Abstract
Background
How to cope with the rapid growth of LTC (long-term care) needs for the old people without activities of daily living (ADL), which is also a serious hazard caused by public health emergencies such as COVID-2019 and SARS (2003), has become an urgent task in China, Germany, Japan, and other aging countries. As a response, the LTCI (long-term care insurance) system has been executed among European countries and piloted in 15 cities of China in 2016. Subsequently, the influence and dilemma of LTCI system have become a hot academic topic in the past 20 years.
Methods
The review was carried out to reveal the effects of the LTCI system on different economic entities by reviewing relevant literature published from January 2008 to September 2019. The quality of 25 quantitative and 24 qualitative articles was evaluated using the JBI and CASP critical evaluation checklist, respectively.
Results
The review systematically examines the effects of the LTCI system on different microeconomic entities such as caretakers or their families and macroeconomic entities such as government spending. The results show that the LTCI system has a great impact on social welfare. For example, LTCI has a positive effect on the health and life quality of the disabled elderly. However, the role of LTCI in alleviating the financial burden on families with the disabled elderly may be limited.
Conclusion
Implementation of LTCI system not only in reducing the physical and mental health problems of health care recipients and providers, and the economic burden of their families, but also promote the development of health care service industry and further improvement of the health care system. However, the dilemma and sustainable development of the LTCI system is the government needs to focus on in the future due to the sustainability of its funding sources.
Keywords: aging society, LTC, long-term care, LTCI, long-term care insurance, fund-raising, effectiveness, dilemma
Introduction
The aging of the global population has created an enormous demand for LTC (Long-Term Care) for the old people without activities of daily living (ADL) and with a heavy financial burden on their family.1 The European and American countries, such as the Netherlands in the 1960s and the United States in the 1970s, have introduced LTCI (Long-Term Care Insurance), but it exists only as a kind of insurance under the Health insurance. In 1995, Germany took the lead in setting up LTCI (Long-Term Care Insurance) system, which became the sixth largest independent insurance system after health insurance, unemployment insurance and other insurance systems. To a large extent, it meets the needs of LTC services for the elderly and alleviates the poverty of the elderly caused by personal payment.2
LTCI system, including public LTCI (government-mandated) and private LTCI (individual voluntary), refers to an institutional arrangement to share the nursing expenses incurred by people who cannot take care of themselves due to chronic diseases or physical and psychological disability (WHO).3 The European and American countries have their characteristics in the specific implementation policies of the LTCI system, such as fundraising. For example, Germany was the first country to implement the LTCI system in the form of social legislation. In 1995, the LTCI law came into effect and became the fifth pillar insurance, along with endowment insurance, medical insurance, accident insurance, and unemployment insurance. German LTCI system emphasizes two essential principles, namely, “Home care priority” and “Prevention and rehabilitation priority.” All medical insurance policyholders must attend the LTCI, regardless of gender or age as long as an adult. LTCI system in Germany emphasizes the “peer-to-peer” rights and obligations (Beneficiaries must pay certain fees in advance).4,5 Another type of LTCI system is the full coverage model of LTCI benefits in the Nordic. In addition, Japan, the East Asian countries' neighbors of China, have implemented LTCI system since 2000. All the applicants can decide the care level in the amount available and the care beyond a fixed amount must be undertaken privately. All of them are all facing sustainable development problems because of the lack of funds.
In China, private LTCI is still in its infancy, while public LTCI is partly funded by medical insurance, and together with general SOSS (Social Old-age Service Security), such as endowment insurance, forms part of the provision of health services for the elderly. It is different between LTCI and SOSS. First, SOSS mainly provides daily life for the elderly, while LTCI not only includes life help but also includes health care and psychological comfort. Second, SOSS is funded by public finance grants, welfare lotteries, and individual contributions. LTCI (public LTCI in China mainly) was made up of part of medical insurance, which paid by employers, employees, and the government financial burden. Third, SOSS mainly provides free or low-fee services for the “Three no” (no work, no income, no provider) elderly, and disabled or semi-disabled elderly, while LTCI offers different services for the corresponding time according to the disability level identified when the elderly apply for services.
The rapid aging of the population has emphasized the emergency of health care for the old people in China. The elderly without activities of daily living (ADL) caused by chronic diseases, environmental pollution, or accidental injuries is increasing, and the prevalence rate of chronic diseases in the elderly is as high as 54%.6–10 Although the LTC services demand for the elderly was snowballing, the provision of LTC services such as fundraising far from keeping up with its demand. As a countermeasure, the public LTCI system was piloted in 15 cities since 2016, including Qingdao of Shandong province, Chengdu of Sichuan province, and Chongqing, which had a profound impact on the people and economies of the pilot areas (as shown in Table 1). The implementation of LTCI system in China has produced certain economic and social impacts, but due to its short implementation time, the policy effect is not significant enough, and relevant academic research is not in-depth enough, so there is still a lot of research space in both quantitative and qualitative research.
Table 1.
Long-Term Care Insurance in Part of LTCI Pilot Cities in China (Unit: RMB)
| City | Start Time | Institution Care Expenditure | Home Care Expenditure | Community Care Expenditure |
|---|---|---|---|---|
| Qingdao | July, 2012 | 65 yuan/person/day | 50 yuan/person/day | 1600 yuan/year |
| Chongqing | March, 2018 | 26 yuan/day for severely disabled persons, 20 yuan/day for moderately disabled persons. | – | 30 yuan/day for severely disabled, 25 yuan/day for moderately disabled. |
| Changchun | May, 2015 | LTCI pays 70% and reimburses 750 yuan for the whole month | 25 yuan/person/day | LTCI pays 70% and reimburses 750 yuan for the whole month |
| Qiqihar | October,2017 | LTCI pays 55%,25 yuan/person/day | LTCI pays 50% | LTCI pays 50%,20 yuan/person/day |
| Jingmen | December, 2016 | LTCI pays 75%,100 yuan/person/day | 40 yuan/person/day | LTCI pays 80%,100 yuan/person/day |
| Chengdu | July, 2017 | LTCI pays 70% | LTCI pays 75% | – |
| Nantong | January, 2017 | 50 yuan/person/day | – | 1200 yuan/month |
| Guangzhou | April, 2017 | LTCI pays 75%, 120 yuan/person/day | LTCI pays 90% | LTCI pays 75% |
| Anqing | January, 2017 | LTCI pays 50%,40 yuan/person/day | 750 yuan/month | 750 yuan/month |
| Ningbo | December, 2017 | 60 yuan/person/day | 50 yuan/person/day | 50 yuan/person/day |
| Shanghai | January, 2018 | LTCI pays 85% | LTCI pays 90% | LTCI pays 90% |
Note: The results were summarized according to the pilot program of pilot cities.
