The novel coronavirus (COVID-19) pandemic has created an urgent need for pragmatic best-practice approaches that maximize safety for both patients and care providers during the tracheal intubation of patients who are suspected or confirmed to be infected. Literature reporting experiences during the severe acute respiratory syndrome (SARS) epidemic revealed that providers who engaged in tracheal intubation had a substantial increase in risk of viral transmission.1, 2, 3 Longstanding principles of emergency airway management, including excellent preoxygenation and rapid sequence intubation techniques, apply to patients with suspected or confirmed COVID-19 infection. However, some accepted and common practices may also substantially increase the risks to health care providers in this setting: Specifically, droplet generation and aerosol generation before, during, and after tracheal intubation creates risk for the proceduralist.
We convened a multidisciplinary working group of acute care providers to develop a novel shared paradigm for tracheal intubation at Mayo Clinic Hospital during the COVID-19 pandemic. Our working group consisted of representatives from the specialties of anesthesiology, critical care medicine, emergency medicine, pediatric anesthesiology, pediatric critical care medicine, and pediatric emergency medicine. Our implementation of novel care processes, which was guided by existing empiric data and expert consensus, involved 3 discrete steps: multidisciplinary review and synthesis of current knowledge; development of novel care processes and cognitive aids to assist providers at the bedside within our institution; and, most importantly, robust generation of a shared mental model of the novel paradigm of airway care during the COVID-19 pandemic. We were guided by 2 overarching goals—safe patient care during tracheal intubation and safety of the patient care team—and 3 core principles: minimize aerosol generation, maximize first attempt success, and minimize exposure of care providers.4, 5, 6, 7, 8, 9, 10, 11
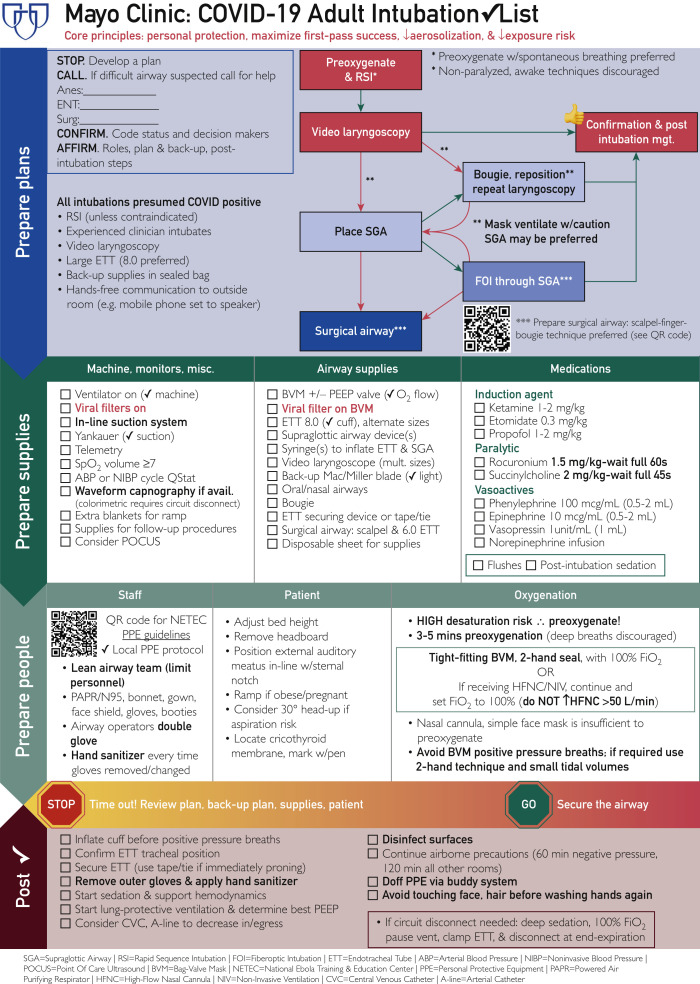
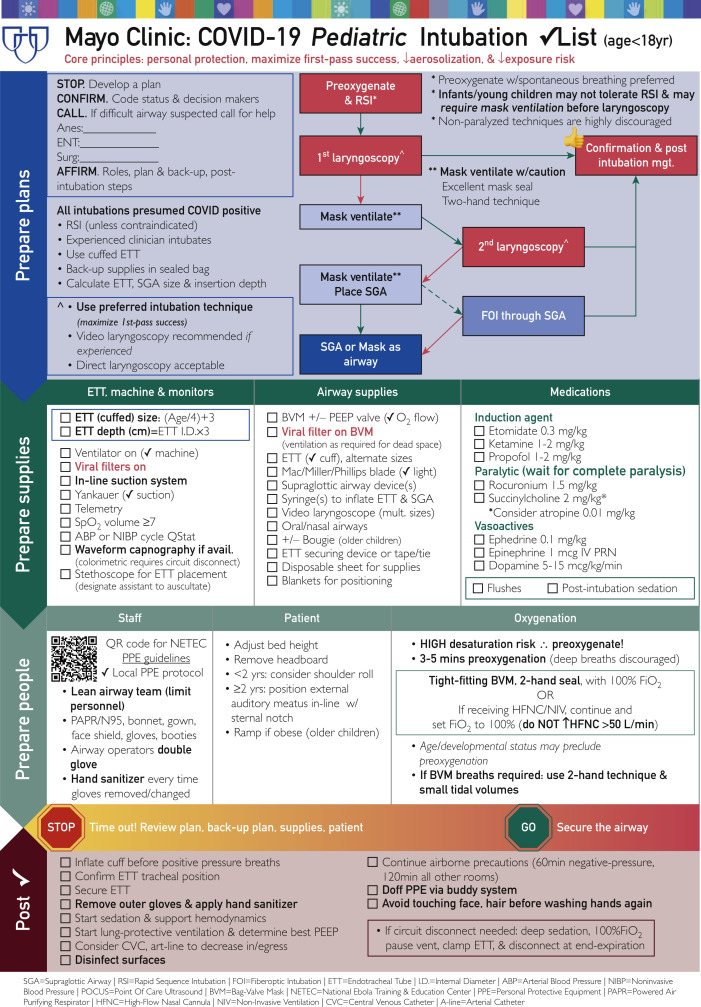
Our group used existing expert recommendations and supporting evidence to generate discrete and broadly applicable steps for providers to use during the tracheal intubation of patients with suspected or known COVID-19 (Table ). We engaged in an iterative process to ensure that each step was applicable to each specialty group, avoiding a focus on niche interests that could create confusion in varied care settings. We paid particular attention to highlight areas in which processes were novel (eg, avoidance of positive pressure mask ventilation to decrease aerosol generation, the use of a viral filter, and limiting ventilation circuit disconnections) and differed from existing accepted tracheal intubation practices. We used this information to generate novel cognitive aids in the form of procedural checklists for adult and pediatric patients (Figures 1 and 2 ) for bedside use in our institution. We then employed webinars to conduct frequent informational sessions and discussions to facilitate the development of a robust shared mental model at our institution.
