Abstract
COVID-19 is a pandemic disease that recently been spreading all over the globe. Health-care bodies recognize that organized and written protocols are essential tools to help in fighting this highly contagious virus. In this review, we published our protocol and recommendations in the pediatric anesthesia department in our hospital in preparation for the management of children who are confirmed or suspected in perioperative periods.
Keywords: Airway, COVID-19, pediatric anesthesia, perioperative
Introduction
The World Health Organization has declared a global health emergency as the 2019-nCoV outbreak spreads across the world,[1,2,3,4] with confirmed patients in Saudi Arabia.[5]
While providing optimal treatment for those patients, careful execution of infection control measures is necessary to prevent nosocomial transmission to other patients and health-care workers providing care.[6,7,8]
The disease attacks the respiratory system and presents with flu-like symptoms, which may progress to a severe form of pneumonia and acute respiratory distress syndrome or even death.[9] The severity of the disease is reported to be mild in the pediatric age group, but transmission from this population was reported.[10,11]
Pediatric anesthesiologists are health-care workers (HCWs) who are involved in the care of pediatric patients in perioperative settings and situations of difficult airway management. They are expected to handle these cases most effectively and safely.[12,13,14,15]
Clinical recommendations and action plans are advised to maximize patients' and health-care workers' safety.[16,17]
In response to this crisis we are in the Department of Pediatric Anesthesia in King Abdullah Specialized Children Hospital (KASCH), Riyadh, Saudi Arabia organized a rapid task force to review the latest recommendations regarding caring of confirmed or suspected of COVID-19 in pediatrics in the perioperative period.
Our aim in this document is to review the most recent recommendations for the pediatric anesthesia and operating room in preparation for anticipated perioperative care of acute respiratory illness (ARI), such as COVID-19, confirmed or suspected, pediatrics patients in a pandemic or crisis and afterward.
Our Objectives include:
Develop a strategy to manage space, staff, and supplies in the pediatric operating room in order to provide optimum care to patients with ARI in preparation for a pandemic
Facilitate care of patients with known or suspected respiratory pathogens (such as SARS-CoV2) who need surgery
Implement infection prevention measures to reduce the risk of viral transmission to other patients or health-care workers in the operating room
Optimize the quality of care provided for patients with ARI such as COVID-19.
Materials and Methodology
Using a combination of relevant terms, we electronically search these electronic databases (PubMed Central®, Google scholar®) for published and ahead of print articles. We also search PROSPERO and ClinicalTrial.gov for planned studies and published protocols.
All citation was retrieved to reference manager (Mendeley Desktop v1.19.5). Relevant articles and citation titles and abstract was screened and included in the manuscript of this review. The manuscript was prepared by two reviewers (T.J and NZ) and reviewed and modified by the other two reviewers (A.H and A.A). Any disagreement was resolved by discussion and voting.
Infection Prevention Strategies
Engineering aspects
Ideally, a negative pressure room is necessary however, the standard Operating room (OR) in our hospital are designed to be at positive pressure. As compensation, the frequency of air changing is increased more than 20 per hour in order to reduce viral load rapidly[18,19]
Operating room has a ventilation system with an integrated high-efficiency particulate air (HEPA) filter; however, a portable HEPA filter [Figure 1] should be used during intubation and extubation only. However, it must be It must be turned off during surgery.
Figure 1.

Portable HEPA filter
Management Strategies
Administrative aspects
It is the responsibility of the surgeon and the primary nurse to inform OR nurse and infection control practitioner (ICP) regarding COVID-19 confirmed or suspected patients coming for urgent surgery
Operating room nurse must immediately inform OR staff about the case in order to prepare and double-check with ICP
Precautions should be taken while transferring the patient to OR
One operating room should be dedicated to COVID-19 suspected and confirmed cases requiring surgery. In the unlikely event that a second COVID-19 patient needs emergency surgery (e.g., E1 case), a second OR in the same area or complex will be utilized, both rooms should be far from the other rooms where regular cases should be done
The patient should enter and exit OR through specified entrance, bypassing OR holding. This path should be labeled by proper signage to prevent further contamination
Airborne precautions should be observed and practiced throughout the patient's perioperative journey. An airborne isolation sign will be placed outside the OR door.
Personal Protective Equipments (PPE)
A comprehensive program for the use of PPE should be enforced. Health-care personnel is medically cleared and trained to use PPE
All staff is fitted with the N95 masks. Staff who does not pass the N95 fitting test will use powered air-purifying respirator (PAPR)
Refresher training for the use and maintenance of the PAPR should be conducted.[20]
Simulation Drills
Drills are essential for testing the preparedness of our isolation OR and procedures[21,22]
Drills should take place in the actual OR to improve safety in high-risk stressful situations[21,22,23]
Drills should show how to improve teamwork, patient safety, and behavior through conducting a series of simulations of various scenarios[24]
The final scenario should involve a crisis that requires the participants to perform resuscitation while wearing PPEs and PAPRs.
