Abstract
Background.
Physical activity exerts cancer-protective effects, yet most Americans are inactive, especially in the South, where cancer incidence rates are generally higher. Telephone-based approaches can help overcome physical activity intervention barriers in this region (literacy, costs, lack of transportation/technology, distance from facilities) and can be automated via interactive voice response (IVR) systems for improved reach and cost-effectiveness.
Aims.
To evaluate the Deep South IVR-supported Active Lifestyle (DIAL) intervention.
Method.
A pilot randomized controlled trial was conducted among 63 underactive adults in Birmingham, Alabama, from 2015 to 2017.
Results.
Retention was 88.9% at 12 weeks, and ≥75% adherence (IVR contact on at least 63 out of 84 days) was noted among 62.5% of intervention participants. Intervention participants reported larger increases in self-reported minutes of moderate-to-vigorous intensity physical activity from baseline to 12 weeks than the wait-list control arm (median change = 47.5 vs. 5.0 minutes, respectively, p = .09). Moreover, the intervention produced significantly greater increases in physical activity self-regulation (p < .001) and social support from family (p = .001) and friends (p = .009) from baseline to 12 weeks, compared with the wait-list control. Significant decreases in self-reported sleep disturbance also were found in the intervention arm but not among the controls, p < .05. Overall, intervention participants reported being satisfied with the DIAL program (71.4%) and would recommend it to friends (92.9%).
Discussion.
Findings support the feasibility, acceptability, and preliminary efficacy of the DIAL intervention.
Conclusion.
Next steps include intervention refinement in preparation for a fully powered efficacy trial and eventual dissemination to rural counties.
Keywords: cancer prevention, physical activity, telehealth
Cancer is a major public health concern in the United States. National data show that nearly 40% of Americans will be diagnosed with cancer during their lifetime (National Cancer Institute, 2017b). Regular physical activity is an established modifiable risk factor, with evidence suggesting the strongest relationship between high levels of physical activity and lower risk of colon, breast, and endometrial cancers (National Cancer Institute, 2017a). The role of physical activity in cancer prevention is recognized by the American Cancer Society (ACS) and reflected in their guidelines that adults engage in a minimum of 150 minutes of moderate-intensity or 75 minutes of vigorous-intensity physical activity per week to reduce cancer risk ( ACS, 2017).
Despite the benefits of physical activity, only half (i.e., 51%) of all Americans report meeting ACS guidelines (Centers for Disease Control and Prevention, 2017). Moreover, disparities emerge when examining physical activity profiles by geographical region. Residents of the Deep South (i.e., Alabama, Mississippi, Georgia, South Carolina, and Louisiana; Merriam-Webster, 2017) have the lowest activity levels, with prevalence data showing that only 38% to 50.5% of residents report meeting the ACS physical activity recommendations (Centers for Disease Control and Prevention, 2017). Such physical inactivity, along with other factors, likely contributes to the high cancer incidence rates found in this region (i.e., 462.1 per 100,000 persons vs. national average of 436.6 per 100,000 persons; U.S. Cancer Statistics Working Group, 2017). Low physical activity levels and disproportionate cancer burden among adults living in the Deep South call for effective interventions to promote physical activity and reduce cancer risk in this region.
The physical and demographic landscapes of the Deep South present unique barriers for researchers to consider when designing physical activity interventions for these populations. For example, many individuals in the South reside in rural areas (U.S. Department of Commerce, 2012) and often must travel substantial distances to access resources (e.g., doctor’s offices, community centers). Likewise, individuals living in the Southern United States have lower literacy levels (Kirsch, Jungeblut, Jenkins, & Kolstad, 2002) and technology access (i.e., computers, Internet) when compared with the U.S. population as a whole (Perrin, 2017; U.S. Census Bureau, 2014). Accordingly, when developing physical activity interventions for residents of these areas, researchers should recognize these characteristics and identify effective intervention strategies to overcome these potential barriers to physical activity intervention participation.
Thus, we adapted an existing interactive voice response (IVR) system to deliver social cognitive theory (SCT) based physical activity counseling and used extensive formative research (11 focus groups) on physical activity barriers and intervention preferences in the Deep South to help inform our efforts (Pekmezi et al., 2013). Telephone delivery of the intervention was selected because virtually all American households (i.e., 97%) have wireless or landline telephone service. Telehealth approaches can help overcome intervention delivery barriers related to literacy, technology access, transportation, long distances from clinics/centers, child care concerns, and work-related issues (Attwood, Morton, Mitchell, Van Emmenis, & Sutton, 2016; Ingram, Wilbur, McDevitt, & Buchholz, 2011; Martinez, Arredondo, Perez, & Baquero, 2009). Moreover, the automated IVR system requires fewer personnel and financial resources than traditional face-to-face interventions or even provider-based telephone counseling and thus has greater potential for widespread dissemination. The purpose of this study was to pilot a 12-week individually tailored, IVR-supported physical activity intervention for cancer prevention in the Deep South. Specific outcomes were to examine the feasibility, acceptability, and preliminary efficacy of the intervention to improve physical activity and related psychosocial variables.
Method
Design
The Deep South IVR-supported Active Lifestyle (DIAL) study was a randomized controlled feasibility trial of a 12-week IVR-supported physical activity intervention for cancer risk reduction compared with a wait-list control condition among 63 individuals living in the Deep South. Program adherence and retention were examined and participant satisfaction survey data were collected postintervention. Physical activity was assessed using the 7-Day Physical Activity Recall and via accelerometry at baseline and 12 weeks. Changes in related psychosocial outcomes also were assessed at these time points. The research design is discussed in detail in a prior report (Pekmezi, Ainsworth, Holly, et al., 2017).
Setting and Sample
Research activities for the DIAL study were conducted at the University of Alabama at Birmingham (UAB) Center for the Study of Community Health from 2015 to 2017. The trial received approval from the UAB Institutional Review Board and was registered with ClinicalTrials.gov (NCT02627235). Participants were mostly recruited via flyers on campus and local municipal buildings, community centers, and libraries in Birmingham, AL.
