Abstract
Background:
The transition from choosing to initiating home dialysis therapies (HDTs) is not clearly standardized for patients and staff, causing increased anxiety and suboptimal self-management for chronic kidney disease (CKD) patients. At BC Renal, a “Transition to HDTs” guidebook (the Guide) was designed, outlining a step-wise approach to transitioning to HDTs for patients, to help address some of these concerns.
Objective:
We used the Logic Model evaluation framework to assess the value of the Guide to improve patient and staff experience with transitioning to HDTs.
Design:
This is a prospective cohort quality improvement study.
Setting:
This study took place at home dialysis programs in British Columbia, Canada, with 2 pilot sites and 2 control sites.
Patients:
Patients above age 18 who attended kidney care clinics and identified HDT as their renal replacement treatment of choice were included in this study.
Measurements:
Patient demographics were obtained from British Columbia Renal Patient Records and Outcomes Management Information System, with differences analyzed using Mann-Whitney U test and chi-square test where applicable. Patient surveys were based on Likert rating scales, analyzed using Cochran-Armitage trend test. All tests were 2-sided, with P < .05 considered significant.
Methods:
The study enrolled patients from December 2018 to April 2019 at 2 pilot and 2 control sites. Patients were followed up for 8 months. The intervention strategies included (1) training of front-line staff to use the Guide and (2) dissemination of the guide to patients. Evaluation tools measuring data at baseline and at the 8-month point included (1) qualitative and quantitative patient surveys, (2) qualitative staff surveys, (3) structured feedback session with renal care staff, and (4) transition rate and time between choosing and starting a HDT.
Results:
In total, 108 patients were enrolled: 43 patients at pilot sites and 65 in control sites. Twenty-three of 65 in control vs 18 of 43 in pilot transitioned to a HDT by 8-month follow-up. Transition time was 80 vs 89 days in pilot vs control group, but it was not statistically different (P = .37). The proportion of patients that transitioned to a HDT was 42% vs 35% in pilot vs control group (P = .497). Patients’ anxiety, illness knowledge, and activation of resources were not significantly different between patients who successfully transitioned at control and pilot sites. During interviews, patients confirmed that the Guide was effective and helped retain knowledge. The staff felt that the intervention did not increase their workload and that the Guide was a good communication tool, but was used inconsistently.
Limitations:
We had a small sample size and limited number of patients enrolled who chose home hemodialysis, with none in the control group. The results are therefore more applicable to peritoneal dialysis.
Conclusions:
The Logic Model was useful to evaluate our multi-intervention strategy. While there were no statistically significant differences in transition time, rate, and patient anxiety with or without the Guide, qualitative opinions from patients indicate that the Guide was a useful supplement. In addition, feedback from renal care staff suggested that the Guide served as a framework for communicating the transition process with patients, and was perceived as a useful tool. Future work is required to standardize the Guide’s utilization.
Trial registration:
As this is a quality improvement evaluation study, trial registration is not applicable.
Keywords: patient education, quality improvement, patient engagement, home dialysis
Abrégé
Contexte:
L’absence de normalisation, tant pour les patients que pour les soignants, dans la procédure de transition entre le choix de la dialyse à domicile (DD) comme thérapie de remplacement rénal et l’initiation du traitement engendre de l’anxiété et se traduit par une autogestion sous-optimale de la maladie chez les patients atteints d’IRC. Un guide de « transition vers la DD » (le Guide) a été élaboré par le BC Renal. Ce document destiné aux patients décrit une approche de transition par étapes et répond à certaines préoccupations.
Objectif:
Le cadre d’évaluation du modèle logique a été utilisé pour mesurer la capacité du Guide à améliorer l’expérience des patients et du personnel soignant lors de la transition vers la DD.
Type d’étude:
Une étude de cohorte prospective mesurant la qualité de l’amélioration.
Cadre:
L’étude s’est tenue dans le cadre du programme de DD de la Colombie-Britannique (Canada), sur deux sites pilotes et deux sites contrôles.
Sujets:
Les patients adultes qui fréquentaient les cliniques de santé rénale sélectionnées et qui avaient choisi la DD comme thérapie de remplacement rénal ont été inclus.
Mesures:
Les caractéristiques démographiques des patients ont été obtenues à partir de la base de données PROMIS (Renal Patient Records and Outcomes Management Information System) de la Colombie-Britannique. Selon le cas, les tests U de Mann-Whitney ou de chi-deux ont servi à analyser les différences. Les enquêtes menées auprès des patients étaient basées sur les échelles de notation de Likert et ont été analysées à l’aide du test de tendance Cochran-Armitage. Tous les tests étaient bilatéraux et un résultat de p inférieur à 0,05 a été considéré comme significatif.
Méthodologie:
L’étude a inclus des patients entre décembre 2018 et avril 2019 dans deux sites pilotes et deux sites contrôles, et le suivi s’est étalé sur huit mois. Les stratégies d’intervention visaient la formation du personnel de première ligne à l’utilisation du Guide et la diffusion de celui-ci aux patients. L’expérience des participants a été évaluée à l’inclusion et après huit mois de suivi à l’aide des outils suivants: (1) enquêtes qualificatives et quantitatives auprès des patients, (2) enquêtes qualitatives auprès des soignants, (3) séances de rétroaction structurées avec les soignants, (4) taux de transition et temps écoulé entre le choix de la DD comme modalité et l’initiation de la procédure.
