Abstract
Background
The coronavirus disease 2019 (COVID-19) pandemic has led to unprecedented challenges for health care systems globally. We designed and administered a global survey to examine the effects of COVID-19 on vascular surgeons and explore the COVID-19-related stressors faced, coping strategies used, and support structures available.
Methods
The Pandemic Practice, Anxiety, Coping, and Support Survey for Vascular Surgeons was an anonymous cross-sectional survey sponsored by the Society for Vascular Surgery Wellness Task Force. The survey analysis evaluated the effects of COVID-19-related stressors on vascular surgeons measured using the Generalized Anxiety Disorder 7-item scale. The 28-item Brief Coping Orientation to Problems Experienced inventory was used to assess the active and avoidant coping strategies. Survey data were collected using REDCap (Research Electronic Data Capture) from April 14, 2020 to April 24, 2020 inclusive. Additional qualitative data were collected using open-ended questions. Univariable and multivariable analyses of the factors associated with the anxiety levels and qualitative analysis were performed.
Results
A total of 1609 survey responses (70.5% male; 82.5% vascular surgeons in practice) from 58 countries (43.4% from United States; 43.4% from Brazil) were eligible for analysis. Some degree of anxiety was reported by 54.5% of the respondents, and 23.3% reported moderate or severe anxiety. Most respondents (∼60%) reported using active coping strategies and the avoidant coping strategy of “self-distraction,” and 20% used other avoidant coping strategies. Multivariable analysis identified the following factors as significantly associated with increased self-reported anxiety levels: staying in a separate room at home or staying at the hospital or a hotel after work (odds ratio [OR], 1.39; 95% confidence interval [CI], 1.08-1.79), donning and doffing personal protective equipment (OR, 1.81; 95% CI, 1.41-2.33), worry about potential adverse patient outcomes due to care delay (OR, 1.47; 95% CI, 1.16-1.87), and financial concerns (OR, 1.90; 95% CI, 1.49-2.42). The factors significantly associated with decreased self-reported anxiety levels were hospital support (OR, 0.83; 95% CI, 0.76-0.91) and the use of positive reframing as an active coping strategy (OR, 0.88; 95% CI, 0.81-0.95).
Conclusions
Vascular surgeons globally have been experiencing multiple COVID-19-related stressors during this devastating crisis. These findings have highlighted the continued need for hospital systems to support their vascular surgeons and the importance of national societies to continue to invest in peer-support programs as paramount to promoting the well-being of vascular surgeons during and after the COVID-19 pandemic.
Keywords: Coping strategies, COVID-19, GAD-7 scale, Brief COPE Survey, Financial stress, Personal protective equipment
Article Highlights.
-
•
Type of Research: The COVID-19 [coronavirus disease 2019] Pandemic Practice, Anxiety, Coping and Support Survey for Vascular Surgeons was an anonymous cross-sectional global survey sponsored by the Society for Vascular Surgery Wellness Task Force.
-
•
Key Findings: The survey evaluated the effect of COVID-19-related stressors on 1609 vascular surgeons from 58 countries from April 14 to 24, 2020 using the general anxiety disorder scale and the brief Coping Orientation to Problems Experienced inventory. Higher self-reported anxiety and stress levels were significantly associated with staying in a separate room at home or staying at the hospital or a hotel after work (odds ratio [OR], 1.39; 95% confidence interval [CI], 1.08-1.79), donning and doffing personal protective equipment (OR, 1.81; 95% CI, 1.41-2.33), worry about potential adverse patient outcomes due to care delay (OR, 1.47; 95% CI, 1.16-1.87), and financial concerns (OR, 1.90; 95% CI, 1.49-2.42). Lower self-reported anxiety levels were associated with hospital support (OR, 0.83; 95% CI, 0.76-0.91) and the use of positive reframing as an active coping strategy (OR, 0.88; 95% CI, 0.81-0.95).
-
•
Take Home Message: The survey identified several areas in which vascular surgeons can be supported at institutional, regional, and national societal levels.
As of June 15, 2020, 7.9 million people had been infected and 434,432 individuals have died worldwide from the coronavirus disease 2019 (COVID-19) caused by the severe acute respiratory syndrome coronavirus 2. This has led to unprecedented challenges for health care systems globally, in addition to the physical and psychological challenges to health care workers. A survey of health care workers treating patients with COVID-19 in China demonstrated high rates of depression, anxiety, and insomnia.1 , 2 Vascular surgeons have faced unique difficulties related to changes in practice patterns, such as the cancellation of cases and clinics, and the possibility of redeployment to duties outside their specialty.3, 4, 5, 6 The survey was designed to examine the effects of COVID-19 by assessing the related anxiety of vascular surgeons, the coping strategies they have used, and their use of available support structures. The survey was available from April 14, 2020 to April 24, 2020, during which the case numbers had increased from 1.8 million to 2.6 million people infected worldwide.
Methods
Institutional review board approval
The Pandemic Practice, Anxiety, Coping, and Support Survey for Vascular Surgeons, an anonymous cross-sectional survey sponsored by the Society for Vascular Surgery (SVS) Wellness Task Force, was reviewed by the University of Washington Human Subjects Division and deemed exempt (approval no. 009926) owing to the minimal risk and nonidentifiable nature of the data. The respondents had provided consent by clicking on “agree to participate in this survey” before opening the survey.
Survey design
The COVID-19 Pandemic Practice, Anxiety, Coping, and Support Survey for Vascular Surgeons was an anonymous cross-sectional global survey sponsored by the Wellness Task Force of the SVS. The impetus for the survey was the observation of the importance of peer-to-peer support among vascular surgeons during the pandemic.7 The survey (Appendix, online only) covered domains derived from ongoing real-time discussions among vascular surgeons using SVSConnect and the Vascular Surgery COVID-19 WhatsApp group chat. The primary objective was to evaluate the personal effects on vascular surgeons measured using the Generalized Anxiety Disorder 7-item (GAD-7) scale, a widely used self-report measure of recent anxiety (previous 2 weeks).8 The 28-item Brief Coping Orientation to Problems Experienced (Brief-COPE) inventory was used to assess the active and avoidant coping strategies used.9 The participants were invited to share through an open-ended query any personal experiences. The Google reCAPTCHA feature was used to distinguish human from machine input to thwart spam. The survey data were collected using a secure REDCap (Research Electronic Data Capture) data capture platform hosted at the University of Washington.10 , 11
Survey dissemination
A multimodality approach to dissemination was used, starting with the SVS membership and the Association of Program Directors in Vascular Surgery electronic mailing lists. Dissemination was amplified by leveraging other organizational mailing lists, podcasts, newsletters, and social media platforms.