Adults (ages 21 years or older) who were underactive (reporting less than 60 min/week of moderate-intensity physical activity) and able to speak and read English were considered eligible. Participants also had to be willing to be assigned to either study condition, have access to a telephone, and not plan to move from the Birmingham, Alabama, area for at least 4 months. Cardiovascular and musculoskeletal risk factors were assessed using the Physical Activity Readiness Questionnaire (Canadian Society for Exercise Medicine, 1994). A history of heart disease, myocardial infarction, angina, stroke, body mass index (BMI) over 45, orthopedic conditions that limit mobility, or any serious medical condition that would make physical activity unsafe were grounds for ineligibility (see Figure 1).
Figure 1.
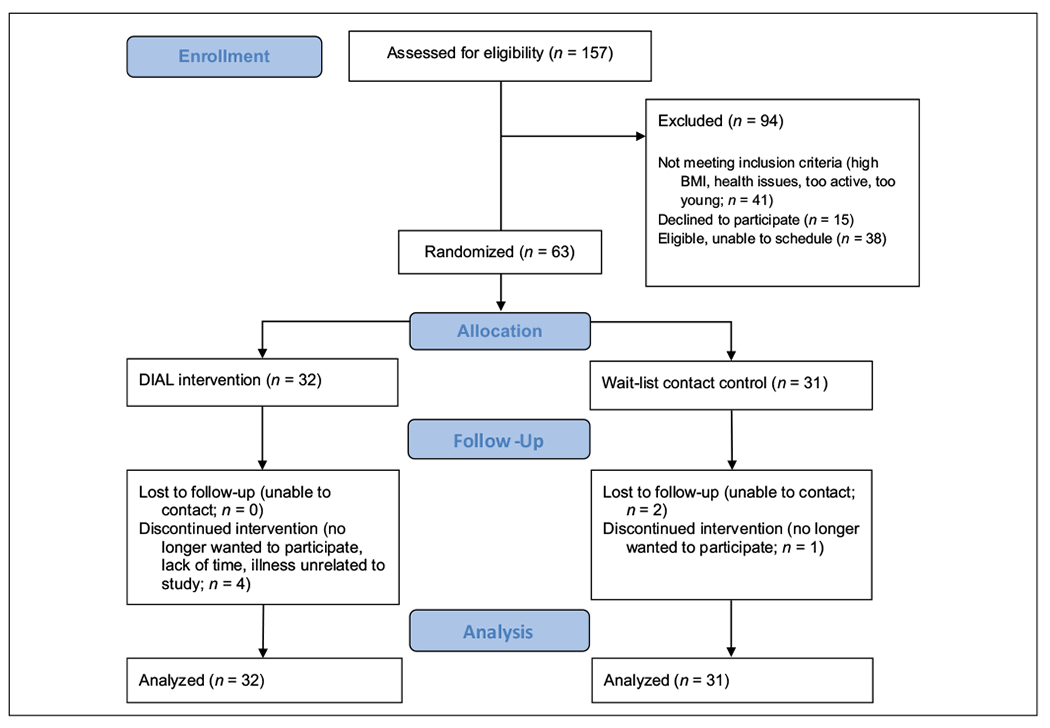
Study flow diagram.
Protocol
Once initial eligibility was established by phone, participants attended an orientation session to watch a video on the study protocol and complete the informed consent process with research staff. Physical activity and psychosocial variables were measured at the baseline assessment at the research center. Participants were then randomly assigned to either the DIAL intervention or wait-list control condition using a list of random numbers. Physical activity and psychosocial variables were reassessed at 12 weeks at the research center.
DIAL Intervention
Participants received AccuSplit AE120XL pedometers and education from research staff on intervention goals (gradually increasing moderate-to-vigorous aerobic physical activity until national physical activity guidelines are reached) and injury prevention (warm-ups, cool-downs, flexibility training). Then, the participants called the automated IVR system each day for 12 weeks to record steps and physical activity and receive feedback on progress via IVR and monthly mail-delivered graphic-based feedback reports. SCT served as the framework for this intervention (Bandura, 1986) and describes a dynamic ongoing process in which personal factors, environmental factors, and health behavior exert influence upon each other. Several key SCT constructs (self-regulation, self-efficacy, enjoyment, outcome expectations, social support) were directly targeted by the DIAL intervention (via daily self-monitoring IVR calls, 3-monthly SCT-based counseling IVR calls; see Table 1). Counseling modules addressing the physical activity barriers identified during formative research with the community (e.g., lack of time, negative outcome expectations, enjoyment, social support) were also available via IVR. See prior report (Pekmezi, Ainsworth, Holly, et al., 2017) for more details on the intervention.
Table 1.
Application of Social Cognitive Theory in DIAL Intervention.
| SCT construct | How SCT construct was targeted by DIAL intervention | Examples of relevant IVR counseling messages |
|---|---|---|
| Self-regulation | Tracked pedometer step counts and MVPA via daily IVR calls, received feedback on progress via IVR system and monthly graphic-based reports, along with monetary incentives for self-monitoring | “You are on your way to meeting the national guidelines. Keep up the good work. Consider leaving yourself reminders and finding a walking partner to help you reach that goal.” |
| Self-efficacy | Received individually tailored IVR-supported phone counseling at 4, 8, and 12 weeks | “You sound unsure about your ability to exercise, even more so than last time we spoke. Try squeezing in a 10-minute walk 1 or 2 days this week. Meeting this small goal will help you feel more sure that you can fit physical activity into your life.” |
| Social support | Received individually tailored IVR-supported phone counseling at 4, 8, and 12 weeks | “You have people in your life who support your efforts to be physically active. This can be very helpful. Ask them to remind you to walk or maybe even take a walk with you.” |
| Outcome expectations | Received individually tailored IVR-supported phone counseling at 4, 8, and 12 weeks | “You don’t expect much good to come from exercising, same as last time we talked. Physical activity can be energizing, improve your mood, and leave you feeling refreshed. Keep this in mind as you try to make physical activity a habit.” |
| Enjoyment | Received individually tailored IVR-supported phone counseling at 4, 8, and 12 weeks | “You enjoy physical activity, more so today than the last time we spoke. That’s great! Try exciting new activities like tai chi or kick boxing so it stays fun.” |
Note. SCT = social cognitive theory; DIAL = Deep South IVR-supported Active Lifestyle; IVR = interactive voice response; MPVA = moderate-to-vigorous physical activity.