The implementation of LTCI system in China has produced specific economic and social impacts, but due to its short implementation time, the policy effect is not significant enough, and relevant academic research is not in-depth enough. In view of the high rate of disability and deaths among the elderly of SARS (2003) and COVID-2019, it is imperative to deepen the LTCI system in the “post- COVID-2019 era” in order to mitigate the negative impact of COVID-2019 and similar public health emergencies that may occur again in the future. The purpose of this paper is twofold: a) Systematically sorted the existing related literature at China and abroad, aimed at the impact of LTCI system on the microscopic economic entities such as nursing care recipients and the family, as well as to the macroeconomic entities such as national economy, social welfare, etc. And then try to find out the LTCI system development, continue to deepen the research direction and space, and put forward further research prospects. b) Learn from the experiences of the LTCI system in other countries and further promote the in-depth reform of the LTCI system in China by comparing the social welfare impact of the LTCI system in China with other countries.
Materials and Methods
The review was implemented to reveal the effects of the LTCI system on different economic entities by reviewing relevant literature published from January 2008 to September 2019.
Design
This review methodology followed the checklist presented by PRISMA (the Project for Systematic Review and Meta-Analysis Preferred Reporting), which is useful for critical appraisal of published systematic reviews, although it is not a quality assessment tool to measure the quality of a systematic review. Meanwhile, this review used JBI Critical Appraisal Checklist to evaluate the quality of the quantitative research, and the Critical Appraisal Skills Programme (CASP) to assess the quality of the qualitative research.
Search Process and Inclusion Criteria
The following primary databases were taken into account: Web of Science (WOS), PubMed, Medline, CNKI (China), and WanFangData (China) with time filter January 2008 to September 2019. The following mixtures of nouns were practiced under the word “and/or” to top limit the range and type of material searched: “LTCI” OR “Long-Term Care Insurance” and “economic” AND “effect”. The review is included in the study published before September 2019 when our review begins writing, and not included the conference summary or editorials. Finally, 49 articles were retained for the review.
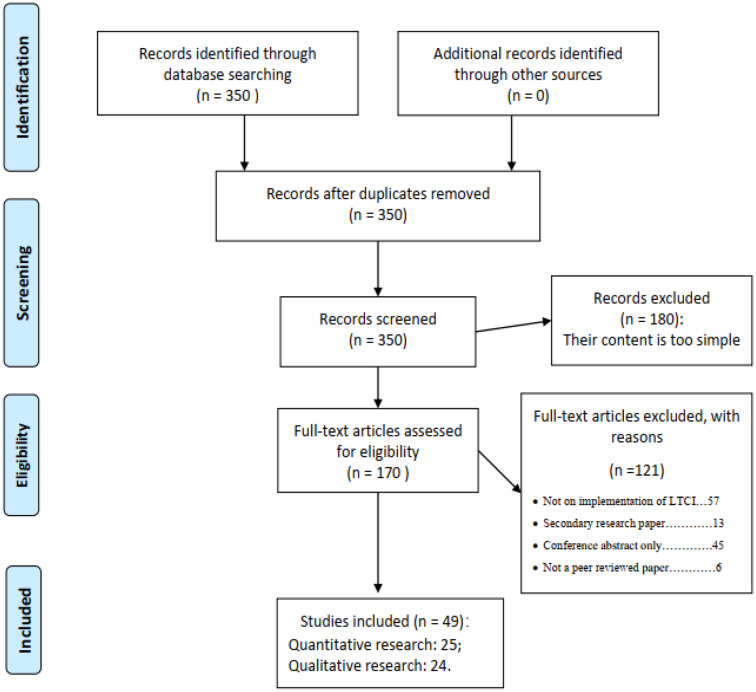
Data Extraction Process
Our review methodology followed the checklist presented by PRISMA (the Project for Systematic Review and Meta-Analysis Preferred Reporting), which was published in 2009 and consists of a checklist and a flow diagram.11 Three reviewers appraised the studies for inclusion. The material extracted from the included publication included the study purpose, analysis tools, outcome measurements, and time frames. The data extraction process is made in Figure 1.
Figure 1.
Data extraction process (PRISMA).
Note: Adapted from Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group (2009). Preferred Reporting Items for Systematic Review and Meta-Analyses:The PRISMA Statement. PLoS Med 6(7):e1000097.11
Quality Appraisal
The JBI Critical Appraisal Checklist was used to evaluate the quality of the 25 quantitative articles, and The Critical Appraisal Skills Programme (CASP) was used to assess the value of the 24 qualitative articles.
