Abstract
Background:
COVID-19 is thought to be the most significant public health threat the modern world has encountered. Health care workers (HCWs) face enormous pressure due to work overload, negative emotions, exhaustion, lack of contact with their families, and risk of catching the infection and death.
Aim:
This study aims to assess the level of stress perceived by HCWs and possible associated factors during the COVID-19 outbreak in Palestine.
Methods:
A cross-sectional sample of 430 frontlines HCWs was conducted using an online self-reported questionnaire. HCWs’ stress from the COVID-19 outbreak, factors that increase stress, and the activities that reduced stress were assessed. Chi-square test was used to compare between a categorical variable and the study outcome; associations are presented as odds ratios (OR) and confidence intervals (95% CI) with 0.05 significance level. Al-Najah National University institutional review board granted ethics approval.
Results:
Most respondents (74.0%) reported high-stress levels during the outbreak. Fear of transmitting the virus to family was the most stressful factor (91.6%). HCWs who did not have training on the outbreak response were more likely to have high-stress levels (OR = 2.7 [95% CI = 1.7-4.4], P < .001). Those with high stress reported being disappointed (OR = 2.4 [95% CI = 1.5-3.6], P < .001), and strongly considered taking sick leave (OR = 3.9 [95% CI = 1.9-7.9], P < .001).
Conclusion:
HCWs are under tremendous stress, given the ongoing COVID-19 pandemic. Understanding the psychological impact of the outbreak on HCWs and the activities that mitigate the stress is crucial to guide policies and interventions that can maintain psychological well-being.
Keywords: health care workers, stress, Palestine, stressors, COVID-19
Introduction
The novel coronavirus outbreak of pneumonia emerged in Wuhan, China days before the 2020 New Year, and has subsequently garnered worldwide attention. By the end of April 2020, Coronavirus disease 2019 (COVID-19) had invaded most countries with almost 20 million confirmed cases as of the time of manuscript submission, and a reported crude case fatality rate of 4% based on the current case description of the World Health Organization (WHO).1 Compared to previous Coronavirus outbreaks, COVID-19 appears to be more contagious, with a more extended incubation period, and on the 16th of March the WHO declared it a pandemic infectious disease.2
COVID-19 is currently thought to be the most significant public health threat the modern world has encountered. The severity of the disease, the unavailability of a vaccine, little evidence on the effectiveness of potential therapeutic agents, and no presumably pre-existing immunity in the population make everyone potentially susceptible and fearful about catching the infection.3
Health care is a highly stressful profession and considered among the top stressful professions during normal circumstances.4 Facing this large scale, infectious public health event puts medical staff under both physical and psychological pressure.5,6 Since the early emergence of the disease, it has been recognized that personnel working in health care facilities and caring for patients with COVID-19 are under tremendous stress.7 Previous experience from coronavirus outbreaks such as Severe Acute Respiratory Syndrome- Coronavirus-1 (SARS CoV-1) and the Middle East Respiratory Syndrome Coronavirus (MERS-CoV) demonstrated varying levels of anxiety and nervousness among frontline health care workers (HCWs).8,9
Data regarding HCWs occupational hazard of exposure in the current emergency is suboptimal.10 Available data in China showed that 3000 HCWs were infected, and at least 22 died.11 A significant proportion of HCWs experienced anxiety, depression, and insomnia.12
The psychological burden of the outbreak is due to several factors. Besides the fear of death and the high risk of infection, HCWs face enormous pressure due to work overload, negative emotions, lack of contact with their families, and exhaustion.13 The extreme preventive practices and the use of whole-body personal protective equipment (PPE) have been linked to many psychological effects.14 Stress may be compounded when HCWs are shunned because others, including family, fear that they may transmit infection.
Higher levels of stress and emotional exhaustion were shown to be associated with higher absenteeism, intention to exit the profession, and low quality personal and family life.15 Assessing the level of stress, and its source should be a priority for health service managers and other stakeholders.4 To date, epidemiological data on the mental health problems and psychiatric morbidity of those suspected or diagnosed with the 2019-nCoV and their treating health professionals is minimal; therefore how to respond to these challenges during the outbreak is unknown.16
Palestine reported the first 7 confirmed cases of COVID-19 on March 5, 2020. Since then, HCWs have faced a rapidly increasing workload of possible COVID-19 patients and been on the receiving end of harassment and discrimination because of public COVID-19 fears. This study aims to assess the level of stress perceived by HCWs and possible associated factors during the COVID-19 outbreak in Palestine.
