Abstract
Objective:
Mental health issues in late life are a growing public health challenge as the population aged 65 and older rapidly increases worldwide. An updated understanding of the causes of mood disorders and their consequences in late life could guide interventions for this underrecognized and undertreated problem. We undertook a population-based analysis to quantify the prevalence of mood disorders in late life in Ontario, Canada, and to identify potential risk factors and consequences.
Method:
Individuals aged 65 or older participating in 4 cycles of a nationally representative survey were included. Self-report of a diagnosed mood disorder was used as the outcome measure. Using linked administrative data, we quantified associations between mood disorder and potential risk factors such as demographic/socioeconomic factors, substance use, and comorbidity. We also determined associations between mood disorders and 5-year outcomes including health service utilization and mortality.
Results:
The prevalence of mood disorders was 6.1% (4.9% among males, 7.1% among females). Statistically significant associations with mood disorders included younger age, female sex, food insecurity, chronic opioid use, smoking, and morbidity. Individuals with mood disorders had increased odds of all consequences examined, including placement in long-term care (adjusted odds ratio [OR] =2.28; 95% confidence interval [CI], 1.71 to 3.02) and death (adjusted OR = 1.35; 95% CI, 1.13 to 1.63).
Conclusions:
Mood disorders in late life were strongly correlated with demographic and social/behavioral factors, health care use, institutionalization, and mortality. Understanding these relationships provides a basis for potential interventions to reduce the occurrence of mood disorders in late life and their consequences.
Keywords: mood disorders, aging, epidemiology
Abstract
Objectif:
Les questions de santé mentale en âge avancé sont un problème croissant de santé publique alors que la population des 65 ans et plus s’accroît rapidement dans le monde entier. Une mise à jour des connaissances sur les causes des troubles de l’humeur et leurs conséquences en âge avancé pourrait guider les interventions pour ce problème mal reconnu et sous-traité. Nous avons entrepris une analyse dans la population afin de quantifier la prévalence des troubles de l’humeur en âge avancé en Ontario, Canada, et de nommer les facteurs de risque potentiels et les conséquences.
Méthode:
Les personnes de 65 ans ou plus participant à 4 cycles d’une enquête représentative à l’échelle nationale ont été incluses. L’auto-déclaration d’un trouble de l’humeur diagnostiqué a servi de mesure de résultat. À l’aide de données administratives couplées, nous avons quantifié les associations entre le trouble de l’humeur et les facteurs de risque potentiels comme les facteurs démographiques/socio-économiques, l’utilisation de substances, et la comorbidité. Nous avons aussi déterminé les associations entre les troubles de l’humeur et les résultats à 5 ans, y compris l’utilisation des services de santé et la mortalité.
Résultats:
La prévalence des troubles de l’humeur était de 6,1 % (4,9 % chez les hommes, 7,1 % chez les femmes). Les associations statistiquement significatives avec les troubles de l’humeur étaient notamment un plus jeune âge, le sexe féminin, l’insécurité alimentaire, l’utilisation chronique d’opioïdes, le tabagisme, et la morbidité. Les personnes souffrant de troubles de l’humeur avaient des probabilités accrues de toutes les conséquences examinées, dont le placement dans des soins de longue durée (RC [rapport de cotes] ajusté = 2,28; IC [intervalle de confiance] à 95 % 1,71 à 3,02); et la mort (RC ajusté = 1,35; IC à 95 % 1,13 à 1,63).
Conclusions:
Les troubles de l’humeur en âge avancé étaient fortement corrélés aux facteurs démographiques et sociaux/comportementaux, à l’utilisation des soins de santé, à l’institutionnalisation et à la mortalité. Comprendre ces relations constitue une base pour des interventions potentielles en vue de réduire la présence des troubles de l’humeur en âge avancé et leurs conséquences.
Introduction
Mood disorders among older adults (those aged 65 or older) are a burdensome public health issue, leading to psychological distress, social isolation, and poorer quality of life.1 This issue currently poses increasing concern due to the rapid growth of the older adult population worldwide. The global population of older adults is expected to reach approximately 16% in 2050 compared to 9% in 2018.2 Populations are expected to have increased comorbidities and dependency as individuals live longer.3 Health care systems may be both unprepared to adequately address these mental health issues and burdened by this population due to adverse outcomes that may arise due to mood disorders in late life. There is a gap in recent knowledge of the scope of mood disorders among this population, potential risk factors, as well as the potential consequences for individuals and the health care system, particularly based on linked population-based data. Although previous studies have explored associations between mood disorders and factors such as comorbidity, there is an opportunity to consider additional sociodemographic factors.
The 2017 Ontario Action Plan for Seniors released by the Government of Ontario reported that 7.2% of older adults in Ontario were considered to have a mood disorder in 2013-2014.4 A 2005 analysis of depression in elderly Canadians reported prevalence of 2.6% and 4% for major and minor depression, respectively, based on data from the Canadian Study of Health and Aging.5 The study reported higher prevalence of depression in females compared to males (9.3% vs. 2.9%) as well as in institutionalized individuals compared to community-dwelling individuals (12.7% vs. 6.0%).5
Beyond detrimental effects to the individual, mood disorders in this population can be taxing to the health care system. Others have evaluated health care utilization within this population, finding higher cost to health care systems by depressed individuals compared to nondepressed individuals.6,7 A recent analysis investigated direct costs associated with depression in Ontario, attributing annual costs of $210 million to those with major depressive disorder.8
We therefore undertook an analysis to (1) determine the prevalence of self-reported mood disorders diagnosed by a health professional among the older adult population in Ontario; (2) analyze risk factors associated with mood disorders; and (3) longitudinally assess consequences of mood disorders including health care use, long-term care placement, and mortality.
Methods
Setting and Population
Ontario is the most populous province in Canada, with a population of 13.4 million in 2016.9 Older adults are the fastest aging group in Ontario and are expected to double from 2.3 million in 2016 to 4.6 million by 2041.4
The study sample of Ontarians was derived from 4 cycles of the Canadian Community Health Survey (CCHS), a nationally representative survey of household residents conducted through both telephone and in-person interviews.10 The survey includes individuals from all provinces aged 12 or older, excluding those living in long-term care, on First Nation reserves, and individuals serving in the Canadian Armed Forces.10 Community-dwelling respondents living in Ontario, interviewed in the 2005, 2007, 2009, and 2011 cycles aged 65 or older at the interview date were pooled into the primary cohort. Individuals were excluded if their last contact with the health system was greater than 8 years prior to responding to the CCHS.