Statistical analysis
The survey analysis evaluated the effect of several COVID-19-related stressors on vascular surgeons measured using the GAD-7 scale. The GAD-7 scale degrees of anxiety are scored as mild, moderate, and severe according to cutoff scores of 5, 10, and 15, respectively.8 The 28 questions in the Brief-COPE inventory were scored to delineate the 14 coping strategies.9 The categorical data are presented as numbers and percentages. The continuous data are presented as the median and interquartile range (IQR). The parametric Student t test was used to compare normally distributed data and the nonparametric Wilcoxon rank sum test was used to compare the non-normally distributed GAD-7 scores. The Pearson χ 2 test was used to compare the degree of anxiety stratified by different factors. A multivariable ordinal logistic regression analysis using a proportional odds cumulative logit model was performed to evaluate the factors associated with the self-reported anxiety levels (defined as no, mild, moderate, and severe anxiety) by the 1259 respondents who had completed the GAD-7 survey. The multivariable model was built using a two-step process. The first step allowed for all factors that were significant on univariable analysis to be considered for entry into the model using a stepwise selection process (with the exception of the coping strategies from the Brief COPE survey). A significance level of P = .05 was required to allow a variable into the model and to stay in the model. The second step allowed for variables selected in the first step to be retained, and the stepwise selection was performed on the coping strategies. Special considerations were made for the variables that were highly correlated; specifically, the hospital support variables “operating room protocols,” “adequate personal protective equipment (PPE),” “preoperative testing of patients,” and “opportunities to interact with leadership” were highly correlated. The responses to the hospital support variable “transparency from leadership about COVID management and planning” were nearly identical to those for “opportunities to interact ...”; as such, the two were considered interchangeable. A new variable, “summative hospital support,” was created as a sum of the four significant individual hospital support variables. The variables in which the responses were limited owing to the “does not apply” option (ie, the following variables: “lack of PPE,” “terminating contracts of some of my employees,” and “the impact of hiatus on my career advancement”) were not included in the model because they did not represent the entire population of the respondents. The data were analyzed using SAS, version 9.4, for Windows (SAS Institute Inc, Cary, NC) and SPSS, version 19.0, for Windows (IBM Corp, Armonk, NY).
The narrative responses to the open-ended questions were systematically analyzed using qualitative thematic analysis by two independent investigators (K.W. and N.M.). Open coding was used to derive first-cycle codes consisting of short phrases directly from the data. Next, the initial codes were analyzed to determine how the codes could be grouped into themes that had succinctly captured the important pattern in the data. The themes were reviewed to ensure minimal overlap and to identify any subthemes that might have been contained within a given theme.
Results
Survey respondents
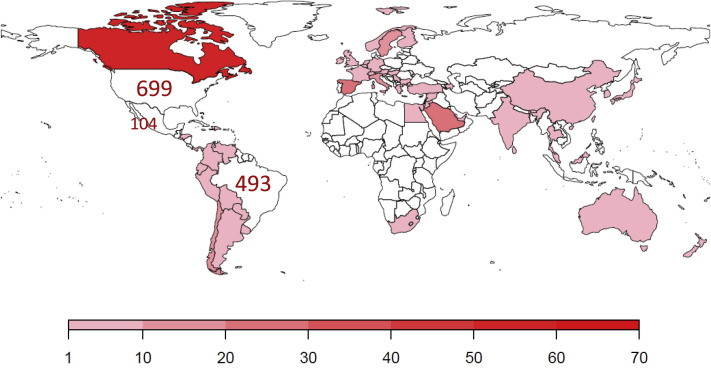
The size of the potential respondents or audience stratified by the mode of dissemination and estimated response rate are detailed in Supplementary Table I (online only). The survey was opened 1867 times. Of those, 258 records were excluded either because of no response (n = 253) or duplicated status (n = 5), leaving 1609 unique survey responses (70.5% male) from 58 countries eligible for analysis (Supplementary Fig 1, online only). Most of the respondents were from the United States (n = 699; 43.4%), Brazil (n = 493; 30.6%), and Mexico (n = 104; 6.5%). Most were board-certified vascular surgeons in practice (n = 1328; 82.5%), followed by vascular surgeons in training (n = 236; 14.7%; Table I ). A small number (n = 45; 2.8%) had been board certified in another specialty and performed vascular surgery interventions. They were included in the board-certified vascular surgeons group for analysis, because no differences were found in the responses between the two groups.
Supplementary Fig 1 (online only).
Map showing the geographic distribution of the 1609 survey respondents across the world.
Table I.
Characteristics of survey respondents (N = 1609)
| Characteristic | No. (%) |
|---|---|
| Practice duration | |
| In training | 236 (14.7) |
| In practice <10 years | 549 (34.1) |
| In practice 10-20 years | 412 (25.6) |
| In practice >20 years | 412 (25.6) |
| Gendera | |
| Male | 1134 (70.5) |
| Female | 461 (28.6) |
| Primary practice (n = 1373) | |
| Academicb | 469 (34.1) |
| Veterans Affairs or government runb | 61 (4.4) |
| Multispecialty clinic | 380 (27.6) |
| Community | 258 (18.7) |
| Solo | 125 (9.1) |
| Outpatient practice only | 80 (5.8) |
| Type of hospital (n = 1114) | |
| Urban teaching | 756 (67.9) |
| Urban nonteaching | 283 (25.4) |
| Rural teaching | 40 (3.6) |
| Rural nonteaching | 35 (3.1) |
| Size of hospital (n = 1278) | |
| <50 beds | 32 (2.5) |
| 50-99 beds | 62 (4.9) |
| 100-200 beds | 168 (13.1) |
| 201-300 beds | 202 (15.8) |
| 301-400 beds | 173 (13.5) |
| >400 beds | 619 (48.4) |
| Do not know | 22 (1.7) |
| Institutional leadership (n = 1257) | 656 (52.2) |
| Practice at >1 hospital (n = 1087) | 740 (68.1) |
| Completed the GAD-7 scale | 1518 (94.3) |
| Completed the Brief-COPE inventory | 1366 (84.9) |
Brief-COPE, Brief Coping Orientation to Problems Experienced; GAD-7, Generalized Anxiety Disorder 7 item.
Gender noted as “prefer not to say” in 14 responses.
Overlap between Veterans Affairs and academic appointments led to lower than expected numbers in this category.
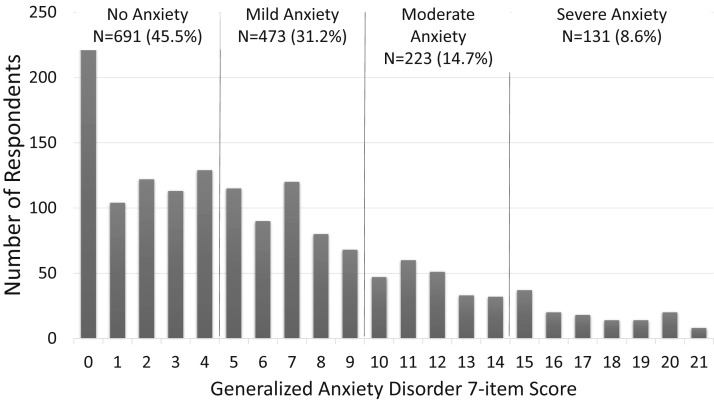
The GAD-7 scale was completed by 1518 respondents (94.3%; Supplementary Fig 2, online only). No differences were found in the GAD-7 completion rates between the vascular surgeons in practice and training nor by gender. However, regional variations were found, with more respondents from the United States compared with from other countries (97.3% vs 92.1%; P < .001). The median GAD-7 scale score was 5 (IQR, 2-9), with 54.5% of respondents reporting some level of anxiety and 23.3% reporting moderate or severe anxiety (Supplementary Fig 3, online only). No statistically significant differences were found in the median GAD-7 scale scores among the vascular surgeons in practice and those in training (median, 5; IQR, 2-9; vs median, 6; IQR, 2-9; P = .591). Women had higher GAD-7 scale scores compared with the men (median, 7; IQR, 4-11; vs median, 4; IQR, 1-8; P < .001).