Methods
While a cross-sectional research design was adopted, the sampling method generally followed convenience sampling. The study population included frontline HCWs (physicians, nurses, and other allied health professionals; lab and radiology technicians) working in hospitals and primary healthcare centers who were likely to deal with suspected or confirmed COVID-19 patients. Online software was used to design an electronic web-based questionnaire. It was sent, with 2 invitations to participate, to HCWs through closed institutional groups using different social media tools (WhatsApp and Messenger). This method was used to reach as many frontline HCWs as possible in COVID-19 related quarantine circumstances and to comply with social distancing guidelines and taking advantage of the high rate of internet use among Palestinians.17
The time frame was planned to capture the uncertainty and the lack of experience with the COVID-19 outbreak by sampling over 2 weeks (March 29-April 15) in which the peak of cases and deaths in Palestine occurred.
The sample size calculation was based on the formula: [n = Z2*P*(1−P)/d2],18 where Z (=1.96) is the statistic for a level of confidence, P is the expected proportion of subjects presented mental disorders, and d is the precision. The minimum required sample size (n) to meet the study objectives was estimated at 385 healthcare professionals by assuming 50% expected proportion, which is the maximum variability, a 95% confidence interval (CI), and a 5% absolute precision either side of the proportion.
The questionnaire had 36 questions in 3 sections: section 1 explored HCWs’ demographic information, and section 2 assessed stress and stressful factors from the COVID-19 outbreak using a Likert scale from 0 to 5, where “0” means no stress and “5” indicates very severe stress. Section 3 assessed knowledge regarding COVID-19 through 6 multiple-choice questions. A correct answer was assigned 1 point, and an incorrect answer was assigned 0 points. The total knowledge score ranged from 0 to 6, with a higher score denoting a better knowledge of COVID-19. Factors contributing to the reduction of stress were explored in multiple response questions were that the participant could check all that applied.
The questionnaire was built based on an extensive literature review.8,19,20 It was reviewed by 3 experts in the field and pre-tested for its validity and reliability. A pilot study was framed on Google Forms (the online questionnaire form). Twenty HCWs were selected purposively, included male and female doctors, nurses, and allied health professionals from different age groups and health care settings. The questionnaire was tested for its content and feasibility, delivery, and ease of filling it out.
This study was approved and implemented in collaboration with the Palestinian Ministry of Health. Ethical approval was obtained from Al-Najah National University Institutional Review Board (Reference No: F. MED 3/20/10). Detailed information about the study’s aim and what participation would involve was provided on the first page of the online questionnaire. Participants could withdraw at any time, without providing a reason, and that all information and opinions given would be confidential and anonymous.
The Statistical Package for the Social Sciences software (SPSS version 20.0) was used for data analysis. Frequencies and percentages of occurrence summarized categorical socio-demographic data. The age and experience variables were categorized into 2 groups: <35 years of age or ≥35, and <10 years of experience in health care or ≥10, respectively. The perceived level of stress was categorized into high-stress levels for those who ranked their stress level ≥3 and low stress for those who ranked <3. HCWs’ knowledge was categorized into 2 groups; adequate knowledge for those who answered correctly ≥4 questions and inadequate knowledge for those who answered correctly <4 questions. Cronbach’s alpha was computed to assess the internal consistency of the stress and emotions related statements. It was 0.90, which indicates an excellent level of self-consistency.
Chi-square test was used to compare categorical variables with the study outcome; associations are presented as odds ratios (OR) and confidence intervals (95%CI). A P-value of <.05 was used to determine statistical significance.
Results
Four hundred thirty HCWs (211 doctors and 219 nurses or allied health professionals) from the West Bank of Palestine agreed to participate. The average age of the participants was 36 (±8.9) years the majority married (77.2%), have children (74.1%), and living with their families during the outbreak (89.7%). About 54% of the participants worked in primary healthcare settings, and 243 (56.0%) have ≥10 years of work experience. Of HCWs, 157 (36.5%) reported having contact with suspected or confirmed COVID-19 cases (Table 1). HCWs’ knowledge of COVID-19 was assessed with 6 questions, and two thirds (66.0%) showed adequate knowledge.