Firstly, we assessed the quality of each article based on the JBI Critical Appraisal Checklist. As designed for use in systematic reviews, JBI (Joanna Briggs Institute) Critical Appraisal Tools have been developed by the JBI Scientific Committee following extensive peer review. All features of the study that meet the following eight criteria are included in the final summary: (1) distinct purpose; (2) complete information of sample variable; (3) data foundation; (4) the effective of data sorting; (5) thought of ethical rules; (6) suggestions; (7) effective results; and (8) application of an appropriate quantitative methodology and clearly stated findings.12 The methodological quality was appraised by the yes/no questions listed in the JBI Critical Appraisal Checklist. Averagely, each article concerning analytics scored 7.5 out of 8. Out of 25 articles, seven articles did not detail the data source. Secondly, the CASP (Critical Appraisal Skills Programme) checklist was used to assess the quality of the 24 qualitative articles. Critical Appraisal Skills Programme (CASP) was developed in 1993 and helped develop an evidence-based approach to health and social care.13 Five questions (out of 10) in the checklist were not appropriate to the qualitative articles. So, we assessed the articles on a 5-point scale. Articles included in our review displayed high methodological quality as 18 articles (out of 24) scored 5. We adopted the three-step processing method proposed by Levy.et al14 to summarize the knowledge system. First, during the review process, we extract the information we need by identifying the title, defining the problem, and listing the more critical findings. We then compared each article with articles related to similar issues to ensure that no irrelevant information was considered. The final relevant information was aggregated and stored in Excel. The final classification provides abstracts, conclusions, and possible reviewer comments for different articles.
Results
A Brief Review of Relevant Literature
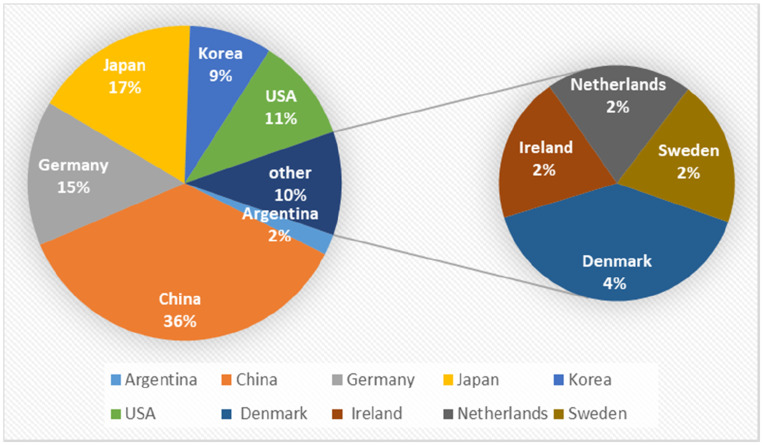
The review includes 49 articles, of which 25 are quantitative articles, and 24 are qualitative articles. Our results showed that qualitative or quantitative analysis accounted for roughly half of all the literature, but qualitative research accounted for 72% of the literature in Chinese, while quantitative research accounted for 80.7% of the literature in English. Besides, more and more articles have been published on the influence of LTCI system, especially in the last 2 years (2018 and 2019) accounted for more than 50% of all relevant papers published in this decade. Furthermore, the classification of articles published focused on the influence and dilemma of LTCI system in different countries is presented in Figure 2.
Figure 2.
Classification of publication by country studied.
As can be seen from Figure 2, of all 49 articles, the most studied countries are China, Japan, Germany, the United States, and South Korea. There was some literature on the study of Nordic welfare states such as Denmark and Sweden, but the number is not large. In addition, few studies on the LTCI system in developing countries except China. For example, a well-known scholar named Lloyd-sherlock has published several articles focused on Argentina and studies the availability of LTC infrastructure and formal services for the old people.15,16
Micro Perspective: Effects of LTCI on Caretakers and Their Families
As shown in Table 2, from the point of view of the microscopic subject, the influence of LTCI (Long-Term Care Insurance) was mainly reflected in the effects on the health and quality of life of the caretakers, the financial burden on the caretakers and their families, and the choice of different types of care, etc.
Table 2.
Literature Related to the Impact of LTCI on Caretakers and Their Families
| Author, Date | Publication | Sample | Methodology | Sample Period | Key Findings |
|---|---|---|---|---|---|
| Purpose 1: Effects of LTCI on the health and quality of life of the caretakers | |||||
| Choi and Joung (2016)17 | Arch Gerontol Geriatr | Korea | Cox proportional hazard regression | January 2009–April 2012 | They used Cox models to identify the effect of service utilization on mortality while adjusting for covariates. It is found that the hazard ratio of participant death of those using long-term care services was significantly lower than for those who did not use these services. |
| Lee et al (2019)18 | Int J Geriatr Psychiatry | Korea | Logistic regression | 2008–2009 | The propensity score matching method was used, yielding 416 participants in each group. Paired samples t‐tests and logistic regression analyses were conducted and found that cognitive function and disability declined less in the LTCI care group. |
| Milte et al (2019)19 | Ageing & Society | Argentina | Qualitative methodologies | 2016–2017 | The paper conducted a clandestine audit by older people living in the community and found that there has been a rapid growth in the availability of formal services, but that there are many gaps in provision, especially for older people with complex care needs. |
| Purpose 2: Effects of LTCI on the financial burden on the caretakers and their families | |||||
| Sugiyama et al (2018)20 | Geriatrics & Gerontology International | Japan | Cross-sectional analysis | 2010 | The present study was a cross-sectional analysis of nationally representative data in Japan (2010 Comprehensive Survey of Living Conditions). It is found that, facilitating health check-up participation for family caregivers of care recipients with higher care-need levels might be an effective intervention for decreasing the gap in health behavior possibly caused by informal caregiving. |
| Iwamoto and Saito (2010)21 | Journal of the Japanese and International Economies | Japan | Investigation | 2001 | They only use the sample of households whose household head is an employee. It is found that, publicly financed home care may have limited impact among the abler, but that it may be both more cost-effective and beneficial than institutional care for the least prepared. |
| Tamiya (2011)22 | The Lancet | Japan | Systematic review | 1998–2004 | They used the data from academic published work to review the effect of the long-term care insurance system in Japan and found that increasing the use of formal health care at lower family costs has had mixed results for career well-being. |
| Chen Fei (2013)23 | Times finance | China | Qualitative analysis | 2011 | Long-term care insurance can effectively reduce the cost of providing for the aged and reduce the double burden of family economic life. |
| Kim and Lim (2015)24 | Journal of Public Economics | South Korea | Regression discontinuity design | 2008–2010 | They used administrative data to estimate the first-year impact of subsidies for formal home and institutional care on informal care use and medical expenditures. It is found that, publicly financed home care may have limited impact among the abler |
| Purpose 3: Effects of LTCI on nursing workforce providers | |||||
| GeyerandKorfhage (2015)25 | Health Econ | Germany | Structural model | 2001–2010 | They use a mixed logit with random coefficients to estimate the random utility maximization and found that benefits in kind have small positive effects on labor supply. Labor supply elasticities of cash benefits are more significant and negative. |