Résultats:
L’étude porte sur un total de 108 patients (43 en site pilote et 65 en site contrôle). Au cours des huit mois de suivi, 23 patients des sites contrôles et 18 patients des sites pilotes ont fait la transition vers la DD. Le temps écoulé entre la décision et l’initiation de la DD s’établissait à 80 et 89 jours (pilotes vs contrôles), une différence qui n’a pas été considérée significative (P = 0,37). La proportion de patients qui sont passés à la DD était de 42 % et de 35 % (pilotes vs contrôles [P = 0,497]). Le niveau d’anxiété du patient, les connaissances à l’égard de la maladie et l’activation des ressources n’ont pas été jugés significativement différents entre les patients qui avaient réussi la transition, indépendamment du site. Au cours des entretiens, les patients ont confirmé que le Guide était efficace et qu’il aidait à retenir les connaissances. Les soignants ont quant à eux mentionné que les interventions n’augmentent pas leur charge de travail et que le Guide est un bon outil de communication, mais qu’il est utilisé de manière inconstante.
Limites:
L’échantillon de patients est faible; peu de sujets avaient choisi l’hémodialyse comme modalité, dont aucun dans le groupe contrôle. Nos résultats s’appliquent donc davantage à la dialyse péritonéale.
Conclusion:
Le modèle logique s’est avéré utile pour évaluer notre stratégie à interventions multiples. Bien que nous n’ayons pu observer de différences significatives dans le taux de transition, le temps requis pour procéder et le niveau d’anxiété du patient (avec ou sans le Guide), les avis qualitatifs des patients suggèrent que le Guide est un complément utile. La rétroaction du personnel soignant indique qu’il sert de cadre pour discuter du processus de transition avec les patients, et qu’il est perçu comme un outil utile. D’autres études sont requises pour normaliser l’utilisation du Guide.
Enregistrement de l’essai:
Il s’agit d’une étude mesurant la qualité de l’amélioration de l’expérience, l’enregistrement n’est donc pas requis.
What was known before
Despite advantages to home dialysis for patients transitioning from chronic kidney disease, the prevalence of home dialysis uptake in Canada has remained unchanged, at 30% over the last 5 years. Many barriers to home dialysis initiation have been identified, with numerous efforts made in hopes to improve patients’ experience in transitioning to a home dialysis modality.
What this adds
Our study demonstrates an effective approach to systematically evaluate a quality improvement project aimed to help patients with transitioning to home dialysis. By providing patients with a guidebook that clearly outlines steps of transitioning to home dialysis, we have shown that this is well-received by patients and medical staff supporting them through their transition to home dialysis. We also gained further insight on the importance of the types of educational resources offered in alleviating stress and anxiety during transitions to home dialysis.
Introduction
Chronic kidney disease (CKD) is prevalent in our aging population, with approximately 10% of Canadians affected—a portion will go on to have end-stage kidney disease (ESKD) requiring renal replacement treatment (RRT)1 which can be life altering. Home dialysis modalities including peritoneal dialysis (PD) and home hemodialysis (HHD) are becoming more popular due to better patient autonomy, convenience, and reduced burden to the healthcare system.2 From a cost perspective, home dialysis is a significantly cheaper alternative to in-center hemodialysis (cHD), with an average Canadian cost savings of $28 000 per patient per year (comparing cHD to PD maintenance costs).3 However, despite its stated benefits compared with cHD, there appears to be a lag in uptake of home dialysis modalities worldwide.4 In Canada, the prevalence of ESKD patients on dialysis using a home dialysis therapy (HDT) modality remains relatively unchanged: 23.1% in 2008 compared with 24.9% in 2018.5
The transition to home dialysis is often a confusing and frightening time for patients6 and has been identified to be fraught with significant barriers to initiating a home dialysis modality. Inadequate transition may lead to suboptimal dialysis initiation, including potential delay in starting a chosen dialysis treatment and starting an alternative dialysis modality emergently.7 Several barriers have been identified in transitioning patients to a home dialysis modality. These include anxiety about the unknown, fear of change, inadequate support when initiating home dialysis, and lack of educational resources.2 Barriers to medical staff involved in preparing patients for dialysis include lack of detailed home dialysis training, shortage of staff, and insufficient time for adequate understanding of patients’ transition journey.6,8 In addition, medical professionals including nurses, dietitians, pharmacists, and social workers who are assisting patients with the transition process may be unclear about what stage the patient is at in their transition process, and therefore have difficulty providing optimal support.
British Columbia (BC) Renal is a unique network of kidney services within BC that supports the planning, monitoring, and development of province-wide kidney care initiatives to improve the lives of British Columbians living with kidney disease. Despite decades of experience with home dialysis modalities, and significant effort toward improving their uptake, the prevalence rate of HDTs within BC remains at approximately 30%, unchanged over the past 5 years. The transition period from a patient choosing to start a home dialysis modality has been identified by the province as an area of focus for quality improvement efforts.
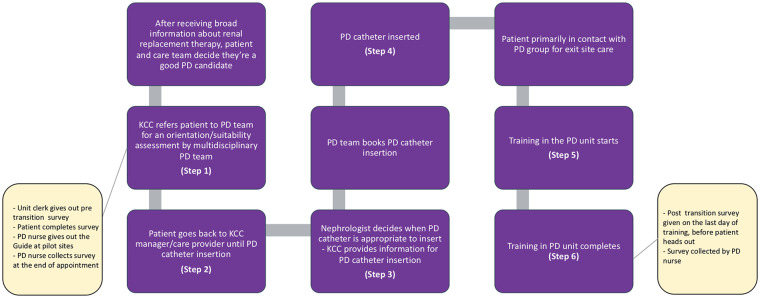
At BC Renal, a Transitions to Home Dialysis Guidebook (the Guide) has been created in response to identified barriers to the transition process, through a needs assessment conducted with patients and medical staff. The content of the Guide was designed and vetted by a committee comprised of clinicians, allied health and patient partners over a period of 2 years (2017-2018). The Guide is a resource meant to be used by both patients and the Multidisciplinary Team (MDT), and outlines 6 key steps within the transition to home dialysis (Figure 1). The aim of the Guide was to improve the transition experience for patients by (1) alleviating patient anxiety, (2) improving patient understanding of disease, and (3) reducing delays in transition to a chosen dialysis modality.
