Abstract
Background:
The complication of prematurity is the second commonest cause of under-five mortality in Ethiopia. Amhara region has the highest neonatal mortality rate in the country. There was no previous study and this study aimed to assess the survival of preterm neonates and its associated factors of preterm neonatal mortality admitted to Felege Hiwot Specialized Hospital, Bahir Dar, Ethiopia, to take necessary action to maximize survival of preterm babies in developing countries.
Methods:
A retrospective cross-sectional study was conducted among 686 preterm neonates admitted in Felege Hiwot Specialized Hospital from 1 August 2017 to 30 July 2018. Kaplan–Meier survival curve was used to show the survival rate of preterm neonates and the multivariate Cox proportional hazards model was used to identify covariates of survival of preterm neonates. Those variables having a p-value less than 0.05 were statistically significant for the survival of preterm neonates.
Result:
Out of 686 preterm neonates admitted from 1 August 2017 to 30 July 2018, 49.1% neonates were improved and discharged and 36.1% died. The survival rate was 0%, 19.4%, 46.7% and 75% for gestational age <28 weeks, 28–31 + 6 weeks, 32–33 + 6 weeks and 34–36 + 6 weeks, respectively. In the multivariate Cox regression model, respiratory distress syndrome, necrotizing enterocolitis, asphyxia, hospital-acquired infection, birth weight, gestational age and place of delivery were significantly associated with time to death of preterm neonates at 95% confidence level (p < 0.05).
Conclusion:
The mortality rate (36.1%) of preterm neonates is unacceptably high in Felege Hiwot hospital compared to other similar hospitals in Ethiopia. More than 50% of preterm neonatal deaths can be prevented with available resources. Neonatal units with adequate and committed manpower, using a strict aseptic technique, proper follow-up, early detection and timely management of complications, are recommended to improve the survival of preterm neonates.
Keywords: Analysis, neonates, preterm, survival
Background
The neonatal period is defined as the first 28 days after birth or up to the 44th post-menstrual week in preterm infants. Live born infants delivered before 37 weeks or 259 days of gestation from the first day of the last menstrual period are termed premature which is a major determinant of neonatal mortality and morbidity.1,2 Preterm neonates are classified based on birth weight into normal birth weight (NBW) (2500–3999 g), low birth weight (LBW) (1500–2499 g), very low birth weight (VLBW) (1000–1499 g) and extremely very low birth weight (EVLBW) (<1000 g), which are inverse proportional to their survival.3
Globally, 15 million preterms are born every year and their number is rising. Of these, 1.1 million preterms die from a complication of preterm birth each year.2,4 Africa accounts for 31% of preterm births in the globe. In many developing countries, infants weighing less than 2000 g (corresponding to about 32 weeks of gestation in the absence of intrauterine growth retardation) have little chance of survival. In contrast, the survival rate of infants born at 32 weeks in developed countries is similar to that of infants born at term.5
Prematurity is associated with increased neonatal morbidity and mortality.3,6 Prematurity is the second leading cause of under-five mortality. Of all early neonatal deaths (deaths within the first 7 days of life) that are not related to congenital malformations, 28% is due to preterm birth.7 Preterm birth complications account for 35% of neonatal mortality in which more than three-quarters of premature babies can be saved with feasible and cost-effective care.8
Even though the survival of preterm infants has been globally improving during the second half of the 20th century, survival in Africa is the poorest in the world. The average decline in child mortality in Africa is 42%, compared with a decline of 60%–72% in other regions over the same period.9,10 Preterm babies have a risk of death that is around 13 times higher than full-term babies.11
The preterm rate in Ethiopia is 10%–14%, ranking 11th in the world in 2010.9 Ethiopia is the country with the lowest survival of premature babies. The complication of prematurity is the second (24.5%) commonest cause of under-five mortality in Ethiopia.12 In a study done at Tikur Anbessa specialized hospital, the overall survival was 69.3%.13 The neonatal mortality rate of the Amhara regional state is higher (47) than the national neonatal mortality rate (29) per 1000 birth births in 2016.12 This research aimed to study the survival rate, time to discharge, time to death and peak time to death of preterm neonates in Felege Hiwot specialized hospital (FHSH) neonatal intensive care unit (NICU) and contributing factors of mortality.
Methods
Study area
The study was conducted in Bahir Dar city, Northwest Ethiopia. Bahir Dar is the capital of Amhara regional state, located 578 km away north-northwest of Addis Ababa. The total population of the city is 649,429 by 2012. Felege Hiwot specialized Hospital is established in 1963 and serving more than 8 million peoples.
Study design and period
A hospital-based retrospective cross-sectional study was conducted among preterm neonates admitted to Felege Hiwot specialized hospital from 1 August 2017 to 30 July 2018. The study was conducted from 1 December 2018 to 8 February 2019.