Information from the CCHS was linked to administrative databases available through the Institute for Clinical Evaluative Sciences (ICES). Demographic and outcome data were ascertained from numerous sources including the registry of individuals residing in Ontario, and health care service databases linked through the Ontario Health Insurance Plan (OHIP). A complete description of data sets used is provided in Supplemental Table 1A. These data sets were linked using unique encoded identifiers and analyzed at ICES. ICES is an independent, nonprofit research institute whose legal status under Ontario’s health information privacy law allows it to collect and analyze health care and demographic data, without consent, for health system evaluation and improvement.
Analysis 1: Prevalence of Mood Disorders
We first quantified the prevalence of a self-reported mood disorder using a measure provided from the four cycles of the CCHS. Individuals were considered to have a mood disorder if they answered yes to the question: “Do you have a mood disorder such as depression, bipolar disorder, mania, or dysthymia?” The question is asked in the context of a condition that is expected to last or has lasted 6 months or more and was diagnosed by a health professional.11 This measure of a self-reported health professional-diagnosed condition was the most appropriate available in all 4 cycles of the CCHS. For individuals who participated in multiple cycles, the first cycle of participation was used as their index interview date.
Analysis 2: Potential Risk Factors
We then performed a cross-sectional analysis to identify potential risk factors associated with having a mood disorder. Baseline characteristics of the population and potential risk factors for mood disorders were collected. Age was categorized into 3 groups (65 to 74, 75 to 84, and 85 and older). Self-reported level of education was categorized into levels of less than secondary education, some postsecondary education, and a postsecondary degree or diploma. Income was reported as quintiles of household income based on the 2006 Canadian census. Immigration status was also ascertained from the CCHS. Marital status was divided into categories of married/common-law, widowed, or single (including separated or divorced). Self-reported living situation was also assessed and dichotomized into lives alone and lives with another individual.
Factors relating to substance use included in the analysis were smoking status, alcohol consumption, and opioid use. Chronic opioid use was defined as 120 or more cumulative calendar days of filled opioid prescriptions in the year prior to the index date. Opioid use was restricted to those aged 66 and over, as the Ontario Drug Benefit data set only includes individuals at age 65. The Johns Hopkins Adjusted Clinical Group System was used to assign patients to one or more of 32 adjusted diagnosis groups (ADGs).12 Diagnoses within an ADG are similar clinically and in terms of expected need for health care.
Health care service use in the previous 2 years of the index date was investigated descriptively as a factor associated with mood disorders. This included visits to a psychiatrist; whether a patient had low, moderate, or high continuity of care with their primary care physician; and enrollment in a primary care model. Approximately three-quarters of Ontarians are formally enrolled with a primary care provider, and approximately one-quarter are enrolled with a provider who works in an interprofessional Family Health Team. Family Health Teams include mental health professionals Health Teams include mental health professionals such as social workers, psychologists, and a variety of other professionals practitioners and pharmacists. Factors associated with having a mood disorder such as perceived general health, mental health, and sense of belonging were ascertained from the CCHS. Detailed descriptions of measures used are listed in Supplemental Table 1B.
Analysis 3: Consequences of Mood Disorders
Finally, we conducted a longitudinal assessment of health service utilization, long-term care placement, and mortality associated with mood disorders. Each individual was followed until 5 years after the index interview date. Main outcomes investigated included general and mental health–related emergency department visits, general and mental health–related hospitalizations, admission to long-term care, and death. Other outcomes included visits to a psychiatrist, new antidepressant use, and homecare use. Outcome data were ascertained through linked administrative databases including Ontario’s health care registry, physician claims, and hospital and emergency department discharge abstracts (Supplemental Table 1A).
Statistical Analysis
We used cross-tabulations to quantify the prevalence of potential risk factors by sex and mood disorder status. Population sizes were reported as an average of the 4 cycles pooled to provide a more accurate estimate of the actual population between the years 2005 and 2012. To quantify crude associations between potential risk factors and mood disorder, bivariate logistic regression was initially performed. Stratified and nonstratified multivariable logistic regressions were then performed in an exploratory analysis to adjust for confounding in males and females. Four models were constructed, each adding covariates to build on the previous model. Observations with missing values of included variables were excluded for the regression analysis, with the exception of alcohol consumption which had a very high proportion of missing responses, and therefore, a category for missing responses was added.
Model 1 included age category and sex; Model 2 included Model 1 variables plus immigration status, level of education, income quintile, and food security; Model 3 included Model 2 variables plus chronic opioid use, smoking status, and alcohol consumption; Model 4 included Model 3 variables plus the number of Johns Hopkins ADGs.
Associations between mood disorder and health care use, long-term care placement, and mortality were also investigated. Crude bivariate logistic regression was performed along with multivariable models constructed with the same covariates and in the same fashion as for potential risk factors.
All estimates and confidence limits reported were quantified using sample weights provided by Statistics Canada. To account for the complex design of the CCHS, bootstrap sampling weights were applied using balanced repeated replication. The “pooled approach” of combining multiple CCHS cycles was used to increase sample size for regression analyses.13 Estimates with coefficients of variation between 16.6% and 33.3% were flagged with a note of caution due to potentially high levels of error. Cells including estimates with coefficients of variations >33.3% were suppressed due to unreliability. We performed all analyses using SAS statistical software (SAS Enterprise Guide version 7.1, SAS Institute, Cary, NC).
Ethics Approval
ICES is a prescribed entity under section 45 of Ontario’s Personal Health Information Protection Act. Section 45 authorizes ICES to collect personal health information, without consent, for the purpose of analysis or compiling statistical information with respect to the management of, evaluation or monitoring of, the allocation of resources to or planning for all or part of the health system. Projects conducted under section 45, by definition, do not require review by a Research Ethics Board. This project was conducted under section 45 and approved by ICES’ Privacy and Legal Office. The Sunnybrook Health Sciences Centre Research Ethics Board (REB) acts as the REB of record for some ICES studies, and it has determined that studies that fall under section 45 do not require REB review and approval.