Hospital Strategies
Optimizing bed capacity
Management of Patients, Families, and Staff
Patients and their families are screened through a questionnaire. Patients who fulfill the criteria for suspected respiratory pathogens, such as COVID-19 infection are isolated, referred to infectious disease, and tested for the virus
Elective surgery should be postponed if the patient has traveled to affected areas, national or international. The number of accompanying family members should restricted to one[6]
Staff caring for patients suspected of respiratory pathogens such as COVID-19 and those who care for other patients are separated to reduce the risk of in-hospital transmission
Staff caring for COVID-19 patients will continue with their usual clinical work while wearing surgical masks and will monitor themselves for fever and respiratory symptoms
In case of inadequate PPE at the time of close contact, the staff member will be relieved from duty, whereas the infectious diseases team assesses the risk of transmission and plans subsequent management. Staff members who develop fever or respiratory symptoms will be screened at employee flu clinic.
Communications and Staff Support
Communication channels, including a website, should be established, and daily email updates, should be maintained to all staff
Resources, including reading material and a helpline, should be provided by institution to help staff cope with related anxiety and burnout.[25]
Pediatric Anesthesia Departmental Strategies
Operating room
General principles
The priority is patient safety and infection prevention to HCW's
The Hospital infection control and prevention updates should be strictly followed, applied and continuously monitored
Staff involved with a COVID-19 case should be N95 fit-tested and wear the N95 masks or PAPR and appropriate PPE throughout the procedure, and No screening for COVID-19 will be done in OR
Avoid Using Air forcing warming device to prevent Hypothermia instead of that apply other measures including warming OR, fluid mattress, fluid warmer etc
The “High Quality” Viral filter should be installed between the breathing circuit and the patient's airway with the capability to sample gas from the machine side of the filter
HME is preferred to preserve humidification, however If the filter only is used, reducing fresh gas flow is an essential strategy for preserving humidity (1-2 L/min or less), and place a second filter [Figure 2] at the end of the expiratory limb at the connection to the anesthesia machine
Local conditions of filter availability will determine what devices can be employed, alternatives are described below, and breathing circuits should be discarded after every patient[17]
Anesthesia Consultant should lead all Anesthesia procedures in OR, early communication between HCWs involved in confirmed or suspected COVID-19 cases is strongly advised, and the case definition will follow infectious diseases division and infection control department
No parents are allowed inside the OR, and consent for anesthesia is to be taken during pre-anesthesia assessment in the patient's admission location
Traffic and flow of contaminated air are minimized by locking all doors to the OR during surgery, with only one possible route for entry and exit
A station with PPE supplies, including N95 masks, should be available outside the dedicated COVID-19 OR; prepared for donning and doffing of PPE, and Airborne Isolation sign should be placed outside the OR door, and steps of donning and doffing PPE are numbered in sequence, and posters are put up to guide staff
Only essential equipment should be kept in the room, frequently touched equipment such as anesthesia machines, ultrasound machines, laptops, and workstations should be wrapped and covered with transparent plastic [Figure 3]. Disposable equipment should be used as much as possible[26,27]
Mobile airway trolley, drugs (induction, emergency), and airway equipment should be well prepared and on standby for usage to minimize the induction time, with signage labeled inside the OR
Minimize the numbers of unnecessary personal in the OR: three nurses in the OR (one scrub nurse, one circulating, and one for documentation), two anesthesia team members (consultant, assistant consultant if needed, and technologist), and to eliminate the need of the staff inside the OR to leave; one nurse stays outside the frontal door together with an anesthesia technician to support the team inside[18]
Aerosol generating procedures is reported as a risk factor to increase transmission of respiratory infection to HCWs. Procedures with a high risk of aerosolization from highest to lowest include: tracheal intubation, tracheostomy, suction prior intubation, invasive ventilation, manual ventilation prior intubation, chest compression/defibrillator and bronchoscopy.[6,28]
Figure 2.
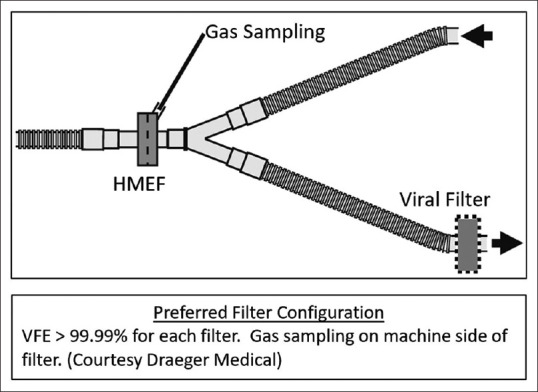
Preferred filter configuration
Figure 3.