| Sakka (2019)26 | Geriatr Gerontol In | Japan | Cross-sectional study | March 2015 - July 2016 | They used structural equation modeling (SEM) and found that the decrease in care burden is significant for employed family caregivers to reduce their FWC and maintain their work-life balance. |
| Umegaki et al (2014)27 | Arch Gerontol Geriatr | Japan | x2 analysis | April 2010 | Lower age of caregivers, a more advanced need classification level, and more satisfaction with the services were independently associated with a reduction of the care burden. |
| Purpose 4: Effects of LTCI on the choice of different types of care | |||||
| Schmitz and Westphal (2015)28 | J Health Econ | Germany | Propensity score method | 2002–2010 | They used the model of Rubin (1974) to estimate the effect and found that there is a considerable negative short-term effect of informal care provision on mental health, which fades out over time. |
| Gao (2019)29 | Chinese medical insurance | China | Logistics regression | From July to September 2017 | There are three phenomena in adult long-term care: first, more than half of the interviewees have experienced long-term care; second, more than half of the interviewees support the view that young people should be prepared for long-term care; third, more than half of the interviewees prefer home (community) care. |
| Coe, et al (2015)30 | J Health Econ | USA | Microscopic investigation | 1998–2006 | It test if expectations about future informal care receipt, and LTCI purchase decisions vary between individuals whose parents or in-laws have used LTC versus those who have not. They found parental use of a nursing home decreases expectations that one’s children will provide informal care. Nursing home use by either a parent or in-law increases LTCI purchase probability by 0.8 percentage points. |
| Tsai (2015)31 | J Health Econ | USA | Empirical research | 1999–2000 | They used the Second Longitudinal Study of Aging (LSOA II) and found that, as retirement incomes rise, older people are increasingly using formal care and relying less on informal home care provided by their children. |
| Lehnert, et al (2018)32 | Eur J Health Econ | Germany | Preferences Discrete choice experiment | 2015.12–2016.06 | Preferences and marginal willingness to pay (WTP) for HCBS were assessed with respect to five HCBS attributes. It is found that in light of the great importance of high care quality to respondents, reimbursement for services by HCBS providers could be more strongly linked to the quality of services. |
Effects of LTCI on the Health and Quality of Life of the Caretakers
The effects on the health of the disabled elderly are the primary objective of LTCI implementation. Choi and Joung used Cox proportional risk regression model to prove that LTCI services can help reduce health expenditure and protect the health of the elderly aged 65 and above.17 Lee et al compared the changes in cognitive function, behavioral symptoms, and physical function of Korean LTCI care and individual care in 1 year and found that the elderly experienced less cognitive decline and decreased disability progression in LTCI care.18 Milte et al found a strong association between processes of care delivery and quality of life of care recipients.19 All the theoretical research is becoming more and more in-depth, which were conducted from the perspectives of different age groups, nursing time, and health recovery degree, etc.
Effects of LTCI on the Financial Burden on the Caretakers and Their Families
Most studies have confirmed that LTCI can help reduce the financial burden on families with the disabled elderly. Sugiyama et al believed that Japan’s public compulsory LTCI system alleviated the nursing burden of home caregivers for the elderly.20 Iwamoto and Saito found that LTCI (Long-Term Care Insurance) helps Japanese families to reduce the welfare losses associated with disabled family members.21 Other Japanese scholars Tamiya have different views, and he thinks the LTCI was challenged by the dissatisfaction of necessary support for the family caregivers and the sustainability of the system.22 Chinese scholar Chen et al believed that LTCI could effectively reduce the cost of old-age care and the double burden of family economic life because of the shrinking family size, the soaring number of empty-nest families, and the rising nursing costs in China.23 Other researchers have taken this step further by dividing dysfunctional elderly families into high-income and low-income families, for example, Kim and Lim found that in South Korea, government nursing subsidy can lead to an increase in the use of formal long-term care but has a limited impact on people with better income status.24
Effects of LTCI on Nursing Workforce Providers
LTCI’s impact on the labor market is not well studied, but it is a meaningful topic that deserves further study. Geyer and Korfhage proposed that home care is generally considered as a cost-saving alternative to formal home care and fixed care, but the opportunity cost caused by the reduced supply of caregivers was often overlooked. Many informal caregivers are of working age and face the dual burden of providing care and work.25 Sakka found that the reduction of the burden of care for dementia patients and the reduction of behavioral and psychological symptoms of dementia are of great significance to the reduction of family–work conflict and the maintenance of work–life balance for employed family caregivers.26 Umegaki et al conducted a survey and found that a total of 68.8% of nursing staff said that the introduction of LTCI service reduced the nursing burden, and 86.8% of nursing staff were satisfied with LTCI nursing service.27 These only studies have analyzed the dilemma between going to work and taking care of the disabled elderly facing family members through micro survey research.
Effects of LTCI on the Choice of Different Types of Care
The choice of different types of care is related not only to the wishes of the disabled elderly themselves but also to the wishes of their family members. Schmitz et al used data from the German socio-economic group and found that informal nursing had a considerable negative short-term impact on the mental health of female caregivers, which gradually disappeared over time. After 5 years of care, the effect was still negative, but small and insignificant, with virtually zero short - and medium-term effects on health.28 Gao proposed that parents’ long-term care experience would, in turn, influence their children’s willingness to long-term care.29 Coe et al found that parents’ use of nursing homes reduced people’s expectation of informal care for their children, and parents or in-laws’ use of nursing homes increased the probability of LTCI purchase by 0.8 percentage points.30 Tsai, another scholar, proposed that with the increase of retirement income, higher social security benefits would encourage those who would not otherwise use any home care to use formal home care, and the elderly would be encouraged to use these two types of home care services. Future needs will increasingly include high-demand care for people with cognitive and physical disabilities.31 Lehnert et al proposed that more than half of the respondents preferred home (community) care.32 To sum up, both the disabled elderly and their family members’ choices are related to economic income, social insurance, and other factors.
