Abstract
Background and Aims:
Oropharyngeal seal pressure (OSP) achieved by a supraglottic airway device holds due importance as it indicates the feasibility of positive pressure ventilation, the degree of airway protection from supra-cuff soiling and also relates to postoperative morbidity. The primary outcome measure was to assess and compare OSP in different head and neck positions with Baska mask® and I-gel™. Secondary outcome measures were to compare peak inspiratory pressure (PIP), exhaled tidal volume (ETV), ease of insertion, time taken for insertion, number of attempts, intraoperative manipulations, and postoperative airway morbidity with both the devices.
Materials and Methods:
Seventy consenting adults scheduled for a variety of surgical procedures under general anesthesia were allocated to Group B and Group G using Baska mask® and I-gel™ respectively. All statistical calculations were done using SPSS (Statistical Package for the Social Science). The comparison of quantitative variables between the study groups was done using Student t-test and within the variables was done by paired t-test. For comparing categorical data, Chi-square (χ2) test was performed.
Results:
OSP was significantly higher in group B than in group G in all head and neck positions (neutral 33 ± 2.8 vs. 23.2 ± 1.8, flexion 35.5 ± 2.5 vs. 25.2 ± 1.6, extension 30.6 ± 2.7 vs. 21.4 ± 1.7, right lateral 32.6 ± 2.8 vs. 23.0 ± 1.5. left lateral 32.6 ± 2.7 vs. 23.1 ± 1.7 cm H2O, respectively) (P = 0.000). PIP increased significantly in group G as compared to group B in flexion. (P = 0.009). Baska mask® had significantly higher ETV in flexion compared to I-gel™. (P = 0.009).
Conclusion:
Baska mask® may provide a useful alternative to I-gel™ where the glottic seal has precedence over ease of insertion.
Key words: Epiglottis, glottis, hoarseness, pharyngeal muscles, tidal volume
INTRODUCTION
Baska mask®, a third-generation supraglottic airway device (SGAD) recently being used in children, patients undergoing ambulatory surgeries and procedures requiring pneumoperitoneum facilitates a better airway seal which increases with intermittent positive pressure ventilation.[1,2,3] I-gel™ is another cuffless device made of soft gel-like thermoplastic elastomer to create an intimate interface for interaction with supraglottic tissue.[4] Till date there has been a paucity of randomised studies to compare oropharyngeal seal pressure (OSP) of Baska mask® with I-gel™. The primary objective of this study was to compare OSP in different head and neck positions and the secondary outcome measures were to compare peak inspiratory pressure, exhaled tidal volume, ease of insertion, time taken for insertion, number of attempts, intraoperative manipulations and postoperative airway morbidity using Baska mask® and I-gel™ in paralysed adult patients.
Materials and Methods
This prospective, randomised, study was conducted in a tertiary care hospital from March 2018 to August 2019 after Institutional Ethics Committee approval (REF/2018/03/018381, CTRI/2018/03/012888). The procedure follows the guidelines laid down in Declaration of Helinski 2013. After written informed consent, 70 American Society of Anaesthesiologists(ASA) grade I/II patients weighing 50–90 kg with body mass index (BMI) < 35 kg/m2, posted for surgical procedures of less than 2-h duration under general anaesthesia were included in the study. Patients having cervical spine disease, any history of gastroesophageal reflux disease, upper respiratory tract symptoms in the previous 10 days, mouth opening of <2.5 cm were excluded from the study. The patients were randomised into two groups: group B (Baska mask®) and group G (I-gel™) using computer-generated random numbers table (http://www.randomiser.org). The allocation was concealed in sealed opaque envelopes that were opened just before shifting the patient inside the operation theatre. It was impossible to blind the device operator due to obvious technical reasons, but investigators observing the patient in the postoperative period, those analysing the data and the participants were blinded to the group allocation. The placement of the device was done by an anesthesiologist who had an experience of inserting a minimum of 50 SGADs before this study and was not involved in the collection of data in this study. The anatomical placement of the device was confirmed by fibreoptic evaluation.