Table 1.
Demographic Characteristics of Participant Health Care Workers (n = 430).
| Characteristic | Total sample |
Health care
workers/profession |
|
|---|---|---|---|
| Frequency (%) | Doctor (n = 211) Frequency (%) |
Other HCWs†(n = 219) Frequency (%) |
|
| Sex | |||
| Male | 194 (45.2) | 134 (69.1) | 60 (30.9) |
| Female | 235 (54.8) | 77 (32.8) | 158 (67.2) |
| Age | |||
| <35 years | 206 (48.7) | 114 (55.3) | 92 (44.7) |
| ≥35 years | 217 (51.3) | 97 (44.7) | 120 (55.3) |
| Health care setting | |||
| Primary health care | 234 (54.3) | 96 (41.0) | 138 (59.0) |
| Hospitals | 196 (45.4) | 115 (58.7) | 81 (41.3) |
| Experience | |||
| <10 | 187 (44.0) | 120 (64.2) | 67 (35.8) |
| ≥10 years | 243 (56.0) | 91 (37.4) | 152 (62.6) |
| Marital status | |||
| Married | 332 (77.2) | 151 (45.5) | 181 (54.5) |
| Unmarried | 98 (22.7) | 60 (61.2) | 38 (38.8) |
| Have children | |||
| Yes | 318 (74.1) | 137 (43.1) | 181 (56.9) |
| No | 111 (25.9) | 73 (65.8) | 38 (34.2) |
| Living with family | |||
| Yes | 384 (89.7) | 190 (49.5) | 194 (50.5) |
| No | 44 (10.3) | 20 (45.5) | 24 (45.5) |
| Reported having contact with a suspected or confirmed case | |||
| Yes | 157 (36.5) | 84 (53.5) | 73 (46.5) |
| No | 273 (63.5) | 127 (46.5) | 146 (53.5) |
Nurses and allied health care professionals; lab and radiology technicians.
HCWs were asked to rate their level of stress during the outbreak over a scale of 6. Of them, 318 [74.0% (95% CI = 69.8%-78.3%)] reported high levels of stress; levels 3, 4, and 5 (Figure 1).
Figure 1.
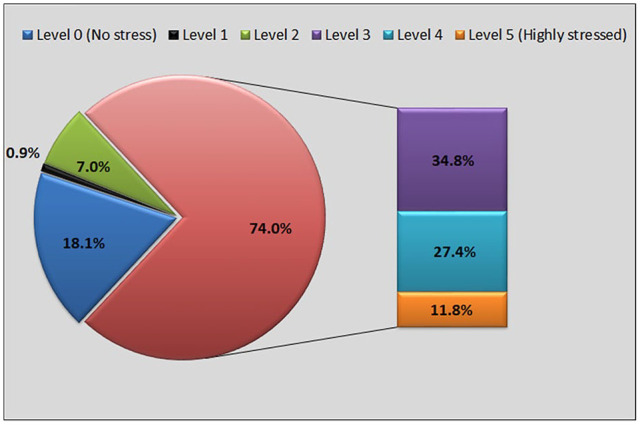
Distribution of perceived stress level among health care workers.
Of the factors that increased stress, the fear of transmitting the virus to family was the highest (91.6%), followed by the fact that the disease has no treatment (87.7%), and the fear of acquiring the infection personally (85.8%). Table 2 summarizes the most common stressors perceived by HCWs.
Table 2.
Factors Reported by Health Care Works to Increase Their Stress.