Figure 1.

The transitions to home dialysis guidebook (the guide) steps 1 to 6 summary.
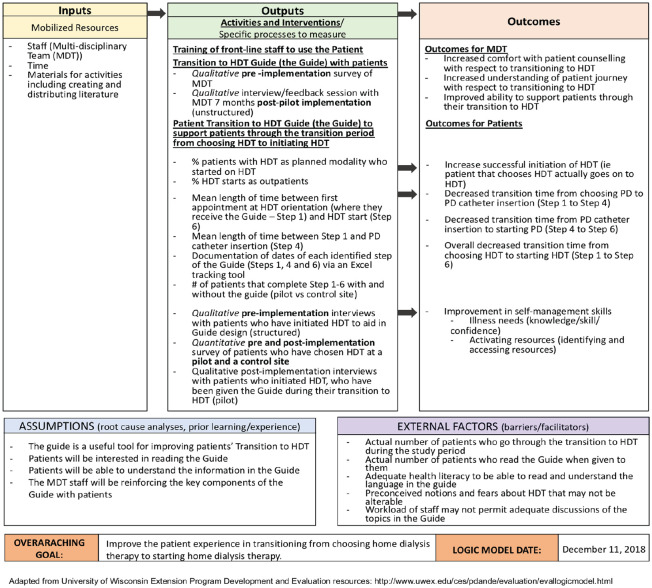
We utilized the Logic Model,9 a validated tool to evaluate this quality improvement initiative, over a 8-month pilot (December 2018-August 2019) (Figure 2). Previous studies evaluating a variety of health initiatives have successfully applied the Logic Model, including but not limited to evaluating a treatment program for mood disorders,10 a mobile phone-supported intervention for stroke rehabilitation,11 and a public health program for Type II diabetes prevention and management.12
Figure 2.
The logic model framework for evaluation of the guide.
By using this structured approach, we aim to determine the efficacy of the Guide as an example of a province-wide quality improvement (QI) initiative. We also hope to elicit additional information to guide further QI projects to improve transitions to home dialysis.
Methods
The Guide
An informal needs assessment was conducted among patients on home dialysis who were willing to participate. Information collected included frequently asked questions by patients transitioning to home dialysis, opinions on available educational resources, what patients found helpful or not helpful during their transition, and what patients felt were missing during their transition. The Guide was developed based on this assessment by a home dialysis MDT. Multiple revisions were made based on input by patients and MDT staff prior to initiation of this evaluation project. Two versions of the Guide were created, one for PD and one for HHD, following the same steps. The PD version of the Guide can be found in Supplemental Appendix 5.
Patients and transition time
Inclusion criteria for patients included patients over 18 years of age who had identified a home dialysis modality as their RRT of choice to their care providers, attended a home dialysis information session (for PD or HHD), and who were able and willing to consent to completing the surveys and interviews. Patients had to be able to read and write in English, or had a family member or friend be present to act as an interpreter. Exclusion criteria were limited to those patients who were not willing to participate in the study. Patients were enrolled prospectively in this study from December 2018 to April 2019, and followed up for 8 months. Patients had the choice to opt out of participation at any time during the study.
The transition time was defined as the time between when the patient attended a home dialysis information session (for PD or HHD) (step 1) and when they completed the training for their chosen home dialysis modality (step 6). The Guide was distributed to patients at step 1, at two pilot sites within BC. Two control sites were used for the study. The process map for patient survey administration and data collection is outlined in Figure 3 for PD patients and described in detail below. Patients are deemed eligible for home dialysis through a series of standardized assessments at the Kidney Care Clinic (KCC) that evaluate patient factors such as employment and home environment, as well as functional capabilities to ensure a plan can be put in place for home dialysis. An example of the assessments can be found in Supplemental Appendix 6. Nursing staff who were not involved in the data analysis and study design kept track of surveys and patient information. The researchers received anonymized surveys and additional demographics information was obtained through Patient Records and Outcome Management Information System (PROMIS), a provincial renal care community’s information system.
Figure 3.
Sample process map for survey administration & data collection for patients transitioning to PD.
Note. PD = peritoneal dialysis; KCC = Kidney Care Clinic.
Patient surveys
Quantitative pre- and posttransition surveys were created based on feedback for the creation of the Guide from patients and MDT about their experiences with home dialysis transitioning. At the time patients attended their first home dialysis information session (step 1), the pretransition survey was given at pilot and control sites (Supplemental Appendix 1). Patients were asked to rate their level of anxiety, understanding of their disease and home dialysis, and preparedness at this time. Once patients completed their training program (step 6), the posttransition quantitative survey was given, asking patients to rate the same parameters as in the pretransition survey (Supplemental Appendix 2). Posttransition surveys were collected until August 2019. The parameters in the surveys were based on 3- to 5-point Likert rating scales. Results were compared between pilot and control sites at step 1 and step 6, respectively.
Patient interviews
Enrolled patients who completed their transition from pilot and control sites were randomly selected for an informal telephone interview. A standard set of questions regarding patients’ experience with the quality and quantity of information received at each step of their transition to home dialysis (steps 1, 4 and 6) were asked (Supplemental Appendix 3). Specific feedback regarding the guide was asked of the pilot site participants. Responses were recorded and two researchers separately analyzed for themes. Following comparison of individual lists of themes, the researchers drew out common themes. Interviews were conducted until no additional themes were found.