Table.
Mayo Clinic Hospital COVID-19 Pandemic Intubation Guideline
| Preparation |
| 1. Don appropriate PPE: N95 mask + face shield or PAPR with bonnet, gown, double gloves, and booties, while a team member observes for proper technique. |
| 2. Lean team: only necessary personnel during AGP. |
| 3. Back-up provider with donned PPE outside, in communication with team (eg, speakerphone). |
| 4. Call for help early if a difficult airway is anticipated. |
| 5. Closed-loop, detailed communication of the intubation plan and back-up plan. |
| a. Prepare equipment for preoxygenation and first intubation attempt. |
| b. Ensure that back-up equipment is prepared in sealed bag, easily accessible in room. |
| 6. Close the door, and hang “Procedure in Progress” sign during AGP. |
| Procedure |
| 7. Use an intubation checklist (Adult or Pediatric). |
| 8. Intubation should be performed by an experienced provider. |
| 9. Preoxygenation for 3 to 5 minutes with 100% O2 with tight mask seal and viral filter. |
| a. Prioritize spontaneous patient breathing, avoiding deep breaths (may cause cough). |
| 10. RSI technique with high-dose paralytic, unless contraindicated. |
| a. Young children may not tolerate apnea and may require careful mask ventilation. |
| 11. Await full paralysis (45 to 60 seconds) and apnea before removing the preoxygenation device. |
| 12. Video laryngoscopy is strongly preferred (but best device for provider should be used). |
| a. If performing direct laryngoscopy, maximize the provider face-to-patient face distance. |
| 13. Consider use of early rescue SGA (Air-Q LMA [Salter Labs, Chicago, Illinois] or King LT [Eugene, Oregon]) if first attempt is unsuccessful. |
| 14. Mask ventilate ONLY IF CRITICAL NEED (OPA, tight 2-hand seal, viral filter, low TV breaths). |
| 15. Immediately inflate the ETT cuff (including children) before ventilating patient. |
| 16. Remove outside pair of gloves, and use hand sanitizer on inner gloves. |
| 17. Attach ventilator circuit. |
| a. Circuit with HME (ETT: in-line suction; HME/filter: capnography device, circuit). |
| b. Circuit without HME (ETT: in-line suction; capnography device, circuit). |
| 18. Confirmation with visualization, waveform capnography, and bilateral chest rise. |
| a. When in question, auscultation, colorimetric capnography, or POCUS may be required. |
| Postprocedure |
| 19. Limit disconnections of the ventilator circuit. |
| a. Ventilator paused at end expiration, excellent sedation/paralysis, and consider ETT clamp. |
| 20. Dispose of all airway equipment immediately in a predesignated plastic bag. |
| 21. Doff PPE while a team member observes for proper technique, avoiding contamination. |
| 22. After intubation, note time on door when room may be entered without airborne PPE (varies by room and requires air turnover of at least 7 times). |
AGP = aerosol-generating procedure; ETT = endotracheal tube; HME = heat and moisture exchanger; LMA = laryngeal mask airway; LT = laryngeal tube; OPA = oropharyngeal airway; PAPR = powered air purifying respirator; POCUS = point of care ultrasound; PPE = personal protective equipment; RSI = rapid sequence intubation; SGA = supraglottic airway; TV = tidal volume.