| Factors | Frequency | Percentage |
|---|---|---|
| The fear of transmitting COVID-19 to family | 394 | 91.6 |
| The fact that there is no treatment for COVID-19 | 377 | 87.7 |
| The possibility of catching the infection | 370 | 85.8 |
| Being a health care worker and know about COVID-19 | 359 | 83.5 |
| Knowing that the disease is uncontrolled | 346 | 80.5 |
| The lack of experience in such outbreaks | 336 | 78.1 |
| Feeling unsafe and things are not under the control | 311 | 72.3 |
| My colleagues’ fear | 297 | 69.1 |
| Fear from being isolated or quarantined | 295 | 68.6 |
| Feeling ostracized from people because I dealt with suspected cases | 75 | 17.1 |
The univariable analysis explored the relation between HCWs’ perceived high-stress levels and their characteristics. HCWs’ gender, age, job title, experience, marital status, having children, reported dealing with suspected or confirmed cases, knowledge, and type of health care setting showed no significant relation with high-stress levels. On the other hand, not having training on outbreak response and being disappointed while working on this outbreak was associated with high-stress levels. HCWs who did not get training on the outbreak response were 2.7 times more likely to have high-stress levels (P < .001, OR = 2.7 [95% CI = 1.7-4.4]). HCWs with high-stress levels are 2.4 times more likely to report being disappointed while working on this outbreak (P < .001, OR = 2.4 [95% CI = 1.5-3.6]). Additionally, HCWs with high-stress levels are 4 times more likely to strongly think about taking sick leave (P < .001, OR = 3.9 [95% CI = 1.9-7.9]) (Table 3).
Table 3.
Factors Associated With Perceived High-Stress Level Among HCWs During COVID-19 Outbreak.
| Characteristic | Perceived stress level | P value* | OR (95% CI) | |
|---|---|---|---|---|
| High (n = 318) | Low or none (n = 112) | |||
| Sex | ||||
| Male | 138 (71.1%) | 56 (28.9%) | .237 | 0.76 (0.5-1.2) |
| Female | 179 (76.2%) | 56 (23.8%) | ||
| Age | ||||
| <35 years | 157 (76.3%) | 49 (23.7%) | .364 | 0.81 (0.5-1.3) |
| ≥35 years | 157 (72.4%) | 60 (27.6%) | ||
| Health care setting | ||||
| Primary health care | 172 (73.5%) | 62 (26.5%) | .817 | 1.1 (0.70-1.6) |
| Hospitals | 146 (74.6%) | 50 (25.4%) | ||
| Job title | ||||
| Physicians | 153 (72.5%) | 58 (27.5%) | .504 | 1.2 (0.8-1.9) |
| Other health care workers† | 165 (75.3%) | 54 (24.7%) | ||
| Experience | ||||
| <10 years | 145 (77.5%) | 42 (22.5%) | .137 | 0.72 (0.5-1.1) |
| ≥10 years | 173 (71.3%) | 70 (28.2%) | ||
| Marital status | ||||
| Married | 245 (73.8%) | 87 (26.2%) | .891 | 1.1 (0.6-1.7) |
| Unmarried | 73 (74.5%) | 25 (25.5%) | ||
| Have children | ||||
| Yes | 236 (74.2%) | 82 (25.8%) | .798 | 0.91 (0.6-1.5) |
| No | 81 (73.0%) | 30 (27.0%) | ||
| Living with family | ||||
| Yes | 284 (74.0%) | 100 (26.0%) | .860 | 0.93 (0.5-1.9) |
| No | 32 (72.7%) | 12 (27.3%) | ||
| Reported having contact with a suspected or confirmed case | ||||
| Yes | 117 (74.5%) | 40 (25.5%) | .839 | 0.95 (0.6-1.5) |
| No | 201 (73.6%) | 72 (26.4%) | ||
| Knowledge | ||||
| Adequate‡ | 210 (73.9%) | 74 (26.1%) | .995 | 0.99 (0.6-1.6) |
| Inadequate | 108 (74.0%) | 38 (26.0%) | ||
| Got training on outbreak response | ||||
| Yes | 56 (57.7%) | 41 (42.3%) | <.001 | 2.7 (1.7-4.4) |
| No | 262 (78.7%) | 71 (21.3%) | ||
| Felt disappointed while working on this outbreak& | ||||
| Yes | 203 (81.0%) | 48 (19.0%) | <.001 | 2.4 (1.5-3.6) |
| No | 115 (64.2%) | 64 (35.8%) | ||
| Strongly thought about sick leave | ||||
| Yes | 80 (89.9%) | 9 (10.1%) | <.001 | 3.9 (1.9-7.9) |
| No | 238 (69.8%) | 103 (30.2%) | ||
Abbreviations: CI: confidence interval; OR: odds ratio.
Chi-square test.
Nurses, and allied health care professionals; lab and radiology technicians.
Having a score of ≥4/6 on knowledge questions.
