Abstract
Background
Comprehensive control of multiple cardiovascular risk factors reduces cardiovascular risk but is difficult to achieve.
Design
A multinational, cross-sectional, observational study.
Methods
The International ChoLesterol management Practice Study (ICLPS) investigated achievement of European Society of Cardiology (ESC)/European Atherosclerosis Society (EAS) guideline low-density lipoprotein cholesterol (LDL-C) targets in patients receiving lipid-modifying therapy in countries outside Western Europe. We examined the rate of, and association between, control of multiple risk factors in ICLPS participants with dyslipidaemia, diabetes and hypertension (N = 2377).
Results
Mean (standard deviation) age of patients was 61.4 (10.4) years; 51.3% were male. Type 2 diabetes was the most common form of diabetes (prevalence, 96.9%). The prevalence of metabolic syndrome was 67.8%, obesity 40.4%, atherosclerotic disease 39.6% and coronary artery disease 33.5%. All patients were at high (38.2%) or very high (61.8%) cardiovascular risk according to ESC/EAS guidelines. Body mass index (BMI) was <25 kg/m2 in 20.3% of patients, 62.8% had never smoked and 25.2% were former smokers. Overall, 12.2% achieved simultaneous control of LDL-C, diabetes and blood pressure. Risk factor control was similar across all participating countries. The proportion of patients achieving individual guideline-specified treatment targets was 43.9% for LDL-C, 55.5% for blood pressure and 39.3% for diabetes. Multiple correspondence analysis indicated that control of LDL-C, control of blood pressure, control of diabetes, BMI and smoking were associated.
Conclusion
Comprehensive control of multiple cardiovascular risk factors in high-risk patients is suboptimal worldwide. Failure to control one risk factor is associated with poor control of other risk factors.
Keywords: Cardiovascular disease, diabetes mellitus, dyslipidaemia, hypertension, observational study, risk factors
Introduction
INTERHEART demonstrated that dyslipidaemia, diabetes, hypertension, smoking and abdominal obesity are important cardiovascular risk factors in both sexes, at all ages and in all regions of the world.1 The combination of several mildly increased risk factors can be more deleterious than the presence of one isolated risk factor of ‘high intensity’, and treatment guidelines recommend comprehensive control of risk factors.2 Guidelines on cardiovascular prevention recommend targets for cardiovascular risk factor control (Supplementary Table 1).3 Diabetes, which is often accompanied by multiple risk factors, is associated with high cardiovascular risk.2,4 Intensive therapy targeting multiple risk factors reduces the risk of cardiovascular events and cardiovascular mortality in these patients.4 Observational studies suggest that control of multiple risk factors is inadequate,5–13 with reporting rates of simultaneous attainment of glycated haemoglobin (HbA1c), blood pressure and low-density lipoprotein cholesterol (LDL-C) goals of 4–30%.5–8 Studies in non-Western populations are limited, but generally report multifactor control rates of up to ∼10%.10–12 Variations between countries have not been studied extensively; however, poor control of risk factors has been implicated in the higher rates of cardiovascular events and mortality observed in low- and middle-income countries (LMICs) compared with high-income countries (HICs), despite the lower risk-factor burden in LMICs.14
For each patient, multiple factors interact to determine the likelihood of good risk factor control. In some instances, patient behaviour (e.g. medication adherence, exercise, smoking) may be the dominant determinant, while in other instances healthcare system-related factors (e.g. availability or reimbursement for medication, public information on cardiovascular diseases and their risk factors, adequate physician support and follow-up) or physician-related factors (e.g. correct identification of risk, optimizing medication for those not at target) influence goal attainment the most.
We hypothesized that, irrespective of country/geographical region, there is a relationship between control of multiple risk factors, such that patients with poor control of one risk factor are less likely to achieve control of others. The International ChoLesterol management Practice Study (ICLPS) was a multinational, cross-sectional, observational study to investigate the achievement of European Society of Cardiology (ESC)/European Atherosclerosis Society (EAS) guideline LDL-C targets,15 and their determinants, in real-world clinical practice in countries outside Western Europe.16 Here we report goal achievement data in ICLPS participants with both diabetes and hypertension. We also investigate any association between control of predominantly physician-modifiable (LDL-C, blood pressure and diabetes) and predominantly patient-modifiable (body weight and smoking) risk factors using an exploratory multiple correspondence analysis (MCA).