After pre-anesthetic check-up, patients were kept fasting for 8 h before surgery. Routine monitoring was done in the form of non-invasive blood pressure (NIBP), electrocardiography (ECG), pulse oximetry, and end-tidal carbon dioxide (ETCO2). Induction of anaesthesia was achieved with injection propofol in the dose of 2–2.5 mg/kg, morphine 0.1 mg/kg, and vecuronium 0.1 mg/kg intravenous to facilitate insertion of I-gel™ or Baska mask®. The patients were ventilated with 50% oxygen in nitrous oxide and 1% isoflurane. The integrity and function of the Baska mask® (Logikal Health Products PTY. Ltd, Morisset, NSW, Australia) and I-gel™ (Intersurgical Ltd. Wokingham, Berkshire, UK) were checked by occluding the airway opening of the proximal connector end with one thumb, holding the mask head with the other hand placing the other thumb over the airway opening of the mask to seal. The pressure was applied for 5 s using a reservoir-bag squeeze to confirm the absence of leak in the device.[5,6] The devices were lubricated with water-based gel before insertion. Size 3 and 4 of I-gel™ were used for patients weighing less than 50 kg and between 50 and 90 kg, respectively. Size 4 and 5 of Baska mask® were used for patients weighing between 50 and 70 kg and more than 70 kg, respectively. Effective ventilation was defined as SpO2>95%, ETCO2<50 mmHg and tidal volume >6 ml/kg. At the end of the surgery, the SGADs were removed when protective reflex returned to normal. The number of attempts required for an insertion were recorded and the failed attempt was defined as the removal of the device from the mouth before insertion. A maximum of three attempts were allowed and after that endotracheal tube was inserted for airway management and the patient was excluded from the study. OSP was measured by closing the expiratory valve of the circle system at a fixed gas flow of 3 L/min and noting the airway pressure (maximum allowed was 40 cm H2O) at which equilibrium was reached. The interobserver reliability and accuracy of this measuring system have already been validated.[7] The success of insertion was assessed by the number of insertion attempts (counted when Baska mask® and I-gel™ were taken in and out of a mouth). Ease of insertion was qualitatively evaluated using four-point scale.[8] The insertion time (the time between picking up the prepared mask and successful placement) was assessed in all the cases. The anatomical placement of both the devices in situ was assessed clinically and by fibreoptic evaluation (3.7 mm bronchoscope, Karl Storz, Tuttlingen, Germany)in neutral position based on Brimacombe scoring system.[9]
The neutral position was maintained with the external auditory canal level with the top of the shoulder and the ear line (from the external ear to the superior orbital margin) vertical and OSP, PIP, ETV, ETCO2 and fibreoptic grading were recorded in the neutral position. Then the patient was repositioned in the following positions: maximal extension which was achieved by extending neck till resistance was felt, maximal flexion (about 45° each) which was obtained by flexing the neck at a point when chin touches sternum and maximal rotation to the left or right (about 90°) as noted preoperatively. Each position change started from a neutral position after 30–60 s of the stable period and the depth of insertion of the SGAD constantly maintained as in neutral position. The readings of OSP, PIP, ETV, ETCO2 were taken 1 min after head and neck positions before the start of surgery. Postoperative airway morbidity such as sore throat, dysphagia, dysphonia graded as none, mild, moderate or severe, at 0, 2, and 24 h postoperatively were also noted. The sore throat was defined as constant pain or discomfort in the throat independent of swallowing; dysphonia was defined as difficulty in speaking or pain on speaking: dysphagia was defined as difficulty or pain provoked by swallowing.[10]
The data were described in terms of range; mean ± standard deviation (±SD), frequencies (number of cases), and relative frequencies (percentages) as appropriate. The comparison of quantitative variables between the study groups was done using Student t-test and within the variables was done by paired t-test. For comparing categorical data, Chi-square (χ2) test was performed and the exact test was used when the expected frequency was less than 5. A P value <0.05 was considered statistically significant. All statistical calculations were done using SPSS (Statistical Package for the Social Science) version 21 (IBM Corp. Armonk, N.Y, USA) statistical program for Microsoft Windows.