This referred to the environment in which they were working.
Regarding factors that helped reduce stress, HCWs ranked being involved in activities like prayers, sports, and exercise as the most common (80.5%). This was followed by having clear guidelines for infection prevention (64.7%), the availability of PPE (57.3%), and the support of colleagues (Table 4).
Table 4.
Factors Reported by Health Care Workers to Reduce Their Stress.
| Strategy | Total | Perceived stress level | P value* | |
|---|---|---|---|---|
| High (n = 318) | Low or none (n = 112) | |||
| Did relaxation activities, for example, involved in prayers, sports, exercise, etc. | 347 (80.5%) | 254 (79.9%) | 92 (82.1%) | .6.3 |
| Having clear guidelines for infection prevention | 279 (64.7%) | 209 (65.7%) | 69 (61.6%) | .433 |
| Availability of personal protective equipment | 247 (57.3%) | 177 (55.7%) | 70 (62.5%) | .208 |
| Colleagues’ support | 244 (56.6%) | 181 (56.9%) | 62 (55.4%) | .774 |
| Sharing jokes or humor among colleagues | 179 (41.5%) | 132 (41.5%) | 46 (41.1%) | .935 |
Chi-square test.
Discussion
Palestinian HCWs reported high levels of stress during the first weeks of the current COVID-19 pandemic. In Palestine, this stress is on top of the uncertainty and challenge of living under occupation.21 These realities make it especially important that HCWs are prepared and supported in dealing with the challenges they may face.
Our sample included equivalent numbers of doctors and nurses or allied health care workers. There was little change in perceived stress between, genders, age, practice setting (primary health care vs hospital), job title (physician vs nurse), amount of health care experience, knowledge about COVID-19 (adequate vs inadequate), and whether or not the individual dealt with a suspected or confirmed case. This is in line with other studies that showed no relation between age, experience, job title, and stress.22,23 However, female gender reported significant association with stress among Indian HCWs,22 and women reported significantly higher posttraumatic stress symptoms in Hubei Province—the heart of COVID-19 pandemic.23,24 On the other hand, studies showed that nurses’ were more likely to have acute stress due to their different roles in COVID-19 patient care.22 Our findings may be attributed to the fact that during our study, Palestinian females HCWs were less likely to care for COVID-19 patients due to childcare responsibilities, and most COVID-19 patients were not severe enough to need hospitalization.
Furthermore, the level of uncertainty during this pandemic may equalize the stress response, so that even those with more experience in the healthcare setting, differing roles (doctor vs nurse), and acuity differences of the patients (hospital vs primary care) did not alter the stress HCWs experienced. HCWs reported significantly less stress if they received training on the outbreak response. The importance of preparation for managing the pandemic with clearly outlined guidelines and protocols, even if they are continually being adjusted, is critical and has been supported in other research.25 HCWs recounted more stress if they felt disappointed while working on the outbreak. The Arabic word used translates as let down or disappointed. While cross-sectional studies cannot show cause and effect, disappointment was reported as feeling unsafe and out of control. Perhaps this is due to failures in the healthcare system’s response, such as inadequate PPE, lack of guidelines, lack of training, and long work hours. Participants who felt the most stress were 4 times more likely to consider taking sick leave, which removes them from the environment, but further burdens their colleagues, and has implications for patient care.
Frontline HCWs are under massive pressure as the result of their professional obligation. Most participants reported the risk of contagion, fear of transmitting to family, and the uncertainty related to COVID-19 because there was no treatment, and their colleagues’ fear contributed to feeling stress. These are valid fears with COVID-19 as asymptomatic individuals have transmitted the disease to multiple family members,26 and HCWs have died.11
These high levels of stress are in addition to worldwide reports of burnout for physicians even before the pandemic.27 This underlines the importance of healthcare systems and managers doing all they can to support front line HCWs. To ensure minimal risk of infection when treating patients with COVID-19, the CDC recommends the use of PPE including a gown, gloves, and either an N95 respirator plus a face shield/goggles or a powered, air-purifying respirator (PAPR).28 There is limited availability of N95 masks, respiratory isolation rooms, and PAPR, in many places around the world including Palestine.21 Creating supportive environments at work and giving HCWs time off to pursue activities that help them manage the stress is also important,11 and supported by our findings.