Multidisciplinary Team
The MDT consisted of cHD, PD, and HHD nurses, pharmacists, and social workers at pilot and control sites who were willing to participate in the study. Staff had the choice to opt out of participation at any time during the study.
MDT surveys and group feedback
MDT members at pilot and control sites who were involved in supporting patients through their transition to home dialysis were given written, open-ended question surveys prior to the project implementation (Supplemental Appendix 4). Questions were asked with regard to their knowledge of the transition process and what challenges and barriers they experience or observe in patients throughout the transition process. At the end of the 8-month period, an informal interview was conducted with MDT staff at pilot sites to discuss their experiences in using the Guide and to seek ideas for broader implementation. Responses were recorded and grouped by theme.
Data analysis
Descriptive statistics such as mean with standard deviation or median with interquartile range were reported for continuous variables depending on the underlying distribution. Categorical variables were reported as frequency with percentage. Two-sample t test, Mann-Whitney U test, chi-square test, and Fisher exact test where appropriate were employed to examine the differences between pilot and control groups in terms of patient characteristics at step 1, proportion of patients transitioned to home therapies, timing of transition, and timing of catheter insertion. The Likert scale responses to the survey questionnaire were treated as ordinal categories. Cochran-Armitage trend test was used to compare between groups for the responses separately at steps 1 and 6 due to anonymous nature of survey data collection. All tests were 2-sided with P < .05 considered significant. Analyses were performed in SAS software, version 9.4 (SAS Institute Inc, Cary, NC).
Ethical considerations
The project was submitted to ethics committees of the Interior Health and Fraser Regional Health Authorities. Approval was deemed not necessary as this was a quality improvement initiative.
Results
Demographics
During the 8-month period, 43 of 43 patients from pilot sites and 65 of 65 patients from control sites completed the pretransition survey. The pilot and control site populations were comparable with regard to age, gender and ethnicity; no significant differences were found on statistical analysis (Table 1). However, the control group had significantly more predialysis patients compared with pilot (P = .033). Predialysis patients in this study refer to patients who received at least 3 months of care at a regional kidney care clinic, had not been on dialysis previously, nor received a kidney transplant. Among predialysis patients, there were no significant differences in the mean glomerular filtration rate (GFR), the number of patients in CKD stage 5 and 4, and the 2-year KFRE. Fourteen pilot and 17 control patients completed the posttransition survey. Ten patients (5 from pilot, 5 from control) who completed step 6 participated in the qualitative interviews.
Table 1.
Baseline Characteristics of Study Cohort.
| Pilot (n = 43) | Control (n = 65) | P value | |
|---|---|---|---|
| Home dialysis modality of choice | |||
| PD | 30 | 65 | .0001 |
| HHD | 13 | 0 | |
| Age (mean, SD) | 64 (15) | 64 (14) | .915 |
| Male | 28 (65%) | 40 (62%) | .706 |
| Race/ethnicity: Caucasian | 21 (49%) | 32 (49%) | .968 |
| Treatment modality prior to enrollment | |||
| Predialysis | 28 (65%) | 54 (83%) | .033 |
| Previous transplant | 1 (2%) | 2 (3%) | |
| Facility-based hemodialysis | 13 (31%) | 9 (14%) | |
| Peritoneal dialysis | 1 (2%) | 0 | |
| Among predialysis patients | |||
| eGFR (mean, SD) | 14.2 (5.0) | 12.9 (4.8) | .270 |
| CKD stage 4 | 11 (39%) | 19 (35%) | .715 |
| CKD stage 5 | 17 (61%) | 35 (65%) | |
| 2-year KFRE risk | 23.1% [12.7%, 50.3%] |
30.2% [15.3%, 53.7%] |
.38 |
Note. PD = peritoneal dialysis; HHD = home hemodialysis; eGFR = estimated glomerular filtration rate; CKD = chronic kidney disease.
Transition Rate and Duration
Of all the patients who completed step 1, 42% completed step 6 and started home dialysis at pilot sites, compared with 35% at control sites (P = .497) at 8-month follow-up (Table 2). When comparing only predialysis patients, 43% at pilot sites compared with 33% at control sites completed step 6 (P = .396). At control sites, 15% of predialysis patients ended up on in-center hemodialysis and 7% passed away compared with 7% and 4%, respectively, at pilot sites by 8-month follow-up (P = .63). By 8 months, 50% of patients who chose PD as their home dialysis of choice had their PD catheter inserted in the pilot group compared with 30% in control (P = .290).
Table 2.
Patient Status by End of 8-Month Follow-Up.
| All patients | Pilot (N = 43) |
Control (N = 65) |
P value |
|---|---|---|---|
| No. of patients who transitioned to PD or HHD | 18 (42%) | 23 (35%) | .497 |
| Home dialysis modality of choice | |||
| PD | 13 | 23 | .0001 |
| HHD | 5 | 0 | |
| Status of patients who did not transition: | |||
| Predialysis | 13 (30%) | 24 (37%) | .40 |
| Transplanted | 1 (2%) | 0 (0%) | |
| Facility-based hemodialysis | 10 (23%) | 13 (20%) | |
| Deceased | 1 (2%) | 5 (8%) | |
| Predialysis patients only | Pilot (N = 28) |
Control (N = 54) |
P value |
| No. of patients who transitioned to PD or HHD | 12 (43%) | 18 (33%) | .396 |
| Status of patients who did not transition: | |||
| Predialysis | 13 (46%) | 24 (44%) | .63 |
| Transplanted | 0 (0%) | 0 (0%) | |
| Facility-based hemodialysis | 2 (7%) | 8 (15%) | |
| Deceased | 1 (4%) | 4 (7%) | |
| PD patients only | Pilot (N = 30) |
Control (N = 65) |
P value |
| No. of patients who had PD catheter inserted | 15 (50%) | 25 (38%) | 0.290 |
Note. PD = peritoneal dialysis; HHD = home hemodialysis.