Figure 1.
Mayo Clinic COVID-19 adult intubation checklist.
Figure 2.
Mayo Clinic COVID-19 pediatric intubation checklist.
Multiple guidelines and resources have been published in recent months to provide conceptual guidance to providers as they navigate new paradigms of care during the COVID-19 pandemic. We believe it is imperative that each institution employs a multidisciplinary approach to implement these principles effectively within their individual care settings. We share our novel cognitive aids here in the hope that they may serve as useful guides to others.
Footnotes
Grant Support: No grant support was provided for this article.
Potential Competing Interests: The authors report no competing interests.
Supplemental Online Material
References
- 1.Raboud J., Shigayeva A., McGeer A. Risk factors for SARS transmission from patients requiring intubation: a multicentre investigation in Toronto, Canada. PLoS One. 2010;5(5):e10717. doi: 10.1371/journal.pone.0010717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tran K., Cimon K., Severn M. Aerosol-generating procedures and risk of transmission of acute respiratory infections to healthcare workers: a systematic review. PLoS One. 2012;7(4):e35797. doi: 10.1371/journal.pone.0035797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Esquinas A., Pravinkumar S., Scala R. Noninvasive mechanical ventilation in high-risk pulmonary infections: a clinical review. Eur Respir Rev. 2014;23(134):427–438. doi: 10.1183/09059180.00009413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization Clinical management of severe acute respiratory infection (SARI) when COVID-19 disease is suspected: interim guidance. https://apps.who.int/iris/rest/bitstreams/1272156/retrieve Published March 13, 2020. Accessed March 28, 2020.
- 5.Brown C., Mosier J., Carlson J., Gibbs M. Pragmatic recommendations for intubating critically ill patients with suspected COVID-19. JACEP Open. 2020;1(2) doi: 10.1002/emp2.12063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zou M., Yuguang H., Wuhua M. Expert recommendations for tracheal intubation in critically ill patients with novel coronavirus disease 2019. Chin Med Sci J. 2020;35(2):105–109. doi: 10.24920/003724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wax R.S., Christian M.D. Practical recommendations for critical care and anesthesiology teams caring for novel coronavirus (2019-nCoV) patients. Can J Anesth. 2020;67(5):568–576. doi: 10.1007/s12630-020-01591-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Brewster D., Chrimes N., Do T. Consensus statement: Safe Airway Society principles of airway management and tracheal intubation specific to the COVID-19 adult patient group. Med J Aust. 2020;212(10):472–481. doi: 10.5694/mja2.50598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Alhazzani W., Moller M., Arabi Y. Surviving Sepsis Campaign: guidelines on the management of critically ill adults with coronavirus disease 2019 (COVID-19) Crit Care Med. 2020;48(6):440–469. doi: 10.1097/CCM.0000000000004363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zucco L., Levy N., Ketchandji D. Perioperative considerations for the 2019 Novel Coronavirus (COVID-19): clinical communication from the Anesthesia Patient Safety Foundation (APSF). Online publication February 12, 2020. https://www.apsf.org/news-updates/perioperative-considerations-for-the-2019-novel-coronavirus-covid-19/
- 11.Matava C., Kovatsis P., Summers J. Pediatric airway management in COVID-19 patients: consensus guidelines from the Society for Pediatric Anesthesia's Pediatric Difficult Intubation Collaborative and the Canadian Pediatric Anesthesia Society. Anesth Analg. 2020;131(1):61–73. doi: 10.1213/ANE.0000000000004872. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.