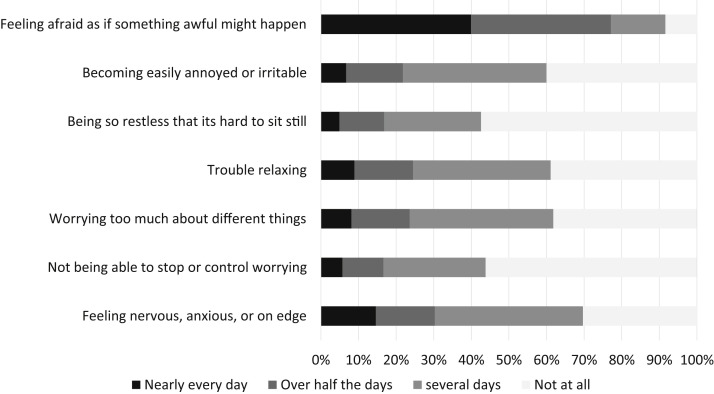
Supplementary Fig 2 (online only).
Bar graph showing the responses to the Generalized Anxiety Disorder 7-item scale (n = 1518).
Supplementary Fig 3 (online only).
Bar graph showing the number of respondents for each Generalized Anxiety Disorder 7-item scale scores and the interpretation of the scores as degrees of anxiety (no, mild, moderate, and severe anxiety).
COVID-19 practice effect
Vascular surgeons experienced cancellation of elective surgical procedures (1143 of 1303; 87.7%), call schedule alterations (400 of 1291; 30.9%), and the need to assist with clinical duties other than those of a vascular surgeon (353 of 1064; 33.2%). Less than one quarter of the respondents (332 of 1609; 20.6%) had operated on or placed a central venous access (including hemodialysis catheter) for a patient with confirmed COVID-19 infection, and 257 respondents (16%) had operated on a patient who was later found to have a COVID-19 infection. A total of 624 of 1602 respondents (38.8%) indicated they were considered at "high" risk of COVID-19 infection, most of whom were vascular surgeons in practice for >20 years (55.4%). Only 27 of the 1606 respondents (1.7%) reported testing positive for COVID-19. Several occupational stressors were significantly associated with increasing levels of anxiety as measured using the GAD-7 scale (Supplementary Table II, online only), including the lack of PPE and donning and doffing PPE, which were noted as stressors by 54.4% (710 of 1305) and 71.9% (928 of 1290) of the respondents, respectively. Preoperative testing of patients for COVID-19 was performed at fewer than one third of respondents' hospitals (475 of 1305; 29.5%).
Personal effects and stressors
Nearly one half (47.8%) of the respondents knew someone who had died of COVID-19, including a family member (n = 92; 5.7%) or medical provider from their own hospital (n = 330; 20.5%). Worrying that family and friends or colleagues would become infected with COVID-19 was a significant stressor for 65.8% and 59.8% of the respondents, respectively. In the month before the survey, 35.9% of the respondents had reviewed or made their will, designated or discussed again their medical power of attorney, or reviewed or applied for disability and/or life insurance. More than one third of the respondents (36.9%) had discussed dying with their family and/or friends.
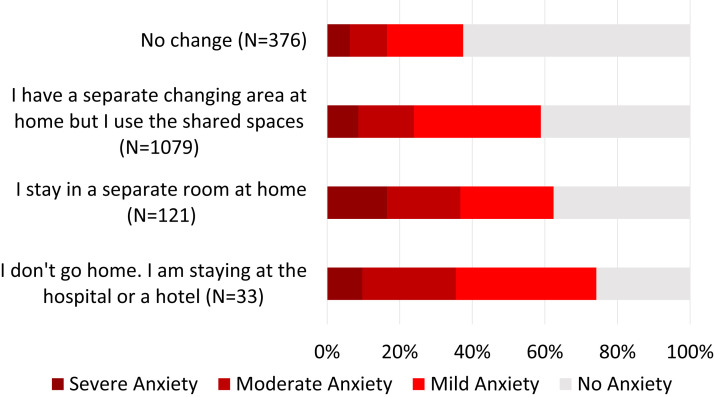
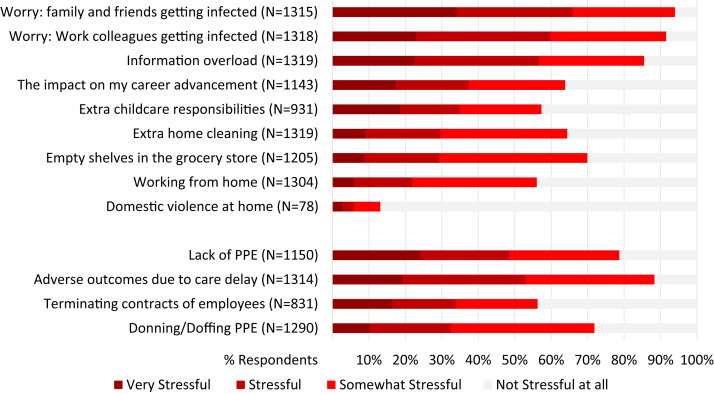
Most (77.1% of 1601) had noted they had implemented COVID-19-related modifications to their home routine after work. Changes included a separate changing area at home, staying in a separate room at home, or staying at the hospital or a hotel. Staying in a separate room and/or not going home were associated with higher self-reported anxiety levels (Supplementary Fig 4, online only). Working from home was stressful for 56.1% of 1304 respondents. Additional COVID-19-related stressors included extra childcare responsibilities, extra home cleaning, domestic violence at home, and empty shelves (Fig 1 ).
Supplementary Fig 4 (online only).
Bar graph showing the degree of self-reported anxiety (no, mild, moderate, and severe anxiety) associated with coronavirus disease 2019-related modifications of home routine after work (n = 1518). The difference in self-reported anxiety degree was statistically significant (P < .001).
Fig 1.
Magnitude of stress reported by vascular surgeons toward occupational and personal coronavirus disease 2019-related stressors. PPE, Personal protective equipment.
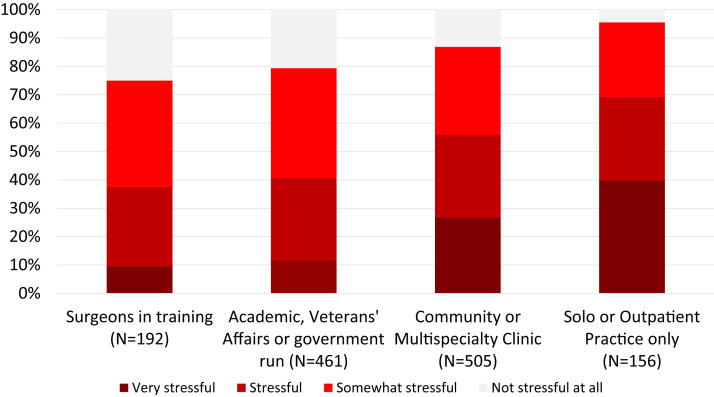
Financial concerns
Financial concerns were stressful for most respondents (1098 of 1314; 83.5%). Significant variation was found in the degree of perceived financial stress when stratified by the type of practice, with those in solo or outpatient-based practices reporting the highest perceived stress levels (Supplementary Fig 5, online only). Additionally, among those who had employees (n = 750), 58% reported stress regarding the need to terminate their contracts.