Group sample size of 31 in each group was calculated using a two-sided two-sample t-test. Taking results of our pilot study (10 patients in each group) as reference achieving at least 80% power to detect a difference of 7.45 between the null hypothesis and the mean OSP of Baska group is 31.67 cm of H2O and the alternative hypothesis mean of Igel group is 24.22 with known group standard deviations of 1.60 and 1.52, respectively, with a significance level α of 0.05. Taking into consideration the possible attrition rate of 10%, a sample size of 35 in each group was taken for the study.
RESULTS
Seventy enrolled patients completed the study [Figure 1]. These patients were comparable concerning demographic profile [Table 1]. Haemodynamic variables and ETCO2 were comparable in both the groups and the difference was statistically insignificant (P > 0.05).
Figure 1.
Consort Flowchart
Table 1.
Comparison of demographic data in both groups
| Group B (n=35) | Group G (n=35) | P | |
|---|---|---|---|
| Weight (kg) | 60.06 (5.58) | 58.46 (6.09) | 0.256 |
| ASA grade (I/II) | 16/19 | 18/17 | 0.632 |
| Gender (male/female) | 25/10 | 27/8 | 0.584 |
| Duration of surgery (min) | 57.57 (3.51) | 56.57 (3.98) | 0.269 |
| Device size | 6/29 | 8/27 | 0.550 |
All variables except ASA status, gender and device size are expressed as mean (SD). Group B stands for Baska mask® group and group I stand for I-gel group
OSP was significantly higher in the Baska mask® group than in the I-gel™ group in all head and neck positions (P = 0.000) [Figure 2]. In both the groups, mean OSP increased in flexion as compared to the neutral position (P = 0.000) and decreased in extension as compared to the neutral position (P = 0.164). Change in mean OSP was insignificant in lateral rotation of the neck [Figure 2]. In the present study, peak inspiratory pressure (PIP) increased significantly in both Baska mask® and I-gel™ group with the change in position from neutral to flexion (P = 0.009). It was observed that there was a decrease in mean PIP in extension as compared to the neutral position with the devices but the difference was not statistically significant (P > 0.05). Mean PIP in lateral rotation of neck was insignificant in both the groups in comparison to neutral position (P > 0.05) [Table 2]. The percentage increase in PIP from neutral to flexion was significantly more with I-gel™ compared to Baska mask® (52% vs. 33.7%; P = 0.010). The percentage change in mean PIP from neutral to extension with Baska mask® and I-gel™ was 29.5% and 32% (P = 0.262), respectively. Baska mask® had significantly higher exhaled tidal volume (ETV) in flexion compared to I-gel™ (P = 0.009). There was significantly greater percentage decrease in ETV with I-gel™ compared to Baska mask® during flexion (45.2%, vs. 30.6%, P = 0.00) [Table 3]. In the present study fibreoptic bronchoscopy revealed that 40%of patients (n = 40) in Baska mask® and 51% (n = 18) in I-gel™ group had score 4, 22.9% (n = 8) in Baska mask® group, and 25.7% (n = 9) in I-gel™ group had score 3, score 2 views in 17.1% of patients (n = 6) in each group, 20% patients (n = 7) in the Baska mask® group, and 5.7% (n = 2) in the I-gel™ group had score 1 view of the glottis. But ventilation was not compromised in any of the grades as evidenced by maintained ETCO2. Time taken for device insertion was less in the I-gel™ group than Baska mask® group (12.14 ± 2.61 s vs. 15.80 ± 5.39 s) and the difference was statistically significant (P = 0.001). First attempt insertion success was better with I-gel™ group then Baska mask® group but the difference was statistically insignificant (P = 0.137). None of the patients in both groups required a third attempt or tracheal intubation. Device insertion was very easy in the I-gel™ group as compared to the Baska mask® group but the results were not statistically significant (P = 0.203). Both the groups required intraoperative manipulations in the form of pushing and pulling of the device but the difference was statistically insignificant (P > 0.05). The blood staining of the device on removal was seen in 6 patients in group B and 3 patients in group G but the difference was statistically insignificant (P = 0.284). In the present study sore throat was assessed immediately postoperatively, at 2 h and 24 h. In the immediate postoperative period, 7 patients in group B and 2 patients in group G while at 2 h postoperatively, 3 patients in group B and 1 patient in group G had a sore throat. But the difference was statically insignificant. At 24 h postoperatively none of the patients complained of sore throat in any group.
