat retracted tears in the acute setting may have diminished the effect of timing on subjective outcomes. Additionally, 2 patients with a complete, chronic proximal hamstring rupture required allograft augmentation for repair. These procedures were technically more involved with decompression of the sciatic nerve, which resulted in an increased duration of surgery and may have affected clinical results within the sample group.
A major strength of our study is the overall large sample size of proximal hamstring tears. Additionally, the mean follow-up was 43 months, with a median of 38 months. This was similar among the various groups, which allowed for a more accurate comparison of outcomes given the distribution of patients in the later stages of rehabilitation or returning to physical activities. The follow-up was longer than 12 months for 83 patients. Furthermore, all surgical procedures were performed by the senior author using the same operative technique and rehabilitation protocol. Also, the 75% response rate is considered relatively high for participation in a telephone/mail survey. Overall, the greatest strength of the study is that we subcategorized proximal hamstring avulsions by tear type and time from injury to surgery to allow for a more comprehensive comparison between groups and potentially reduce the effect of bias.
Conclusion
This study demonstrates that partial and complete proximal hamstring ruptures performed in both the acute and the chronic settings can achieve successful outcomes overall. Tears treated chronically (>6 weeks) may experience less subjective strength in the operative limb compared with the contralateral limb and pain with prolonged sitting. Our findings highlight the importance of increased awareness of proximal hamstring ruptures for a proper diagnosis by providers in the medical community in addition to a general understanding of the treatment options and timing of surgical interventions by musculoskeletal specialists.
Acknowledgment
The authors thank Samuel W. Golenbock, MS, and Qingping Cui, MPH, for assisting with statistical analysis.
Footnotes
Final revision submitted March 1, 2020; accepted March 13, 2020.
One or more of the authors has declared the following potential conflict of interest or source of funding: B.C.S. has received educational support from Arthrex and Smith & Nephew, grant support from Linvatec, and hospitality payments from Biomet, Encore Medical, and Stryker. T.H.W. has received educational support from Arthrex and Smith & Nephew, faculty speaker fees from Linvatec, consulting fees from Stryker, and hospitality payments from ArthroCare and Kairos Surgical. S.L.M. has received educational support from Kairos Surgical and consulting fees from DePuy and Parcus Medical. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from New England Baptist Hospital (protocol No. 1038383-1).
References
- 1. Aldridge SE, Heilpern GN, Carmichael JR, Sprowson AP, Wood DG. Incomplete avulsion of the proximal insertion of the hamstring: outcome two years following surgical repair. J Bone Joint Surg Br. 2012;94(5):660–662. [DOI] [PubMed] [Google Scholar]
- 2. Amstutz HC, Thomas BJ, Jinnah R, Kim W, Grogan T, Yale C. Treatment of primary osteoarthritis of the hip: a comparison of total joint and surface replacement arthroplasty. J Bone Joint Surg Am. 1984;66(2):228–241. [PubMed] [Google Scholar]
- 3. Barnett AJ, Negus JJ, Barton T, Wood DG. Reattachment of the proximal hamstring origin: outcome in patients with partial and complete tears. Knee Surg Sports Traumatol Arthrosc. 2015;23(7):2130–2135. [DOI] [PubMed] [Google Scholar]
- 4. Binkley JM, Stratford PW, Lott SA, Riddle DL. The Lower Extremity Functional Scale (LEFS): scale development, measurement properties, and clinical application. North American Orthopaedic Rehabilitation Research Network. Phys Ther. 1999;79(4):371–383. [PubMed] [Google Scholar]
- 5. Birmingham P, Muller M, Wickiewicz T, Cavanaugh J, Rodeo S, Warren R. Functional outcome after repair of proximal hamstring avulsions. J Bone Joint Surg Am. 2011;93(19):1819–1826. [DOI] [PubMed] [Google Scholar]
- 6. Bodendorfer BM, Curley AJ, Kotler JA, et al. Outcomes after operative and nonoperative treatment of proximal hamstring avulsions: a systematic review and meta-analysis. Am J Sports Med. 2018;46(11):2798–2808. [DOI] [PubMed] [Google Scholar]
- 7. Bowman KF, Jr, Cohen SB, Bradley JP. Operative management of partial-thickness tears of the proximal hamstring muscles in athletes. Am J Sports Med. 2013;41(6):1363–1371. [DOI] [PubMed] [Google Scholar]