Wait-List Control Condition
The wait-list control participants were instructed to maintain their normal routine until completion of the 12-week assessments. Then they were provided the same 12-week trial of the DIAL intervention and also completed postintervention 7-Day Physical Activity Recalls and participant satisfaction questionnaires.
Measures
Physical Activity and Anthropometric Measures.
Self-report moderate-to-vigorous physical activity minutes per week was assessed by the 7-Day Physical Activity Recall (PAR) at baseline and 12 weeks (Blair et al., 1985; Sallis et al., 1985). The PAR has previously shown reliability, internal consistency, and validity with objective activity measures (Hayden-Wade, Coleman, Sallis, & Armstrong, 2003; Irwin, Ainsworth, & Conway, 2001; Leenders, Sherman, Nagaraja, & Kien, 2001; Pereira et al., 1997; Sloane, Snyder, Demark-Wahnefried, Lobach, & Kraus, 2009; Wilkinson, Huang, Walker, Sterling, & Kim, 2004).
Participants also received ActiGraph GT3X accelerometers at orientation and wore them for 7 days before the baseline assessment. At 12 weeks, participants were mailed the devices and wore them for another 7 days. The accelerometers measure movement and intensity and have been validated with heart rate telemetry (Janz, 1994) and total energy expenditure (Melanson & Freedson, 1995). ActiLife software version 6.1 was used to validate and analyze bouts of activity, with a cut-point of 1,952 counts/minute selected as the minimum threshold for moderate-intensity activity (Freedson, Melanson, & Sirard, 1998). Moreover, a minimum valid wear time was set at 5 days of at least 600 minutes of wear or 3,000 minutes of wear over 4 days. Consistent with the physical activity data collected by the PAR (i.e., physical activity bouts of 10 minutes or more) and the focus of the national guidelines, only activity bouts ≥10 minutes were included in the estimation of total minutes/week of activity. These 10-minute activity bouts were defined as achieving the aforementioned cut-point for moderate-intensity activities or greater (i.e., >1,951 counts/minute) for at least 10 consecutive minutes, with allowance of 1 to 2 minutes below these thresholds during the 10-minute period (Troiano et al., 2008).
The 6-Minute Walk Test was performed at these same time points, to measure the distance the participants walked in a 6-minute period on a hard, flat surface (Butland, Pang, Gross, Woodcock, & Geddes, 1982; Cahalin, Pappagianopoulos, Prevost, Wain, & Ginns, 1995; Solway, Brooks, Lacasse, & Thomas, 2001) and to obtain objective data on physical performance. Height and weight were measured with a portable stadiometer (Seca 213, Chino, CA) and EatSmart Precision Plus digital bathroom scale (Taylor Precision Products Incorporation, Oak Brook, IL).
Psychosocial Variables.
At baseline, demographics were assessed by a questionnaire that included items related to age, gender, education, employment, income, marital status, race, and ethnicity.
Social cognitive theory constructs were assessed at baseline and 12-week assessments at the research center (along with the physical activity and anthropometric measures) and via IVR at weeks 4,8, and 12 to inform the individually tailored IVR-based physical activity counseling. Adherence in the current study was defined as completion of at least 2 of 3 monthly counseling calls, as well as recording physical activity via IVR on at least 63 days over the 12-week intervention period, that is, approximately 75% of the possible 84 daily calls. To promote and maintain adherence, participants received up to $43.25 for completing IVR calls (see prior report for further detail on incentives; Pekmezi, Ainsworth, Holly, et al, 2017), along with reminder emails and phone calls from staff when more than two consecutive days of IVR calls were missed. SCT surveys included 13 items on social support for physical activity participation from family and friends (α = .61-.91; Sallis, Grossman, Pinski, Patterson, & Nader, 1987), 9 items on outcome expectations (anticipated outcomes of physical activity; α = .89; Resnick, Zimmerman, Orwig, Furstenberg, & Magaziner, 2000), 18 items on physical activity enjoyment (α = .96; Resnick et al., 2000), and 5 items on self-efficacy (confidence in one’s ability to be physically active, despite barriers; α = .82; Kendzierski & DeCarlo, 1991). Moreover, self-regulation (tracking physical activity progress and setting goals) was measured using a 10-item scale with a reliability estimate, Cronbach’s α, of .78 (Anderson, Winett, Wojcik, & Williams, 2010).
Brief PROMIS® subscales on anxiety, depression, fatigue, and sleep disturbance, variables positively influenced by regular physical activity (U.S. Department of Health and Human Services, 2008), also were measured at baseline and 12 weeks (α = .83-.95; Cella et al., 2010). The raw sum scores were converted to T-scores for analyses, using conversion tables published on the PROMIS® web site (http://www.nihpromis.org/default.aspx).
Postintervention participant satisfaction with the program was assessed with an 18-item measure that the research team has used in several past studies (Pekmezi, Ainsworth, Holly, et al., 2017; Pekmezi, Ainsworth, Joseph, et al., 2017; Pekmezi et al. 2013).
Data Analyses
Participant characteristics, retention, adherence, and program satisfaction were summarized using descriptive statistics, including means and standard deviations for continuous variables. The physical activity variables had nonnormal distributions and summary statistics included medians and interquartile ranges (IQRs). Changes in moderate-to-vigorous physical activity were compared between treatment arms using a median test, and the within-group changes were compared with the sign test. Data were analyzed by intent-to-treat, and missing data points were imputed by carrying the baseline value forward. Potential intervention effects on weight, BMI, and psychosocial variables were explored using repeated-measures multivariate analyses of covariance and calculation of adjusted means and 95% confidence intervals (CIs). Sensitivity analyses were conducted within treatment arms stratifying by overall call adherence and monthly call adherence for predetermined cut-points. A sign test was conducted to examine changes in physical activity from 12 weeks to 24 weeks in the wait-list control arm and ascertain the replicability of intervention effects.