Sample size determination
All preterm neonates (686) who had a complete chart and no congenital anomaly admitted to FHSH NICU from 1 August 2017 to 30 July 2018 were included as study units. We used the whole cases as sample size as it was not possible to use sample size calculation formula of survival analysis for this study as there was no known relative hazard and censoring rate of our variables from previous study in same setups.
Sampling procedures
From 1083 preterm neonates admitted to FHSH NICU from 1 August 2017 to 30 July 2018, 686 preterm neonates were selected as the study sample. Others were excluded from the study unit due to the congenital anomaly or incompleteness of charts (Figure 1).
Figure 1.

Flow diagram of the overall recruitment of preterm neonates in Felege Hiwot hospital, Bahir Dar, Ethiopia, from 1 August 2017 to 30 July 2018.
Inclusion and exclusion criteria
Inclusion criteria
Preterm neonates admitted in Felege Hiwot specialized hospital NICU from 1 August 2017 to 30 July 2018.
Exclusion criteria
Preterm neonates admitted to FHSH NICU and who had congenital anomaly and incomplete charts are considered under exclusion criteria.
Operational definitions
Inborn: a baby who was born in Felege Hiwot specialized hospital.
Out born: neonate who was born outside the Felege Hiwot specialized hospital.
Discharged against medical advice: The family of the newborn refused the continuation of inpatient management and left the hospital while the neonate was not a candidate for discharge.
Neonatal death: neonate died in the hospital and death summary was written on a chart.
Data collection tools and procedures
A structured data abstraction sheet was used to collect the data from the preterm neonate’s chart. The questionnaire was taken from different kinds of literature and modified to the required variables (see supplemental material). Two BSc nurse data collectors and one BSc nurse supervisor participated during the data collection process. The data were collected from 1 December 2018 to 10 January 2019.
Statistical analysis
Data were entered and cleaned using EpiData version 3.1 and exported to SPSS program version 21 for further analysis. Descriptive data were presented using text, tables and figures. Kaplan–Meier (KM) chart to estimate the survival rate and multivariate Cox regression model to identify covariates of survival of preterm neonates was used. A bivariate Cox regression model analysis was performed (at p < 0.20) for each independent and outcome of interest (time to death and discharge of preterm neonates) to identify independent predictors. Variable with a bivariate test of a p-value < 0.20 was a candidate for the multivariate Cox regression model along with all variables. Covariates having p < 0.05 in multivariate Cox regression analysis were considered as statistically significant for preterm survival and finally verified by different model assessment both graphically and numerically.
Results
Socio-demographic and health factors of mothers
The antenatal steroid was given to 85 (12.4%) of mothers of preterm babies. Of the mothers who had preterm neonate, 130 (19%) had preterm premature rupture of membrane (PPROM) and/or chorioamnionitis, 115 (16.8%) had preeclampsia/eclampsia and 32 (4.7%) had antepartum hemorrhage which was responsible for overall 40.5% of preterm labor. Around 28% of mothers of preterm babies had a medical problem such as diabetes mellitus (0.7%), cardiac illness (0.3%) and chronic hypertension (0.1%). Forty (5.8%) mothers who delivered preterm babies were less than 20 years. The mean maternal age was 27 years and the mean parity was 2.66. The youngest mother was 16 years old and the oldest mother was 48 years old. The residential area was Bahir Dar city in 55.7% of mothers.
Neonatal and health service characteristics
In this study, a total of 686 preterm neonates were included. The mode of delivery was spontaneous vaginal delivery (SVD) in 75.2% of cases and 23.2% were delivered by cesarean section (CS). Only 5.8% of neonates were born at home and 53.6% were inborn. Out of all neonates, 426 (62.1%) were males. About 88.9% of preterm babies admitted in first day of life. Fifteen (2.2%) of preterm neonates were below 28 weeks of gestational age (GA), which is said to be not viable by definition in Ethiopia.
Moderate to severe hypothermia was diagnosed in 484 (70.55%) of preterm neonates at admission. Appearance, pulse, grimace, activity and respiratory (APGAR) scores were not reported in 246 (35.9%) out born neonates (Table 1). Weight for GA was appropriate for 89.2% preterm babies and 10.2% were small for GA. The diagnosis of sepsis, respiratory distress syndrome (RDS) and hyperbilirubinemia was made in 632 (92.1%), 305 (40.5%) and 237 (34.5%), respectively, at the time of admission. From the total preterm neonates, 16.5% developed necrotizing enterocolitis (NEC) and 5.4% had perinatal asphyxia (PNA) with stage II or III hypoxic-ischemic encephalopathy. Twins and triplets accounted for 38.3% and 2.8% of preterm neonates, respectively. Eighty-eight (12.8%) preterm neonates were diagnosed to have a healthcare-associated infection.
Table 1.