At the pilot sites, it took patients on average 80 days to complete steps 1 to 6 (transition to home dialysis of choice) compared with 89 days for patients at the control sites (P = .37) (Table 3). For PD patients, the average number of days from step 1 to step 4 (catheter insertion) was 47 days at pilot sites compared with 31 days at control sites (P = .78), while it took 82 vs 89 days to complete transition to PD for pilot vs control patients (P = .58).
Table 3.
Time to PD Catheter Insertion & Home Dialysis Transition for Patients Who Transitioned by 8 Months.
| PD patients only | Pilot (N = 13) | Control (N = 23) | P value |
|---|---|---|---|
| Average time to PD catheter insertion (days) | 47 [11, 78] | 31 [15, 55] | .78 |
| Average time to PD (days) | 82 [43, 135] | 89 [57, 113] | .58 |
| All patients | Pilot (N = 18) | Control (N = 23) | P value |
| Average time to PD or home hemodialysis (days) | 80 [47, 135] | 89 [57, 113] | .37 |
Note. PD = peritoneal dialysis.
Patient Level of Anxiety and Preparation
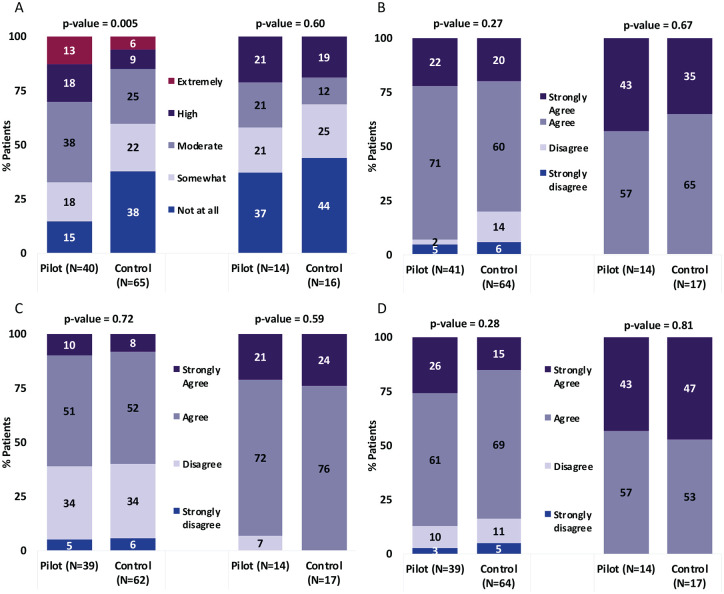
At step 1, pilot patients were significantly more nervous about starting home dialysis compared with control patients (Figure 4A). However, at step 6, there was no significant difference between pilot and control patients, with 58% to 69% of patients feeling “somewhat” to “not at all” nervous about starting home dialysis.
Figure 4.
Patient survey response to feeling nervous about starting home dialysis training (A), feeling prepared to start home dialysis training (B), knowing what questions to ask during transition to home dialysis (C), and having a good understanding of how to manage disease (D).
Patients’ feeling of preparedness for home dialysis and knowledge of what questions to ask during training were not significantly different between pilot and control sites at step 1 and step 6 (Figure 4B and 4C). Their understanding of how to manage their disease were also not significantly different at step 1 and step 6 (Figure 4D). At step 6, for both pilot and control sites, 93% to 100% of responses to feeling prepared, knowing what questions to ask, and understanding how to manage disease were “agree” to “strongly agree.”
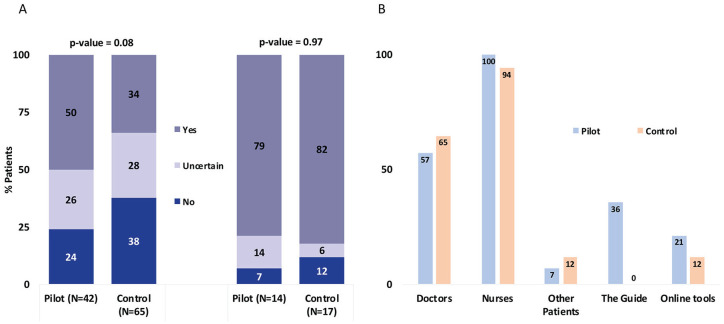
At both pilot and control sites, the proportion of patients who self-reported that they knew what was going to happen at the time of home dialysis training were not significantly different at step 1 and step 6 (Figure 5A). At step 6, 79% to 82% of patients answered “yes” to knowing what to expect at home dialysis training.
Figure 5.
(A) Patient survey response to understanding home dialysis training pre and post transition; (B) % of patients who selected resources used to help with home dialysis training.
Resources Used for Home Dialysis Preparation
At both pilot and control sites, patients used similar resources to prepare for their home dialysis training, with the top choice for both groups being nurses, followed by doctors (Figure 5B).
The only difference between the groups was that the pilot sites had access to the Guide. However, only 36% of patients at pilot sites overtly stated using the Guide as their resource for preparation (Figure 5B).
Patient Feedback on Transitioning to Home Dialysis
Ten patients (5 from the pilot sites and 5 from control sites) participated in structured qualitative interviews discussing the quality and quantity of information received at 3 prespecified time points during the transition process—steps 1, 4, and 6. Specific feedback regarding the guide was asked of the pilot site participants. Illustrative quotes are shown in Table 4.
Table 4.