Results
The average weighted population of the pooled cycles consisted of 1,643,203 individuals, representing the average of the annual eligible population through the years 2005 to 2012. Baseline characteristics of the population are detailed in Table 1. Females predominated, accounting for 55% of the total population. The highest proportion of individuals were in the youngest age category, with the smallest proportion in the oldest (57.4% aged 65 to 74 and 8.2% aged 85 or older). A higher proportion of males were married (80.8%) compared to females (51.7%), with a substantially lower proportion of males living alone (15.2% vs. 35.2%). There were low overall proportions of both food insecurity (2.7%) and chronic opioid use (3.7%), though both were slightly higher among females compared to males.
Table 1.
Weighted Population Characteristics, Canadian Community Health Survey, 2005, 2007, 2009, and 2011 Cycles for Those Aged 65 or Older.
| Male (n = 738,785) | Female (n = 904,418) | Total (n = 1,643,203) | |
|---|---|---|---|
| Age category | |||
| 65 to 74 | 444,958 (60.2) | 498,448 (55.1) | 943,405 (57.4) |
| 75 to 84 | 244,959 (33.2) | 319,693 (35.4) | 564,651 (34.4) |
| 85 or older | 48,868 (6.6) | 86,278 (9.5) | 135,146 (8.2) |
| Immigrant | 301,370 (40.8) | 342,336 (37.9) | 643,707 (39.2) |
| Marital status | |||
| Married/common-law | 597,117 (80.8) | 468,012 (51.7) | 1,065,129 (64.8) |
| Widowed | 74,561 (10.1) | 326,526 (36.1) | 401,087 (24.4) |
| Other | 67,107 (9.1) | 109,880 (12.1) | 176,987 (10.8) |
| Living arrangement | |||
| Lives alone | 112,151 (15.2) | 318,242 (35.2) | 430,393 (26.2) |
| Income quintile | |||
| 1 (lowest) | 121,499 (16.4) | 179,527 (19.9) | 301,026 (18.3) |
| 2 | 146,736 (19.9) | 187,222 (20.7) | 33,958 (20.3) |
| 3 | 148,070 (20.0) | 173,557 (19.2) | 321,627 (19.6) |
| 4 | 152,644 (20.7) | 184,400 (20.4) | 337,044 (20.5) |
| 5 (highest) | 168,308 (22.8) | 178,037 (19.7) | 346,345 (21.1) |
| Level of education | |||
| Secondary school or less | 309,410 (41.9) | 496,331 (54.9) | 805,741 (49.0) |
| Some postsecondary education | 38,180 (5.2) | 41,675 (4.6) | 79,856 (4.9) |
| Postsecondary degree/diploma | 381,564 (51.6) | 356,420 (39.4) | 737,983 (44.9) |
| Food security | |||
| Sometimes or often insecure | 44,130 (2.1) | 28,484 (3.1) | 44,130 (2.7) |
| Smoker | 72,224 (9.8) | 82,204 (9.1) | 154,427 (9.4) |
| Average Daily Alcohol Consumption, median (IQR); mean (SD) | 0 (0 to 0.75); 0.77 (0.09) | 0 (0 to 0.12); 0.35 (0.05) | 0 (0 to 0.5); 0.56 (0.05) |
| Alcohol consumption | |||
| Less than weekly | 178,854 (24.2) | 293,218 (32.4) | 472,072 (28.7) |
| 1 to 6 times weekly | 202,389 (27.4) | 168,384 (18.6) | 370,773 (22.6) |
| Everyday | 177,140 (24.0) | 102,271 (11.3) | 269,412 (17.0) |
| Any opioid user | 161,334 (21.8) | 208,009 (23.0) | 369,342 (22.5) |
| Chronic opioid user | 21,366 (2.9) | 39,520 (4.4) | 60,886 (3.7) |
| JH ADG (comorbidity) | |||
| No/low scores (0 to 4) | 190,385 (25.8) | 222,359 (24.6) | 412,744 (25.1) |
| Moderate scores (5 to 9) | 359,156 (48.6) | 441,395 (48.8) | 800,551 (48.7) |
| High scores (≥10) | 189,244 (25.6) | 240,664 (26.6) | 429,907 (26.2) |
| Continuity of care | |||
| Low | 187,081 (25.3) | 227,861 (25.2) | 1,659,764 (25.3) |
| Moderate | 58,150 (7.9) | 83,482 (9.2) | 566,528 (8.6) |
| High | 379,446 (51.4) | 476,842 (52.7) | 3,425,151 (52.1) |
| Enrollment in primary care model | 528,755 (72.3) | 669,814 (74.7) | 1,198,569 (73.6) |
| Enrollment in FHT | 118,855 (16.1) | 147,374 (16.3) | 266,229 (16.2) |
Note. Includes individuals who did not respond yes or no to having a diagnosed mood disorder. Results represent an average of the actual Ontario population between 2005 and 2012. Column percentages may not sum to 100% due to missing values. IQR = interquartile range; SD = standard deviation; JH ADG = Johns Hopkins Adjusted Diagnosis Group; FHT = Family Health Team.
A total of 100,174 individuals endorsed having a diagnosed mood disorder, with an overall prevalence of 6.1%. Stratified analyses indicated a higher prevalence of mood disorder in late life among females (7.1%) compared to males (4.9%). The overall prevalence of mood disorder decreased with increasing age, with a prevalence of 6.9% in those aged 65 to 74, 5.2% in those aged 75 to 84, and 4.2% in those aged 85 or older.
Baseline frequencies of potential risk factors based on mood disorder status are detailed in Table 2. The proportion of individuals with mood disorders was higher in females for all potential risk factor categories. A higher proportion of individuals with mood disorders was observed in nonimmigrants, those separated, divorced, or single, and those living alone. A slight drop in the proportion of individuals with mood disorders was observed in the highest household income quintile. The proportion of individuals with mood disorders was almost 3-fold higher among those with food insecurity compared to those without insecurity (14.8% vs. 5.9%). A relationship of similar magnitude was observed among chronic opioid users compared with nonchronic users (16.2% vs. 5.7%). The percentage of individuals with mood disorders increased with increasing levels of comorbidities, ranging from 3.8% with 0 to 4 Johns Hopkins ADGs to 8.9% in those with 10 or more ADGs.
Table 2.