Results
Sample Characteristics
The sample included underactive adults. The mean age was 43 years old, and the mean BMI was over 30 kg/m2. A majority of the participants were male (55.6%) and African American (58.7%). Most reported at least some college level education (92%), full-time employment (63.5%), and household incomes less than $50,000 per year (61.9%). The intervention arm had significantly higher BMIs and were less likely to have children living at home than the control arm, but no other significant group differences in demographic, physical activity, or psychosocial variables were found at baseline. Demographic characteristics are further described in Table 2 and our prior report (Pekmezi, Ainsworth, Holly, et al., 2017).
Table 2.
Demographic Characteristics of DIAL Study Participants.
| Characteristics | Intervention (N = 32), M (SD) or % | Control (N = 31), M (SD) or % | Overall (N = 63), M (SD) or % |
|---|---|---|---|
| Age | 43.6 (11.7) | 42.4 (12.2) | 43.0 (11.8) |
| Male | 53.1% | 58.1% | 55.6% |
| Race | |||
| Black or African American | 65.6% | 51.6% | 58.7% |
| White | 28.1% | 38.7% | 33.3% |
| Asian | 3.1% | 9.7% | 6.3% |
| Other | 3.1% | 0.0% | 1.6% |
| More than or some college education | 93.9% | 90.3% | 92% |
| Full-time employment | 59.4% | 67.7% | 63.5% |
| Household annual income <50,000 | 56.2% | 67.7% | 61.9% |
| No children living at home* | 84.4% | 54.8% | 69.8% |
| BMI* | 33.2 (6.9) | 29.0 (6.4) | 31.1 (6.9) |
Note. DIAL = Deep South IVR-supported Active Lifestyle; BMI = body mass index.
p < .05 between groups.
Retention and Adherence
Overall, retention was high at 12 weeks (88.9%; 95% CI = [77.8, 95.0]) and did not differ by group. Most intervention participants (62.5%; 95% CI = [43.8, 78.3]) demonstrated adequate adherence by calling the IVR system on at least 63 days (≥75% of the 84 required days) and completing at least 2 of the 3 required monthly calls (78.1%). In fact, 19 participants completed all 3 monthly calls, 6 completed 2 of the 3 monthly calls, 3 completed a single monthly call, and another 4 did not complete any monthly calls.
Participant Satisfaction
Of the intervention participants who completed the participant satisfaction questionnaire (N = 14; 43.8%), most were “satisfied” or “very satisfied” with the DIAL program (71.4%) and would recommend it to a friend (92.9%). Participants reported wearing the provided pedometer often (92.9%) and calling in to the DIAL line at least a few times per week (92.3%). Moreover, participants found the DIAL line easy to use (85.7%).
Changes in Physical Activity From Baseline to 12 Weeks
DIAL intervention participants reported larger increases in minutes of moderate-to-vigorous intensity physical activity from baseline to 12 weeks than the control group (median change of 47.5 vs. 5 minutes/week, respectively), p = .09. However, accelerometer data indicated no significant changes within or between groups. Such a discrepancy in findings (and lack of significant correlation between objective and self-report findings) may be due to difficulty obtaining valid accelerometer data at 12-week assessments from over 52% of the sample.
Trends in the data indicated that adherence to intervention protocol resulted in greater physical activity. Intervention participants who called the IVR system for the required 84 days (N = 14) reported a median of 93.5 minutes/week of moderate-to-vigorous physical activity (IQR 40, 150) at 12 weeks, whereas those who called less than 84 days (N = 18) reported 75.0 minutes/week of moderate-to-vigorous physical activity (IQR 55, 150) at 12 weeks, p = .45. Intervention participants who completed the 3 required monthly counseling calls (N = 19) reported a median of 95.0 (IQR 45, 150) minutes/week of moderate-to-vigorous physical activity at 12 weeks and those who did not (N = 13) reported 60.0 (IQR 45, 160) minutes/week of moderate-to-vigorous physical activity at 12 weeks, p = .23.
There were no significant between group differences in changes in weight or 6 minute walk distance from baseline to 12 weeks (p > .05). However, trends in the data indicate non-significant increases in 6 minute walk distance at 12 weeks for the intervention arm (M = +7.1 meters, SD = 77.2) and decreases in control arm (M = −12.0, SD = 69.7), p = .65. See Table 3 for changes from baseline to 12 weeks in physical activity measures.
Table 3.
Changes in Physical Activity and Related Variables Between Baseline and 12 Weeks.
| Intervention (n = 32) |
Control (n = 31) |
||||||
|---|---|---|---|---|---|---|---|
| Variables | Baseline median (IQR) | 12-week median (IQR) | Change (IQR) | Baseline median (IQR) | 12-week median (IQR) | Change (IQR) | Between group p |
| Self-reported physical activity (moderate-to-vigorous minutes/week, 7-day PAR) | 25 (0, 45) | 60 (42.5, 147.5) | 47.5 (0, 91.5)* | 45 (0, 60) | 75 (12, 135) | 5 (0, 95)* | .09 |
| Accelerometer measured physical activity (moderate-to-vigorous minutes/week) | 10 (0, 40) | 12 (0, 34) | 0 (0, 0) | 1 3 (0, 47) | 10 (0, 39) | 0 (−10, 0) | .57 |
| Baseline mean (SD) | 12-week mean (SD) | Mean Change (SD) | Baseline mean (SD) | 12-week mean (SD) | Mean Change (SD) | Adjusted mean change between groups [95% CI] | |
| 6-minute walk test (meters) | 341.4 (68.9) | 355.7 (85.9) | 7.1 (77.2) | 362.1 (61.1) | 355.7 (57.8) | −12.0 (69.7) | −8.9 [−47.7, 29.9] |
| BMI (kg/m2) | 33.2 (7.0) | 34.2 (7.6) | 0.7 (1.9) | 29.0 (6.4) | 29.0 (6.1) | 0.2 (1.1) | −1.1 [−3.2, 1.0] |
| Weight (kg) | 91.2 (19.7) | 93.5 (22.0) | 1.9 (5.6) | 82.3 (18.3) | 82.5 (15.5) | 0.6 (3.3) | −0.4 [−1.2, 0.3] |
Note. IQR = interquartile range; PAR = physical activity recall; CI = confidence interval.
p < .05.
