Cardiovascular disease (CVD) mortality has declined over the years.1,2 However, consistent trends were not observed among adults <50 years.1 We examined CVD mortality trends among adults 25 to 44 years to gain further insight about this population. The Centers for Disease Control and Prevention Wide-ranging Online Data for Epidemiologic Research database was used, which includes the assigned cause of mortality from all death certificates filed in the 50 states and District of Columbia.2 We examined underlying causes of death listed as CVD (the International Statistical Classification of Diseases, Tenth Revision Codes: 100–178); ischemic heart disease (IHD) (I20 to I25), cerebrovascular disease (I60 to I69), heart failure (HF), (I50) and infective endocarditis (IE) (I33). Mortality rates were age-adjusted using the 2000 U.S. standard population. Results were stratified by age, sex, and race. Temporal trends were examined to identify changes in slope using Join-point Regression Program version 4.7.0.0, which models consecutive linear segments on a log scale, connected by joinpoints where the segments meet.3 Annual percent change (APC) with 95% confidence intervals (CIs) were calculated using Monte Carlo permutation test. Statistical significance was set at 5%.
Between 1999 and 2018 (total population aged 25 to 44 of 1,675,571,454), there were 373,363 deaths attributed to overall CVD; most occurred due to IHD (n = 140,566), followed by cerebrovascular disease (n = 52,395), HF (n = 8,705), and IE (n = 3,183). The age-adjusted mortality rate (AAMR) per 100,000 population for overall CVD (24.8 to 21.8), IHD (10.5 to 6.8) and cerebrovascular disease (3.7 to 2.8) decreased; but increased for HF (0.4 to 0.8) and IE (0.2 to 0.4). Overall, men had higher AAMRs than women, Blacks had higher AAMRs than other races, and non-Hispanics had higher AAMRs than Hispanics.
From 1999 to 2013, APC in AAMR for overall CVD was −1.2 (95%CI, −1.5, −0.8), which slowed down between 2013 and 2018 (0.4 [95%CI, −1.2, 2.0]). While this trend was consistent for cerebrovascular disease, reduction in APC in AAMR for IHD accelerated since 2002 (Figure 1). Conversely, APC in AAMR substantially increased for HF and IE since 2012 and 2010, respectively. Generally, mortality trends were stagnant in Asians/Pacific Islanders, American Indians/American Natives and Hispanics. The APC in AAMR increased for ages 25 to 34 years and men for HF and IE; Women, Whites and non-Hispanics for IE; and Blacks for HF.
Figure 1.
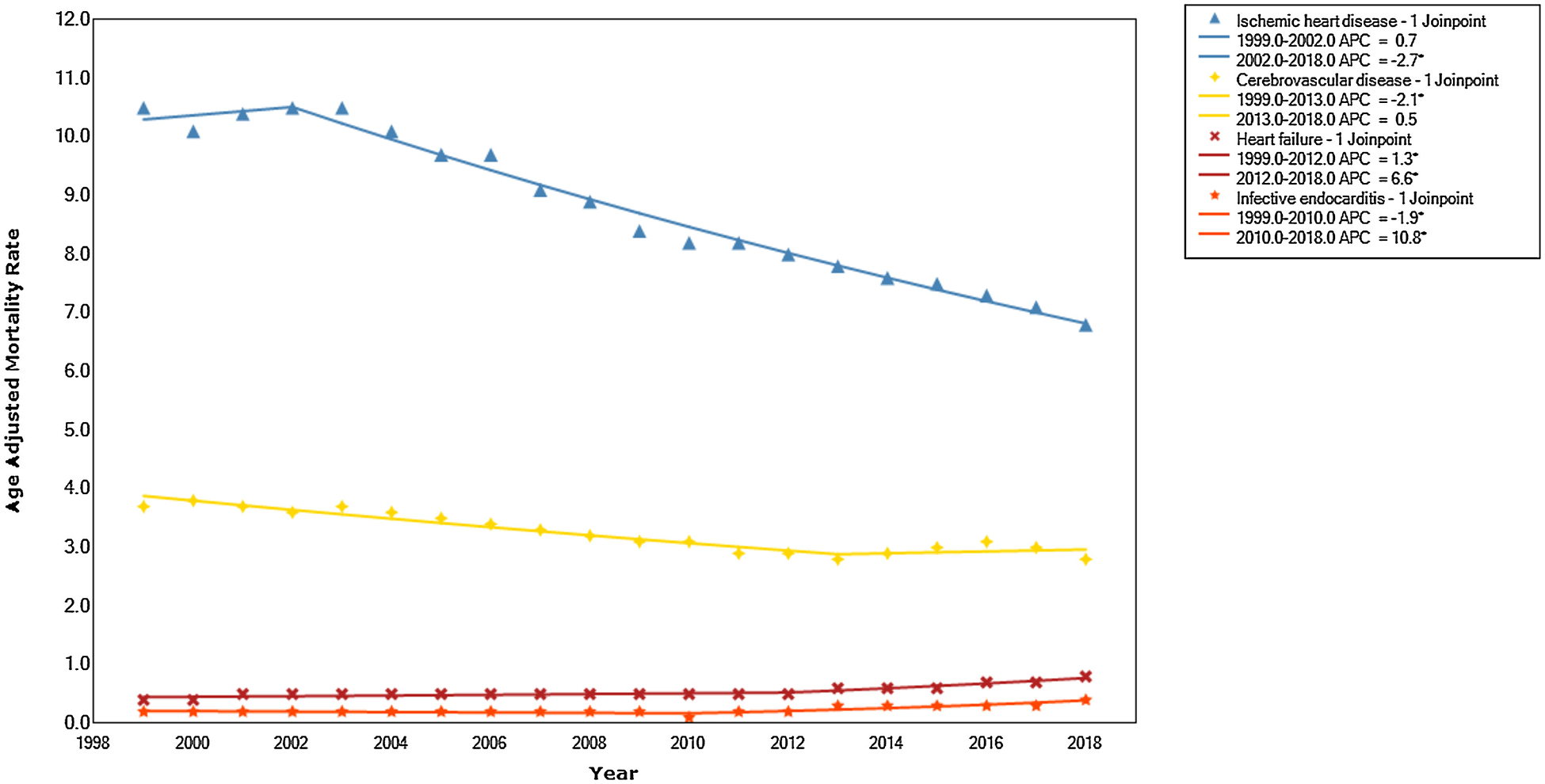
Trends in cardiovascular death among young adults aged 25 to 44 years, 1999 to 2018. *Indicates that the annual percent change (APC) is significantly different from zero at the alpha = 0.05.