Frequency distribution of different variables of preterm neonates admitted to FHSH, Bahir Dar, Ethiopia, from 1 August 2017 to 30 July 218.
| Variables | Category | Number of cases | Outcome |
|
|---|---|---|---|---|
| Improved and discharged | Death | |||
| Age at admission | 0–1 day | 610 (88.9%) | 286 (46.9%) | 234 (38.3%) |
| 1.01–3 | 40 (5.8%) | 24 (60%) | 7 (17.5%) | |
| 3.01–7 | 24 (3.5%) | 18 (75%) | 4 (16.6%) | |
| 7.1–28 | 12 (1.7%) | 9 (75%) | 2 (16.7%) | |
| Gestational age | 26–27.9 | 15 (2.2%) | 0 (0%) | 15 (100%) |
| 28–31.9 | 201 (29.3%) | 39 (19.4%) | 122 (60.7%) | |
| 32–33.9 | 199 (29%) | 93 (46.7%) | 65 (32.7%) | |
| 34–36.9 | 271 (39.5%) | 205 (75.6%) | 45 (16.6%) | |
| Admission temperature | >37.5 | 94 (13.7%) | 15 (75%) | 2 (10%) |
| 36.5–37.5 | 88 (12.8%) | 59 (62.7%) | 22 (23.4%) | |
| 36–36.4 | 476 (69.4%) | 49 (55.7%) | 22 (25%) | |
| 32–35.9 | 8 (1.2%) | 211 (44.3%) | 198 (41.6%) | |
| <32 | 20 (2.9%) | 3 (37.5%) | 3 (37.5%) | |
| Fifth-minute APGAR score | 0–3 | 3 (0.4%) | 1 (33.3%) | 2 (66.7%) |
| 4–6 | 49 (7.1%) | 15 (30.6%) | 29 (59.2%) | |
| 7–10 | 388 (56.6%) | 213 (54.9%) | 122 (31.4%) | |
| Unknown | 246 (35.9%) | 108 (43.9%) | 94 (38.2%) | |
| Hypoglycemia | 77 (11.2%) | 43 (55.8%) | 27 (35.1%) | |
| Meningitis | 37 (5.4%) | 19 (51.4%) | 7 (18.9%) | |
| Anemia | 38 (5.5%) | 14 (36.8%) | 20 (52.6%) | |
| Polycythemia | 15 (2.2%) | 7 (46.7%) | 3 (20%) | |
| Total | 337 (49.1%) | 247 (36.1%) | ||
FHSH: Felege Hiwot specialized hospital.
More than half (58%) was LBW (Figure 1). The minimum and maximum birth weights were 620 and 3400 g. The mean and standard deviation of admission weight and GA were1684 g (SD = ±455) and 32.9 weeks (SD = ±2.5), respectively. The mean age at admission is 15 h and the duration of hospital stay was 10 days and the mean duration of antibiotics was 8 days. The minimum and maximum hospital stays were 5 h and 53 days, respectively.
KM survival curves
The KM curve shows that the pattern of the patients who have RDS lying below than those who have no RDS, which means that patients who have RDS had lower survival compared with patients who have no RDS. The mortality of preterm babies increases as the GA decreases (Figures 2–5).
Figure 2.
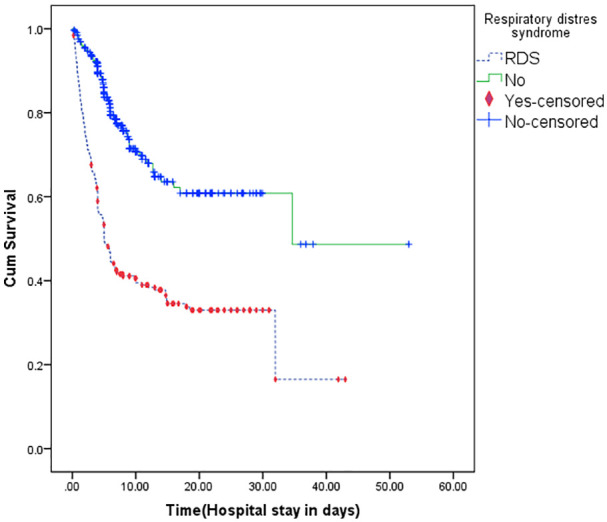
Kaplan–Meier curve comparing survival of preterm with neonates RDS versus without RDS.
Figure 3.
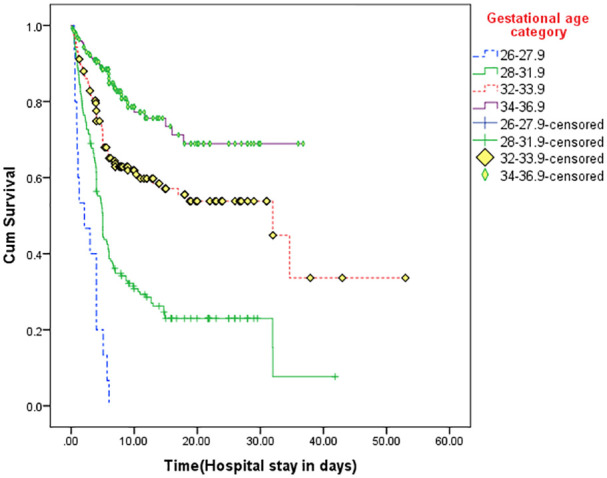
Kaplan–Meier curve of survival of preterm neonates based on gestational age category.