Educating the public about preventive measures and imposing community sanctions also helps to limit the workload for HCWs. Interestingly, less than a fifth of our sample reported feeling ostracized because of their exposure to COVID-19. Perhaps this is due to the strong community commitment to HCWs as heroes because in Palestine they have been victims of the political unrest.29
This study has limitations. First, this study’s cross-sectional nature makes it challenging to identify the cause–effect relationship between independent and dependent variables. Second, obtaining the data through self-report questionnaires makes it liable for reporting bias; those interested in the topic of feeling stress chose to respond. We were unable to compare the differences between responders and non-responders. Finally, the study did not assess other variables that may impact study outcomes, such as the respondents’ socioeconomic status. Our findings may not be generalizable to Gaza, which has additional challenges, but HCWs worldwide are under tremendous stress, given the ongoing COVID-19 pandemic.11
Conclusion
In conclusion, our study showed that high levels of stress are present among Palestinian HCWs. As the pandemic continues, essential clinical and policy strategies are needed to support HCWs. Training on outbreak responses should be considered for all HCWs. Understanding the psychological impact of this outbreak and the activities that mitigate the stress is crucial to guide policies and interventions that can maintain the psychological well-being of HCWs. Updating them with clear evidence-based guidelines for infection prevention and updating them as the evidence changes, and making PPE routinely available should be considered by health authorities. Psychological support could include counseling services and the development of support systems among colleagues. These steps are imperative to ensure high-quality care for patients.
Acknowledgments
We are incredibly grateful to all Health Care Workers who took part in this study despite the immense pressure they are facing in the COVID-19 pandemic.
Footnotes
Author Contributions: BM: literature search, conceptualization and study design, development of the questionnaire, data collection, analysis, data interpretation, manuscript writing. ZN: conceptualization and study design, development of the questionnaire, analysis, data interpretation, manuscript writing. TZ: development of the questionnaire, data interpretation, manuscript writing. All authors have seen and approved the final version of the manuscript for submission.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Zaher Nazzal  https://orcid.org/0000-0002-2655-6109
https://orcid.org/0000-0002-2655-6109
References
- 1. WHO. Report of the WHO-China joint mission on Coronavirus disease 2019 (COVID-19) Situation report—93. Geneva: World Health Organization; 2020. [Google Scholar]
- 2. Nicks BA, Wong O. Coronavirus Disease 2019 (COVID-19): A Global Crisis. Medicine, 2020. https://reference.medscape.com/slideshow/2019-novel-coronavirus-6012559. Accessed August 21, 2020.
- 3. ECDC. Novel Coronavirus Disease 2019 (COVID-19) Pandemic: Increased Transmission in the EU/EEA and the UK—Sixth Update. Vol. 2019 Stockholm: ECDC; 2020. [Google Scholar]
- 4. Birhanu M, Gebrekidan B, Tesefa G, Tareke M. Workload determines workplace stress among health professionals working in Felege-Hiwot Referral Hospital, Bahir Dar, Northwest Ethiopia. J Environ Public Health. 2018;2018:6286010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Wu P, Fang Y, Guan Z, et al. The psychological impact of the SARS epidemic on hospital employees in China: exposure, risk perception, and altruistic acceptance of risk. Can J Psychiatry. 2009;54:302-311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Ofner-Agostini M, Gravel D, McDonald LC, et al. Cluster of cases of severe acute respiratory syndrome among Toronto healthcare workers after implementation of infection control precautions: a case series. Infect Control Hosp Epidemiol. 2006;27:473-478. [DOI] [PubMed] [Google Scholar]
- 7. Canadian Psychological Association. “Psychology works” fact sheet: emotional and psychological challenges faced by frontline health care providers during the COVID-19 pandemic. 2020. https://cpa.ca/docs/File/Publications/FactSheets/PW_COVID-19_FrontLineHealthCareProviders.pdf. Accessed July 12, 2020.