Figure 2.
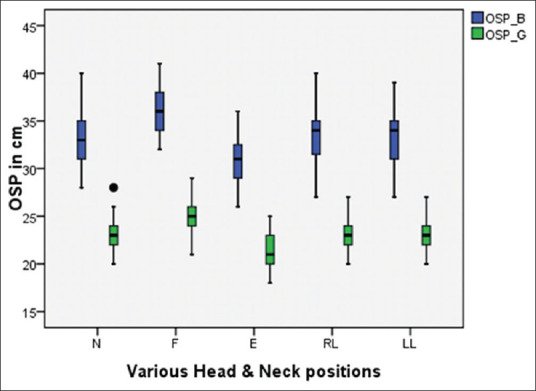
Oropharyngeal seal pressures (OSP) achieved with the Baska mask® and I-gel™ in different head and neck positions. The bottom and top of the box are the first and third quartiles, the band inside the box is the median value, the whiskers represent the 10th percentile and the 90th percentile and the black dots represent outliers
Table 2.
Comparison of peak inspiratory pressure and exhaled tidal volume in both groups in different head and neck positions
| Positions | PIP (cm H2O) |
ETV (ml/kg) |
||||
|---|---|---|---|---|---|---|
| Mean (SD) | P | Mean (SD) |
P | |||
| Group B | Group G | Group B | Group G | |||
| N | 11.4 (1.3) | 11.1 (1.3) | 0.157 | 7.31 (0.7) | 7.1 (0.8) | 0.08 |
| F | 15.1 (1.7) | 16.0 (1.2) | 0.009 | 5.0 (1.1) | 4.5 (1.1) | 0.009• |
| E | 8.0 (2.1) | 7.5 (1.5) | 0.087 | 9.0 (0.8) | 8.9 (0.8) | 0.168 |
| RL | 12 (1.6) | 11.6 (1.6) | 0.178 | 7.1 (1.0) | 7.3 (1.4) | 0.346 |
| LL | 12.2 (1.8) | 11.6 (1.6) | 0.169 | 7.2 (1.0) | 7.3 (1.4) | 0.288 |
Peak Inspiratory Pressure (PIP), Exhaled Tidal Volume (ETV) achieved in different head and neck positions. Data is expressed as mean±SD; *P<0.05 is considered significant. N – Neutral, F – Flexion, E – Extension, RL – Right lateral, LL – Left lateral. Group B stands for Baska mask® group and Group G stands for I gel group
Table 3.