Changes in Physical Activity-Related Psychosocial Variables From Baseline to 12 Weeks
The intervention participants reported significantly greater improvements in physical activity self-regulation (M = 0.8, SD = 0.8 vs. M = −0.1, SD = 0.07; between group p < .001) and social support from family (M = 3.6, SD = 10 vs. M = −3.3, SD = 10.8; between group p = .001) and friends (M = 4.4, SD = 10.4 vs. M = −1.2, SD = 10.8; between group p = .009) from baseline to 12 weeks, compared to the wait-list control participants. A significant within group decrease in sleep disturbance from baseline to 12 weeks was also found in the intervention arm (M = −4.0, SD = 5.3, p < .001) and not the control arm. However, there were no significant changes in physical activity self-efficacy, enjoyment, outcome expectations, and the other PROMIS subscales (anxiety, depression, fatigue). See Table 4 for changes from baseline to 12 weeks in psychosocial measures.
Table 4.
Changes in Psychosocial Variables Between Baseline and 12 Week.
| Intervention (n = 32) |
Control (n = 31) |
||||||
|---|---|---|---|---|---|---|---|
| Variables | Baseline mean (SD) | 12-week mean (SD) | Mean change (SD) | Baseline mean (SD) | 12-week mean (SD) | Mean change (SD) | Between group p |
| Physical activity self-efficacy (range = 1-5) | 2.5 (0.9) | 2.7 (0.9) | 0.2 (0.5) | 2.3 (0.7) | 2.5 (0.8) | 0.2 (0.6) | .75 |
| Physical activity enjoyment (range = 18-126) | 92.2 (18.9) | 96.9 (20.0) | 3.5 (13.8) | 91.5 (21.3) | 89.0 (19.9) | −1.7 (17.7) | .16 |
| Physical activity self-regulation (range = 1-5) | 2.4 (0.6) | 3.1 (0.7) | 0.8 (0.8)* | 2.3 (0.7) | 2.1 (0.7) | −0.1 (0.7) | .0004 |
| Anxiety (range = 36.3-82.7) | 51.4 (11.0) | 48.5 (9.4) | −1.9 (7.3) | 50.4 (9.7) | 50.9 (8.7) | −0.6 (8.3) | .68 |
| Depression (range = 37.1-81.1) | 46.5 (10.6) | 42.5 (7.3) | −3.2 (8.3) | 46.6 (9.8) | 46.6 (9.8) | −0.6 (8.7) | .26 |
| Fatigue (range = 29.4-83.2) | 52.2 (7.2) | 49.8 (8.4) | −1.2 (6.9) | 50.9 (8.5) | 51.1 (6.2) | 0.4 (6.4) | .56 |
| Sleep (range = 28.9-76.5) | 52.5 (6.9) | 47.6 (7.2) | −4.0 (5.3)* | 49.5 (6.7) | 48.8 (8.0) | −0.8 (6.0) | .11 |
| Family support (range = 13-65) | 33.2 (11.4) | 37.8 (8.6) | 3.6 (10.0) | 30.8 (12.2) | 26.8 (9.9) | −3.3 (10.8) | .0012 |
| Friend support (range = 13-65) | 31.8 (10.4) | 36.6 (8.8) | 4.4 (10.4)* | 29.4 (12.1) | 27.4 (9.2) | −1.2 (10.8) | .0088 |
| Outcome expectations for physical activity (range = 1-5) | 4.0 (0.7) | 4.3 (0.6) | 0.2 (0.5) | 4.0 (0.6) | 4.0 (0.5) | 0.03 (0.4) | .30 |
Note. Boldface indicates statistical significance (p < .05).
p < .05 within group change.
Replication of Results in Wait-List Control Arm at 24 Weeks
The wait-list control group increased moderate-to-vigorous physical activity from 12 weeks (median = 75) to 24 weeks (median = 120), p = .0569. Participant satisfaction data indicate that the intervention also was well received in this arm. Of the 22 wait-list control participants who responded, 81.8% described the DIAL program as helpful/very helpful and 90.9% would recommend it to a friend. Moreover, 81% of wait-list control participants reporting being satisfied/very satisfied with the intervention.
The wait-list control arm demonstrated similar adherence to intervention protocols during their 12-week DIAL trial as the original intervention arm, with 42.3% of the wait-list control arm calling the IVR system daily (vs. 43.8% of the intervention arm). In fact, participants who received the intervention after 12 weeks on wait-list may have even shown a slight advantage in terms of adherence to the monthly counseling call protocol (73.1% completed all 3 calls), compared to those who received the intervention up front (59.4%).
Discussion
Findings support the feasibility, acceptability, and preliminary efficacy of the DIAL intervention. The high retention rate at 12 weeks and positive participant satisfaction survey feedback indicate that this telephone-delivered intervention was well received in our sample. Moreover, the intervention participants reported larger increases in physical activity from baseline to 12 weeks than the control group, which supports preliminary efficacy. There were also significant improvements in sleep disturbance and theoretical constructs (physical activity self-regulation and social support from family and friends) which often serve as early indicators of behavior change.
There has been a paucity of research on IVR-supported physical activity interventions. A recent Cochrane review of automated telephone communication systems for preventive health care and management of long-term conditions (Posadzki et al., 2016) found only three physical activity IVR studies (Jarvis, Friedman, Heeren, & Cullinane, 1997; King et al., 2007; Sparrow, Gottlieb, Demolles, & Fielding, 2011). Prior telephone-based physical activity interventions have mostly been delivered by research staff and/or health care providers (not automated) and found similar self-report physical activity and psychosocial outcomes as the current study. In fact, the physical activity gains (M = 101.9 minutes/week of moderate intensity or greater physical activity at 12 weeks, SD = 73.9) from this automated, IVR-supported DIAL intervention were only slighter smaller than those found after 6 months of health educator-provided telephone counseling (M = 123.32 minutes/week of moderate intensity or greater physical activity, SD = 97.64) in another study (Marcus et al., 2007). Past research from Rogers and colleagues also found that 12-week supervised exercise programs improved sleep quality among breast cancer survivors (Rogers et al., 2017), but few other telephone-based physical activity interventions (to our knowledge) have examined this important quality of life variable; warranting future research on this topic.