- 8. Brucker PU, Imhoff AB. Functional assessment after acute and chronic complete ruptures of the proximal hamstring tendons. Knee Surg Sports Traumatol Arthrosc. 2005;13(5):411–418. [DOI] [PubMed] [Google Scholar]
- 9. Chahal J, Bush-Joseph CA, Chow A, et al. Clinical and magnetic resonance imaging outcomes after surgical repair of complete proximal hamstring ruptures: does the tendon heal? Am J Sports Med. 2012;40(10):2325–2330. [DOI] [PubMed] [Google Scholar]
- 10. Cohen S, Bradley J. Acute proximal hamstring rupture. J Am Acad Orthop Surg. 2007;15(6):350–355. [DOI] [PubMed] [Google Scholar]
- 11. Cohen SB, Rangavajjula A, Vyas D, Bradley JP. Functional results and outcomes after repair of proximal hamstring avulsions. Am J Sports Med. 2012;40(9):2092–2098. [DOI] [PubMed] [Google Scholar]
- 12. Cross MJ, Vandersluis R, Wood D, Banff M. Surgical repair of chronic complete hamstring tendon rupture in the adult patient. Am J Sports Med. 1998;26(6):785–788. [DOI] [PubMed] [Google Scholar]
- 13. Folsom GJ, Larson CM. Surgical treatment of acute versus chronic complete proximal hamstring ruptures: results of a new allograft technique for chronic reconstructions. Am J Sports Med. 2008;36(1):104–109. [DOI] [PubMed] [Google Scholar]
- 14. Harris JD, Griesser MJ, Best TM, Ellis TJ. Treatment of proximal hamstring ruptures: a systematic review. Int J Sports Med. 2011;32(7):490–495. [DOI] [PubMed] [Google Scholar]
- 15. Klingele KE, Sallay PI. Surgical repair of complete proximal hamstring tendon rupture. Am J Sports Med. 2002;30(5):742–747. [DOI] [PubMed] [Google Scholar]
- 16. Konan S, Haddad F. Successful return to high level sports following early surgical repair of complete tears of the proximal hamstring tendons. Int Orthop. 2010;34(1):119–123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Lempainen L, Sarimo J, Heikkila J, Mattila K, Orava S. Surgical treatment of partial tears of the proximal origin of the hamstring muscles. Br J Sports Med. 2006;40(8):688–691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Marx RG, Stump TJ, Jones EC, Wickiewicz TL, Warren RF. Development and evaluation of an activity rating scale for disorders of the knee. Am J Sports Med. 2001;29(2):213–218. [DOI] [PubMed] [Google Scholar]
- 19. Mica L, Schwaller A, Stoupis C, Penka I, Vomela J, Vollenweider A. Avulsion of the hamstring muscle group: a follow-up of 6 adult non-athletes with early operative treatment. A brief report. World J Surg. 2009;33(8):1605–1610. [DOI] [PubMed] [Google Scholar]
- 20. Miller SL, Gill J, Webb GR. The proximal origin of the hamstrings and surrounding anatomy encountered during repair: a cadaveric study. J Bone Joint Surg Am. 2007;89(1):44–48. [DOI] [PubMed] [Google Scholar]
- 21. Rust DA, Giveans MR, Stone RM, Samuelson KM, Larson CM. Functional outcomes and return to sports after acute repair, chronic repair, and allograft reconstruction for proximal hamstring ruptures. Am J Sports Med. 2014;42(6):1377–1383. [DOI] [PubMed] [Google Scholar]
- 22. Sallay PI, Ballard G, Hamersly S, Schrader M. Subjective and functional outcomes following surgical repair of complete ruptures of the proximal hamstring complex. Orthopedics. 2008;31(11):1092. [PubMed] [Google Scholar]
- 23. Sandmann GH, Hahn D, Amereller M, et al. Mid-term functional outcome and return to sports after proximal hamstring tendon repair. Int J Sports Med. 2016;37(7):570–576. [DOI] [PubMed] [Google Scholar]
- 24. Sarimo J, Lempainen L, Mattila K, Orava S. Complete proximal hamstring avulsions: a series of 41 patients with operative treatment. Am J Sports Med. 2008;36(6):1110–1115. [DOI] [PubMed] [Google Scholar]
- 25. Shambaugh BC, Olsen JR, Lacerte E, Kellum E, Miller SL. A comparison of nonoperative and operative treatment of complete proximal hamstring ruptures. Orthop J Sports Med. 2017;5(11):2325967117738551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Skaara HE, Moksnes H, Frihagen F, Stuge B. Self-reported and performance-based functional outcomes after surgical repair of proximal hamstring avulsions. Am J Sports Med. 2013;41(11):2577–2584. [DOI] [PubMed] [Google Scholar]
- 27. Subbu R, Benjamin-Laing H, Haddad F. Timing of surgery for complete proximal hamstring avulsion injuries: successful clinical outcomes at 6 weeks, 6 months, and after 6 months of injury. Am J Sports Med. 2015;43(2):385–391. [DOI] [PubMed] [Google Scholar]
- 28. van der Made AD, Reurink G, Gouttebarge V, Tol JL, Kerkhoffs GM. Outcome after surgical repair of proximal hamstring avulsions: a systematic review. Am J Sports Med. 2015;43(11):2841–2851. [DOI] [PubMed] [Google Scholar]
- 29. Wood DG, Packham I, Trikha SP, Linklater J. Avulsion of the proximal hamstring origin. J Bone Joint Surg Am. 2008;90(11):2365–2374. [DOI] [PubMed] [Google Scholar]