Weighted Frequencies Percent with Mood Disorder Based on Potential Risk Factors of Mood Disorder, Canadian Community Health Survey, 2005, 2007, 2009, and 2011 Cycles for Those Aged 65 or Older.
| Percent with Mood Disorder, n (%) | |||
|---|---|---|---|
| Male (n = 737,774) | Female (n = 901,946) | Total (n = 1,639,720) | |
| Total with mood disorder | 36,029 (4.9) | 64,145 (7.1) | 100,174 (6.1) |
| Age category | |||
| 65 to 74 | 24,219 (5.4) | 40,676 (8.2) | 64,896 (6.9) |
| 75 to 84 | 10,123 (4.1) | 19,529 (6.1) | 29,652 (5.3) |
| 85 or older | 1,687 (3.5)a | 3,940 (4.6)a | 5,627 (4.2) |
| Immigration status | |||
| Nonimmigrant | 22,034 (5.0) | 42,294 (7.5) | 64,328 (6.4) |
| Immigrant | 12,995 (4.7) | 21,851 (6.4) | 35,846 (5.6) |
| Marital status | |||
| Married/common-law | 27,366 (4.6) | 30,771 (6.6) | 58,137 (5.5) |
| Widowed | 3,100 (4.2) | 21,818 (6.7) | 24,919 (6.2) |
| Separated/divorced/single | 5,516 (8.3) | 11,529 (10.6) | 17,044 (9.7) |
| Living arrangement | |||
| Lives alone | 7,067 (6.3) | 25,696 (8.1) | 32,763 (7.6) |
| Lives with others | 28,962 (4.6) | 38,143 (6.5) | 67,105 (5.6) |
| Income quintile | |||
| 1 (lowest) | 5,869 (4.8) | 13,647 (7.7) | 19,516 (6.5) |
| 2 | 6,781 (4.6) | 14,353 (7.7) | 21,134 (6.3) |
| 3 | 7,250 (4.9)a | 12,554 (7.2) | 19,803 (6.2) |
| 4 | 8,124 (5.3) | 14,044 (7.6) | 22,168 (6.6) |
| 5 (highest) | 7,810 (4.6) | 9,524 (5.4) | 17,335 (5.0) |
| Level of education | |||
| Secondary school or less | 13,566 (4.4) | 35,193 (7.1) | 48,759 (6.1) |
| Some postsecondary education | 1,731 (4.5)a | 3,070 (7.4)a | 4,802 (6.0) |
| Postsecondary degree/diploma | 20,135 (5.3) | 24,818 (7.0) | 44,953 (6.1) |
| Food security | |||
| Secure | 33,686 (4.7) | 59,373 (6.8) | 93,059 (5.9) |
| Sometimes or often insecure | 2,100 (13.4)a | 4,447 (15.6)a | 6,547 (14.8) |
| Smoking Status | |||
| Nonsmoker | 28,513 (4.3) | 54,835 (6.7) | 83,348 (5.6) |
| Smoker | 7,516 (10.4) | 9,310 (11.3) | 16,826 (10.9) |
| Alcohol consumption | |||
| Less than weekly | 8,561 (4.8) | 19,523 (6.7) | 28,084 (6.0) |
| 1 to 6 times weekly | 8,127 (4.0) | 9,610 (5.7) | 17,737 (4.8) |
| Everyday | 7,048 (4.0) | 5,656 (5.5) | 12,704 (4.6) |
| Any opioid user | |||
| No | 25,497 (4.4) | 44,000 (6.3) | 69,497 (5.5) |
| Yes | 10,532 (6.5) | 20,145 (9.7) | 30,677 (8.3) |
| Chronic opioid user | |||
| No | 33,026 (4.6) | 57,274 (6.6) | 90,300 (5.7) |
| Yes | 3,003 (14.1) | 6,870 (17.4) | 9,874 (16.2) |
| JH ADGs (comorbidity) | |||
| No/low scores (0 to 4) | 5,305 (2.8)a | 10,415 (4.7) | 15,720 (3.8) |
| Moderate scores (5 to 9) | 16,646 (4.6) | 29,639 (6.7) | 46,285 (5.8) |
| High scores (≥10) | 14,078 (7.5) | 24,092 (10.1) | 38,169 (8.9) |
| Continuity of care | |||
| Low | 9,852 (5.3) | 15,876 (7.0) | 25,727 (6.2) |
| Moderate | 3,340 (5.7) | 5,907 (7.1) | 9,247 (6.5) |
| High | 18,054 (4.8) | 34,725 (7.3) | 52,778 (6.2) |
| Enrollment in primary care model | |||
| Yes | 26,928 (5.1) | 49,190 (7.4) | 76,118 (6.4) |
| No | 8,691 (4.3) | 14,383 (6.3) | 23,074 (5.4) |
| Enrollment in FHT | |||
| Yes | 6,068 (5.1) | 12,157 (8.3) | 18,224 (6.9) |
| No | 29,961 (4.8) | 51,988 (6.9) | 81,950 (6.0) |
Note. JH ADG = Johns Hopkins Adjusted Diagnostic Group, FHT = Family Health Team.
a Values are reported with caution as per Statistics Canada guidelines (“Estimates with coefficients of variation between 16.6% and 33.3% should be accompanied by a warning to caution users about the high levels of error. Estimates with coefficients of variation higher than 33.3% are deemed to be unreliable”).
Overall, 3.4% of the cohort had a psychiatrist visit in the 2 years prior to the index interview. Forty percent of individuals with a psychiatry visit reported a diagnosed mood disorder. Seventeen percent of the cohort was using an antidepressant at any point 2 years prior to the interview. Of these, 23.7% reported a diagnosed mood disorder. The proportion of individuals with mood disorders increased with decreasing perceived general and mental health in both males and females. Approximately 12% of those with poor/fair general health had mood disorders compared to 3.1% in those with self-perceived health of very good/excellent. Twenty-seven percent of those with poor/fair mental health had mood disorders compared to 3.2% in those with a self-rating of very good/excellent. Individuals with a stronger sense of belonging were less likely to have mood disorders (4.6% in those with strong/somewhat strong sense of belonging vs. 8.6% somewhat weak/very weak sense of belonging).