The current study also extends the existing literature by providing a more interactive, personalized IVR approach, as past IVR-based physical activity studies have often been unidirectional (Dubbert, Cooper, Kirchner, Meydrech, & Bilbrew, 2002; Morey et al., 2009; Morey et al., 2012) and involved generic physical activity counseling (David et al., 2012; Sparrow et al., 2011) and computer-generated voice (Jarvis et al., 1997; King et al., 2007; Pinto et al., 2002). Specifically, counseling was narrated by the project director (i.e., a familiar, local voice) and individually tailored on SCT constructs with good effect in the current study. In fact, increases in SCT constructs (exercise goal setting and exercise planning) were similar to those found in a prior 12-week IVR-based walking intervention for postmenopausal women (David et al., 2012), which (unlike the current study) did not improve social support. Self-efficacy for physical activity was enhanced by the health educator-provided telephone counseling (Marcus et al., 2007) but not by either the current or the previously mentioned IVR interventions (David et al., 2012). This may prove a difficult variable to address via automated counseling. Thus, additional formative research and intervention refinement will be needed to determine how to best approach this SCT construct (and others which were targeted, yet remained unchanged in the current study; e.g., enjoyment and outcome expectations).
Strengths and Limitations
Strengths of this study include the use of a theory-informed intervention and randomized trial design, with a wait-list control arm that allowed for replication of findings. In fact, 7-Day Physical Activity Recall interview data suggests that the 12-week waiting period may have given the control arm time to mentally prepare for behavior change and/or perhaps primed them for intervention. The use of a small convenience sample (recruited mostly from flyers distributed near the university in Birmingham, Alabama) with high levels of education may limit the generalizability of findings to less educated and/or rural samples. Moreover, there were issues with missing/invalid accelerometer data at 12 weeks, which made it difficult to corroborate 7-Day Physical Activity Recall interview findings.
Adherence rates for the rather demanding intervention protocols were adequate in the current study and higher for monthly calls than daily calls. As incentives were provided for completing IVR calls, future studies should assess program adherence in situations where participants are not paid for participation and discern whether daily calls are necessary or if a less intensive call (weekly) schedule will result in equivalent (or greater) physical activity improvements. For the current study, participants called into the study line at their convenience, but IVR systems can also initiate these calls. Adherence resulted in slightly larger increases in physical activity in the current study; thus, streamlining the protocol by moving the burden from participant to the automated system could lead to improved call adherence and additional physical activity gains. Future studies should test the relative efficacy of IVR—versus participant—initiated call protocols.
Conclusion
This DIAL intervention has great potential for improving physical activity and cancer reduction efforts in the Deep South. Automated telephone counseling can reach large numbers of people at low cost and does not require travel, literacy, and/or access to advanced technology (smartphone). Most DIAL intervention participants reported gaining some knowledge about exercising (85.7%) and feeling motivated to start (or continue) exercise (71.4%) as a result of this program. However, only 28.6% of intervention participants met the national physical activity guidelines of 150 minutes/week of moderate intensity physical activity at 12 weeks (vs. 18.5% of the control arm). Thus, next steps for this line of research will include intervention refinement (streamlining and adapting IVR protocols for improved adherence, further targeting unchanged SCT constructs) in preparation for a fully-powered efficacy trial and eventual dissemination in rural counties.
Implications for Practice
Interactive voice response systems have great potential for increasing the reach of health educators and other public health professionals. Community health advisors, especially in mostly rural regions such as the Deep South, often cover large geographic areas and encounter vast health disparities and education needs. Practitioners are only able to meet with community members one on one or in small groups as schedules, transportation, funding, and so on, allow. Automated communication systems can serve as useful health education tools by enabling ongoing assessments and counseling between these visits and thereby enhance, extend, and sustain public health efforts.
Acknowledgments
We thank Dr. Cathy Simpson and other collaborators for earlier contributions to this study. We also thank Michelle Constant-Jones, Ashley Sineath, Amanda Burnside, Caroline Keller, Keaira Foster, Meagan Joseph, Claudia Hardy, and Chris Parks at the University of Alabama at Birmingham for their valuable assistance with this project. Most important, we thank our study participants for their time and participation.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Funding sources that supported this work include grants from the National Institutes of Health (R03CA177538, T32HL105349).