Illustrative Quotes From Patient Interviews.
| Feedback | Illustrative quotes |
|---|---|
| Step 1 | “They were pretty straightforward about it, I knew exactly what I was going through.” “For someone fully employed, it was difficult to manage time around these appointments and training.” “I had information session with doctor and nurses in Vancouver, they gave me information on how it works [ . . . ] They were helpful.” “Maybe they could go a little deeper into the issues, with both the types of dialysis like PD and hemo . . . more detail.” “[I] did a lot of research on my own and some info from the agency.” “I got a bunch of brochures, CD’s about PD [ . . . ] it was helpful because I didn’t know anything about what PD was at that time. Everything became more clear after going through the info they provided.” “I think they should cover a little bit more at that time and to make it more clear to the families because [they] are the ones who are taking care of the dialysis.” “[Significant things left out:] dialysis solutions and their impacts on the body, dietary changes.” |
| Step 4 Control | “Would like more nitty gritty of how the catheter works.” “Overall I wasn’t nervous about starting PD because I knew I’m at this point, except for the catheter insertion, I was a little nervous about that, but the nurse was so good, she told me it will be a little painful but that I will be okay.” The nurse and doctors explained everything to me so I knew what to expect; they explained everything to me in detail” |
| Step 4 Pilot | “Info up to this point was enough, was acceptable.” “[I was given] enough information to make me interested in doing it and once I did it I liked it.” “[knowing what to expect was] important for preservation of mind.” “Most valuable piece of info[ . . . ]ones that explained the dialysis and how it worked.” |
| Step 6 Control | “Nothing surprising; they made everything clear.” “They showed you everything, it was quite good.” “They come to my home, check my supplies, make sure they know where I’m doing the PD and it was all good” |
| Step 6 Pilot | “They were pretty knowledgeable and what they passed onto me I retained and I haven’t had a problem.” “I prefer being told than reading.” “[Training was] more than enough, but great.” “The binder given to me was very good; [it] would be useful if they gave it out before the catheter insertion.” |
| About the Guide | “Yea I did read it, it was helpful. I read everything they gave me.” “I found it quite interesting.” “Book was fine, self-explanatory.” “For someone going in blind, it’s very useful and written in a way that’s easy to understand with good diagrams.” |
Note. PD = peritoneal dialysis.
Step 1
Both pilot and control site patients were equally diverse in their views on the quality and quantity of information. The groups were analyzed together as the Guide was given out at step 1.
With regard to quantity of information, patients had discrepant views—some felt that they did not receive enough information, others felt that they received the perfect amount, or too much. Patients felt that they received a lot of written information: “I got a bunch of brochures, CD’s about PD,” and felt that the verbal information from nursing staff was helpful: “information sessions were great.”
When discussing the quality of information, some patients wanted more detailed information at that time point: “I wish they could go deeper into issues,” and felt that important information has been left out, such as “information on dialysis solutions and their impacts on the body, dietary changes.” One patient wanted specific information outlining additional appointments and timelines that needed to occur after choosing PD because “for someone fully employed it was difficult to manage time around these appointments.” Another patient pointed out that it was important to engage families at this step because “they are the ones taking care of the dialysis” in some circumstances.
Step 4
During Step 4, patients in the control group felt that they wanted more detailed information about the catheter insertion and did not feel that they received enough of it. The information they received was obtained from the Kidney Care Clinic (KCC): “the nurses and doctors explained everything to me.”
In the pilot group, most patients felt that the level of information they received was acceptable, but would have liked to receive it earlier. The information they received was obtained from the KCC, booklets, and online resources. Some of the most valuable information received thus far included information on “dialysis, explaining how it worked.”
Step 6
During step 6, patients in the control group felt pleased with the amount and quality of information that they have received: “nothing surprising; they made everything clear.” The hands-on learning was helpful: “they show you everything; it was quite good.”
Similar findings were expressed by the pilot group. They felt that the training was “more than enough,” and stated preference for hands-on learning and verbal information rather than learning through reading: “I prefer being told than reading.”
Feedback on the Guide
When specifically asked about the Guide, the pilot site patients felt that “the book was fine, self-explanatory.” They felt that it was a useful resource for someone who is just starting to learn about home dialysis. Many found it interesting, effective, and helpful. Patients did not use it during the entire transition period and tended to read the Guide once at the time that it was given out.
MDT Feedback
Preimplementation written survey
Ten MDT members participated in the preimplementation written survey. The majority of staff had a general idea of the steps of transition from CKD to PD/HHD, although knowledge was not standardized. When asked to list the 6 steps, steps 2 (PD/HHD will start in 6 months) and 3 (it’s time to have the PD catheter/hemodialysis access inserted/created) were less frequently referenced. Steps 3 to 4 (catheter has been inserted) were most often lumped together as “PD catheter insertion.”
Most staff felt that their role was answering patients’ questions and referring them to appropriate MDT members, reducing anxiety, and increasing comfort with PD/HHD. They felt that the Guide would help reduce anxiety, improve patients’ understanding of the process, and improve their comfort with the transition process.
Major barriers to a successful transition mentioned included anxiety or fear of the unknown, lack of knowledge of what to expect, denial, and feeling overwhelmed. Most staff felt that a standardized approach to this transition would help improve patient outcomes.
Postimplementation group feedback
Seven MDT members participated in the postimplementation group feedback session.
The MDT members reported that they received positive feedback from patients with regards to the Guide. They found the Guide to be helpful: “100% valuable, one more piece of information to make the transition better for patient.” It helped the MDT provide a “framework for other information that we give to patients.” They felt that the Guide “was very well done” and “did not need changes.” They did not feel that the Guide increased their workload. Although the Guide was a useful tool for the MDT at step 1, they did not find that patients referred to it during the transition process again.