Macro Perspective: Effects of LTCI on National Economic Welfare (Medical Expenses, Nursing Industry, Finance, etc.)
LTCI system shows the specific influence on the whole social welfare in release effective demand for Long-term care, promote the public health service system to further development, establish the LTCI (Long-Term Care Insurance) system, improving the efficiency of the Long-term care service, etc.
Some scholars believe that LTCI helps release the effective demand for long-term care. For example, Yang thinks that the implementation of the LTCI system in Shandong province not only meets the medical care needs of the disabled elderly but also solves the problem of excessive medical treatment in the previous hospitalization, and achieves the effect of purchasing higher medical care services at a lower cost.33 Jiang argued that LTCI promotes the release of long-term care effective demand and utilization, promote the sustainable development of the medical service system.34
Others have discussed the impact of LTCI on government health spending and the burden on government budgets. For example, Lee argued that LTCI system has a positive impact on Japan’s economy and society, mainly embodied in reducing the burden of the medical expenses of long-term care family and government, ease the phenomenon of long-term care services in short supply and improve the employment level of the Japanese society.35 It is identical to the views of Hao, who argue that Germany’s LTCI system has achieved significant social reform achievements, reduce the state and the individual family’s heavy financial burden on the long-term care spending.36 Li summarized that the LTCI system in Nantong alleviates the economic burden of disabled personnel and promotes the coordinated development of the care system in urban and rural areas.37 Yu used a long synthetic control method to explore nursing risks influence on medical expenses and found that LTCI can effectively adjust the allocation and utilization of medical resources and fundamentally improve the overall social welfare.38 Geyer and Korfhage used the Labor supply structure model to quantify the indirect financial effects of informal care and showed that increasing formal care subsidies through LTCI had a considerable positive impact on the government budget.39
In addition to the above, other studies have focused on the impact of LTCI on the health care service industry in various regions. Shao found that LTCI of Qingdao is not only solved the problem of long-term care for the disabled elderly but also mobilized the rational allocation of medical resources and the full use of nursing insurance funds, which promoted the development of the elderly care industry and the nursing service industry.40 Shen.et al established a systematic GMM model based on relevant data in China statistical yearbook and operation analysis report of national medical and maternity insurance from 2010 to 2017 and found that LTCI can significantly improve the operation efficiency of basic medical insurance for urban workers.41 ChenandZhao proposed that the LTCI system and regional economic development have mutual influence and restriction, which constitute a complex coupling interaction system.42
Development Dilemma of LTCI
Although the LTCI system has produced many positive social effects, the enormous financial expenditure behind it has also brought a substantial economic burden to governments. Its future development will also be restricted by many factors, which are shown in Table 3.
Table 3.
The Influencing Factors are Limiting the Development of LTCI
| Factors | Representative Article | Results |
|---|---|---|
| Price rise factors | Eggink and Woittiez (2016)45 | Expected price increase in the future will lead to an annual increase of 3.5% in real future expenditure on long-term care in the Netherlands. |
| The rate of elderly disability that cannot be accurately predicted | Ding and Yan (2019)43 | It’s higher to measure the rate of elderly disability used IADL than ADL as a measuring tool. |
| Change in labor supply market factors | Geyer and Korfhage (2015)25 | Benefits in kind and benefits in cash have different effects on the labor market for long-term care services. |
| Other insurance such as private long-term care insurance and Medicare insurance | Sun (2018)44 | Qingdao long-term care insurance funds are limited to basic medical insurance by urban workers |
| Lin et al (2013)46 | Public LTCI and private LTCI have some alternatives. | |
| Kim and Kwon (2015)49 | Compared with families and communities, hospitals remain the foundation of long-term care services for the elderly. |
|
| Brown and Finkelstein (2008)50 | The interaction of public and private insurance |
Table 3 shows many constraints to the development of the LTCI system. For example, the price rise will increase the cost of long-term care and may result in a shortage of funding for public LTCI.45 Geyer and Korfhage found that benefits in kind and benefits in cash have different effects on the labor market for long-term care services.25 Lin et al argued that public LTCI and private LTCI are complementary and alternative.46
Discussion
It is a global problem of how to solve the enormous demand and its massive economic burden of long-term care services for the disabled elderly caused by the aging population. LTCI system is in response to this problem. However, there are still many difficulties, although the LTCI system has been implemented in Europe, such as Germany for 25 years (1995–2020), and has a positive impact on alleviating the long-term care crisis of the aging population. The topic of LTCI has also become an international academic frontier and a hot topic. Therefore, it is necessary to carry out a systematic review of relevant research literature, which is of great significance not only for the further improvement of the LTCI system in European and American countries but also for the aging countries just beginning to implement LTCI system like China. Moreover, Challenges posed by COVID-2019 for subsequent LTC services. Incapacitated or semi-incapacitated elderly with weak immunity due to chronic diseases are its main victims. Meanwhile, in view of the precedent of a high proportion of incapacitated patients with SARS (2003) after treatment, how the average family pays the high cost of care poses a higher challenge to the deepening and improvement of the LTCI system under the pilot.
Some information had been revealed by a preliminary review of relevant literature. First, more and more articles have been published on the social welfare impact of the LTCI system over time, especially in the last 2 years (2018 and 2019) accounted for more than 50% of all relevant papers published in the decade. It verified that the research on the social welfare impact of the LTCI system had been paid more and more attention from the academic circle. Second, the most studied countries are China, Japan, and other countries with large population density and increasingly severe population aging, indicating that the task of long-term care for disabled elderly has been quite tricky, and has been highly valued by governments and academia. One thing to point out is that some Chinese scholars studied the LTCI system of Japan and Germany, reflecting the commonality of social security concepts between China and Japan, Germany.15 Third, few studies on the LTCI system in developing countries except China.16 This may have to do with the fact that economic growth remains the primary goal in most developing countries, and less attention has been paid to the area of long-term care for the disabled elderly.