Footnotes
Declaration of Conflicting Interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- American Cancer Society. (2017). Diet and physical activity: What’s the cancer connection? Retrieved from https://www.cancer.org/cancer/cancer-causes/diet-physical-activity/diet-and-physical-activity.html [Google Scholar]
- Anderson ES, Winett RA, Wojcik JR, & Williams DM (2010). Social cognitive mediators of change in a group randomized nutrition and physical activity intervention: Social support, self-efficacy, outcome expectations and self-regulation in the guide-to-health trial. Journal of Health Psychology, 75(1), 21–32. doi: 10.1177/1359105309342297 [DOI] [PubMed] [Google Scholar]
- Attwood S, Morton KL, Mitchell J, Van Emmenis M, & Sutton S (2016). Reasons for non-participation in a primary care-based physical activity trial: A qualitative study. BMJ Open, 6(5), e011577. doi: 10.1136/bmjopen-2016-011577 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bandura A (1986). Social foundations of thought and action: A social cognitive theory. Upper Saddle River, NJ: Prentice Hall. [Google Scholar]
- Blair SN, Haskell WL, Ho P, Paffenbarger RS, Vranizan KM, Farquhar JW, & Wood PD (1985). Assessment of habitual physical activity by a seven-day recall in a community survey and controlled experiments. American Journal of Epidemiology, 122, 794–804. [DOI] [PubMed] [Google Scholar]
- Butland RJA, Pang J, Gross ER, Woodcock AA, & Geddes DM (1982). Two-, six-, and 12-minute walking tests in respiratory disease. British Medical Journal, 284, 1607–1608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cahalin L, Pappagianopoulos P, Prevost S, Wain J, & Ginns L (1995). The relationship of the 6-min walk test to maximal oxygen consumption in transplant candidates with end-stage lung disease. Chest, 108, 452–459. [DOI] [PubMed] [Google Scholar]
- Canadian Society for Exercise Medicine. (1994). PAR-Q and you. Gloucester, Ontario, Canada: Author. [Google Scholar]
- Cella D, Riley W, Stone A, Rothrock N, Reeve B, Yount S, … Promis Cooperative Group. (2010). The Patient-Reported Outcomes Measurement Information System (PROMIS) developed and tested its first wave of adult self-reported health outcome item banks: 2005–2008. Journal of Clinical Epidemiology, 63, 1179–1194. doi: 10.1016/j.jclinepi.2010.04.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, & Division of Nutrition, Physical Activity, and Obesity. (2017). Nutrition, physical activity, and obesity: Data, trends, and maps. Retrieved from http://www.cdc.gov/nccdphp/dnpao/data-trends-maps/index.html [Google Scholar]
- David P, Buckworth J, Pennell ML, Katz ML, DeGraffinreid CR, & Paskett ED (2012). A walking intervention for postmenopausal women using mobile phones and interactive voice response. Journal of Telemedicine and Telecare, 18(1), 20–25. doi: 10.1258/jtt.2011.110311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dubbert PM, Cooper KM, Kirchner KA, Meydrech EF, & Bilbrew D (2002). Effects of nurse counseling on walking for exercise in elderly primary care patients. Journal of Gerontology: Series A, Biological Sciences and Medical Sciences, 57, M733–M740. [DOI] [PubMed] [Google Scholar]
- Freedson PS, Melanson E, & Sirard J (1998). Calibration of the computer science and Applications, Inc. accelerometer. Medicine & Science in Sports & Exercise, 30, 777–781. [DOI] [PubMed] [Google Scholar]
- Hayden-Wade HA, Coleman KJ, Sallis JF, & Armstrong C (2003). Validation of the telephone and in-person interview versions of the 7-day PAR. Medicine & Science in Sports & Exercise, 35, 801–809. doi: 10.1249/01.MSS.0000064941.43869.4E [DOI] [PubMed] [Google Scholar]
- Ingram D, Wilbur J, McDevitt J, & Buchholz S (2011). Women’s walking program for African American women: Expectations and recommendations from participants as experts. Women Health, 51, 566–582. doi: 10.1080/03630242.2011.606357 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Irwin ML, Ainsworth BE, & Conway JM (2001). Estimation of energy expenditure from physical activity measures: Determinants of accuracy. Obesity Research, 9, 517–525. [DOI] [PubMed] [Google Scholar]
- Janz KF (1994). Validation of the CSA accelerometer for assessing children’s physical activity. Medicine & Science in Sports & Exercise, 26, 369–375. [PubMed] [Google Scholar]
- Jarvis KL, Friedman RH, Heeren T, & Cullinane PM (1997). Older women and physical activity: using the telephone to walk. Women’s Health Issues, 7(1), 24–29. [DOI] [PubMed] [Google Scholar]
- Kendzierski D, & DeCarlo KJ (1991). Physical Activity Enjoyment Scale: Two validation studies. Journal of Sport and Exercise Psychology, 13(1), 50–64. doi: 10.1123/jsep.13.1.50 [DOI] [Google Scholar]
- King AC, Friedman R, Marcus B, Castro C, Napolitano M, Ahn D, & Baker L (2007). Ongoing physical activity advice by humans versus computers: The Community Health Advice by Telephone (CHAT) trial. Health Psychology, 26, 718–727. doi: 10.1037/0278-6133.26.6.718 [DOI] [PubMed] [Google Scholar]
- Kirsch IS, Jungeblut A, Jenkins L, & Kolstad A (2002). Adult literacy in America: A first look at the findings of the National Adult Literacy Survey (NCES 1993-275). Washington, DC: Office of Educational Research and Improvement; Retrieved from https://nces.ed.gov/pubs93/93275.pdf [Google Scholar]
- Leenders NYJM, Sherman WM, Nagaraja HN, & Kien CL (2001). Evaluation of methods to assess physical activity in free-living conditions. Medicine & Science in Sports & Exercise, 33, 1233–1240. [DOI] [PubMed] [Google Scholar]
- Marcus BH, Napolitano MA, King AC, Lewis BA, Whiteley JA, Albrecht A, … Papandonatos GD (2007). Telephone versus print delivery of an individualized motivationally tailored physical activity intervention: Project STRIDE. Health Psychology, 26, 401–409. doi: 10.1037/0278-6133.26.4.401 [DOI] [PubMed] [Google Scholar]
- Martinez SM, Arredondo EM, Perez G, & Baquero B (2009). Individual, social, and environmental barriers to and facilitators of physical activity among Latinas living in San Diego County: Focus group results. Fam Community Health, 32(1), 22–33. doi: 10.1097/01.FCH.0000342814.42025.6d [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melanson EL Jr., & Freedson PS (1995). Validity of the Computer Science and Applications, Inc. (Òsa) activity monitor. Medicine & Science in Sports & Exercise, 27, 934–940. [PubMed] [Google Scholar]
- Merriam-Webster Collegiate Dictionary. (2017). The Deep South. Retrieved from https://www.merriam-webster.com/dictionary/the%20Deep%20South [Google Scholar]