- 8. Khalid I, Khalid TJ, Qabajah MR, Barnard AG, Qushmaq IA. Healthcare workers emotions, perceived stressors and coping strategies during a MERS-CoV outbreak. Clin Med Res. 2016;14:7-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Bai Y, Li Y-C, Lin C-C, Chen J-Y, Chue C-M, Chou P. Survey of stress reactions among health care workers involved with the SARS outbreak. Psychiatr Serv. 2004;55:1055-1057. [DOI] [PubMed] [Google Scholar]
- 10. Zhang M. Protecting healthcare workers in China during the coronavirus outbreak. BMJ. February 14, 2020. [Google Scholar]
- 11. Adams JG, Walls RM. Supporting the health care workforce during the COVID-19 global epidemic. JAMA. 2020;323:1439-1440. [DOI] [PubMed] [Google Scholar]
- 12. Lai J, Ma S, Wang Y, et al. Factors associated with mental health outcomes among health care workers exposed to Coronavirus disease 2019. JAMA Netw Open. 2020;3:e203976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Kang L, Li Y, Hu S, et al. The mental health of medical workers in Wuhan, China dealing with the 2019 novel coronavirus. Lancet Psychiat. 2020;7:e14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. McAlonan GM, Lee AM, Cheung V, et al. Immediate and sustained psychological impact of an emerging infectious disease outbreak on health care workers. Can J Psychiatry. 2007;52:241-247. [DOI] [PubMed] [Google Scholar]
- 15. Suñer-Soler R, Grau-Martín A, Flichtentrei D, et al. The consequences of burnout syndrome among healthcare professionals in Spain and Spanish speaking Latin American countries. Burn Res. 2014;1:82-89. [Google Scholar]
- 16. Xiang Y-T, Yang Y, Li W, et al. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiat. 2020;7:228-229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Palestinian Central Bureau of Statistics. PCBS & MTIT issue a joint press release on the eve of the International Day for Telecommunication and Information Society, May 17, 2019. [Google Scholar]
- 18. Naing L, Winn T, Nordin R. Pratical issues in calculating the sample size for prevalence studies. Arch Orofac Sci. 2006;1:9-14. [Google Scholar]
- 19. Khan MU, Shah S, Ahmad A, Fatokun O. Knowledge and attitude of healthcare workers about middle east respiratory syndrome in multispecialty hospitals of Qassim, Saudi Arabia. BMC Public Health. 2014;14:1281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Alkot M, Albouq M, Shakuri M, Subahi M. Knowledge, attitude, and practice toward MERS-CoV among primary healthcare workers in Makkah Al-Mukarramah: an intervention study. Int J Med Sci Public Heal. 2016;5:952. [Google Scholar]
- 21. OCHA. Occupied Palestinian Territory (OPt): COVID-19 emergency-situation report no. 6 (21–28 April 2020) Vol. 6 OCHA; 2020. [Google Scholar]
- 22. Wilson W, Raj JP, Rao S, et al. Prevalence and predictors of stress, anxiety, and depression among healthcare workers managing COVID-19 pandemic in India: a nationwide observational study. Indian J Psychol Med. 2020;42:353-358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Liu N, Zhang F, Wei C, et al. Prevalence and predictors of PTSS during COVID-19 outbreak in China hardest-hit areas: gender differences matter. Psychiatry Res. 2020;287:112921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Shechter A, Diaz F, Moise N, et al. Psychological distress, coping behaviors, and preferences for support among New York healthcare workers during the COVID-19 pandemic. Gen Hosp Psychiatry. 2020;66:1-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Schwartz J, King C-C, Yen M-Y. Protecting healthcare workers during the Coronavirus disease 2019 (COVID-19) outbreak: lessons from Taiwan’s severe acute respiratory syndrome response. Clin Infect Dis. 2020;71:858-860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Bai Y, Yao L, Wei T, et al. Presumed asymptomatic carrier transmission of COVID-19. JAMA. 2020;323:1406-1407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Dugani S, Afari H, Hirschhorn LR, et al. Prevalence and factors associated with burnout among frontline primary health care providers in low- and middle-income countries: a systematic review. Gates open Res. 2018;2:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. CDC. Guidance for the selection and use of personal protective equipment (PPE) in healthcare settings. Centers for Disease Control and Prevention. August 18, 2014. [Google Scholar]
- 29. UN. “Continuing absence” of political solution to Israel-Palestine conflict “undermines and compounds” UN efforts to end wholesale crisis. UN News. April 29, 2019. https://news.un.org/en/story/2019/04/1037541. Accessed August 7, 2020.