Methods
ICLPS was conducted in 452 centres in 18 countries in Africa, Asia, Eastern Europe, Latin America and the Middle East between August 2015 and August 2016. The methods have been described previously.16 A full list of participating physician investigators (physicians) is provided in Supplementary Table 2. ICLPS was conducted according to the Declaration of Helsinki principles, guidelines for Good Epidemiology Practice and local regulations. Local or regional institutional review boards and/or ethics committee approval was obtained, where required. All patients provided written informed consent.
Patients
ICLPS participants were ≥18 years of age, had been receiving a stable dose and type of lipid-modifying therapy (LMT) for ≥3 months before enrolment, and had had their LDL-C value measured on stable LMT in the previous 12 months. To reduce selection bias, participating investigators recruited eligible patients consecutively (at least five patients were recruited per site) during a predefined two-week interval. All consecutive consenting patients, who attended their physician for any reason, were enrolled at any one site, that is, investigators did not select specific patients for enrolment. Use of a proprotein convertase subtilisin/kexin type 9 (PCSK9) inhibitor in the previous six months was an exclusion criterion.
In the current study, the eligible population comprised ICLPS participants with dyslipidaemia, diabetes and hypertension, in whom achievement of LDL-C, blood pressure and HbA1c target could be assessed. Patients were considered to have hypertension if they had a physician-defined diagnosis or history of hypertension, or systolic (SBP) ≥140 mmHg and/or diastolic blood pressure (DBP) ≥90 mmHg at enrolment.
Data collection and management
The physician completed a case-report form for each patient during a single visit. This case-report form included demographics, findings of physical examination, medical history, lipid values (on current treatment and at diagnosis, if available), HbA1c, current LMTs and the physician’s assessment of the patient’s cardiovascular risk level.
Definitions of risk factor control
Risk factor targets were based on the 2012 European guidelines,3 which were the guidelines in place when the study was planned. LDL-C targets were <1.8 mmol/L (∼70 mg/dL) or 50% LDL-C reduction (for those patients for whom baseline untreated LDL-C was available) when target levels could not be reached for very high-risk patients, and <2.5 mmol/L (∼100 mg/dL) for high-risk patients. Blood pressure control was defined as SBP <140 mmHg and DBP <90 mmHg, and diabetes control as HbA1c <7%. Patients with a body mass index (BMI) <25 kg/m2 were considered to have their body weight controlled. Control of smoking was defined as being a former smoker or having never smoked.
Statistical analysis
Descriptive statistics (mean ± standard deviation (SD) or median, interquartile range (IQR), for continuous variables, and counts (percentages) for categorical data) were used to present the data.
Factors associated with failure to achieve control of blood pressure and diabetes were studied using a mixed categorical model, which included variables at the patient level. Criteria with a p value ≤0.10 in univariate analysis and recorded in more than 80% of patients were checked for collinearity (with Cramer’s V statistics). Selected criteria were included in the model in a descending stepwise procedure. Criteria significant in the model at the 5% level were retained in the final model. C-statistics (a measure of goodness of fit of the logistic models) were calculated with the respective 95% confidence intervals.
The relationships between achievement of LDL-C target, diabetes control and blood pressure control, and BMI and smoking status, were assessed using MCA. MCA graphically represents the relationships between multiple sets of categorical data. Further details are provided in Supplementary Figure 1.
Results
Both diabetes and hypertension were present in 3879/9046 (42.9%) of ICLPS participants (Supplementary Figure 2). Following exclusion of 1502 patients for whom HbA1c was not available, 2377 (61.3%) patients were included in this study (Supplementary Figure 2). Presenting characteristics and medical history of included and excluded patients are compared in Supplementary Table 3.
In Supplementary Table 4, demographics, presenting characteristics and medical history are shown for the study population overall and by the number of predominantly physician-modifiable risk factors controlled. The mean (SD) age of the patients was 61.4 (10.4) years and 51.3% were male. Most patients had type 2 diabetes (96.9%), metabolic syndrome was present in 67.8%, obesity in 40.4%, documented coronary artery disease (CAD) in 33.5% and atherosclerotic disease in 39.6%. All patients were at high (38.2%) or very high (61.8%) cardiovascular risk according ESC/EAS guidelines.