Supplementary Fig 5 (online only).
The degree of stress associated with coronavirus disease 2019-related financial concerns by vascular surgeons (n = 1314). The difference in self-reported stress level was statistically significant by type of practice (P < .001).
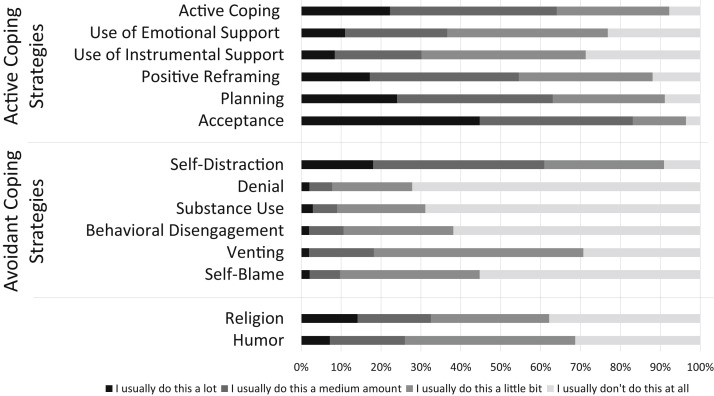
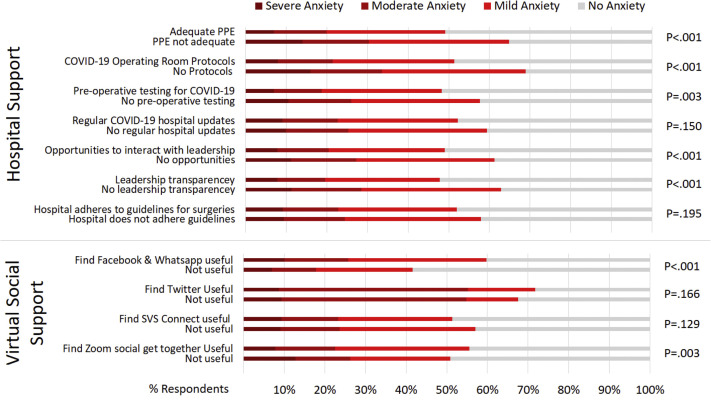
Coping strategies and support structures
The Brief COPE survey was completed by 1366 respondents (84.9%; Fig 2 ). Overall, vascular surgeons frequently used active strategies for coping and infrequently used avoidant strategies, with the exception of “self-distraction.” Most hospital support structures were associated with a reduction in self-reported anxiety levels by vascular surgeons as measured using the GAD-7. In contrast, virtual social media-based support platforms had a mixed effect (Fig 3 ). Of the 1272 respondents who had answered the question regarding knowledge of support resources, 50.4% and 25.1% were familiar with the SVS Physician Wellness Resources and the American College of Surgeons Well-Being Resources, respectively. In addition, 10.7% and 13.6% were familiar with the American Medical Association Managing Mental Health during COVID-19 resource and the Suicide Prevention Lifeline, respectively.
Fig 2.
Coping strategies used by vascular surgeons in practice and training (n = 1366) as measured using the Brief Coping Orientation to Problems Experienced inventory.
Fig 3.
Most hospital support structures were associated with a reduction in self-reported anxiety levels among vascular surgeons as measured using the Generalized Anxiety Disorder 7-item scale while virtual social media based support platforms association to anxiety levels was mixed. COVID-19, Coronavirus disease 2019; PPE, personal protective equipment; SVS, Society for Vascular Surgery.
Multivariable analysis of factors associated with increased self-reported anxiety levels
A total of 1273 respondents (79.2%) had completed the entire survey. Of these 1273 respondents, 1259 (78.2%) had complete data available suitable for multivariable analysis of factors associated with increased self-reported anxiety. The previously presented significant findings were observed using ordinal univariable regression analysis to examine the association between stressors and support structures and the odds of increased self-reported anxiety (Table II ). As the hospital support increased, the odds of greater anxiety decreased (odds ratio [OR], 0.84; 95% confidence interval [CI], 0.78-0.89). More specifically, for every one-unit increase in the summative hospital support, the odds of no anxiety vs mild, moderate, or severe (ie, greater) anxiety was decreased by 16% (ie, [1 − 0.84] × 100%). In contrast, the following factors were associated with increased odds of greater anxiety (Table II):
-
1.
Female gender
-
2.
COVID-19-related modifications of home routine after work: staying in a separate room at home or staying at the hospital or hotel
-
3.
COVID-19-related stressors: donning and doffing PPE, worry about potential adverse patient outcomes due to delayed care, and financial concerns
-
4.
The following active coping strategies: use of emotional support, positive reframing, and planning
-
5.
The following avoidant coping strategies: self-distraction, substance abuse, behavioral disengagement, venting, and self-blame
Table II.
Univariable and multivariable ordinal logistic regressiona
| Variable | Univariable |
Multivariable |
||
|---|---|---|---|---|
| OR (95% CI) | P value | OR (95% CI) | P value | |
| Gender | 2.20 (1.79-2.71) | <.001 | 1.39 (1.08-1.79) | .010 |
| COVID-19-related modifications of home routine | 1.75 (1.50-2.05) | <.001 | 1.38 (1.14-1.67) | .001 |
| COVID-19-related stressors | ||||
| Donning/doffing PPE | 3.87 (3.10-4.84) | <.001 | 1.81 (1.41-2.33) | <.001 |
| Worry about potential adverse patient outcomes due care delay | 2.68 (2.18-3.31) | <.001 | 1.47 (1.16-1.87) | .002 |
| Financial concerns | 3.13 (2.54-3.85) | <.001 | 1.90 (1.49-2.42) | <.001 |
| Summative hospital supportb | 0.84 (0.78-0.89) | <.001 | 0.83 (0.76-0.91) | .001 |
| Active coping strategies | ||||
| Use of emotional support | 1.41 (1.33-1.50) | <.001 | 1.09 (1.01-1.18) | .028 |
| Positive reframing | 1.16 (1.10-1.23) | <.001 | 0.88 (0.81-0.95) | .001 |
| Planning | 1.37 (1.29-1.45) | <.001 | 1.12 (1.03-1.21) | .008 |
| Avoidant coping strategies | ||||
| Self-distraction | 1.66 (1.55-1.78) | <.001 | 1.32 (1.21-1.43) | <.001 |
| Substance abuse | 1.53 (1.43-1.65) | <.001 | 1.16 (1.06-1.27) | .001 |
| Behavioral disengagement | 1.77 (1.63-1.93) | <.001 | 1.26 (1.14-1.39) | <.001 |
| Venting | 2.17 (1.99-2.37) | <.001 | 1.42 (1.28-1.59) | <.001 |
| Self-blame | 2.12 (1.93-2.32) | <.001 | 1.35 (1.21-1.51) | <.001 |
CI, Confidence interval; COVID-19, coronavirus disease 2019; OR, odds ratio; PPE, personal protective equipment.
A proportional odds cumulative logit model was used of factors associated with an increasing degree of self-reported anxiety (no, mild, moderate, and severe anxiety) by 1259 respondents who had completed the Generalized Anxiety Disorder 7-item survey. The model was built in two steps. First, all factors significant on univariable analysis (also listed in Supplementary Table II and Supplementary Fig 2 (online only), Supplementary Fig 3 (online only), Supplementary Fig 4 (online only), Supplementary Fig 5 (online only)) were considered for entry into the model using a stepwise selection process (with the exception of the active and avoidant coping strategies from the Brief Coping Orientation to Problems Experienced survey). Second, the variables selected in the first step were retained, and the active and avoidant coping strategies were included in a stepwise selection process.