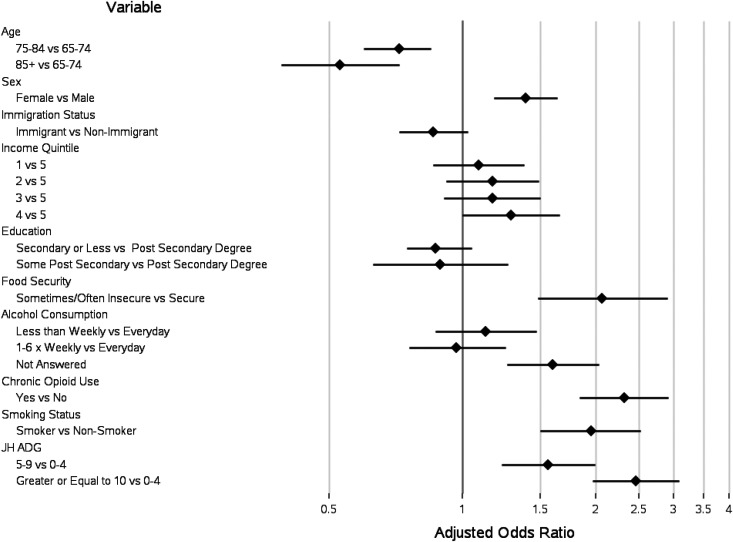
Figure 1 presents results of the completely adjusted regression analysis to quantify associations between potential risk factors and mood disorder (Model 4). Detailed results of all regression analyses are detailed in Supplemental Tables 2A and 2B. Statistically significant correlates of mood disorder in the final adjusted model were age category (odds ratio [OR] 75 to 84 = 0.72; 95% confidence interval [CI], 0.60 to 0.85; OR 85+ = 0.53 95% CI, 0.39 to 0.72), female sex (OR = 1.39; 95% CI, 1.18 to 1.64), the fourth income quintile (OR = 1.29; 95% CI, 1.00 to 1.66), food insecurity (OR = 2.07; 95% CI, 1.48 to 2.90), chronic opioid use (OR = 2.32; 95% CI, 1.84 to 2.92), smoking (OR = 1.95; 95% CI, 1.50 to 2.52), and increased levels of comorbidities (5 to 9 ADGs OR = 1.56; 95% CI, 1.23 to 1.99; >10 ADGs OR = 2.46; 95% CI, 1.97 to 3.08).
Figure 1.
Adjusted weighted associations between potential risk factors and mood disorder, Canadian Community Health Survey, 2005, 2007, 2009, and 2011 cycles for those aged 65 or older. JH ADG = Johns Hopkins Adjusted Diagnostic Group.
Health care service use of the population 5 years post index interview date is detailed in Table 3. Males and females were similar regarding general health services use although a higher percentage of females were admitted to long-term care (4.4% vs. 6.7%) and had new antidepressant use (22.3% vs. 34.8%). The proportion of individuals with a mood disorder using health care services was higher compared to the proportion among individuals without a mood disorder. For example, 47.5% of individuals with a mood disorder were hospitalized compared to 35.6% of individuals without and 53.0% of individuals with a mood disorder required homecare services compared to 37.8% among those who did not.
Table 3.
Cumulative Health Service Utilization by Mood Disorder Status 5 Years Post Index Interview Date, Canadian Community Health Survey, 2005, 2007, 2009, and 2011 Cycles for Those Aged 65 or Older.
| Male | Female | Total | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Mood Disorder | No Mood Disorder | Total | Mood Disorder | No Mood Disorder | Total | Mood Disorder | No Mood Disorder | Total | |
| General emergency department visit, n (%) | 29,243 (81.2) | 502,885 (71.7) | 532,128 (72.1) | 51,969 (81.0) | 593,415 (70.8) | 645,384 (71.6) | 81,212 (81.1) | 1,096,301 (71.2) | 1,177,513 (71.8) |
| Frequency of general emergency department visits, median (IQR) | 1.86 (0.29 to 5.25) | 0.99 (0 to 3.18) | 1.02 (0 to 3.27) | 1.82 (0.31 to 4.52) | 1.04 (0 to 3.23) | 1.09 (0 to 3.34) | 1.83 (0.30 to 4.78) | 1.02 (0 to 3.21) | 1.06 (0 to 3.31) |
| Frequency of general emergency department visits, mean (SD) | 3.98 (0.28) | 2.76 (0.05) | 2.82 (0.05) | 3.91 (0.24) | 2.82 (0.06) | 2.90 (0.06) | 3.93 (0.19) | 2.79 (0.04) | 2.86 (0.04) |
| Mental health-related emergency department visit, n (%) | 2,705 (7.5) | 17,188 (2.4) | 19,893 (2.7) | 7,161 (11.2) | 27,183 (3.2) | 34,344 (3.8) | 9,866 (9.8) | 44,370 (2.9) | 54,237 (3.3) |
| General hospitalizations, n (%) | 17,686 (49.1) | 260,323 (37.1) | 278,009 (37.7) | 29,896 (46.6) | 287,797 (34.4) | 317,693 (35.2) | 47,582 (47.5) | 548,120 (35.6) | 595,702 (36.3) |
| Frequency of general hospitalizations, median (IQR) | 0 (0 to 0.98) | 0 (0 to 0.62) | 0 (0 to 0.64) | 0 (0 to 0.83) | 0 (0 to 0.53) | 0 (0 to 0.56) | 0 (0 to 0.88) | 0 (0 to 0.57) | 0 (0 to 0.60) |
| Frequency of general hospitalizations, mean (SD) | 1.12 (0.1) | 0.76 (0.02) | 0.78 (0.02) | 0.94 (0.05) | 0.75 (0.03) | 0.76 (0.03) | 1.00 (0.05) | 0.75 (0.02) | 0.77 (0.02) |
| Mental health-related hospitalizations, n (%) | 1,843 (5.1) | 14,670 (2.1) | 16,513 (2.2) | 4,101 (6.4) | 16,083 (1.9) | 20,184 (2.2) | 5,944 (5.9) | 30,753 (2.0) | 36,697 (2.2) |
| Admission to long-term care, n (%) | 3,244 (9.0) | 29,194 (4.2) | 32,438 (4.4) | 8,048 (12.5) | 52,635 (6.3) | 60,683 (6.7) | 11,293 (11.3) | 81,828 (5.3) | 93,121 (5.7) |
| Death, n (%) | 8,443 (23.4) | 113,241 (16.1) | 121,684 (16.5) | 10,410 (16.2) | 107,083 (12.8) | 117,493 (13.0) | 18,853 (18.8) | 220,324 (14.3) | 239,177 (14.6) |
| Homecare use, n (%) | 18,780 (52.1) | 251,385 (35.8) | 270,166 (36.6) | 34,273 (53.4) | 330,413 (39.4) | 364,685 (40.4) | 53,053 (53.0) | 581,798 (37.8) | 634,851 (38.7) |
| Psychiatrist visit, n (%) | 10,048 (27.9) | 41,886 (6.0) | 51,934 (7.0) | 18,860 (29.4) | 46,621 (5.6) | 65,481 (7.3) | 28,908 (28.9) | 88,507 (5.7) | 117,415 (7.2) |
| Frequency of psychiatry visits, median (IQR) | 0 (0 to 0.86) | 0 (0 to 0) | 0 (0 to 0) | 0 (0 to 0.67) | 0 (0 to 0) | 0 (0 to 0) | 0 (0 to 0.71) | 0 (0 to 0) | 0 (0 to 0) |
| Frequency of psychiatry visits, mean (SD) | 4.42 (0.77) | 0.52 (0.09) | 0.71 (0.1) | 5.56 (0.89) | 0.64 (0.16) | 0.99 (0.16) | 5.15 (0.63) | 0.58 (0.1) | 0.86 (0.1) |
| New antidepressant use | 24,328 (67.5) | 139,849 (19.9) | 164,177 (22.3) | 52,565 (81.9) | 261,524 (31.2) | 314,089 (34.8) | 76,893 (76.8) | 401,373 (26.1) | 478,266 (29.2) |
Note. IQR = interquartile range, SD = standard deviation, JH ADG = Johns Hopkins Adjusted Diagnostic Group, FHT = Family Health Team.