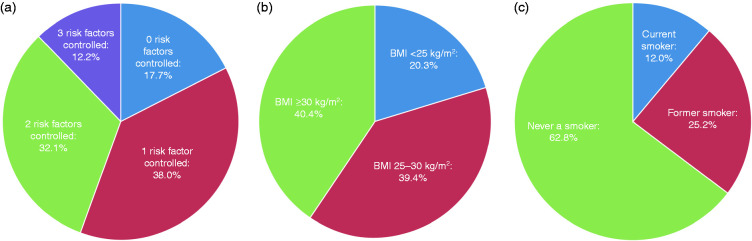
The proportion of patients achieving treatment targets was 43.9% for LDL-C, 55.5% for blood pressure and 39.3% for diabetes (Supplementary Table 4). All three risk factors were controlled in 12.2% of patients (Figure 1(a)). None, one and two risk factors were controlled in 17.7%, 38.0% and 32.1% of patients, respectively (Figure 1(a)). These findings were generally consistent across all participating countries (Supplementary Figure 3). Overall, 20.3% of patients had BMI <25 kg/m2 (Supplementary Table 4; Figure 1(b)), 62.8% had never smoked and 25.2% were former smokers (Supplementary Table 4; Figure 1(c)).
Figure 1.
Proportion of ICLPS participants with both diabetes and hypertension (a) with none, one, two and three risk factors controlled (n = 2377), (b) by BMI category (n = 2339), and (c) by tobacco use category (n = 2377) at enrolment.
ICLPS: International ChoLesterol management Practice Study; BMI: body mass index.
The mean (SD) duration of diabetes was 11.7 (7.4) years in patients with no risk factors controlled and 8.7 (7.4) years in those with all three risk factors controlled (Supplementary Table 4). Almost half (49.4%) of patients with no risk factors controlled were obese compared with less than one-third (30.3%) of those with all three risk factors controlled (Supplementary Table 4).
Table 1 presents the number of patients treated with LMT, antidiabetic therapies and antihypertensive therapies at enrolment, overall and by number of predominantly physician-modifiable risk factors controlled. Of patients with all three risk factors controlled, 21.3% were treated with high intensity statin (versus 32.6% for patients with no risk factors controlled). The proportion of patients taking an angiotensin II receptor blocker (ARB) was relatively high in those with three risk factors controlled (63.7% versus 46.0% in those with no risk factors controlled). Insulin use was frequent in patients with no risk factors controlled (52.9% versus 17.3% in patients with three risk factors controlled).
Table 1.
Use of lipid-modifying, antidiabetic and antihypertensive therapies at enrolment, overall and by number of physician-modifiable risk factors controlled.
| Number of risk factors controlled |
Total N = 2377 | ||||
|---|---|---|---|---|---|
| None n = 420 | One n = 904 | Two n = 764 | Three n = 289 | ||
| LMT | |||||
| Any statin | 408 (97.1%) | 883 (97.7%) | 751 (98.3%) | 287 (99.3%) | 2329 (98.0%) |
| High intensity statin (in statin-treated patients) | 133/408 (32.6%) | 228/883 (25.8%) | 171/751 (22.8%) | 61/287 (21.3%) | 593/2329 (25.5%) |
| On highest dose of statin (in statin-treated patients) | 114/408 (27.9%) | 223/883 (25.3%) | 169/751 (22.5%) | 63/287 (22.0%) | 569/2329 (24.5%) |
| Statin monotherapy | 341 (81.2%) | 753 (83.3%) | 661 (86.5%) | 254 (87.9%) | 2009 (84.5%) |
| Statin + fibrate ± other LMT | 42 (10.0%) | 90 (10.0%) | 59 (7.7%) | 20 (6.9%) | 211 (8.9%) |
| Statin + cholesterol absorption inhibitor ± other LMT | 15 (3.6%) | 29 (3.2%) | 16 (2.1%) | 7 (2.4%) | 67 (2.8%) |
| Antihypertensive therapies | |||||