Percentage change in oropharyngeal seal pressure, peak inspiratory pressure and exhaled tidal volume with change in position from neutral with Baska mask®® and I-gel™
| Mean |
SD |
%change |
Mean |
SD |
%change |
P |
|
|---|---|---|---|---|---|---|---|
| Baska | I-gel | ||||||
| OSP (cmH2O) | |||||||
| N-F | −2.54 | 1.12 | 10.19 | −2.03 | 0.89 | 7.04 | 0.00• |
| N-E | 2.37 | 0.77 | 7.19 | 1.80 | 0.63 | 7.76 | 0.164 |
| N- RL | 0.37 | 0.49 | 1.12 | 0.06 | 0.64 | 0.34 | 0.075 |
| N-LL | 0.31 | 0.68 | 0.96 | 0.09 | 0.66 | 0.25 | 0.119 |
| PIP (cmH2O) | |||||||
| N-F | 3.7 | 2.0 | 33.74 | 5.6 | 1.6 | 52 | 0.010• |
| N-E | 3.4 | 2.0 | 29.55 | 3.7 | 1.9 | 32 | 0.262 |
| N-RL | −0.6 | 2.1 | 6.46 | 0.1 | 2.4 | 1 | 0.145 |
| N-LL | −0.7 | 2.2 | 8 | −0.3 | 2.0 | 4 | 0.216 |
| ETV (ml/kg) | |||||||
| N-F | 2.3 | 1.3 | 30.63 | 3.2 | 1.1 | 45.16 | 0.00 |
| N-E | −1.7 | 1.1 | 24.76 | −1.8 | 1.2 | 27.28 | 0.288 |
| N-RL | 0.2 | 1.4 | 0.85 | −0.3 | 1.4 | 4.68 | 0.138 |
| N-LL | 0.1 | 1.4 | 0.14 | −0.2 | 1.5 | 3.61 | 0.242 |
Data expressed as difference in means (SD) (percentage change). *P<0.05 is considered significant. OSP – Oropharyngeal seal pressures, PIP – Peak inspiratory pressure, ETV – Exhaled tidal volume, SD=Standard deviation
DISCUSSION
In this study, Baska mask® (BM) demonstrated an increase in OSP in all the positions as compared to I-gel™ (P = 0.000) [Figure 2]. Our findings are consistent with the study done by Al-Rawahi SAS et al. in which they have compared PLMA with BM and found significantly higher OSP with BM as compared to PLM.[11] Higher OSP was achieved with PLMA as compared to I-gel™ by Jadhav et al.[12] There is a paucity of studies comparing Baska mask® with I-gel™ in various head and neck positions, so from these studies we conclude the superiority of Baska mask® over I-gel™ regarding OSP. Our findings regarding higher OSP with BM compare well with those reported by Alexiev et al. and Lopez et al.[2,13] Higher OSP with Baska mask can be attributed to the type of material used in the manufacturing of these devices. Baska mask® is made of silicone with the potential to operate normally from -100 to 300°C, while the material used for I-gel™, that is, styrene ethylene butadiene styrene which was expected to warm up to body temperature and result in improved perilaryngeal seal has not been affirmed in clinical practice.[4,14]
Both BM and I-gel™ are Peri-laryngeal (PL) sealers, but in BM there is self-energising mechanism of seal.[15] OSP increased with flexion (P = 0.000) and decreased with extension of the neck (P = 0.164) as compared to neutral position with both the devices. Similar results have been reported in studies using different SGADs in both children and adults.[16,17] Flexion results in a decrease in the longitudinal tension on anterior pharyngeal muscles, which settle over the mask of SGADs providing better seal and reverse is seen during extension. In the current study, group B resulted in a 10.2% increase in mean OSP compared to 7% with I-gel™ from neutral to the flexed neck position. (P = 0.000), which can be accredited to larger and more compliant Baska mask® as compared to I-gel™. In another study by Gupta et al. higher OSP was observed with I-gel™ compared to LMA supreme but there was17.5% increase in OSP with I-gel™ as compared to 18.5% increase with LMA supreme with the change in position from neutral to neck flexion which was neither noted nor commented on. Thus, results should be interpreted with a mean difference or a percentage change with change in position which can alter the clinical explanation of the results.[18]
Baska mask® resulted in significantly lower peak inspiratory pressure (P = 0.01) and higher expired tidal volume (P = 0.01) in flexion compared to I-gel™. I-gel™ resulted in a 52% increase in PIP as compared to 33.7% with Baska mask® and 45.2% decrease in ETV with I-gel™ compared to 30.6% decrease in ETV with Baska mask®. During neck flexion, there is a deterioration of alignment of the laryngeal and pharyngeal axis, restriction of the inlet of larynx and an increase in deviation of posterior epiglottis leading to an increase in PIP with a majority of SGAD including I-gel™. But the area of cross-section of ventilation holes is larger in Baska mask® (30 × 6 mm2 for size 4) as compared to I-gel™ (16 × 7 mm2 for size 4) hence providing an eminent buffer area leading to better preservation of ventilation and added advantage over I-gel™ during neck flexion to tide over limited laryngeal space [Figure 3].[17,19]
Figure 3.