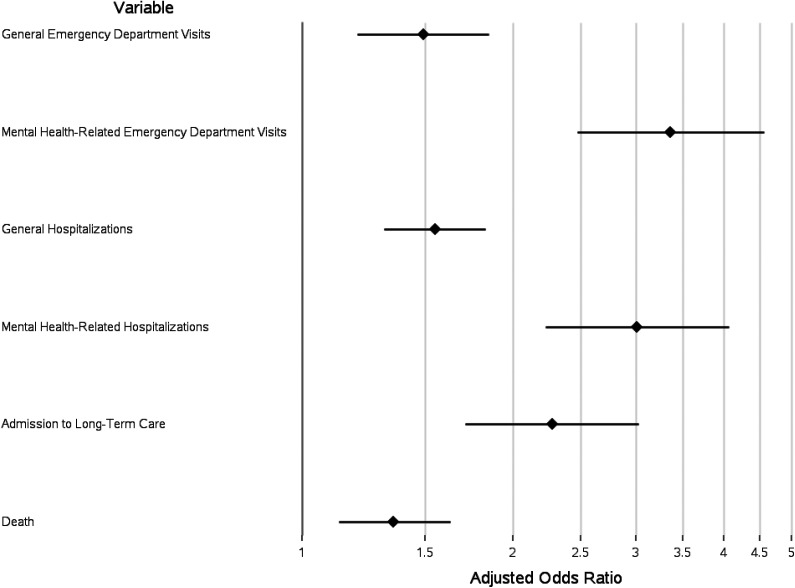
Adjusted logistic regression results quantifying associations between mood disorder and 5-year outcomes are presented in Figure 2. Detailed results of all health service–related regression analyses are detailed in Supplemental Tables 3A and 3B. Individuals with a mood disorder had increased odds of having all outcomes, with all estimates statistically significant in the adjusted models. The strongest associations with having a mood disorder were mental health–related emergency visits (OR = 3.36; 95% CI, 2.47 to 4.56) and mental health–related hospitalizations (OR = 3.01; 95% CI, 2.23 to 4.07). Individuals with a mood disorder had over twice the odds of being admitted to long-term care (OR = 2.28; 95% CI, 1.71 to 3.02) as well as an increased odds of dying compared to individuals without a mood disorder (OR = 1.35; 95% CI, 1.13 to 1.63).
Figure 2.
Adjusted weighted associations between mood disorder and health service utilization outcomes.
Discussion
We report findings of self-reported, diagnosed mood disorders from a population-based analysis in late life in community-dwelling adults living in Ontario, Canada. We found a prevalence of 7.1% among females and 4.9% among males, and the occurrence of a mood disorder was substantially higher in females for all potential risk factors. Statistically significant correlates of mood disorders included age, sex, food insecurity, smoking, chronic opioid use, and comorbidities. We also found that individuals in the second highest (4th) income quintile had higher odds of having a mood disorder in late life compared to those in the highest quintile. Strong associations between health service utilization and mood disorder suggest important consequences for individuals with mood disorders compared to those without.
Overall missingness among responses to survey questions was low, with the exception of alcohol consumption, where the proportion of missing responses was high among both males and females (45% and 37.7%, respectively). Interestingly, when missing was added as a category in regression analyses, we observed strong correlations with alcohol and mood disorder. It is possible that individuals not wishing to share their exposure to alcohol had higher consumption, potentially providing an explanation for this association.
The self-reported prevalence of mood disorders of 4.9% among males and 7.1% among females is higher than the previously reported 12-month prevalence of depression of approximately 1.4% among males and 1.8% among females based on the 2012 CCHS Mental Health Survey (using the World Health Organization Composite International Diagnostic Interview 3.0).14 In contrast, the prevalence of depression in older adults reported in other geographical areas has be reported to vary significantly from 0.4% in Japan to 35% in Hong Kong,15 and a recent systematic review reported a pooled prevalence estimate of 17.1%.16 Heterogeneity among studies is possibly due to different measures used to classify cases of depression. A self-reported measure of a mood disorder diagnosis was used in the present analysis and is likely more inclusive of milder depressive and bipolar spectrum disorders. Similar to others’ findings, we found a decrease in the prevalence of mood disorders with increasing age17,18 and a lower prevalence among males than females.