| Any antihypertensive therapy | |||||
| Yes | 382 (91.0%) | 831 (91.9%) | 700 (91.6%) | 278 (96.2%) | 2191 (92.2%) |
| No | 34 (8.1%) | 66 (7.3%) | 52 (6.8%) | 8 (2.8%) | 160 (6.7%) |
| Unknown | 4 (1.0%) | 7 (0.8%) | 12 (1.6%) | 3 (1.0%) | 26 (1.1%) |
| ACEI | 143 (34.0%) | 258 (28.5%) | 185 (24.2%) | 54 (18.7%) | 640 (26.9%) |
| ARB | 193 (46.0%) | 443 (49.0%) | 409 (53.5%) | 184 (63.7%) | 1229 (51.7%) |
| Diuretic | 156 (37.1%) | 293 (32.4%) | 230 (30.1%) | 101 (34.9%) | 780 (32.8%) |
| Beta-blocker | 148 (35.2%) | 350 (38.7%) | 299 (39.1%) | 115 (39.8%) | 912 (38.4%) |
| Calcium-channel blocker | 142 (33.8%) | 291 (32.2%) | 216 (28.3%) | 87 (30.1%) | 736 (31.0%) |
| Other antihypertensive | 28 (6.7%) | 64 (7.1%) | 42 (5.5%) | 9 (3.1%) | 143 (6.0%) |
| Any antihypertensive combination therapy | 253 (60.2%) | 554 (61.3%) | 445 (58.2%) | 171 (59.2%) | 1423 (59.9%) |
| ACEI ± other antihypertensive therapy | 97 (23.1%) | 182 (20.1%) | 131 (17.1%) | 39 (13.5%) | 449 (18.9%) |
| ARB ± other antihypertensive therapy | 140 (33.3%) | 327 (36.2%) | 287 (37.6%) | 121 (41.9%) | 875 (36.8%) |
| ACEI + ARB ± other antihypertensive therapy | 5 (1.2%) | 13 (1.4%) | 5 (0.7%) | 3 (1.0%) | 26 (1.1%) |
| Antidiabetic therapies | |||||
| Any antidiabetic therapy | 419 (99.8%) | 893 (98.8%) | 748 (97.9%) | 286 (99.0%) | 2346 (98.7%) |
| Insulin | |||||
| Yes | 222 (52.9%) | 393 (43.5%) | 221 (28.9%) | 50 (17.3%) | 886 (37.3%) |
| No | 191 (45.5%) | 493 (54.5%) | 524 (68.9%) | 231 (79.9%) | 1439 (60.6%) |
| Unknown | 7 (1.7%) | 18 (2.0%) | 19 (2.5%) | 8 (2.8%) | 52 (2.2%) |
| Oral antidiabetic | |||||
| Yes | 360 (85.7%) | 781 (86.4%) | 685 (89.7%) | 274 (94.8%) | 2100 (88.3%) |
| No | 55 (13.1%) | 113 (12.5%) | 60 (7.9%) | 9 (3.1%) | 237 (10.0%) |
| Unknown | 5 (1.2%) | 10 (1.1%) | 19 (2.5%) | 6 (2.1%) | 40 (1.7%) |
Data are n (%) or n/n (%).
LMT: lipid-modifying therapy; ACEI: angiotensin-converting enzyme inhibitor; ARB: angiotensin II receptor blocker.
Findings for patients with obesity (Supplementary Tables 5 and 6) and patients with atherosclerotic disease (Supplementary Tables 7 and 8) were consistent with the findings of the study population overall.
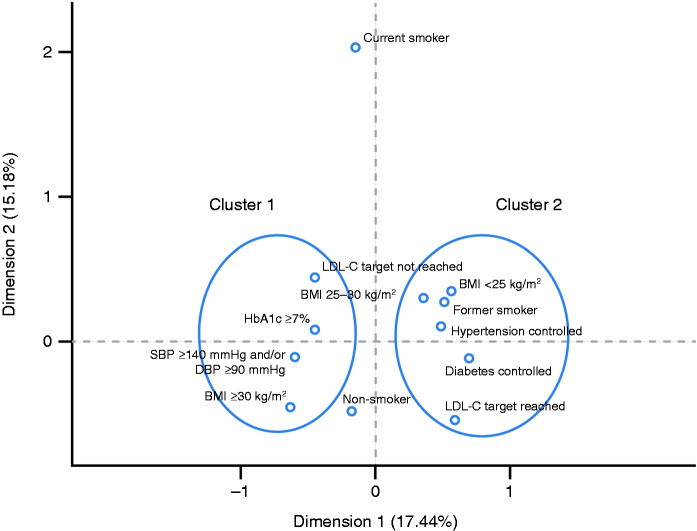
Multiple correspondence analysis
The findings of the MCA are shown in Figure 2. Two clusters were identified (highlighted by circles). Cluster 1 includes ‘LDL-C target not reached’, ‘HbA1c ≥7%’, ‘SBP ≥140 mmHg and/or DBP ≥90 mmHg’ and ‘BMI ≥30 kg/m2’. Cluster 2 includes ‘LDL-C target reached’, ‘diabetes controlled’, ‘hypertension controlled’, ‘BMI <25 kg/m2’ and ‘former smoker’. These findings indicate an association between control of predominantly physician-modifiable and predominantly patient-modifiable risk factors, and suggests that the typical poorly controlled patient is obese with multiple poorly controlled risk factors. The arrangement of these clusters, on opposite sides of the origin, along dimension 1 suggests that this dimension represents risk-factor control, with negative values indicating poorer control and positive values indicating better control.