While the implementation of the LTCI system has a great impact on social welfare, it also faces a great dilemma to be solved.
Firstly, it is shown that LTCI has a positive effect on the health and life quality of the disabled elderly.17–19 However, the beneficiaries of the LTCI system should be further expanded, especially in China with nearly 300 million elderly people.5,47 For example, some pilot cities in China such as Chongqing should gradually relax the conditions for enjoying the long-term care insurance treatment, such as “long-term bed or after treatment of no less than 6 months after the assessment of disability level to meet the criteria for severe disability”, can be appropriately relaxed to moderate disability, and then gradually expand to the full coverage of severe, moderate and mild disability. Geographically, the successful pilot experience of the public LTCI system in 15 pilot cities should also be expanded to more cities as soon as possible.
Secondly, LTCI’s impact on the labor market is a meaningful topic that deserves further study. The dilemma between going to work and taking care of the disabled elderly facing family members25–27 due to the role of LTCI in alleviating the financial burden on families with the disabled elderly may be limited.24 It may also influence family choices about different forms of care.28–32 Therefore, the government has acted simultaneously in implementing the LTCI system from two aspects: improving the professional quality of nursing staff in long-term-care pension institutions, so as to reassure family members.5 At the same time, appropriately raise the current funding standard (eg, 150 yuan/person/year in Chongqing) and the payment standard of care (eg, 30–50 yuan/person/day in Chongqing).1,48
Thirdly, from a macro point of view. LTCI system policy shows the specific influence on the whole social welfare in release effective demand for Long-term care,33 promote the public health service system to further development,34,40 establish the LTCI system, improving the efficiency of the Long-term care service, etc. However, its burden on government budget expenditure is also obvious.35,39 For example, Eggink et al45 found that the expected price increase in the future will lead to an annual increase of 3.5% in real future expenditure on long-term care in the Netherlands. Xu et al predicted the LTC costs for each disability state of the elderly during 2020–2050 in China.48 It is found that the future growth in LTC costs will be tremendous, and the role of LTCI will be even more evident, which is also a significant problem facing many countries around the world. Perhaps, it is a good idea that introducing social capital and strengthen the effective combination of private and public long-term care insurance to play an active role together.46,49,50
Our systematic review shows that the research on the LTCI system has become an international frontier academic topic, and the research on the social welfare impact of LTCI has attracted more and more attention from scholars around the world, with more and more in-depth research contents. However, both the theoretical depth and the empirical method lag far behind the studies of scholars in Germany and other countries,2,51-53 which is also related to the late implementation of LTCI policy in China (since the pilot began in 2016), while that in Germany and other countries has been implemented for more than 20 years (since the 1990s). This provides a broad academic space for our future research. As we know, the formal implementation of pilot LTCI policies in 15 cities carried out from 2016 and reach its peak in 2018–2019 in China. Therefore, this systematic review led us to realize that, restricted by various factors such as Chinese traditional family concept,54 government responsibility boundary,55 and LTC needs assessment system,56,57 the LTCI system is a long-term process that needs to be improved continuously to truly meet the growing and changing long-term care needs,52 which is even more daunting in China having the largest elderly population in the world.
Due to the late start (2016), China’s LTCI system has some immature problems in the specific pilot process, such as fundraising or fund payment. Its impact on social welfare is too short to be obvious for the time being, and relevant studies in the academic circle are few and not in-depth enough. Therefore, this review does not make a more detailed comparison between the academic research results of China and other countries on this topic but combines them into a discussion. As China’s LTCI system has been in practice for a longer time, perhaps in 5 years or so, it would be a good choice to focus on the comparative analysis between China and other countries on the impact of long-term care insurance system on social welfare, which is also our future research focus.
Conclusions
Implementation of LTCI system not only in reducing the physical and mental health problems of health care recipients and providers, and the economic burden of their families, but also promote the development of health care service industry and further improvement of the medical and health care system. However, it cannot be ignored that there are two important questions facing the governments of all countries: a) How to deal with the huge financial expenditure behind public LTCI; and b) How to cooperate with other insurance such as endowment insurance to produce greater social welfare. Therefore, in the future studies, we should further deepen the research on the problems related to LTCI and clarify its influence mechanism, so as to find the right remedy for the disease and the solution to the problem.
Acknowledgments
We thank Professor Timothy Kyng and Professor Fei Guo at Macquarie University for their thoughtful guidance.
Funding Statement
This research was funded by China Chongqing Education Commission Humanities and Social Sciences Research Project “Study on the pilot evaluation and optimization path of Long-term care insurance payment policy”, grant number No: 20SKGH106, the MOE Project of Key Research Institute of Humanities and Social Sciences of Research Center for Economy of Upper Reaches of the Yangtse River, grant number No: CJSYTD201710, and Chongqing Technology and Business University “Responding to Major Public health Emergencies” thematic research project “Study on the deepening Path of Chongqing’s long-term Care Insurance System in the Post-COVID-2019 Era”, grant number No: ctbuyqzx10.
Disclosure
The authors report no conflicts of interest for this work.