Figure 4.
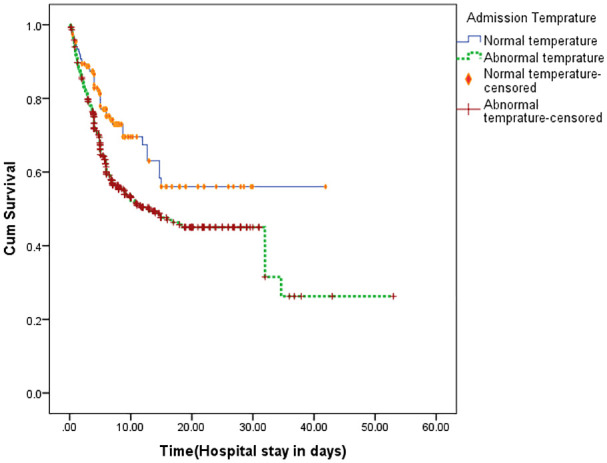
KM curve comparing survival of preterm neonates based on admission temperature.
Figure 5.
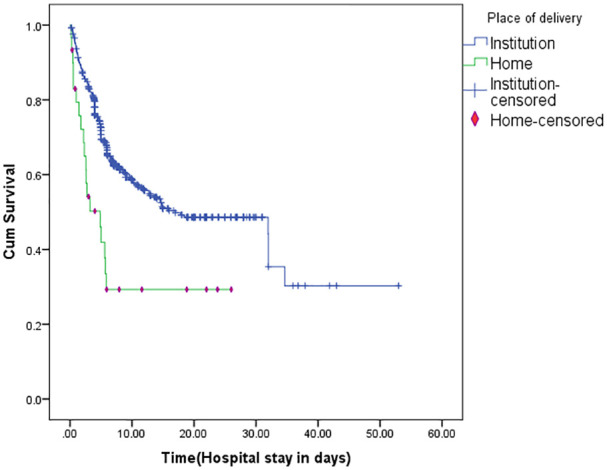
KM curve comparing survival of preterm neonates based on place of birth.
Survival analysis and outcome
Out of 686 admitted preterm babies, 247 (36.1%) were died (Figure 2) and 94 (13.7%) neonates discharged against medical advice. The survival rate of EVLBW, VLBW, LBW and NBW were 0%, 19.9%, 66.1% and 87.5%, respectively. The survival rate was 0%, 19.4%, 40%, 46.7% and 75% for GA < 28 weeks, 28–31 + 6 weeks, 32–33 + 6 weeks and 34–36 + 6 weeks, respectively (Table 1). The survival rate of preterm babies with RDS, sepsis, NEC, hospital-acquired infection (HAI), asphyxia, meningitis and severe hypothermia was 30.2%, 47.3%, 15%, 42%, 37.8%, 51.4%, 47.4% and 37.5%, respectively. As shown in Figure 3, RDS was the commonest cause of death of preterm babies. Based on time to an event, more than 50% of preterm neonates were discharged improved in the first 10 days of life. Only 16.6% of preterm neonatal death occurred in first 24 h of life (Figure 6).
Figure 6.
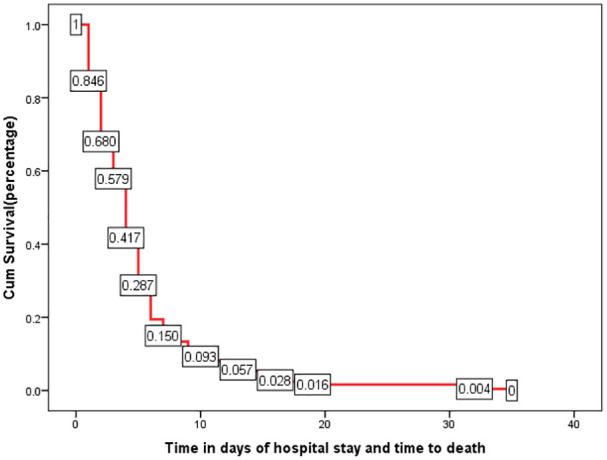
Summary of KM survival estimate of time to death of neonates admitted at FHSH, Bahir Dar, Ethiopia, from 1 August 2017 to 30 July 2018 (n = 686). The graph shows the proportion of neonates who died during the hospital stay. During the first 10 days, the graph went down sharply which shows a higher proportion of death of neonates. More than 92% of death occurs in the first 10 days of admission.