Figure 2.
Multiple correspondence analysis of modifiable risk factors in ICLPS participants with both diabetes and hypertension (n = 2339).
LDL-C: low-density lipoprotein cholesterol; BMI: body mass index; ICLPS: International ChoLesterol management Practice Study; HbA1c: glycated haemoglobin; SBP: systolic blood pressure; DBP: diastolic blood pressure.
Multivariable analysis
The findings of the multivariable analysis of failure to achieve blood pressure and diabetes control are shown in Supplementary Figure 4. Failure to achieve blood pressure control was associated with higher BMI, HbA1c ≥7% (i.e. failure to achieve diabetes control), statin intolerance and failure to achieve LDL-C target (Supplementary Figure 4(a)). Failure to achieve diabetes control was associated with elevated blood pressure, failure to achieve LDL-C target, obesity, very high cardiovascular risk, no health insurance, insurance without drug reimbursement and time since diabetes diagnosis, and was inversely associated with neurocognitive disorders (Supplementary Figure 4(b)).
Discussion
In our study, few patients achieved simultaneous control of LDL-C, blood pressure and HbA1c. There was an association between the control of these modifiable risk factors, body weight and smoking, such that when one risk factor was poorly controlled there was a greater risk that other risk factors were not controlled. This poor control of cardiovascular risk was similar across all participating countries, and was consistent with low goal attainment rates reported previously for studies conducted predominantly in North America and Western Europe.5–13 As ICLPS was performed in countries and geographical regions often overlooked by other international studies, these findings indicate that poor control of multiple risk factors is a worldwide problem.
Despite evidence that physicians escalated treatment in patients with poor risk-factor control, the study population was undertreated overall, as indicated by low prescription rates of high intensity statins, cholesterol absorption inhibitors (CAIs) and antihypertensive therapy including either an angiotensin-converting enzyme inhibitor (ACEI) or ARB. Comparison of cardiovascular risk assessed by investigators and calculated according to guidelines indicates that physicians underestimate risk, which may have contributed to undertreatment. Healthcare system factors, such as limited availability of optimal therapy, restrictive reimbursement policies and inequitable healthcare services, are other important causes of undertreatment in LMICs. As such, socioeconomic factors may account for some variation in attainment of treatment targets between countries. Socioeconomic status is negatively associated with cardiovascular risk and prevalence of diabetes in HICs,17–19 but this relationship is less well studied in LMICs. A systematic review of studies in 17 LMICs reported a lower risk of cardiovascular disease but higher prevalence of diabetes in participants with higher socioeconomic status,20 and higher rates of cardiovascular risk factors are observed in participants living in urban compared with rural areas21,22 and in those with highest wealth,21 likely as a result of a greater adoption of a Western lifestyle. In the present study, both ‘no health insurance’ and ‘insurance without drug reimbursement’ were associated with HbA1c ≥7%, implicating lack of availability of therapy as a factor limiting diabetes control. This is an important finding in terms of worldwide health inequalities and may result from restrictive reimbursement policies. Delays in the approval of new medications in some LMICs may further impair access to optimal therapy.
Our study shows that control of risk factors did not differ markedly among participating countries, and was no better or worse than that observed in European countries in patients with documented coronary disease.13 High rates of obesity, metabolic syndrome, atherosclerotic disease and CAD were noted in the subgroup of patients in whom no risk factors were controlled, which suggests that these patients constitute a group that is particularly difficult to treat. This group had a greater proportion of very high-risk patients, and is therefore challenging to treat in terms of dyslipidaemia, because guidelines specify more stringent LDL-C targets for these patients.15 This group was more likely to be receiving intensive statin therapy and insulin, suggesting that physicians rightly escalate treatment in these patients but that the goals remain difficult to achieve even when using currently recommended treatment regimens. Although the initial intensity of each risk factor is unknown because of a lack of baseline (pre-treatment) data, it is likely that the patients with no risk factors controlled included the most severe and challenging patients.
The finding that predominantly physician-modifiable and predominantly patient-modifiable risk factors were associated suggests that patient attitudes and behaviour may be factors influencing control across multiple risk factors. Non-adherence to therapy may limit the attainment of treatment targets; however, adherence was not assessed in ICLPS. Diabetes control often requires more complex therapy and greater patient involvement compared with control of hypertension and dyslipidaemia. This was reflected in the finding that, of the physician-modifiable risk factors, blood pressure control was the goal most frequently achieved (55.5%) followed by LDL-C (43.9%) and diabetes (39.3%), even when the HbA1c threshold used for defining diabetes control was ‘lenient’ (HbA1c <7%). It is of interest that, in the MCA, ‘former smoker’ clusters with good control of risk factors, while ‘current smoker’ is far removed from the other variables. The patient’s motivation to stop smoking may be a good marker of their ability to control other risk factors; however, this requires further study before any conclusion can be drawn.