References
- 1.Xu X, Huang X, Zhang X, Chen L. Family economic burden of elderly chronic diseases: evidence from China. Healthcare. 2019;7(3):99. doi: 10.3390/healthcare7030099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rhee JC, Done N, Anderson GF. Considering long-term care insurance for middle-income countries: comparing South Korea with Japan and Germany. Health Policy (New York). 2015;119(10):1319–1329. doi: 10.1016/j.healthpol.2015.06.001 [DOI] [PubMed] [Google Scholar]
- 3.Wei-dong D. Long term care insurance: arational choice of old-age security in China. Popul J. 2016;(2):72–81. [Google Scholar]
- 4.Zeng-wen W. The influence of social security income on the utilization rate of nursing service for the elderly. China Popul Sci. 2017;(06):44–53. [Google Scholar]
- 5.Chen L, Zhang X, Xu X. Health insurance and long-term care services for the disabled elderly in china: based on CHARLS data. Risk Manag Healthc Policy. 2020;13:155–162. doi: 10.2147/RMHP.S233949 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Xu X, Zhang L, Chen L, Wei F. Does COVID-2019 have an impact on the purchase intention of commercial long-term care insurance among the elderly in China? Healthcare. 2020;8(2):126. doi: 10.3390/healthcare8020126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Xu X, Xu Z, Chen L, Li C. How does industrial waste gas emission affect health care expenditure in different regions of china: an application of bayesian quantile regression. Int J Environ Res Public Health. 2019;16(15):2748. doi: 10.3390/ijerph16152748 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Xu X, Zhang L, Chen L, Liu C. The role of soil N2O emissions in agricultural green total factor productivity: an empirical study from China around 2006 when agricultural tax was abolished. Agriculture. 2020;10(5):150. doi: 10.3390/agriculture10050150 [DOI] [Google Scholar]
- 9.Huang X, Xu X, Wang Q, Zhang L, Gao X, Chen L. Assessment of agricultural carbon emissions and their spatiotemporal changes in China, 1997–2016. Int J Environ Res Public Health. 2019;16(17):3105. doi: 10.3390/ijerph16173105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Xu X, Huang X, Huang J, Gao X, Chen L. Spatial-temporal characteristics of agriculture green total factor productivity in China, 1998–2016: based on more sophisticated calculations of carbon emissions. Int J Environ Res Public Health. 2019;16(20):3932. doi: 10.3390/ijerph16203932 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. doi: 10.1371/journal.pmed1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tufanaru C, Munn Z, Aromataris E, Campbell J, Hopp L. Chapter 3: systematic reviews of effectiveness. In: Aromataris E, Munn Z (editors). Joanna Briggs institute reviewer’s manual. The Joanna Briggs Institute; 2017. Available from https://reviewersmanual.joannabriggs.org/. [Google Scholar]
- 13.Critical Appraisal Skills Programme. CASP-systematic-review-checklist_2018. Available from: https://casp-uk.net/casp-tools-checklists/.
- 14.Levy Y, Ellis TJ. A systems approach to conduct an effective literature review in support of information systems research. Inf Sci. 2006;9:181–212. [Google Scholar]
- 15.Germany, Japan, Korea long - term care insurance operation comparison and inspiration. China Insur. 2018;(11): 60–64. [Google Scholar]
- 16.Lloyd-Sherlock P, Penhale B, Redondo N. The admission of older people into residential care homes in argentina: coercion and human rights abuse. Gerontologist. 2019;59(4):610–618. doi: 10.1093/geront/gny014 [DOI] [PubMed] [Google Scholar]
- 17.Choi JK, Joung E. The association between the utilization of long-term care services and mortality in elderly Koreans. Arch Gerontol Geriatr. 2016;65:122–127. doi: 10.1016/j.archger.2016.03.013 [DOI] [PubMed] [Google Scholar]
- 18.Lee TW, Yim ES, Choi HS, et al. Day care vs home care: effects on functional health outcomes among long-term care beneficiaries with dementia in Korea. Int J Geriatr Psychiatry. 2019;34(1):97–105. doi: 10.1002/gps.4992 [DOI] [PubMed] [Google Scholar]
- 19.Ratcliffe MR, Bradley J, Shulver C, Crotty W. Evaluating the quality of care received in long-term care facilities from a consumer perspective: development and construct validity of the consumer choice index - six dimension instrument. Ageing Soc. 2019;39(1):138–160. doi: 10.1017/S0144686X17000861 [DOI] [Google Scholar]
- 20.Sugiyama T, Tamiya N, Watanabe T, et al. Association of care recipients’ care-need level with family caregiver participation in health check-ups in Japan. Geriatr Gerontol Int. 2018;18(1):26–32. doi: 10.1111/ggi.13131 [DOI] [PubMed] [Google Scholar]
- 21.Iwamoto Y, Kohara M, Saito M. On the consumption insurance effects of long-term care insurance in Japan: evidence from micro-level household data. J Jpn Int Econ. 2010;24(1):99–115. doi: 10.1016/j.jjie.2009.12.009 [DOI] [Google Scholar]
- 22.Tamiya N, Noguchi H, Nishi A, et al. Population ageing and wellbeing: lessons from Japan’s long-term care insurance policy. Lancet. 2011;378(9797):1183–1192. doi: 10.1016/S0140-6736(11)61176-8 [DOI] [PubMed] [Google Scholar]
- 23.Chen F. The development prospect and influencing factors of long-term care insurance at the present stage in China. Times Finance. 2013;21:155. [Google Scholar]
- 24.Kim HB, Lim W. Long-term care insurance, informal care, and medical expenditures. J Public Econ. 2015;125:128–142. doi: 10.1016/j.jpubeco.2014.12.004 [DOI] [Google Scholar]
- 25.Geyer J, Korfhage T. Long-term care insurance and carers‘ labor supply - a structural model. Health Econ. 2015;24(9):1178–1191. doi: 10.1002/hec.3200 [DOI] [PubMed] [Google Scholar]
- 26.Sakka M, Goto J, Kita S, et al. Associations among behavioral and psychological symptoms of dementia, care burden, and family-to-work conflict of employed family caregivers. Geriatr Gerontol Int. 2019;19(1):51–55. doi: 10.1111/ggi.13556 [DOI] [PubMed] [Google Scholar]