Summative hospital support was created as a sum of the significant individual hospital support variables, including “operating room protocols,” “adequate personal protective equipment,” “preoperative testing of patients,” and “opportunities to interact with leadership,” because they all correlated. “Transparency from leadership about COVID-19 management and planning” was not included because the responses were nearly identical to those for “opportunities to interact with leadership.”
Qualitative analysis
A total of 370 free text responses from 229 respondents (14.2%) shared opinions and emotions. These ranged from seeing the positive aspects of the pandemic such as “Despite all the uncertainty and challenges, the time is exciting to be part of as a provider in deciding on how best to care for a ‘new’ disease” and offering the perspective of the surgeon that we “do more things than operate” to despair “It's a total disaster on all levels of my life.” Three broad themes were identified in the responses: (1) worry and concern for others; (2) stress associated with uncertainty; and (3) financial implications (Table III ).
Table III.
The three broad themes identified in the qualitative analysis of the free text responses
| Theme 1: worry and concern for others |
| Patients |
| “A big concern for me is the indefinite postponement of semi-elective procedures, such as fistulas or revascularization for stable nonhealing wounds/very short distance claudication.” |
| “Many primary care docs have closed entirely, making access to care more difficult for patients.” |
| “I continue to be concerned about the response to COVID patients, specifically the impacts on racial and ethnic minority patients affected by this virus.” |
| “Patients will die from MI, CVA, ruptured aneurysm, aortic valve stenosis, etc. because they are too afraid to come to the hospital.” |
| “There is concern for capability to service the pent up demand created by the delay in vascular care” |
| Family, friends, and colleagues |
| “Upsetting to follow from afar close friends and colleagues being inundated and at risk and little we can do to help. Feel very distant and helpless with family, aging parents across the country and banned from visiting, helping.” |
| “The nurses and ancillary staff taking care of these patients are the truly exceptional people in this pandemic. They often have limited resources and have the most intimate contact with these patients and serve as the primary sources of information for multiple people including physicians and patient families.” |
| Trainees |
| “We have decreased their time physically in the hospital to limit exposure but I don't think they are actually using their time away to read or better themselves from a surgeon standpoint. I worry that a lot of them will fall behind and that they won't get their required numbers.” |
| “Worried about graduating experience given complete stoppage of elective vascular cases.” |
| Theme 2: stress associated with uncertainty |
| Disease process |
| “The big challenge is that a number of patients may be positive and yet be asymptomatic or low symptoms, making it difficult to know. Clearly until we have vigorous testing, we are all in the dark.” |
| “The constant stress to know that many patients could be asymptomatic COVID-19 carriers” |
| “I am disturbed by the lack of PPE, the expectation that providers work without adequate PPE.” |
| Future |
| “The unknown is the worst part. The unknown of how long this is going to be affecting my practice, affecting our lives.” |
| “I'm aware that this is a long term condition, and we have to adapt to it. PPE is going to be there for at least 2 years or even more. We should learn to work and live with it.” |
| Lack of guidelines that account for variation in disease severity |
| “Need guidelines for small office practice where risks are extremely low (one patient in office at a time). Currently restrictions are overkill in this setting.” |
| “The outbreak is local and regional and different institutions have different readiness, etc. and are able to be more flexible in not forgetting about the rest of the population needing health care.” |
| “The need for testing for COVID or not changes every day. The way to manage the OR patient is very dependent on the level of stress of the anesthesia team and nursing. No clear guidelines… . We should manage things locally and not nationally [be] cause every community has [a] different reality.” |
| Theme 3: financial stress |
| “I fear for the ability of our private practice to endure through this financially. I personally won't have the financial means to carry myself for any extended amount of time in order to carry the practice.” |
| “Our large academic hospital-owned physician group announced likelihood of salary cuts starting end April. So more stress, insult to injury, and bad news to come.” |
| “Last month (March) I took a 40% pay cut. This month I am not getting any salary but still working as a vascular surgeon. We furloughed more than half our office staff including US techs and nurses in our OBL… . The exposures to COVID-19 from placing lines continues but it doesn't pay the bills.” |
| “I don't know how long I can keep going without operating. I was just starting to build a practice in my area and I worry that this is going to be a big setback for practice development.” |
OBL, Office-based laboratory; COVID-19, coronavirus disease 2019; CVA, cerebrovascular accident; OR, operative room; PPE, personal protective equipment; techs, technicians; US, ultrasonography.
The most prevalent theme was concern for others, most often patients. Participants expressed fear for patients because of the consequences of delays in care from postponed operations, closed clinics, and patients being afraid to come to the hospital for medical emergencies. Family, friends, and colleagues, especially those working on the front lines of the pandemic, were a major source of worry for vascular surgeons. The respondents also conveyed anxiety for trainees, especially those who had been redeployed to the front lines, and for the potential effects that a lack of operative experience during the pandemic could have on training.
The second theme was the stress associated with uncertainty, which had three subthemes. The first subtheme was uncertainty regarding the disease process, especially asymptomatic carriers, which was related to the stress of not having enough PPE to be able to protect oneself to the extent necessary. The second subtheme was uncertainty regarding the future, specifically when and how the practice of medicine can return to a semblance of routine and the effects of this pandemic on how one practices medicine. The final subtheme was uncertainty regarding the lack of clear guidelines, associated with the lack of an evidence base, the rapidly changing state of the pandemic, and challenges that variations in the severity of the pandemic in different geographic regions and institutions have posed to creating universal guidelines.
Finally, although some respondents were grateful for being in a profession in which providers still have a source of income or having the privilege of having adequate monetary savings, most respondents expressed anxiety regarding the effects of the pandemic on the financial viability of their practices and their institutions.
Discussion
The psychological impact of the COVID-19 pandemic on healthcare providers cannot be overstated. More than one half of the survey respondents reported some degree of anxiety, and 23.3% reported moderate or severe anxiety. Using the threshold score for moderate or severe anxiety, the GAD-7 scale has a sensitivity and specificity of 89% and 82%, respectively, for generalized anxiety disorder and is moderately good at screening for post-traumatic stress disorder (66% sensitivity, 81% specificity).8 The results of our survey have provided largescale global understanding of the current stressors, coping strategies, and opportunities to mitigate the stressors and anxieties of vascular surgeons during the COVID-19 pandemic.