- Morey MC, Peterson MJ, Pieper CF, Sloane R, Crowley GM, Cowper PA, … Pearson MP (2009). The veterans learning to improve fitness and function in elders study: A randomized trial of primary care-based physical activity counseling for older men. Journal of the American Geriatrics Society, 57, 1166–1174. doi: 10.1111/j.1532-5415.2009.02301.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morey MC, Pieper CF, Edelman DE, Yancy WS Jr., Green JB, Lum H, … Taylor GA (2012). Enhanced fitness: A randomized controlled trial of the effects of home-based physical activity counseling on glycemic control in older adults with prediabetes mellitus. Journal of the American Geriatrics Society, 60, 1655–1662. doi: 10.1111/j.1532-5415.2012.04119.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Cancer Institute. (2017a). Physical activity and cancer. Retrieved from https://www.cancer.gov/about-cancer/causes-prevention/risk/obesity/physical-activity-fact-sheet [Google Scholar]
- National Cancer Institute. (2017b, March 22). Understanding cancer. Retrieved from http://www.cancer.gov/about-cancer/understanding/statistics [Google Scholar]
- Pekmezi D, Ainsworth C, Holly T, Williams V, Benitez TJ, Wang K, … Demark-Wahnefried W (2017). Rationale, design, and baseline findings from a pilot randomized trial of an IVR-Supported physical activity intervention for cancer prevention in the Deep South: the DIAL study. Contemporary Clinical Trials Communications, 8, 218–226. doi: 10.1016/j.conctc.2017.10.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pekmezi D, Ainsworth C, Joseph RP, Williams V, Desmond R, Meneses K, … Demark-Wahnefried W (2017). Pilot trial of a home-based physical activity program for African American women. Medicine and Science in Sports and Exercise, 49(12), 2528–2536. doi: 10.1249/MSS.0000000000001370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pekmezi D, Marcus B, Meneses K, Baskin ML, Ard JD, Martin MY, … Demark-Wahnefried W (2013). Developing an intervention to address physical activity barriers for African-American women in the deep south (USA). Women’s Health, 9(3), 301–312. doi: 10.2217/whe.13.20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pereira MA, FitzerGerald SJ, Gregg EW, Joswiak ML, Ryan WJ, Suminski RR, … Zmuda JM (1997). A collection of physical activity questionnaires for health-related research. Medicine & Science in Sports & Exercise, 29(6 Suppl), S1–S205. [PubMed] [Google Scholar]
- Perrin A (2017). Digital gap between rural and nonrural America persists. Retrieved from http://www.pewresearch.org/fact-tank/2017/05/19/digital-gap-between-rural-and-nonrural-america-persists/ [Google Scholar]
- Pinto BM, Friedman R, Marcus BH, Kelley H, Tennstedt S, & Gillman MW (2002). Effects of a computer-based, telephone-counseling system on physical activity. American Journal of Preventive Medicine, 23, 113–120. [DOI] [PubMed] [Google Scholar]
- Posadzki P, Mastellos N, Ryan R, Gunn LH, Felix LM, Pappas Y, … Car J (2016). Automated telephone communication systems for preventive healthcare and management of long-term conditions. Cochrane Database of Systematic Reviews, (12), CD009921. doi: 10.1002/14651858.CD009921.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Resnick B, Zimmerman SI, Orwig D, Furstenberg A-L, & Magaziner J (2000). Outcome Expectations for Exercise Scale: Utility and psychometrics. Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 55, S352–S356. doi: 10.1093/geronb/55.6.S352 [DOI] [PubMed] [Google Scholar]
- Rogers LQ, Courneya KS, Oster RA, Anton PM, Robbs RS, Forero A, & McAuley E (2017). Physical activity and sleep quality in breast cancer survivors: A randomized trial. Medicine & Science in Sports & Exercise, 49, 2009–2015. doi: 10.1249/MSS.0000000000001327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sallis JF, Grossman RM, Pinski RB, Patterson TL, & Nader PR (1987). The development of scales to measure social support for diet and exercise behaviors. Preventive Medicine, 16, 825–836. doi: 10.1016/0091-7435(87)90022-3 [DOI] [PubMed] [Google Scholar]
- Sallis JF, Haskell WL, Wood PD, Fortmann SP, Rogers T, Blair SN, & Paffenbarger RS (1985). Physical activity assessment methodology in the five-city project. American Journal of Epidemiology, 121(1), 91–106. [DOI] [PubMed] [Google Scholar]
- Sloane R, Snyder DC, Demark-Wahnefried W, Lobach D, & Kraus WE (2009). Comparing the 7-day physical activity recall with a triaxial accelerometer for measuring time in exercise. Medicine & Science in Sports & Exercise, 41, 1334–1340. doi: 10.1249/MSS.0b013e3181984fa8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solway S, Brooks D, Lacasse Y, & Thomas S (2001). A qualitative systematic overview of the measurement properties of functional walk tests used in the cardiorespiratory domain. Chest, 119, 256–270. doi: 10.1378/chest.119.1.256 [DOI] [PubMed] [Google Scholar]
- Sparrow D, Gottlieb DJ, Demolles D, & Fielding RA (2011). Increases in muscle strength and balance using a resistance training program administered via a telecommunications system in older adults. Journal of Gerontology: Series A, Biological Sciences and Medical Sciences, 66, 1251–1257. doi: 10.1093/gerona/glr138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Troiano RP, Berrigan D, Dodd KW, Masse LC, Tilert T, & McDowell M (2008). Physical activity in the United States measured by accelerometer. Medicine & Science in Sports & Exercise, 40, 181–188. doi: 10.1249/mss.0b013e31815a51b3 [DOI] [PubMed] [Google Scholar]
- U.S. Cancer Statistics Working Group. (2017). United States cancer statistics: 1999-2014 Incidence and mortality web-based report. Retrieved from http://www.cdc.gov/uscs [Google Scholar]
- U.S. Census Bureau. (2014). Computer and Internet access in the United States: 2012. Retrieved from http://www.census.gov/data/tables/2012/demo/computer-internet/computer-use-2012.html [Google Scholar]
- U.S. Department of Commerce. (2012). 2010 Census population and housing tables. Retrieved from https://www.census.gov/prod/www/decennial.html [Google Scholar]
- U.S. Department of Health and Human Services. (2008). 2008 Physical activity guidelines for Americans. Washington, DC: Author. [Google Scholar]
- Wilkinson S, Huang CM, Walker LO, Sterling BS, & Kim M (2004). Physical activity in low-income postpartum women. Journal of Nursing Scholarship, 36, 109–114. doi: 10.1111/j.1547-5069.2004.04022.x [DOI] [PubMed] [Google Scholar]