Some of the strongest correlates of mood disorders included food insecurity, chronic opioid use smoking, and comorbidities. Although food insecurity was infrequent, the odds of having a mood disorder were high, suggesting significant burden on the individual (more often among women due to an increased prevalence compared to males). The association between substance use and mood disorders is supported in previous literature for mood disorder19-21; however, with the cross-sectional nature of the data available, we are unable to determine the direction of these relationships. The burden of comorbidities is a well-known predictor of mood disorders, such as depression, in older adults, also supported by our findings.22 Individuals with mood disorders were higher users of health care services, consistent with previous findings.7 A systematic review reported similar results of higher service use among depressed individuals compared to those not depressed, including rates of hospitalization of 13% to 39% higher in depressed individuals.7 Between 5% and 37% of depressed individuals saw a psychiatrist compared to 0.2% to 1% among nondepressed individuals.7 Notably, we found strikingly high odds of adverse direct health-related outcomes such as admission to long-term care and death in depressed individuals, adjusted for numerous factors. This finding is in-line with previous literature reporting odds of death among depressed individuals to be 1.73 to 4 times higher compared to nondepressed older adults.23
Policy Implications
The data presented provide correlations between numerous socioeconomic, lifestyle, and behavioral factors and mood disorders, along with strong relationships with health care use, long-term care placement, and mortality. Therefore, we provide insight into opportunities for interventions to address mood disorders in late life and potentially prevent these adverse outcomes. Plausible interventions could be implemented in the form of secondary prevention (screening) and treatment options for individuals with mood disorders (such as depression), for example, a combination of psychotherapy and medication where appropriate.24,25 A study investigating team-based care for the screening and initial treatment of mood disorders in the primary care setting reported an improvement in the quality of care and reduction in aspects of health service utilization.26 Integrated care has been studied specifically in older adults, suggesting that these models of care can be effective in treating late-life depression.27 Although current Canadian guidelines do not advise screening of depression in the primary care setting, this recommendation is based on low-quality evidence.28 Other guidelines recommend screening when appropriate treatment and follow-up can be assured.29
Based on our findings, larger-scale interventions may focus on increased screening of females, those in younger age categories, and those with comorbidities. Other groups to potentially target for screening and treatment are those struggling with food insecurity and those using substances such as smokers and chronic opioid users.
Limitations
This analysis has limitations. We were restricted in the measure of mood disorders and potential risk factors due to the information provided by the CCHS. However, self-reported medical diagnoses as outcomes have been used previously and have been evaluated in other contexts with validity.30-32 Using this measure, however, may have resulted in some misclassification of individuals as having a mood disorder or not. Further, associations between exposures and mood disorders are based on cross-sectional data, and therefore, we cannot establish that risk factors preceded the outcome. We also did not account for the possibility that older adults were less likely to have certain outcomes due to mortality. Although we were unable to adjust for all important factors (e.g., changes in social network or functional capabilities), we present robust estimates adjusted for numerous important lifestyles and behavioral factors.
Conclusion
Mood disorders in late life remains a prominent public health concern, affecting at least 6.1% of older adults in Ontario. Knowledge of demographic, socioeconomic, and behavioral factors correlates among this population provide a basis for interventions to address this problem and potentially reduce its consequences including excessive health care use, long-term care placement, and mortality.
Supplemental Material
Supplementary_material for Mood Disorders in Late Life: A Population-based Analysis of Prevalence, Risk Factors, and Consequences in Community-dwelling Older Adults in Ontario by Rachel Strauss, Paul Kurdyak and Richard H. Glazier in The Canadian Journal of Psychiatry
Acknowledgments
The authors acknowledge the work of Mohammed Rashid in preparing the data used in this analysis.
Authors’ Note: The data set from this study is held securely in coded form at Institute for Clinical Evaluative Sciences (ICES). While data sharing agreements prohibit ICES from making the data set publicly available, access may be granted to those who meet prespecified criteria for confidential access, available at www.ices.on.ca/DAS. The full data set creation plan and underlying analytic code are available from the authors upon request, understanding that the computer programs may rely upon coding templates or macros that are unique to ICES and are therefore either inaccessible or may require modification. Parts of this material are based on data and/or information compiled and provided by the Canadian Institute for Health Information (CIHI). However, the analyses, conclusions, opinions and statements expressed in the material are those of the author(s) and not necessarily those of CIHI. Parts of this material are based on data and information provided by Cancer Care Ontario (CCO). The opinions, results, view, and conclusions reported in this paper are those of the authors and do not necessarily reflect those of CCO. No endorsement by CCO is intended or should be inferred.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Richard Glazier was supported as a clinician scientist by the Department of Family and Community Medicine at St. Michael’s Hospital and at the University of Toronto. This project was funded by the Canadian Institutes of Health Research, Funding Reference Number SOP 162622. This study was supported by the Institute for Clinical Evaluative Sciences (ICES), which is funded by an annual grant from the Ontario Ministry of Health and Long-Term Care (MOHLTC).
ORCID iDs: Rachel Strauss, BSc(Hons)  https://orcid.org/0000-0002-9460-4299
https://orcid.org/0000-0002-9460-4299
Paul Kurdyak, MD, PhD  https://orcid.org/0000-0001-8115-7437
https://orcid.org/0000-0001-8115-7437
Supplemental Material: The supplemental material for this article is available online.
References
- 1. Unutzer J, Patrick DL, Diehr P, Simon G, Grembowski D, Katon W. Quality adjusted life years in older adults with depressive symptoms and chronic medical disorders. Int Psychogeriatr. 2000;12(1):15–33. [DOI] [PubMed] [Google Scholar]
- 2. Population Reference Bureau. 2018 world population data sheet with focus on changing age structures. 2019. [accessed May 13, 2020] https://www.prb.org/2018-world-population-data-sheet-with-focus-on-changing-age-structures/.
- 3. Kingston A, Comas-Herrera A, Jagger C. Forecasting the care needs of the older population in England over the next 20 years: estimates from the population ageing and care simulation (PACSim) modelling study. Lancet Public Health. 2018;3(9): e447–e455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Aging with Confidence: Ontario’s Action Plan for Seniors. Government of Ontario; 2017. [accessed May 13, 2020] https://files.ontario.ca/ontarios_seniors_strategy_2017.pdf.