Most vascular surgeons were concerned about family members becoming infected. Education about transmissibility based on what is known might help allay such fears. Routines to minimize family contact with contaminated clothing such as a having a change of clothes available on return from the hospital, immediate access to laundry and shower facilities on arrival home have been adopted by some to combat these concerns. In our survey, after-work routines involving separation from the family were associated with higher self-reported anxiety levels. Unsurprisingly, concern regarding the lack of PPE and the stress of donning and doffing PPE were also associated with higher anxiety levels, as reported by earlier studies.12, 13, 14 Although the provision of adequate PPE has been challenged by rapid depletion, hospital leadership can provide organizational forms of support that might mitigate anxiety. This support could include updates of available PPE, protocols for reuse, and updates on additional procurement strategies. Having in-person teaching and dedicated staff to supervise donning and doffing of PPE before entering a patient's room and posting protocols for donning and doffing could also serve as methods to mitigate anxiety.13 , 14
A significant number of vascular surgeons who were worried about adverse outcomes for their patients had higher self-reported anxiety levels. One might hypothesize that they are at risk of moral injury, which occurs when we perpetrate, bear witness to, or fail to prevent an act that transgresses our deeply held moral beliefs.15 , 16 As physicians, our deeply held moral belief is always to prioritize the needs of patients first (a theme that was obvious in the qualitative analysis of the free text). Potential adverse outcomes for patients could ensue from the cancellation of scheduled surgical cases due to the reluctance of patients to present to the hospital because of COVID-19-related fear or in the context of COVID-19-induced resource scarcity. Every time physicians are forced to make a decision that transgresses their patients' best interests, they could feel moral injustice. This will increase with repetition into moral injury, a discrete phenomenon from that of burnout.17 Prevention of such must be prioritized.
Another significant COVID-19-related stressor across all groups was related to financial concerns. Solo, private, and community-based practitioners reported significantly higher anxiety levels related to economic changes compared with those working in academic centers. This finding might be associated with the continuous practice overhead cost burden and the drastic reduction of revenues and a lack of significant financial reserves to absorb the economic impact. Strategies to mitigate this impact might be achieved by reducing banked vacation hours, a hiring freeze, furloughs, and salary reduction—all of which would be preferable to layoffs. Support in navigating and applying for government assistance programs could be a valuable tool shared among vascular surgeons and an essential point for advocacy.18
The present study was limited by the reliance on self-report, which can be affected by recall bias, social desirability, and respondent selection bias. Recall bias was addressed by the short dissemination period of 10 days and asking about current experiences limited to the previous 2 to 4 weeks. The anonymous nature of the survey mitigated social desirability bias. A response bias was difficult to predict under the pandemic circumstances. It is possible that the response rate was lower among those most severely affected because of time restraints and feeling overworked at the peak of the pandemic. Alternatively, those most severely affected by the pandemic might have had a greater desire to respond, thus taking the 15 to 20 minutes required to complete the survey to share their experience. We addressed sampling by applying broad dissemination methods. Because of the wide and multimodal dissemination, we were unable to account for an exact response rate; however, this sacrifice ensured a significant participation in the survey. We did not specifically focus on regional variations in the present report because of space limitations; however, additional analysis will be performed to evaluate the differences by region. Finally, the survey was only available in English, potentially limiting the involvement of surgeons with a different primary language.
The present survey was a first step in understanding the psychological impact of COVID-19 on vascular surgeons. Survey respondents reported using more active than avoidant coping strategies. Fewer than 20% of respondents engaged in avoidant strategies, with the exception of “self-distraction.” This is highly relevant because active coping has been considered a more effective method of managing stress, and avoidant coping often exacerbates stress by ignoring the source of the stress.19 A recent report by Pinto et al20 found that self-distraction (mental disengagement) was predictive of traumatic stress after a major surgical complication. An understanding of the coping strategies used offers insight into the opportunities to provide support for colleagues.
Previous experiences with severe acute respiratory syndrome and Middle East respiratory syndrome have shown that psychologic distress persists after the immediate threat of an outbreak has subsided.21, 22, 23, 24, 25 We anticipate the return to a “new normal” with a fundamentally different life than in the pre–COVID-19 era and expect a period of high clinical demands as we care for patients who have had their care delayed. During this period, it will be essential to allow for time to reflect, grieve, and process what has been lost.26
However, relying on coping mechanisms is not enough. Vascular surgeons are already known to experience significant burnout.27 Institutional support via multidisciplinary teams focused on health care workers and peer support programs are paramount in bolstering the resilience and coping of vascular surgeons.28 , 29 Vascular surgeons who perceived that they had hospital support were more likely to report lower anxiety levels, especially when delivered through structured protocols and opportunities to interact with leadership. The importance of support, coupled with genuine expressions of gratitude, cannot be overstated.12 , 30 Additional regional and national societal assistance through bolstering peer-to-peer support systems and providing COVID-19–specific clinical guidelines can also help mitigate anxiety among vascular surgeons.31 These resources remain highly relevant because more than one half the respondents were familiar with societal support programs.
Finally, strategies to combat the prolonged time of uncertainty, decreased production, fear of a second surge, and exhaustion created from ongoing anxiety will need to be considered as we continue to adapt to the rapid changes resulting from COVID-19. We look for guidance and support from national organizations as we proactively adjust our lives and careers through the pandemic. Future survey evaluations of new guidelines and support systems are warranted. Perhaps the most important contribution of the present study will be allowing vascular surgeons to understand that they are not alone and that the COVID-19 pandemic is associated with increased anxiety and stress to a group of surgeons who are well adapted to functioning in high-stress environments. Acknowledging this fact might allow surgeons to seek help when needed.
Conclusions
The findings from the present survey have identified multiple stressors experienced by vascular surgeons globally during this devastating crisis. The survey findings have highlighted the continued need for hospital systems to support their vascular surgeons and for national societies to invest in peer support programs to promote the well-being of vascular surgeons during the COVID-19 pandemic.
Author contributions
Conception and design: SC, AJ, RM, NM, SS, MW
Analysis and interpretation: RC, DC, SC, CL, RM, NM, SS, MS, KW
Data collection: SS
Writing the article: SC, AJ, RM, NM, SS
Critical revision of the article: RC, DC, SC, AJ, CL, RM, NM, SS, MS, MW, KW
Final approval of the article: RC, DC, SC, AJ, CL, RM, NM, SS, MS, MW, KW
Statistical analysis: CL, SS, KW
Obtained funding: Not applicable
Overall responsibility: SS
Acknowledgments
We thank the survey respondents for their time and insights. We also thank the following organizations for helping to disseminate this survey: Association of Program Directors in Vascular Surgery, Audible Bleeding: The Vascular Surgery Podcast, Canadian Society for Vascular Surgery, Chilean Society for Vascular Surgery, German Vascular Research Group, Houston Aortic Symposium, Italian Vascular Society, Japanese Vascular Surgeon Network, SBACV LEMBRA, VA Vascular Surgeons, Endovascular Trauma and Resuscitation Management Society, Australian and New Zealand Society for Vascular Surgery, Vascular and Endovascular Research Network, Singapore Vascular Surgical Collaborative, Vascular Surgery COVID-19 Collaborative, Vascular Low Frequency Disease Consortium, and the Vascular Specialist. We also thank the following individuals for helping to disseminate this survey: Rana Afifi, MD, Fowzan Alkuraya, MD, Marta Ballesteros-Pomar, MD, Hiroshi Banno, MD, Ruth Benson, MD, Christian-Alexander Behrendt, MD, Tomasso Cambiaghi, MD, Andrew Choong, MD, Jason Chuen, MD, Raphaël Coscas, MD, Sharif Ellozy, MD, Thomas Forbes, MD, Edoardo Galeazzi, MD, Flavia Gentile, MD, Andrew Hill, MD, Tal Horer, MD, Rebecka Hultgren, MD, Ahmed Kayssi, MD, Jose Ramon March, MD, Germano Massano, MD, Laura Nicolai, MD, Leigh Ann O'Banion MD, Oscar Ojeda, MD, Gabriel López Peña, MD, Asaf Rabin, MD, Rebecca Reachi, MD, Joy Roy, MD, Ajay Savlania, MD, Murray Shames, MD, Marcone Lima Sobreira, MD, Akiko Tanaka, MD, Gale Tang, MD, Francisco Vargas, MD, Melina Vega, MD, and La Wu, LSA.