PCSK9 inhibitors were not available in most countries that participated in ICLPS at the time of the study. In addition, guidelines updated since ICLPS recommend more intensive pharmacotherapy for blood pressure and glycaemic control.23,24 Combination antihypertensive therapy (either an ACEI or ARB with a calcium-channel blocker or diuretic) is now recommended as initial therapy for most patients with hypertension, preferably as single pill combination.24 For glycaemic control in patients with type 2 diabetes, guidelines advocate for intensification of treatment with glucagon-like peptide-1 receptor agonists, sodium–glucose cotransporter-2 inhibitors or prandial insulin in patients not at glycaemic targets with basal insulin/oral antidiabetic combination therapy.23 The greater use of combination therapy and of newer, more effective medications may improve attainment of treatment targets and reduce cardiovascular risk; however, access to new treatment options is likely to remain limited, at least for a while, in LMICs.
The contribution of patient beliefs and behaviour to poor risk-factor control suggests that new medications alone will not be sufficient to improve multiple risk target attainment. Patient awareness of cardiovascular risk factors is low even among the secondary prevention population,25 and improvements in patient education are necessary across the entire cardiovascular risk continuum. Specific public health policies, such as incentives on proper nutritional behaviour, smoking bans or increased cigarette prices, are likely to impact individual risk factors, although their impact may differ according to socio-economic environment.26 Health promotion interventions that aim to reduce more than one major cardiovascular risk factor in the primary prevention population have had limited benefit for changing patients’ behaviour, although there is a lack of data in LMICs.27
Limitations
ICLPS was subject to limitations that have been described previously.16 These include missing data, the observational nature of the study, a potential for selection bias, and that LMTs and doses varied according to site/physician preference. Approximately 40% of patients with diabetes were excluded from the study population because their HbA1c level was not available. This may have introduced bias because missing HbA1c data may be an indication of poorer overall care. In addition, the majority of the ICLPS population were educated urban residents with health insurance, and only statin-treated patients were enrolled; our study population was therefore not fully representative of all patients with dyslipidaemia, hypertension and diabetes. This potential bias, however, makes our conclusions all the more relevant; even in patients receiving LMT, comprehensive risk factor control remains suboptimal. Patient adherence to medication was not assessed. In addition, guidelines recommend more stringent targets for patients at higher cardiovascular risk,15 therefore the proportion of patients achieving control of no risk factors may have been increased by the higher proportion of very high-risk patients in this group. The lack of baseline data for the risk factors studied is also a limitation because it was not possible to study the dynamic evolution of risk after treatment. Finally, MCA is a visual exploratory analysis only, it is not intended for proving hypotheses, and further research is required to confirm its findings.
Conclusion
This study indicates that control of multiple cardiovascular risk factors in high-risk patients is suboptimal worldwide, with few patients (12.2%) with dyslipidaemia, diabetes and hypertension achieving simultaneous control of LDL-C, blood pressure and HbA1c. Failure to achieve one target was associated with failure to achieve control of other risk factors, further compounding risk.
Limited use of intensive statin therapy, CAI and combination antihypertensive therapy indicates undertreatment of these high-risk patients, which may result from physician and healthcare system factors. However, the observation that attainment rates were similar across participating countries, and similar to rates previously reported in HICs, suggest that poor control of cardiovascular risk is a global problem, largely independent of country and socioeconomic system.
A comprehensive approach should be taken to cardiovascular risk factor management rather than treating individual risk factors in isolation. Wider adoption of intensive therapy coupled with greater patient education is needed to address the worldwide problem of poor risk factor control.
Author contribution
ND, DJB, AJR and RDS contributed to the acquisition or interpretation of data for the work. VD contributed to the conception or design of the work. FM performed the analyses. All authors critically revised the manuscript, gave final approval and agree to be accountable for all aspects of work ensuring integrity and accuracy.