Ideas regarding implementation focused on timing of giving out the Guide, who gives out the Guide, and incorporating the Guide into the transition period. With regard to timing, most MDT members felt that it should be given out as early as possible, “we like having it at the orientation, it outlines the discussion nicely.” They felt that the latest time to introduce the Guide would be after the PD/HHD orientation. Most MDT members felt that the Guide could be given out by any of the MDT members including the PD/HHD nurses, social workers, and KCC staff. When discussing how to best incorporate the guide into daily practice, ideas included asking patients to bring it to each visit “like their medications.” Making posters of steps 1 to 6 to put up in common areas was a popular suggestion to help keep the Guide relevant during appointments. During appointments with patients, using the same language as introduced in the Guide for the different transition steps was felt to be useful by the MDT members to keep patients and the health care team on track.
Discussion
In this Canadian provincial quality improvement study, we demonstrate a systematic evaluation strategy to test the utility of a newly developed Transition to Home Dialysis Guide. While significant differences in transition rate and duration between pilot and control sites were not found, this study has shed light about patients’ experiences during transition to home dialysis, and that the transition process is unique for every individual.
Although our survey results did not show notable differences between patients at pilot and control sites with regard to level of anxiety and preparedness at step 6, we infer that pilot patients had a greater improvement from step 1 to step 6 in level of anxiety. This is seen as the baseline level of nervousness was significantly higher in pilot group compared with control group at step 1, but at step 6 there was no significant difference. However, this was not a formal comparison, a limitation of our study, since surveys were collected anonymously and we could not compare paired responses from the same individual.
When asked to rate their resources used during transition, the top choice for both groups is nurses, followed by doctors. This is consistent with other studies which have shown that patients valued support from physicians, nurses, and peers, although in our study peer support was not as crucial to our patient population.2 While only 36% of patients at pilot sites overtly stated the Guide as one of their resources, we feel this may be due to the manner in which the question was asked on the survey (specifically asking about preparing for training rather than transition in general). Patients are provided with many resources throughout their transition process and may not remember the specific name of the Guide and neglect the choice on the survey. Having many resources may have led to insufficient direct exposure to the Guide at pilot sites, patients may see the Guide as a tool but not as a resource they refer to when trying to understand home dialysis. Finally, as MDT at pilot sites refer to steps in the Guide when educating patients, the information would have been received by the patients without having personally read the Guide at home. This could also have indirectly increased the transition rate seen in our study.
While studies have shown that the approach and attitude toward transition to home dialysis may differ between patients and staff,13 it is reassuring to receive feedback from MDT that the Guide did not increase their workload, and in fact assisted them in speaking a common language with patients. As previous studies have noted that patients consider predialysis training to include any informal conversations with staff,13 having the Guide to refer to between MDT and patients may provide more clarity.
The diversity of responses we received in our qualitative interviews, particularly at step 1, reflected the diverse population we serve across the province. The overall discrepancy in the quantity and type of information patients would like to receive at this time, similar between both pilot and control sites, is as expected due to diverse learning styles in patients.14 This speaks to the challenge of implementing initiatives in general, as there is seldom a solitary solution for the entire population. At Steps 4 and 6, for both control and pilot groups, hands-on learning at the KCC sessions was something patients appreciated and found most useful, rather than reading information. This has been shown in previous studies on predialysis education.13 One of the suggestions that recurred was the preference of receiving information earlier, particularly at pilot sites, consistent with suggestions for optimal dialysis transition in the 2012 review by Saggi et al.15 Thus, this should be kept in mind when selecting the optimal timing for distributing the Guide. Due to the nature of this quality improvement project, we did not have a large number of interviewees and responses were not formally analyzed through qualitative methodology. We also recognize that we did not interview patients who were not successfully transitioned to home dialysis by 8 months. Future studies may benefit from understanding why patients do not transition to their home dialysis of choice in a timely manner.
While this study utilizes a structured approach to evaluate a province-wide initiative, there are some additional limitations. Despite comparable demographics between control and pilot sites, there are still inevitable differences in the structure and culture at each site. Differences for staff including availability and workload may affect the transition process for patients. Other factors influencing transition time not accounted for in this study included hospitalizations, social supports, and economic challenges of relocating for training, especially in rural locations. As well, there were very few patients starting on HHD during our study period and we were unable to find HHD patients in our control sites. The results from the study are therefore more specific for PD and may not be readily applicable to HHD. Moreover, the patients who successfully completed their transition to home dialysis during our study period may be more motivated individuals with potentially better health literacy or supports, and perhaps had fewer adverse outcomes which shortened their transition time. Thus, they may not be wholly representative of all patients who transition to a home modality. Furthermore, it is important to note that many patients who did not transition at the 8-month point were predialysis patients (as opposed to cHD patients) and may not have developed indications for dialysis yet. This would indicate that transition time as an outcome may not be the optimal metric to compare pilot and control patients. Lastly, while interview questions specifically inquired about different timeframes, we relied on patients’ memory as the interviews were conducted retrospectively, after the patients completed their home dialysis training.
Conclusion
In summary, using the Guide along with the expertise of the MDT provides a perceived benefit in supporting patients through the transition period to HDT (particularly for PD). The systematic evaluation of this provincial quality improvement initiative yielded valuable information for further projects. It not only revealed relevant perspectives from both patients and staff with regard to transition to home dialysis, but also highlighted the importance of evaluating all quality improvement initiatives strategically.
Supplemental Material
Supplemental material, 200425_Transition_to_HDT_Appendix for Systematic Evaluation of a Provincial Initiative to Improve Transition to Home Dialysis Therapies by Alice Wang, Linda Turnbull, Janet Williams, Sarah Thomas, Sushila Saunders, Adeera Levin, Ognjenka Djurdjev, Michael Copland, Suneet Singh and Juliya Hemmett in Canadian Journal of Kidney Health and Disease
Acknowledgments
We thank Lee Er for her support in statistical analysis.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Juliya Hemmett  https://orcid.org/0000-0003-3167-844X
https://orcid.org/0000-0003-3167-844X
Supplemental Material: Supplemental material for this article is available online.