From the Society for Vascular Surgery
Footnotes
Author conflict of interest: none.
Additional material for this article may be found online at www.jvascsurg.org.
The editors and reviewers of this article have no relevant financial relationships to disclose per the JVS policy that requires reviewers to decline review of any manuscript for which they may have a conflict of interest.
Additional material for this article may be found online at www.jvascsurg.org.
Appendix (online only).
Supplementary Table I (online only).
Multimodal survey dissemination, potential audience, and estimated response rate
| Organization | Date of dissemination | Potential audience |
|---|---|---|
| Society for Vascular Surgery and affiliated organizations | ||
| Society for Vascular Surgery e-mail lista | April 14, 2020 | 3528 |
| Association of Program Directors in Vascular Surgery e-mail list | April 15, 2020 | 223 |
| Current number of U.S. vascular surgery traineesb | 638 | |
| SVS Connect | April 17, 2020 | 1203 |
| Vascular Specialist Magazinec | April 16, 2020 | 399 |
| Other outreach platforms | ||
| Vascular Surgeons COVID-19 WhatsApp | April 14, 2020 | 256 |
| Vascular Low Frequency Disease Consortium mailing | April 15, 2020 | 30 |
| Brazilian Society of Angiology and Vascular Surgery | April 15, 2020 | 3500 |
| Veterans Affairs vascular surgeons | April 15, 2020 | 97 |
| Social media outreach | ||
| Vascular SVS: @VascularSVS | April 16, 2020 | 5913 |
| Vascular Specialist Online: @VascularOnline | April 16, 2020 | 351 |
| Audible bleeding: @Audiblebleeding | April 16, 2020 | 985 |
| CanadianSVS Twitter: @CanadianSVS | April 18, 2020 | 684 |
| GermanVasc: @VASCevidence | April 18, 2020 | 440 |
COVID-19, Coronavirus disease 2019; SVS, Society for Vascular Surgery.
On April 14, 2020, e-mail letters were sent to 3528 recipients; 3525 were received (3 bounced). Of those received, 1866 were opened (52.9%), and 381 had accessed the survey directly from the e-mail link. On April 23, 2020, a reminder e-mail was sent to the same list. Of these, 1263 were opened (35.8%), and 134 accessed the survey directly from the e-mail, suggesting that 515 respondents had been reached via the SVS e-mail list, and accounting for ∼16.5% if all e-mail letters opened.
The current number of vascular surgery trainees in the United States is 638; therefore, the response rate was 23% (145 of 638).
Supplementary Table II (online only).
Pearson χ2 analysis of factors associated with differences in self-reported anxiety degreea
| Factor | Degree of Anxiety, No. (% within each degree) |
P valueb | |||
|---|---|---|---|---|---|
| No | Mild | Moderate | Severe | ||
| Gender | <.001 | ||||
| Male | 555 (52.1) | 299 (28.1) | 131 (12.3) | 80 (7.5) | |
| Female | 130 (29.5) | 172 (39.1) | 89 (20.2) | 49 (11.1) | |
| Practice duration (n = 1518) | <.001 | ||||
| In training | 94 (13.6) | 82 (17.3) | 29 (13) | 18 (13.7) | |
| In practice <10 years | 197 (28.5) | 170 (35.9) | 104 (46.6) | 44 (33.6) | |
| In practice 10-20 years | 185 (26.8) | 115 (24.3) | 51 (22.9) | 38 (29) | |
| In practice >20 years | 215 (31.1) | 106 (22.4) | 39 (17.5) | 31 (23.7) | |
| Leadership position (n = 1250) | .017 | ||||
| In a leadership position | 326 (50.1) | 182 (28) | 85 (13.1) | 58 (8.9) | |
| Not in a leadership position | 252 (42.1) | 193 (32.2) | 104 (17.4) | 50 (8.3) | |
| Elective cases (n = 1303) | .583 | ||||
| Cancelled | 516 (45.1) | 356 (31.1) | 163 (14.3) | 108 (9.4) | |
| Not cancelled | 81 (50.6) | 47 (29.4) | 20 (12.5) | 12 (7.5) | |
| ICU beds available (n = 1234) | .125 | ||||
| Available | 493 (47.4) | 315 (30.3) | 139 (13.4) | 92 (8.9) | |
| Not available | 75 (38.5) | 69 (35.4) | 33 (16.9) | 18 (9.2) | |
| Operated/placed a central catheter for a patient with COVID-19 infection (n = 1518) | .296 | ||||
| Yes | 475 (42.2) | 367 (32.6) | 175 (15.6) | 108 (9.6) | |
| No | 138 (63.9) | 48 (22.2) | 15 (6.9) | 15 (6.9) | |
| Considered at “high” risk of COVID-19 infection (n = 1514) | .003 | ||||
| Yes | 228 (39) | 199 (34) | 99 (16.9) | 59 (10.1) | |
| No | 462 (49.7) | 272 (29.3) | 123 (13.2) | 72 (7.8) | |
| Stressor | |||||
| Lack of PPE (n = 1150) | <.001 | ||||
| Stressful | 364 (40.2) | 307 (33.9) | 137 (15.1) | 97 (10.7) | |
| Not stressful at all | 166 (67.8) | 53 (21.6) | 20 (8.2) | 6 (2.4) | |
| Donning/doffing PPE (n = 1290) | <.001 | ||||
| Stressful | 345 (37.2) | 318 (34.3) | 156 (16.8) | 108 (11.7) | |
| Not stressful at all | 243 (66.9) | 81 (22.3) | 27 (7.4) | 12 (3.3) | |
| Potential adverse patient outcomes due to care delay (n = 1314) | <.001 | ||||
| Stressful | 496 (42.7) | 375 (32.3) | 176 (15.2) | 114 (9.8) | |
| Not stressful at all | 104 (68) | 32 (20.9) | 8 (5.2) | 9 (5.9) | |
| Financial concerns (n = 1314) | <.001 | ||||
| Stressful | 459 (41.8) | 353 (32.1) | 169 (15.4) | 117 (10.7) | |
| Not stressful | 140 (64.8) | 54 (25) | 17 (7.9) | 5 (2.3) | |
| Terminating contracts of some employees (n = 831) | <.001 | ||||
| Stressful | 167 (35.7) | 167 (35.7) | 87 (18.6) | 47 (10) | |
| Not stressful | 204 (56.2) | 98 (27) | 33 (9.1) | 28 (7.7) | |
| Impact of this hiatus on my career advancement (n = 1143) | <.001 | ||||
| Stressful | 258 (35.3) | 254 (34.8) | 134 (18.4) | 84 (11.5) | |
| Not stressful | 255 (61.7) | 105 (25.4) | 33 (8) | 20 (4.8) | |
COVID-19, Coronavirus disease 2019; ICU, intensive care unit; PPE, personal protective equipment.
Defined as no, mild, moderate, and severe anxiety.
Represents the significance of the difference in the degree of anxiety when comparing each set of factors.