In a prior report up to 2016,1 reduction in premature CVD mortality was driven by 50 to 64 years old. Whereas, the death rates were either flat or increased in certain racial subgroups in <50 years.1 However, the assessment of dynamic CVD mortality trends across different diseases and respective demographic subgroups remained unclear in this age group. This contemporary data showed that in 25 to 44 years old, the mortality rates declined for overall CVD and most of the component diseases, except for HF and IE. During last decade, the death rates either slowed down or continued to rise for HF and IE, except IHD where mortality continued to decline. Significant disparities existed among demographic subgroups.
Limitations of this study include lack of information on comorbidity burden, socioeconomic indicators, risk factors such as smoking and drug abuse and reliance on death certificate data. While the information on death certificates carry the potential of misclassification,4 use of death certificate data is the most feasible method of examining trends of CVD mortality in U.S. population.
In sum, these trends suggest that despite efforts by medical community, it is likely that the treatment strategies have not penetrated equally in young adults.5,6 Factors such as low socioeconomic status, limited access to quality health care, substance abuse, and lack of awareness about preventive strategies can further contribute to this growing burden of CVD in young adults.
Footnotes
Disclosures
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Chen Y, Freedman ND, Albert PS, Huxley RR, Shiels MS, Withrow DR, Spillane S, Powell-Wiley TM, Berrington de Gonzalez A. Association of cardiovascular disease with premature mortality in the United States. JAMA Cardiol 2019;4:1230–1238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.National Center for Health Statistics, CDC. About Underlying Cause of Death 1999–2018. https://wonder.cdc.gov/wonder/help/ucd.html# Accessed on April 1, 2020.
- 3.Woolf SH, Schoomaker H. Life expectancy and mortality rates in the United States, 1959–2017. JAMA 2019;322:1996–2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Benjamin EJ, Muntner P, Alonso A, Bitten-court MS, Callaway CW, Carson AP, Chamberlain AM, Chang AR, Cheng S, Cheng SR, Delling FN, Djousse L, Elkind MSV, Ferguson JF, Fornage M, Jordan LC, Khan SS, Kissela BM, Knutson KL, Kwan TW, Lack-land DT, Lewis TT, Lichtman JH, Longenecker CT, Loop MS, Lutsey PL, Martin SS, Matsushita K, Moran AE, Mussolino ME, O’Flaherty M, Pandey A, Perak AM, Rosamond WD, Roth GA, Sampson UKA, Satou GM, Schroeder EB, Shah SH, Spartano NL, Stokes A, Tirschwell DL, Tsao CW, Turakhia MP, VanWagner LB, Wilkins JT, Wong SS, Virani SS. Heart disease and stroke statistics-2019 update: a report from the american heart association. Circulation 2019;139:e56–e528. [DOI] [PubMed] [Google Scholar]
- 5.Michos ED, Choi AD. Coronary artery disease in young adults: a hard lesson but a good teacher. J Coll Cardiol 2019;74:1879–1882. [DOI] [PubMed] [Google Scholar]
- 6.Yang J, Biery DW, Singh A, Divakaran S, DeFilippis EM, Wu WY, Klein J, Hainer J, Ramsis M, Natarajan P, Januzzi JL, Nasir K, Bhatt DL, Di Carli MF, Blankstein R. Risk factors and outcomes of very young adults who experience myocardial infarction: the partners YOUNG-MI registry. Am J Med 2020;133:605–612.e1. 10.1016/j.amjcard.2020.05.014 [DOI] [PMC free article] [PubMed] [Google Scholar]