Comparison of ventilation apertures of Baska mask® (30 × 6 mm2 for size 4) and I-Gel™ (16 × 7 mm2 for size 4)
In the present study time taken for device insertion was less in the I-gel™ group as compared to in Baska mask® group (P = 0.001). Similar results were contemplated by Kara D et al. and Chaudhary UK et al. in their study comparing Baska mask® and I-gel™ where the median time taken for device insertion in I-gel™ group was less compared to Baska mask® group (P < 0.05).[20,21] The reason for this is that I-gel™ is less bulky, easy to handle, bears high stability, and becomes immediately operational after insertion as having preformed non-inflatable cuff.
Device insertion was very easy in group G as compared to the group B but the result was not statistically significant (P = 0.203). Aziz Rara et al. and Henlin T et al. also contemplated similar results in their study using Baska mask® and I-gel™.[22,23] Postoperatively none of the subjects in both the groups complained of dysphagia or dysphonia. The limitation of our study was that the operator could not be blinded as all device insertions were performed by single experienced anaesthesiologist so our results may not apply to untrained personnel. Airway seal pressure is also affected by use of muscle relaxants, so our results may not be applicable to spontaneously ventilated patients.
CONCLUSION
We concluded that the higher OSP achieved with Baska mask® leads to an added advantage of lower PIP and higher ETV than I-gel™ in maximum flexion.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Weber U, Oguz R, Potura LA, Kimberger O, Kober A, Tschernko E. Comparison of the I-gel and the LMA-Unique laryngeal mask airway in patients with mild to moderate obesity during elective short-term surgery. Anaesthesia. 2011;66:481–7. doi: 10.1111/j.1365-2044.2011.06682.x. [DOI] [PubMed] [Google Scholar]
- 2.Alexiev V, Ochana A, Abdelrahman D, Coyne J, McDonnell JG, O'Toole DP, et al. Comparison of the Baska (®) mask with the single-use laryngeal mask airway in low-risk female patients undergoing ambulatory surgery. Anaesthesia. 2013;68:1026–32. doi: 10.1111/anae.12356. [DOI] [PubMed] [Google Scholar]
- 3.Foetdar S, Singh S, Tripathi RK. The Baska mask® trial in patients undergoing laparoscopic cholecystectomies. Int J Sci Res Pub. 2018;8:23–6. [Google Scholar]
- 4.Nishiyama T, Kohno Y, Kim HJ, Shin WJ, Yang HS. The effects of prewarming the I-gel on fitting to laryngeal structure. Am J Emerg Med. 2012;30:1756–9. doi: 10.1016/j.ajem.2012.02.009. [DOI] [PubMed] [Google Scholar]
- 5.Baskamask.com.au [homepage on the Internet] Sydney: BVLM Pty Ltd; [Last accessed on 2020 May 08]. Available from: http://www.baskamask.com.au/ [Google Scholar]
- 6.Using the i-gel® supraglottic airway. Intersurgical n.d. [Last accessed on 2020 May 08]. Available from: https://www.intersurgical.com/content/files/61747/-1200643841 .