References
- 1.Lai J., Ma S., Wang Y., Cai Z., Hu J., Wei N., et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. 2020;3:e203976. doi: 10.1001/jamanetworkopen.2020.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C.S., et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health. 2020;17:1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ng J.J., Ho P., Dharmaraj R.B., Wong J.C.L., Choong A. The global impact of COVID-19 on vascular surgical services. J Vasc Surg. 2020;71:2182–2183.e1. doi: 10.1016/j.jvs.2020.03.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hemingway J.F., Singh N., Starnes B.W. Emerging practice patterns in vascular surgery during the COVID-19 pandemic. J Vasc Surg. 2020;72:396–402. doi: 10.1016/j.jvs.2020.04.492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ben Abdallah I., La Collegiale A., Coscas R., Javerliat I., Goeau-Brissoniere O., Coggia M., et al. Early experience in Paris with the impact of the COVID-19 pandemic on vascular surgery. J Vasc Surg. 2020;72:373. doi: 10.1016/j.jvs.2020.04.467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Leong Tan G.W., Chandrasekar S., Lo Z.J., Hong Q., Yong E., Lingam P., et al. Early experience in the COVID-19 pandemic from a vascular surgery unit in a Singapore tertiary hospital. J Vasc Surg. 2020;72:12–15. doi: 10.1016/j.jvs.2020.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shalhub S., Mouawad N. COVID-19: socially distant yet never closer. Vascular Specialist. https://vascularspecialistonline.com/covid-19-socially-distant-yet-never-closer/ Available at:
- 8.Spitzer R.L., Kroenke K., Williams J.B., Lowe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166:1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- 9.Carver C.S., Scheier M.F., Weintraub J.K. Assessing coping strategies: a theoretically based approach. J Pers Soc Psychol. 1989;56:267–283. doi: 10.1037//0022-3514.56.2.267. [DOI] [PubMed] [Google Scholar]
- 10.Harris P.A., Taylor R., Thielke R., Payne J., Gonzalez N., Conde J.G. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Harris P.A., Taylor R., Minor B.L., Elliott V., Fernandez M., O'Neal L., et al. The REDCap consortium: building an international community of software platform partners. J Biomed Inform. 2019;95:103208. doi: 10.1016/j.jbi.2019.103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shanafelt T., Ripp J., Trockel M. Understanding and addressing sources of anxiety among health care professionals during the COVID-19 pandemic [e-pub ahead of print] JAMA. 2020;323:2133–2134. doi: 10.1001/jama.2020.5893. [DOI] [PubMed] [Google Scholar]
- 13.Baloh J., Reisinger H.S., Dukes K., da Silva J.P., Salehi H.P., Ward M., et al. Healthcare workers' strategies for doffing personal protective equipment. Clin Infect Dis. 2019;69(Suppl 3):S192–S198. doi: 10.1093/cid/ciz613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kang J., Kim E.J., Choi J.H., Hong H.K., Han S.H., Choi I.S., et al. Difficulties in using personal protective equipment: training experiences with the 2015 outbreak of Middle East respiratory syndrome in Korea. Am J Infect Control. 2018;46:235–237. doi: 10.1016/j.ajic.2017.08.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shay J. Moral injury. Psychoanalytic Psychology. 2014;31:182–191. [Google Scholar]
- 16.Dean W., Talbot S., Dean A. Reframing clinician distress: moral injury not burnout. Fed Pract. 2019;36:400–402. [PMC free article] [PubMed] [Google Scholar]
- 17.Jones E. Moral injury in time of war. Lancet. 2018;391:1766–1767. doi: 10.1016/S0140-6736(18)30946-2. [DOI] [PubMed] [Google Scholar]
- 18.Satiani B., Zigrang T.A., Bailey-Wheaton J.L. COVID-19 financial resources for physicians. J Vasc Surg. 2020 Apr 28 doi: 10.1016/j.jvs.2020.04.482. Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dijkstra M.T., Homan A.C. Engaging in rather than disengaging from stress: effective coping and perceived control. Front Psychol. 2016;7:1415. doi: 10.3389/fpsyg.2016.01415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pinto A., Faiz O., Bicknell C., Vincent C. Acute traumatic stress among surgeons after major surgical complications. Am J Surg. 2014;208:642–647. doi: 10.1016/j.amjsurg.2014.06.018. [DOI] [PubMed] [Google Scholar]
- 21.Chang C.S., Du P.L., Huang I.C. Nurses' perceptions of severe acute respiratory syndrome: relationship between commitment and intention to leave nursing. J Adv Nurs. 2006;54:171–179. doi: 10.1111/j.1365-2648.2006.03796.x. [DOI] [PubMed] [Google Scholar]
- 22.Chua S.E., Cheung V., Cheung C., McAlonan G.M., Wong J.W., Cheung E.P., et al. Psychological effects of the SARS outbreak in Hong Kong on high-risk health care workers. Can J Psychiatry. 2004;49:391–393. doi: 10.1177/070674370404900609. [DOI] [PubMed] [Google Scholar]
- 23.Tam C.W., Pang E.P., Lam L.C., Chiu H.F. Severe acute respiratory syndrome (SARS) in Hong Kong in 2003: stress and psychological impact among frontline healthcare workers. Psychol Med. 2004;34:1197–1204. doi: 10.1017/s0033291704002247. [DOI] [PubMed] [Google Scholar]
- 24.Khalid I., Khalid T.J., Qabajah M.R., Barnard A.G., Qushmaq I.A. Healthcare workers emotions, perceived stressors and coping strategies during a MERS-CoV outbreak. Clin Med Res. 2016;14:7–14. doi: 10.3121/cmr.2016.1303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.McAlonan G.M., Lee A.M., Cheung V., Cheung C., Tsang K.W., Sham P.C., et al. Immediate and sustained psychological impact of an emerging infectious disease outbreak on health care workers. Can J Psychiatry. 2007;52:241–247. doi: 10.1177/070674370705200406. [DOI] [PubMed] [Google Scholar]
- 26.Hartzband P., Groopman J. Physician burnout, interrupted. N Engl J Med. 2020;382:2485–2487. doi: 10.1056/NEJMp2003149. [DOI] [PubMed] [Google Scholar]
- 27.Janko M.R., Smeds M.R. Burnout, depression, perceived stress, and self-efficacy in vascular surgery trainees. J Vasc Surg. 2019;69:1233–1242. doi: 10.1016/j.jvs.2018.07.034. [DOI] [PubMed] [Google Scholar]
- 28.Shapiro J., Galowitz P. Peer support for clinicians: a programmatic approach. Acad Med. 2016;91:1200–1204. doi: 10.1097/ACM.0000000000001297. [DOI] [PubMed] [Google Scholar]
- 29.Albott C.S., Wozniak J.R., McGlinch B.P., Wall M.H., Gold B.S., Vinogradov S. Battle buddies: rapid deployment of a psychological resilience intervention for healthcare workers during the COVID-19 pandemic. Anesth Analg. 2020;131:43–54. doi: 10.1213/ANE.0000000000004912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Adams J.G., Walls R.M. Supporting the health care workforce during the COVID-19 global epidemic. JAMA. 2020;329:1439–1440. doi: 10.1001/jama.2020.3972. [DOI] [PubMed] [Google Scholar]
- 31.Hu Y.Y., Fix M.L., Hevelone N.D., Lipsitz S.R., Greenberg C.C., Weissman J.S., et al. Physicians' needs in coping with emotional stressors: the case for peer support. Arch Surg. 2012;147:212–217. doi: 10.1001/archsurg.2011.312. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.