Bivariate and multivariate analysis
In the bivariate Cox regression model, RDS, sepsis, NEC, meningitis, hyperbilirubinemia, asphyxia, anemia, HAI, admission temperature, birth weight, GA and place of delivery were independent predictors of preterm neonatal mortality at 80% confidence level (p < 0.2). In the multivariate Cox regression model, RDS, NEC, hyperbilirubinemia, asphyxia, HAI, birth weight, GA and place of delivery were significantly associated with time to death of preterm neonates at 95% confidence level (p < 0.05).
Neonates who had RDS were 1.77 times (adjusted hazard ratio (AHR) = 1.77, 95% CI: 1.317, 2.382) higher likelihood of death compared to those neonates who had no RDS. The risk of death of neonates whose GA was less 28 weeks was 2.4 times higher (AHR = 2.4, 95% CI: 1.979, 5.856) compared to those with GA 34 weeks and above. Preterm neonates whose birth weights less than 1000 g were 10.97 times more likely to die compared to those who had NBW. Preterm neonates who had stage III asphyxia were 2.49 times higher likelihood of death compared to those who had no asphyxia (Table 2).
Table 2.
Bivariate and multivariate cox regression analysis of preterm neonatal mortality admitted in FHSH, Bahir Dar, Ethiopia, from 1 August 2017 to 30 July 2018 (n = 584).
| Covariates | Category | Outcome number (%) |
HR 95% CI |
||
|---|---|---|---|---|---|
| Survival | Death | CHR | AHR | ||
| RDS | Yes | 92 (35.8%) | 165 (64.2%) | 3.01 (2.308, 3.926) | 1.771 (1.317, 2.382) |
| No | 245 (74.9%) | 82 (25.1%) | 1 | ||
| Sepsis | Yes | 299 (55.3%) | 242 (44.7%) | 3.222 (1.328, 7.814) | 1.777 (0.72, 4.386) |
| No | 38 (88.4%) | 5 (11.6%) | 1 | ||
| NEC | Yes | 17 (17.2%) | 82 (82.8%) | 2.068 (1.585, 2.699) | 1.848 (1.37, 2.492) |
| No | 320 (66%) | 165 (34%) | 1 | ||
| Meningitis | Yes | 19 (73.1%) | 7 (26.9%) | 0.372 (0.175, 0.791) | 0.53 (0.241, 1.164) |
| No | 318 (57%) | 240 (43%) | 1 | ||
| Hyperbilirubinemia | Yes | 117 (61.3%) | 74 (38.7%) | 0.627 (0.477, 0.824) | 0.581 (0.436, 0.775) |
| No | 220 (56%) | 173 (44%) | 1 | ||
| PNA | Stage III | 3 (33.3%) | 6 (66.7%) | 3.249 (1.1441, 7.327) | 2.459 (1.074, 5.634) |
| Stage II | 11 (40.7%) | 16 (59.3%) | 1.751 (1.053, 2.909) | 1.764 (1.039, 2.996) | |
| No | 323 (58.9%) | 225 (41.1%) | 1 | ||
| Anemia | Yes | 14 (41.2%) | 20 (58.8%) | 1.718 (1.086, 2.718) | 0.9 (0.552, 1.468) |
| No | 323 (58.7%) | 227 (41.3%) | 1 | ||
| HAI | Yes | 37 (53.6%) | 32 (46.4%) | 1.518 (1.038, 2.220) | 1.8 (1.206, 2.757) |
| No | 300 (58.3%) | 215 (41.7%) | 1 | ||
| Admission temperature (T°C) | Abnormal | 229 (53%) | 203 (47%) | 1.649 (1.19, 2.286) | 1.1 (0.815, 1.594) |
| Normal | 108 (71.1%) | 44 (28.9%) | 1 | ||
| GA | <28 | 0 (0%) | 15 (100%) | 13.388 (7.418, 24.164) | 2.394 (0.979, 5.856) |
| 28–31.9 | 39 (24.2%) | 122 (75.8%) | 4.926 (3.497, 6.939) | 2.367 (1.551, 3.612) | |
| 32–33.9 | 93 (58.9%) | 65 (41.1%) | 2.134 (1.457, 3.125) | 1.691 (1.133, 2.524) | |
| 34–36.9 | 205 (82%) | 45 (18%) | 1 | ||
| Birth weight | 600–999 | 0 (%) | 23 (100%) | 43.616 (10.246, 185.67) | 10.968 (2.235, 53.8) |
| 1000–1499 | 46 (26.3%) | 129 (73.7%) | 10.889 (2.691, 44.068) | 4.134 (0.977, 17.49) | |
| 1500–2499 | 263 (73.9%) | 93 (26.1%) | 3.698 (1.911, 15.021) | 2.354 (0.57, 9.723) | |
| 2500-3500 | 28 (93.3) | 2 (6.7%) | 1 | ||
| Place of delivery | Home | 11 (36.7%) | 19 (63.3%) | 2.381 (1.489, 3.806) | 2.08 (1.26, 3.434) |
| Institution | 326 (58.8%) | 228 (41.2%) | 1 | ||
FHSH: Felege Hiwot specialized hospital; HR: hazard ratio; CI: confidence interval; AHR: adjusted hazard ratio; CHR: crude hazard ratio; RDS: respiratory distress syndrome; GA: gestational age; NEC: necrotizing enterocolitis; PNA: perinatal asphyxia; HAI: hospital-acquired infection.