- 5. Ostbye T, Kristjansson B, Hill G, Newman SC, Brouwer RN, McDowell I. Prevalence and predictors of depression in elderly Canadians: the Canadian study of health and aging. Chronic Dis Can. 2005;26(4):93–99. [PubMed] [Google Scholar]
- 6. Bock JO, Luppa M, Brettschneider C, et al. Impact of depression on health care utilization and costs among multimorbid patients—from the multicare cohort study. PLoS One. 2014;9(3):e91973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Luppa M, Sikorski C, Motzek T, Konnopka A, Konig HH, Riedel-Heller SG. Health service utilization and costs of depressive symptoms in late life—a systematic review. Curr Pharm Des. 2012;18(36):5936–5957. [DOI] [PubMed] [Google Scholar]
- 8. Chiu M, Lebenbaum M, Cheng J, de Oliveira C, Kurdyak P. The direct healthcare costs associated with psychological distress and major depression: a population-based cohort study in Ontario, Canada. PLoS One. 2017;12(9):e0184268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Census Profile, 2016 Census. Statistics Canada. 2019. [accessed May 13, 2020]. https://www12.statcan.gc.ca/census-recensement/2016/dp-pd/prof/details/page.cfm?&Geo1=PR&Code1=35&Geo2=PR&Code2=01&Data=Count&SearchText=ontario&SearchType=Begins&SearchPR=01&B1=All&TABID=1
- 10. Canadian Community Health Survey—Annual Component. Statistics Canada. 2018. [accessed May 13, 2020]. http://www23.statcan.gc.ca/imdb/p2SV.pl?Function=getSurvey&SDDS=3226.
- 11. Canadian Community Health Survey (CCHS): Questionnaire for Cycle 3.1—June 2005. Statistics Canada. 2012. [accessed May 13, 2020]. http://www23.statcan.gc.ca/imdb/p3Instr.pl?Function=getInstrumentList&Item_Id=33185&UL=1V&
- 12. The Johns Hopkins ACG System. The Johns Hopkins University. 2019. [accessed May 13, 2020]. https://www.hopkinsacg.org.
- 13. Thomas S, Wannell B. Combining cycles of the Canadian Community Health Survey Statistics Canada. 2015. [accessed May 13, 2020]. https://www150.statcan.gc.ca/n1/pub/82-003-x/2009001/article/10795/findings-resultats-eng.htm. [PubMed]
- 14. Statistics Canada. Health at a glance: mental and substance use disorders in Canada. 2015. [accessed May 13, 2020] https://www150.statcan.gc.ca/n1/pub/82-624-x/2013001/article/11855-eng.htm#a9.
- 15. Beekman AT, Copeland JR, Prince MJ. Review of community prevalence of depression in later life. Br J Psychiatry. 1999;174:307–311. [DOI] [PubMed] [Google Scholar]
- 16. Luppa M, Sikorski C, Luck T, et al. Age- and gender-specific prevalence of depression in latest-life—systematic review and meta-analysis. J Affect Disord. 2012;136(3):212–221. [DOI] [PubMed] [Google Scholar]
- 17. Streiner DL, Cairney J, Veldhuizen S. The epidemiology of psychological problems in the elderly. Can J Psychiatry. 2006;51(3):185–191. [DOI] [PubMed] [Google Scholar]
- 18. Patten SB, Williams JV, Lavorato DH, Wang JL, McDonald K, Bulloch AG. Descriptive epidemiology of major depressive disorder in Canada in 2012. Can J Psychiatry. 2015;60(1):23–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Yun WJ, Shin MH, Kweon SS, Ryu SY, Rhee JA. Association of smoking status, cumulative smoking, duration of smoking cessation, age of starting smoking, and depression in Korean adults. BMC Public Health. 2012;12:724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Scherrer JF, Salas J, Copeland LA, et al. Increased risk of depression recurrence after initiation of prescription opioids in noncancer pain patients. J Pain. 2016;17(4):473–482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Scherrer JF, Salas J, Sullivan MD, et al. The influence of prescription opioid use duration and dose on development of treatment resistant depression. Prev Med. 2016;91:110–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Voinov B, Richie WD, Bailey RK. Depression and chronic diseases: it is time for a synergistic mental health and primary care approach. Prim Care Companion CNS Disord. 2013;15(2):8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Blazer DG. Depression in late life: review and commentary. J Gerontol A Biol Sci Med Sci. 2003;58(3):249–265. [DOI] [PubMed] [Google Scholar]
- 24. Baldwin RC, Anderson D, Black S, et al. Guideline for the management of late-life depression in primary care. Int J Geriatr Psychiatry. 2003;18(9):829–838. [DOI] [PubMed] [Google Scholar]
- 25. National Guidelines for Seniors’ Mental Health. The assessment and treatment of depression. Markham (ON): Canadian Coalition for Seniors’ Mental Health; 2006. [Google Scholar]
- 26. Reiss-Brennan B, Brunisholz KD, Dredge C, et al. Association of integrated team-based care with health care quality, utilization, and cost. JAMA. 2016;316(8):826–834. [DOI] [PubMed] [Google Scholar]
- 27. Dham P, Colman S, Saperson K, et al. Collaborative care for psychiatric disorders in older adults: a systematic review. Can J Psychiatry. 2017;62(11):761–771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Joffres M, Jaramillo A, Dickinson J, et al. Recommendations on screening for depression in adults. CMAJ. 2013;185(9):775–782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Siu AL, Bibbins-Domingo K, Grossman DC, et al. Screening for depression in adults: US preventive services task force recommendation statement. JAMA. 2016;315(4):380–387. [DOI] [PubMed] [Google Scholar]
- 30. Fowles JB, Fowler EJ, Craft C. Validation of claims diagnoses and self-reported conditions compared with medical records for selected chronic diseases. J Ambul Care Manag. 1998;21(1):24–34. [DOI] [PubMed] [Google Scholar]
- 31. Sanchez-Villegas A, Schlatter J, Ortuno F, et al. Validity of a self-reported diagnosis of depression among participants in a cohort study using the Structured Clinical Interview for DSM-IV (SCID-I). BMC Psychiatry. 2008;8:43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Fan AZ, Strine TW, Huang Y, et al. Self-rated depression and physician-diagnosed depression and anxiety in Florida adults: Behavioral Risk Factor Surveillance System, 2006. Prev Chronic Dis. 2009;6(1):A10. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary_material for Mood Disorders in Late Life: A Population-based Analysis of Prevalence, Risk Factors, and Consequences in Community-dwelling Older Adults in Ontario by Rachel Strauss, Paul Kurdyak and Richard H. Glazier in The Canadian Journal of Psychiatry