- 7.Thakur DP, Malde AD. A study of effect of lateral position on oropharyngeal seal pressure of i-gel® and ProSeal™ LMA in children. Indian J Anaesth. 2020;64:125–30. doi: 10.4103/ija.IJA_635_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.El-Radaideh K, Amarin Z, Rashdan Y, Rabadi D, Khraise W, Omari M. The perilaryngeal airway and the laryngeal tube in short ophthalmic procedures in adults: A prospective randomized comparative study. J Anesth Clin Res. 2011;2:1–5. [Google Scholar]
- 9.Joshi R, Rudingwa P, Kundra P, Panneerselvam S, Mishra SK. Comparision of Ambu AuraGain™ and LMA® ProSeal in children under controlled ventilation. Indian J Anaesth. 2018;62:455–60. doi: 10.4103/ija.IJA_86_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sharma M, Sinha R, Trikha A, Ramachandran R, Chandralekha C. Comparison of effects of ProSeal LMA™ laryngeal mask airway cuff inflation with air, oxygen, air: Oxygen mixture and oxygen: Nitrous oxide mixture in adults: A randomised, double-blind study. Indian J Anaesth. 2016;60:566–72. doi: 10.4103/0019-5049.187787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Al-Rawahi SAS, Aziz H, Malik AM, Khan RM, Kaul N. A comparative analysis of the Baska mask® vs Proseal laryngeal mask for general anesthesia with IPPV. Anaesth Pain Intensive Care. 2013;17:233–6. [Google Scholar]
- 12.Jadhav PA, Dalvi NP, Tendolkar BA. I-gel versus laryngeal mask airway-Proseal: Comparison of two supraglottic airway devices in short surgical procedures. J Anaesthesiol Clin Pharmacol. 2015;31:221–5. doi: 10.4103/0970-9185.155153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.López AM, Muñoz-Rojas G, Fontanals M, de San José I, Hermoso A, Valero R. Clinical evaluation of the Baska mask® laryngeal mask in adult patients in ambulatory surgery. Rev Esp Anestesiol Reanim. 2015;62:551–6. doi: 10.1016/j.redar.2015.01.003. [DOI] [PubMed] [Google Scholar]
- 14.RTV silicone rubber. [Last accessed on 2020 May 08]. Available from: http://www.shinetsusilicone.global.com/catalog/pdf/rubber_e.pdf .
- 15.Alexiev V, Salim A, Kevin LG, Laffey JG. An observational study of the Baska® mask: A novel Supraglottic airway. Anaesthesia. 2012;67:640–5. doi: 10.1111/j.1365-2044.2012.07140.x. [DOI] [PubMed] [Google Scholar]
- 16.Jain D, Ghai B, Bala I, Gandhi K, Banerjee G. Evaluation of I-gel™ airway in different head and neck positions in anesthetized paralyzed children. Paediatr Anaesth. 2015;25:1248–53. doi: 10.1111/pan.12748. [DOI] [PubMed] [Google Scholar]
- 17.Kim HJ, Lee K, Bai S, Kim MH, Oh E, Yoo YC. Influence of head and neck position on ventilation using the air-Q® SP airway in anaesthetized paralysed patients: A prospective randomized crossover study. Br J Anaesth. 2017;118:452–7. doi: 10.1093/bja/aew448. [DOI] [PubMed] [Google Scholar]
- 18.Gupta S, Dogra N, Chauhan K. Comparison of I-gel™ and laryngeal mask airway supreme™ in different head and neck positions in spontaneously breathing pediatric population. Anesth Essays Res. 2017;11:647–50. doi: 10.4103/aer.AER_238_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sanuki T, Uda R, Sugioka S, Daigo E, Son H, Akatsuka M, et al. The influence of head and neck position on ventilation with the I-gel airway in paralysed, anaesthetised patients. Eur J Anaesthesiol. 2011;28:597–9. doi: 10.1097/EJA.0b013e32834698f4. [DOI] [PubMed] [Google Scholar]
- 20.Kara D, Sarikas CM. Comparison of the Baska and I-gel supraglottic airway devices: A randomized controlled study. Ann Saudi Med. 2019;39:302–8. doi: 10.5144/0256-4947.2019.302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chaudhary UK, Mahajan SR, Mahajan M, Sharma C, Sharma M. A comparative analysis of the Baska mask® versus I-gel for general anesthesia in surgical patients undergoing laparoscopic cholecystectomy. Acta Med Int. 2018;5:69–73. [Google Scholar]
- 22.Aziz RARA, Osman YM. Comparison of I-gel with Baska mask® airway for controlled ventilation in obese patients undergoing ambulatory surgery: A prospective randomized trial. J Anesth. 2017;5:29–35. [Google Scholar]
- 23.Henlin T, Sotak M, Kovaricek P, Tyll T, Balcarek L, Michalek P. Comparison of five 2nd generation Supraglottic airway devices for airway management performed by novice military operators. Biomed Res Int 2015. 2015:201898. doi: 10.1155/2015/201898. doi: 10.1155/2015/201898. [DOI] [PMC free article] [PubMed] [Google Scholar]