- 27.Umegaki H, Yanagawa M, Nonogaki Z, et al. Burden reduction of caregivers for users of care services provided by the public long-term care insurance system in Japan. Arch Gerontol Geriatr. 2014;58(1):130–133. doi: 10.1016/j.archger.2013.08.010 [DOI] [PubMed] [Google Scholar]
- 28.Schmitz H, Westphal M. Short- and medium-term effects of informal care provision on female caregivers’ health. J Health Econ. 2015;42:174–185. doi: 10.1016/j.jhealeco.2015.03.002 [DOI] [PubMed] [Google Scholar]
- 29.Gao Q. Analysis on influencing factors of adults’ willingness to long-term care. Chin Med Insur. 2019;1:31–34. [Google Scholar]
- 30.Coe NB, Skira MM, Van Houtven CH. Long-term care insurance: does experience matter? J Health Econ. 2015;40:122–131. doi: 10.1016/j.jhealeco.2015.01.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tsai Y. Social security income and the utilization of home care: evidence from the social security notch. J Health Econ. 2015;43:45–55. doi: 10.1016/j.jhealeco.2014.10.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lehnert T, Günther OH, Hajek A, et al. Preferences for home- and community-based long-term care services in Germany: a discrete choice experiment. Eur J Health Econ. 2018;19(9):1213–1223. doi: 10.1007/s10198-018-0968-0 [DOI] [PubMed] [Google Scholar]
- 33.Yang W, Liu H, Liu S. Investigation and improvement of the long-term care insurance pilot in Shandong province. China Market. 2019;26:32–37. [Google Scholar]
- 34.Jiang M. Exploration of the impact of long-term care insurance on the development of elderly health service industry. China Health Res. 2019;22(01):38–42. [Google Scholar]
- 35.Lee SH. Long-term care insurance in Japan: operational mechanism, social impact and implications. China Collective Econ. 2015;18:167–168. [Google Scholar]
- 36.Hao J, Li X. Long term care insurance in Germany: institutional design, economic impact and implications. Popul J. 2014;36(02):104–112. [Google Scholar]
- 37.Li X, Zhu M. Basic care insurance in Nantong: system design, operation effect and prospect. Soc Secur Res. 2018;3:50–57. [Google Scholar]
- 38.Yu X, Liu H, Yang W. Effects of long-term care insurance on medical costs: a synthetic control study based on Qingdao model. Insur Res. 2019;2:114–127. [Google Scholar]
- 39.Geyer J, Haan P, Korfhage T. Indirect fiscal effects of long-term care insurance. Fisc Stud. 2017;38(3):393–415. doi: 10.1111/j.1475-5890.2017.12140 [DOI] [Google Scholar]
- 40.Shao W. Experience summary of China’s long-term care insurance system in the pilot phase. J Changchun Univ. 2018;28(01):7–11. [Google Scholar]
- 41.Shen Y, Song Z, Liu S. Study on the effect of long-term care insurance on the operation efficiency of basic medical insurance for urban workers. Modern Trade Ind. 2019;40(33):132–134. [Google Scholar]
- 42.Chen K, Zhao N. Evaluation and optimization of coordination degree between long-term care insurance system and regional economic development. Financ Theor Pract. 2019;6:87–93. [Google Scholar]
- 43.Ding H, Yan J. Measurement and variation trend of the disability rate of the elderly in China. Chin Popul Sci. 2018;3:97–108. [Google Scholar]
- 44.Sun J. Research on the predicament and countermeasures of long-term care insurance system in Qingdao. Northern Econ Trade. 2018;3:85–87. [Google Scholar]
- 45.Eggink E, Ras M, Woittiez I. Dutch long-term care use in an ageing population. J Econ Ageing. 2017;9:63–70. doi: 10.1016/j.jeoa.2016.08.001 [DOI] [Google Scholar]
- 46.Lin H, Prince J. The impact of the partnership long-term care insurance program on private coverage. J Health Econ. 2013;32(6):1205–1213. doi: 10.1016/j.jhealeco.2013.09.010 [DOI] [PubMed] [Google Scholar]
- 47.Zeng L, Xu X, Zhang C, Chen L. Factors influencing long-term care service needs among the elderly based on the latest anderson model: a case study from the middle and upper reaches of the Yangtze river. Healthcare. 2019;7(4):157. doi: 10.3390/healthcare7040157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Xu X, Chen L. Projection of long-term care costs in China, 2020–2050: based on the bayesian quantile regression method. Sustainability. 2019;11(13):3530. doi: 10.3390/su11133530 [DOI] [Google Scholar]
- 49.Kim H, Jung YI, Kwon S. Delivery of institutional long-term care under two social insurances: lessons from the Korean experience. Health Policy (New York). 2015;119(10):1330–1337. doi: 10.1016/j.healthpol.2015.07.009 [DOI] [PubMed] [Google Scholar]
- 50.Brown JR, Finkelstein A. The interaction of public and private insurance: medicaid and the long-term care insurance market. Am Econ Rev. 2008;98(3):1083–1102. doi: 10.1257/aer.98.3.1083 [DOI] [Google Scholar]
- 51.Zhang L, Zhong R. Analysis of the concept, path and effect of the reform of the Japanese insurance system – based on the perspective of financial pressure relief. Soc Secur Res. 2019;5:52–62. [Google Scholar]
- 52.Gannon B, Davin B. Use of formal and informal care services among older people in Ireland and France. Eur J Health Econ. 2010;11(5):499–511. doi: 10.1007/s10198-010-0247-1 [DOI] [PubMed] [Google Scholar]
- 53.Koike S, Furui Y. Long-term care-service use and increases in care-need level among home-based elderly people in a Japanese urban area. Health Policy (New York). 2013;110(1):94–100. doi: 10.1016/j.healthpol.2012.12.011 [DOI] [PubMed] [Google Scholar]
- 54.Wang L. Government or family: reflection on the supply responsibility of long-term care service. Acad Forum. 2018;41(05):117–124. [Google Scholar]
- 55.Qi C. Some problems to be clarified in the establishment of long-term care insurance system. Disabil Res. 2019;(03):10–15. [Google Scholar]
- 56.Yang W, Liu H, Liu S. Investigation and improvement measures on the status of long-term care insurance pilot in Shandong province. China Market. 2019;26:32–37. [Google Scholar]
- 57.Sun J. Analysis on welfare elements of China’s long-term care insurance system and optimization strategies. Beijing Soc Sci. 2019;(10):107–116. [Google Scholar]