References
- 1. Turin TC, Coresh J, Tonelli M, et al. Short-term change in kidney function and risk of end-stage renal disease. Nephrol Dial Transplant. 2012;27(10):3835-3843. https://www.narcis.nl/publication/RecordID/oai:pure.rug.nl:publications%2Ff014d63f-aec9-47be-b73d-53a70d2dcc5f. Accessed August 6, 2020. [DOI] [PubMed] [Google Scholar]
- 2. Sauvé C, Vandyk AD, Bourbonnais FF. Exploring the facilitators and barriers to home dialysis: a scoping review. Nephrol Nurs J. 2016;43(4):295-308. https://www.ncbi.nlm.nih.gov/pubmed/30550056. Accessed August 6, 2020. [PubMed] [Google Scholar]
- 3. Beaudry A, Ferguson TW, Rigatto C, Tangri N, Dumanski S, Komenda P. Cost of dialysis therapy by modality in Manitoba. Clin J Am Soc Nephrol. 2018;13(8):1197-1203. https://www.ncbi.nlm.nih.gov/pubmed/30021819. Accessed August 6, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. MacGregor MS, Agar JWM, Blagg CR. Home haemodialysis—international trends and variation. Nephrol Dial Transplant. 2006;21(7):1934-1945. https://www.ncbi.nlm.nih.gov/pubmed/16537659. Accessed August 6, 2020. [DOI] [PubMed] [Google Scholar]
- 5. Canadian Institute for Health Information, Access Data and Reports. “CORR annual statistics: renal replacement therapy (dialysis and kidney transplantation) for ESKD, 2009 to 2018.” https://www.cihi.ca/en/access-datareports/results?query=dialysis&Search+Submit=.Published2019. Accessed August 6, 2020.
- 6. MorfÃ-n JA, Yang A, Wang E, Schiller B. Transitional dialysis care units: a new approach to increase home dialysis modality uptake and patient outcomes. Semin Dial. 2018;31(1):82-87. https://onlinelibrary.wiley.com/doi/abs/10.1111/sdi.12651. Accessed August 6, 2020. [DOI] [PubMed] [Google Scholar]
- 7. Mendelssohn DC, Malmberg C, Hamandi B. An integrated review of “unplanned” dialysis initiation: reframing the terminology to “suboptimal” initiation. BMC Nephrology. 2009;10(1):22. https://www.ncbi.nlm.nih.gov/pubmed/19674452. Accessed August 6, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Golper TAMD, Saxena ABMD, Piraino BMD, et al. Systematic barriers to the effective delivery of home dialysis in the United States: a report from the Public Policy/Advocacy Committee of the North American Chapter of the International Society for Peritoneal Dialysis. Am J Kidney Dis. 2011;58(6):879-885. https://www.clinicalkey.es/playcontent/1-s2.0-S0272638611011437. Accessed August 6, 2020. [DOI] [PubMed] [Google Scholar]
- 9. W. K. Kellogg Foundation, Logic Model Development Guide. W.K. Kellogg Foundation logic model development guide. https://www.bttop.org/sites/default/files/public/W.K.%20Kellogg%20LogicModel.pdf. Accessed August 6, 2020.
- 10. Osuch E, Vingilis E, Summerhurst C, Demy J, Wammes M, Arcaro J. Process evaluation of a treatment program for mood and anxiety disorders among emerging adults: preentry factors, engagement, and outcomes. Psychiatric Services. 2019;70(3):211-218. 10.1176/appi.ps.201800219. Accessed August 6, 2020. [DOI] [PubMed] [Google Scholar]
- 11. Terio M, Eriksson G, Kamwesiga JT, Guidetti S. What’s in it for me? a process evaluation of the implementation of a mobile phone-supported intervention after stroke in Uganda. BMC Public Health. 2019;19:562 http://urn.kb.se/resolve?urn=urn:nbn:se:uu:diva-387283. Accessed August 6, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. West JF. Public health program planning logic model for community engaged type 2 diabetes management and prevention. Eval Program Plann. 2014;42:43-49. https://www.sciencedirect.com/science/article/pii/S0149718913000803. Accessed August 6, 2020. [DOI] [PubMed] [Google Scholar]
- 13. Combes G, Sein K, Allen K. How does pre-dialysis education need to change? findings from a qualitative study with staff and patients. BMC Nephrology. 2017;18(1):334 https://www.ncbi.nlm.nih.gov/pubmed/29169332. Accessed August 6, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. McLaughlin K, Jones H, VanderStraeten C, et al. Why do patients choose self-care dialysis. Nephrol Dial Transplant. 2008;23(12):3972-3976. https://www.ncbi.nlm.nih.gov/pubmed/18577531. Accessed August 6, 2020. [DOI] [PubMed] [Google Scholar]
- 15. Saggi SJ, Allon M, Bernardini J, Kalantar-Zadeh K, Shaffer R, Mehrotra R. Considerations in the optimal preparation of patients for dialysis. Nat Rev Nephrol. 2012;8(7):381-389. https://www.ncbi.nlm.nih.gov/pubmed/22487703. Accessed August 6, 2020. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, 200425_Transition_to_HDT_Appendix for Systematic Evaluation of a Provincial Initiative to Improve Transition to Home Dialysis Therapies by Alice Wang, Linda Turnbull, Janet Williams, Sarah Thomas, Sushila Saunders, Adeera Levin, Ognjenka Djurdjev, Michael Copland, Suneet Singh and Juliya Hemmett in Canadian Journal of Kidney Health and Disease