Discussion
This study showed that 49.1% of preterm neonates were improved and discharged and the mortality rate was 36.1% which is nearer to Jimma University Specialized Hospital (34.9%) from a cohort study done 4 years back which had less than half the number of total admissions than Felege specialized Hiwot hospital.14 The overall mortality rate of preterm neonates is higher than 30.7% in Tikur Anbessa13,15 and 25.2% in Gondar university hospital.12 This higher preterm neonatal mortality in FHSH is likely due to poor quality of care in FHSH.
The survival of preterm babies with PNA (37.8%) was lower than that of Jimma University (64.3%) possibly better set up and experienced.14 Prematurity and LBW have been associated with an increased incidence of sepsis. Chorioamnionitis and rupture of the membrane increase the risk of sepsis to 2–4 folds.2 The diagnosis of sepsis is high (92%) in this study in which the diagnosis was made clinically in almost all cases. Clinical diagnosis of sepsis has poor sensitivity and specificity as signs and symptoms of sepsis in premature are non-specific and overlapping.
Clinical diagnosis of sepsis has to be supported by blood culture and other investigations. High incidence of HAI (12.8%) in this study may be due to a higher number of admissions compared to the number of beds, overcrowding and poor adherence to an aseptic technique by health professionals in the hospital.3 Of all admissions, 83.4% had hypothermia and 77.1% of total and 72.1% inborn had moderate hypothermia at admission which is better than in the Tikur Anbessa hospital but worse than Jimma University hospital.13,14 Only 27.9% of inborn neonates had normal admission temperature, while the labor ward is only two floors away from NICU. This shows warm chain transport and early referral were not properly practiced.
GA and birth weight are the major determinants of survival in premature babies. The survival rate of preterm neonates were 0%, 19.4%, 46.7% and 75.6% for GA < 28 weeks, 28–31 + 6 weeks, 32–33 + 6 weeks and 34–36 + 6 weeks, respectively, in Felege Hiwot hospital. The survival rate of neonates below 28 weeks was equivalent to Gondar university hospital unlike that of other setups that have a higher survival rate. Over 90% of extremely preterm babies (<28 weeks) born in low-income countries die within the first few days of life; yet less than 10% of babies of this gestation die in high-income settings, a 10:90 survival gap.9 From a retrospective chart review of 397 preterms from 1 July 2011 to 30 June 2012 G.C. in Tikur Anbessa hospital survival of infants was 40% for GA < 28 weeks, 54.5% for 28–31 weeks, 74.6% for 32–34 weeks and 100% for 35–36 + 6days of GA. One research 5 years ago in Kenya showed 86.7% survival rate of neonates whose GA < 34 weeks.9,13,16,17 The survival rate of EVLBW infants was found to be 34.43% in Tikur Anbessa hospital. EVLBW infants (<1000 g) remain at high risk for death and disability with 30%–50% mortality in the USA.18,19 Overall survival was 70.5%. Survival of infants below 1001 g birth weight was 34.9% compared to 85.8% for those between 1001 and 1500 g at birth in Johannesburg Academic Hospital 9 years ago.20 This study showed that the survival of preterm babies is significantly low at Felege Hiwot hospital at each respective GA and birth weight even compared to low-income countries. This may be due to a lack of well-equipped neonatal ICU setup, neonatologist, political commitment, standard laboratory service and advanced treatment modalities of preterm babies.
In this study, it was found that 85% of the preterm neonates died in the first 7 days of life, and of this, 16.6% of them died in the first 24 h of life and 43% died in first 72 h of life. The first 24 h of life mortality was significantly lower compared to other research works in which the highest mortality occurs in the first 24 h of life. This indicates that care during the first few hours of life is acceptable. Most of the death occurred from second to seventh day of life, particularly 3–7 days (42% of death) which showed the later complication of prematurity is responsible for the majority of death. A poor preventive strategy, poor follow-up, failure to detect complication and taking timely intervention after first day of life is the possible explanation for this problem.3,4,7
Trophic feeding was the mode of initial feeding for all GA < 34 weeks and birth weight <1500 g. Despite this, NEC was among the major (16.5%) cause morbidity and mortality (33.2%). Only 15% of neonates who developed NEC survived in this hospital which is alarmingly high compared to other studies.2,3,6 This low survival of neonates who developed NEC in FHSH is possibly due to improper time of initiation and feeding advancement, detection at an advanced stage, lack of serial bedside X-ray and lack of surgical experience. Absence of parenteral feeding option when enteral feeding is not possible also hampers the recovery from NEC.