Supplemental Material
Supplemental Material for The challenge of multiple cardiovascular risk factor control outside Western Europe: Findings from the International ChoLesterol management Practice Study by Dirk J Blom, Raul D Santos, Veronique Daclin, Florence Mercier, Alvaro J Ruiz, Nicolas Danchin and on behalf of the ICLPS study group in European Journal of Preventive Cardiology
Acknowledgements
The authors thank the patients, their families, trial staff and all investigators involved in this study. We also thank Gemma Grundy, BSc, from Sanofi for coordinating the development of the ICLPS sub-analyses and this manuscript. Medical writing assistance and editorial support, under the direction of the authors, were provided by Fiona Van, PhD, and Elke Sims, MLangTrans, both of Prime (Knutsford, UK), funded by Sanofi according to Good Publication Practice guidelines (https://annals.org/aim/fullarticle/2424869/goodpublication-practice-communicating-company-sponsoredmedical-research-gpp3).
Declaration of conflicting interests
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: DJB, RDS, VD, AJR and ND report non-financial support from Sanofi during the conduct of the study; FM reports grants from Sanofi and other support from Stat Process during the conduct of the study. VD is an employee of Sanofi. DJB reports personal fees from Aegerion, Akcea, Amgen, AstraZeneca, Gemphire, Merck Sharp Dohme and Sanofi; RDS reports personal fees from Akcea, Amgen, AstraZeneca, Merck Sharp Dohme, Merck, Sanofi/Regeneron, Biolab, Esperion, Kowa and Novo-Nordisk, and is a recipient of a scholarship from the Conselho Nacional de Pesquisa e Desenvolvimento Tecnologico (CNPq) process # 303734/2018-3; AJR reports personal fees from Sanofi, Amgen, Pfizer, Valentech and Merck Sharp Dohme; ND reports grants, personal fees and non-financial support from Amgen, AstraZeneca, Bayer, Boehringer Ingelheim, Bristol-Myers Squibb, Daiichi Sankyo, Eli Lilly, Intercept, Merck Sharp Dohme, Novo Nordisk, Pfizer, Sanofi and Servier.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by Sanofi.
References
- 1.Yusuf S, Hawken S, Ounpuu S, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): Case-control study. Lancet 2004; 364: 937–952. [DOI] [PubMed] [Google Scholar]
- 2.Piepoli MF, Hoes AW, Agewall S, et al. 2016 European Guidelines on cardiovascular disease prevention in clinical practice: The Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts): Developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR). Eur J Prev Cardiol 2016; 23: NP1–NP96. [DOI] [PubMed] [Google Scholar]
- 3.Perk J, De Backer G, Gohlke H, et al. European Guidelines on cardiovascular disease prevention in clinical practice (version 2012). The Fifth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of nine societies and by invited experts). Developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR). Eur Heart J 2012; 33: 1635–1701. [DOI] [PubMed] [Google Scholar]
- 4.Rawshani A, Rawshani A, Franzén S, et al. Risk factors, mortality, and cardiovascular outcomes in patients with type 2 diabetes. N Engl J Med 2018; 379: 633–644. [DOI] [PubMed] [Google Scholar]
- 5.Song Y, Liu X, Zhu X, et al. Increasing trend of diabetes combined with hypertension or hypercholesterolemia: NHANES data analysis 1999–2012. Sci Rep 2016; 6: 36093–36093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bertoni AG, Clark JM, Feeney P, et al. Suboptimal control of glycemia, blood pressure, and LDL cholesterol in overweight adults with diabetes: The Look AHEAD Study. J Diabetes Complications 2008; 22: 1–9. [DOI] [PubMed] [Google Scholar]
- 7.Schroeder EB, Hanratty R, Beaty BL, et al. Simultaneous control of diabetes mellitus, hypertension, and hyperlipidemia in 2 health systems. Circ Cardiovasc Qual Outcomes 2012; 5: 645–653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fan W, Song Y, Inzucchi SE, et al. Composite cardiovascular risk factor target achievement and its predictors in US adults with diabetes: The Diabetes Collaborative Registry. Diabetes Obes Metab 2019; 21: 1121–1127. [DOI] [PubMed] [Google Scholar]
- 9.Bhatt DL, Eagle KA, Ohman EM, et al. Comparative determinants of 4-year cardiovascular event rates in stable outpatients at risk of or with atherothrombosis. JAMA 2010; 304: 1350–1357. [DOI] [PubMed] [Google Scholar]
- 10.Wang CY, Yu NC, Sheu WH, et al. Team care of type 2 diabetes mellitus in Taiwan. Diabetes Res Clin Pract 2014; 106: S309–S313. [DOI] [PubMed] [Google Scholar]
- 11.Wan EYF, Fung CSC, Yu EYT, et al. Effect of multifactorial treatment targets and relative importance of hemoglobin A1c, blood pressure, and low-density lipoprotein-cholesterol on cardiovascular diseases in Chinese primary care patients with type 2 diabetes mellitus: A population-based retrospective cohort study. J Am Heart Assoc 2017; 6: e006400–e006400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Liu L, Lou Q, Guo X, et al. Management status and its predictive factors in patients with type 2 diabetes in China: A nationwide multicenter study. Diabetes Metab Res Rev 2015; 31: 811–816. [DOI] [PubMed] [Google Scholar]
- 13.Kotseva K, De Backer G, De Bacquer D, et al. Lifestyle and impact on cardiovascular risk factor control in coronary patients across 27 countries: Results from the European Society of Cardiology ESC-EORP EUROASPIRE V registry. Eur J Prev Cardiol 2019; 26: 824–835. [DOI] [PubMed] [Google Scholar]
- 14.Yusuf S, Rangarajan S, Teo K, et al. Cardiovascular risk and events in 17 low-, middle-, and high-income countries. N Engl J Med 2014; 371: 818–827. [DOI] [PubMed] [Google Scholar]
- 15.Catapano AL, Graham I, De Backer G, et al. 2016 ESC/EAS Guidelines for the management of dyslipidaemias. Eur Heart J 2016; 37: 2999–3058. [DOI] [PubMed] [Google Scholar]
- 16.Danchin N, Almahmeed W, Al-Rasadi K, et al. Achievement of low-density lipoprotein cholesterol goals in 18 countries outside of Western Europe: The International ChoLesterol management Practice Study (ICLPS). Eur J Prev Cardiol 2018; 25: 1087–1094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kaplan GA, Keil JE. Socioeconomic factors and cardiovascular disease: A review of the literature. Circulation 1993; 88: 1973–1998. [DOI] [PubMed] [Google Scholar]
- 18.Jaffiol C, Thomas F, Bean K, et al. Impact of socioeconomic status on diabetes and cardiovascular risk factors: Results of a large French survey. Diabetes Metab Res Rev 2013; 39: 56–62. [DOI] [PubMed] [Google Scholar]
- 19.Chaturvedi N, Jarrett J, Shipley MJ, et al. Socioeconomic gradient in morbidity and mortality in people with diabetes: Cohort study findings from the Whitehall Study and the WHO Multinational Study of Vascular Disease in Diabetes. BMJ 1998; 316: 100–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Williams J, Allen L, Wickramasinghe K, et al. A systematic review of associations between non-communicable diseases and socioeconomic status within low- and lower-middle-income countries. J Glob Health 2018; 8: 020409–020409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rarau P, Pulford J, Gouda H, et al. Socio-economic status and behavioural and cardiovascular risk factors in Papua New Guinea: A cross-sectional survey. PLoS One 2019; 14: e0211068–e0211068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Aamir AH, Ul-Haq Z, Mahar SA, et al. Diabetes Prevalence Survey of Pakistan (DPS-PAK): Prevalence of type 2 diabetes mellitus and prediabetes using HbA1c: A population-based survey from Pakistan. BMJ Open 2019; 9: e025300–e025300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Davies MJ, D’Alessio DA, Fradkin J, et al. Management of hyperglycaemia in type 2 diabetes, 2018. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetologia 2018; 61: 2461–2498. [DOI] [PubMed] [Google Scholar]
- 24.Williams B, Mancia G, Spiering W, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J 2018; 39: 3021–3104. [DOI] [PubMed] [Google Scholar]
- 25.Lechowicz M, Wiliński J, Kameczura T, et al. Awareness of cardiovascular risk factors in ambulatory cardiology patients. Folia Med Cracov 2015; 55: 15–22. [PubMed] [Google Scholar]
- 26.Tauras JA, Huang J, Chaloupka FJ. Differential impact of tobacco control policies on youth sub-populations. Int J Environ Res Public Health 2013; 10: 4306–4322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Uthman OA, Hartley L, Rees K, et al. Multiple risk factor interventions for primary prevention of cardiovascular disease in low- and middle-income countries (review). Cochrane Database of Systematic Reviews 2015; 8: CD011163–CD011163. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material for The challenge of multiple cardiovascular risk factor control outside Western Europe: Findings from the International ChoLesterol management Practice Study by Dirk J Blom, Raul D Santos, Veronique Daclin, Florence Mercier, Alvaro J Ruiz, Nicolas Danchin and on behalf of the ICLPS study group in European Journal of Preventive Cardiology