The leading causes of death were RDS (35.73%), uncontrolled sepsis (22.89%) and NEC (12.85%) which accounted for 71.47% of overall death in this NICU. There may be an overlapping cause of death but only one most likely cause is incriminated as a cause of each death. Other causes of death were asphyxia, apnea of prematurity, pulmonary hemorrhage and immediate lack of oxygen. Lack of oxygen directly or indirectly incriminated for the death of 17 (6.83%) infants. This was due to the dependence of the hospital on oxygen importation from Addis Ababa, the capital of Ethiopia, which was not sustainable due to political unrest. None report of death due to an immediate lack of oxygen from other setups. Oxygen plantation in this city totally can prevent the problem. This means that more than 50% of preterm neonatal death can be prevented with available resources in FHSH.
In this study, the potential determinant of premature infants’ mortality was identified by applying the stepwise selection of covariates in a Cox regression model. RDS, NEC, PNA, place of delivery, hyperbilirubinemia, HAI, GA and birth weight were statistically significant variables for mortality of premature infants. These significant variables are statistically associated with time to death of premature infants admitted to this NICU and consistent with previous studies.6,19 Premature neonates who had RDS and home delivery were 43.5% (AHR = 0.565, 95% confidence interval (CI): 0.42, 0.76) and 51.6% (AHR = 0.481, 95% CI: 0.291, 0.794) more likely to die than those infants without RDS and institutional delivery, respectively. If preterm neonate develops NEC or HAI, the risk of death will increase to 45.9% (AHR = 0.541, 95% CI: 0.401, 0.73) and 45.2% (AHR = 0.548, 95% CI: 0.363, 0.829), respectively. The HR (95% CI) for premature infants admitted to NICU who had RDS was 1.771 (1.317, 2.382) of premature infants those who had RDS 1.77 times higher than those infants without RDS. Preterm neonates with RDS had a hazard of death lower than that of Jimma University.15
The strength of this study is that it had included most of predictors of preterm neonatal survival and associated factors. Data collection was also complete and reliable. The sample size was large and enables to get more reliable result for generalization for most hospitals of Ethiopia. The limitation of the study is 24.9% of preterm babies were excluded due to incompleteness of charts as the study was retrospective and 5.4% withdraw from treatment. The study was conducted only in public referral hospital where high risk neonates were admitted. Home deliveries were not part of the study, as we failed to track the deaths that occurred at home and this may underestimate the neonatal mortality rate because home deliveries are at increased risk of complications and deaths. Moreover, withdrawal neonates may encounter deaths that could underestimate our neonatal mortality rate.
Conclusion
The survival rate of EVLBW, VLBW, LBW and NBW was 0%, 19.9%, 66.1% and 87.5%, respectively. The survival rate was 0%, 19.4%, 40%, 46.7% and 75% for GA < 28 weeks, 28–31 + 6 weeks, 32–33 + 6 weeks and 34–36 + 6 weeks, respectively. Neonates with GA < 28 weeks, weight <1000 g and acute bilirubin encephalopathy had no chance of survival. The overall survival rate of preterm neonates was 49.1% and the overall mortality rate was 36.1% which signifies very low survival and high mortality rate compared to other hospitals with similar setups in Ethiopia.
Hypothermia, sepsis, RDS, NEC, hyperbilirubinemia and HAI were among the leading causes of morbidity. RDS, sepsis and NEC were the leading cause of death. A higher number of neonatal death occurred after 24 h of life. RDS, NEC, PNA, home delivery, hyperbilirubinemia, HAI, abnormal admission temperature, lower birth weight and far GA from term were statistically significant variables for mortality of premature neonates at 95% confidence level (p < 0.05). More than 50% of preterm neonatal deaths can be prevented with available resources in FHSH.
Recommendation
A prospective study is recommended to get more reliable and complete data of patients. Following strict aseptic technique by the caregiver and attendants, isolating septic neonates in a separate room, decreasing overcrowding (establishing other NICUs in other hospitals) and early discharge is vital to decrease HAI. Most of the death occurs after 24 h of life, proper follow-up, early detection and timely management of complications are mandatory. Timely initiation, proper escalating of trophic feeding according to patient’s condition and proper follow-up to pick NEC as early as possible is the key to decrease it.
Supplemental Material
Supplemental material, Questionnaire for Survival and associated factors of mortality of preterm neonates admitted to Felege Hiwot specialized hospital, Bahir Dar, Ethiopia by Ayanaw Tamene, Gedefaw Abeje and Zelalem Addis in SAGE Open Medicine
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval: Ethical approval was obtained from Bahir Dar University, College of Medicine and Health Science Ethics Review Committee, but specific ethical approval number was not given during that time.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Informed consent: Consent from minor groups was waived, as it was a retrospective study.
ORCID iD: Ayanaw Tamene  https://orcid.org/0000-0002-7991-9612
https://orcid.org/0000-0002-7991-9612
Supplemental material: Supplemental material for this article is available online.
References
- 1. International classification of diseases related health problems. 10th rev. Geneva: World Health Organization, 1992. [Google Scholar]
- 2. Martin RJ, Fanaroff AA, Walsh MC. Fanaroff and Martin’s neonatal-perinatal medicine: diseases of the fetus and infant. 10th ed. Philadelphia, PA: Saunders, 2015. [Google Scholar]
- 3. Kliegman R, Staton BST, Geme J, et al. Nelson textbook of pediatrics. 20th ed. Springer: Elsevier, 2015. [Google Scholar]
- 4. Born too soon: The global actions report on preterm birth (Save the Children WHO), 2012, https://www.who.int/pmnch/media/news/2012/preterm_birth_report/en/
- 5. Beck S, Wojdyla D, Say L, et al. The worldwide incidence of preterm birth: a systematic review of maternal mortality and morbidity. Bull World Health Organ 2010; 88: 31–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Hay WW, Levin MJ, Sondheimer JM, et al. Current diagnosis & treatment: pediatrics. 19th ed. New York: McGraw-Hill, 2009. [Google Scholar]
- 7. Lawn JE, Wilczynska-Ketende K, Cousens SN. Estimating the causes of 4 million neonatal deaths in the year 2000. Int J Epidemiol 2006; 35(3): 706–718. [DOI] [PubMed] [Google Scholar]
- 8. MCEE_ WHO Methods and data sources for child cause of death, 2000_2016, February 2018. [Google Scholar]
- 9. Liu L, Johnson HL, Cousens S, et al. Global, regional, and national causes of child mortality: an updated systematic analysis for 2010 with time trends since 2000. Lancet 2012; 379: 2151–2161. [DOI] [PubMed] [Google Scholar]
- 10. Ahmad OB, Lopez AD, Inoue M. The decline in child mortality: a reappraisal. Bull World Health Org 2000; 78: 1175. [PMC free article] [PubMed] [Google Scholar]
- 11. World Health Organization. World Health Report 2005: make every mother and child count. Geneva: World Health Organization, 2005. [Google Scholar]
- 12. Hayelom G, Sahle MBW. Survival of neonates and predictors of their mortality in Tigray region, Northern Ethiopia: prospective cohort study. BMC Public Health 2017; 17: 62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Merertu T, Bogale W, Yonas R. Survival of preterm infants admitted to Tikur Anbessa Hospital NICU, Addis Ababa. Ethiop J Ped Child Health 2014; 10(10): 68–78. [Google Scholar]
- 14. Million W, Sudhir K, Tafere T. Modeling determinants of time-to-death in premature infants admitted to neonatal intensive care unit in Jimma University Specialized Hospital. Ann Data Sci 2017; 4: 361–381. [Google Scholar]
- 15. Sheferaw Y, Salie A, Zinabu T. Survival analysis of premature infants admitted to neonatal intensive care unit (NICU) in Northwest Ethiopia using semi-parametric frailty model. J Biomet Biostat 2015; 6: 223. [Google Scholar]
- 16. Su BH, Hsieh WS, Hsu CH, et al. Neonatal outcomes of extremely preterm infants from Taiwan: comparison with Canada, Japan, and the USA. Pediatr Neonatol 2015; 56: 46–52. [DOI] [PubMed] [Google Scholar]
- 17. Patel A, Kandasamy Y. Outcome of premature neonates born in a tertiary neonatal intensive care unit in Nairobi. Kenya. J Pediatr Neonatal Individual Med 2017; 6(1): 2442. [Google Scholar]
- 18. Mukherjee S, Shaw SC, Devgan A, et al. Survival and morbidities in very low birth weight (VLBW) infants in a tertiary care teaching hospital. Int J Contemp Pediatr 2017; 4(6): 2170–2174. [Google Scholar]
- 19. Glass HC, Costarino AT, Stayer SA, et al. Outcomes for extremely premature infants. Anesth Analg 2015; 120(6): 1337–1351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Ballot DE, Chirwa TF, Cooper PA, et al. Determinants of survival in very low birth weight neonates in a public sector hospital in Johannesburg. BMC Pediatr 2010; 10: 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, Questionnaire for Survival and associated factors of mortality of preterm neonates admitted to Felege Hiwot specialized hospital, Bahir Dar, Ethiopia by Ayanaw Tamene, Gedefaw Abeje and Zelalem Addis in SAGE Open Medicine