Anesthesia machine wrapped and covered with transparent plastic
Operating room setup
Medications [Table 1] will be put in a plastic box prepared before OR. If more medications required, then the anesthesia technician outside the room will provide it to the team keeping the treating team inside OR
Automated dispensing cabinet Omnicell™ will be relocated outside the OR to minimize contamination as it needs fingerprint. It will be placed near the rear door, and an anesthesia technician/technologist will be responsible for it
Endorsement, team briefing, and timeout will be conducted inside the OR with anesthesiologists, nurses, and one member of the surgical team scrubbed and present. A safe distance from the patient should be maintained all time.
Table 1.
Medication in the plastic box
| Agent | Qauntity |
|---|---|
| Induction agent | One ampoule of propofol. |
| Muscle relaxant | One ampoule of succinylcholine/one ampoule of rocuronium |
| Anticholinergic | One ampoule of atropine/two ampoules of glycopyrrolate |
| Anti-emetic | One ampoule of dexamethasone/one ampoule of metoclopramide/one ampoule of granisterone |
| Analgesic | One vial of perfalgan (IV acetaminophen) |
| Opioids | Opioids need to be withdrawn in syringes to the desired dilution, and empty vials will be returned to the Omnicell™ as per policy |
Staff Management
Staff separation and segregation
Staff is segregated into those caring for infected patients and those caring for other patients to reduce the possibility of in-hospital transmission; three consultants will be dedicated to COVID-19 patients for two weeks, in the case of E1 COVID-19, the on-call consultant will handle the case, and then he/she will be substituting one of the three consultants dedicated to COVID-19 patients
Large group meetings are suspended to reduce potential cross-infection among health-care personnel, and web-based conferencing is used to enable communication.
Exposure and spread minimization
Routine postoperative visits are suspended and replaced by phone calls, virtual clinic where applicable to reduce staff traffic around the hospital, and non-urgent preoperative assessment visits are postponed
Pregnant and immunocompromised staff will not care for patients with an ARI such as COVID-19.
Pediatric Anesthesia and Airway Management
Pre-anesthesia assessment clinic (PAC)
During a pandemic or crisis, there will be no clinics, and assessment will be conducted in the patient's admission location. The virtual clinic will be activated and the assessment will be performed via phone for some patients. Recommended PPE for HCWs in the PAC includes white medical gowns, medical gloves, eye protection shields, disposable surgical caps, and surgical masks or test fit N95 masks[29]
Patients receiving preoperative evaluation should enter the consultation room one by one to minimize close contact with the clinician and other individuals
The patient's body temperature should be measured (electronic thermometer) before entering the consultation room. If the body temperature is higher than 37.3°C, then he or she must be immediately escorted to the flu clinic and should be reported to infection control
Anesthesiologists should take a detailed history and conduct a thorough physical examination, particularly a careful chest examination, and hand hygiene must be performed following contact with each patient
Suspected cases of infection with 2019-nCoV, even with average body temperature, should be reported to Infection Control immediately
At the end of each shift, cleaning and disinfection procedures should be performed in the PAC as appropriate for 2019-nCoV.[29]
Anesthesia induction
The time between induction and securing the airway with endotracheal tubes (ETTs) should be minimal to reduce the risk of virus shedding [Figure 4]
A portable HEPA filter should be used during intubation and extubation only and turned off during surgery[26]
The number of people inside the OR should be kept at a minimum; three nurses (one scrub nurse, one circulating and one for documentation), two surgeons (consultant, assistant consultant if needed), and two anesthesia team members (consultant, assistant consultant if needed and technologist)
Surgeons, circulating nurse, and nursing for documentation should stay as far as possible from the patient during airway manipulation[18]
Pre-oxygenation should be performed using a tight face mask, whereas the patient is covered with a transparent plastic bag to minimize the spread of airway secretions to the air[30]
Unnecessary high flow or closure of the APL valve should be avoided
Sedation is to be utilized whenever possible and safe especially in uncooperative or combative children
IV induction with rapid sequence technique is to be performed[30]
Positive pressure ventilation is to be avoided and otherwise is necessary, ensure a tight mask seal and use two hand technique or small frequent tidal volume[30]
The use of ETT with micro-cuffs is highly recommended. Video-assisted laryngoscopy is recommended over direct laryngoscopy in order to keep the operator as far as possible from the patient's airway.[16] Airway manipulation should be attempted after assuring the patient is completely paralyzed to avoid coughing.
Closed inline suction [Figure 5] should be connected whenever possible[26]
Proper ETT location is to be confirmed by observing the dark line in the ETT through Glidescope, bilateral chest rising, and ET CO2, and a disposable stethoscope is to be used to auscultate the chest for other reasons.
Figure 4.

Intubation using PPE in a simulation drill
Figure 5.

Closed inline suction
Difficult Airway Management Outside OR
Pediatric anesthesiologists are often called for difficult airway management in either the emergency department (ER) or pediatric intensive care unit (PICU)
Majority of difficult airway cases can be managed with same equipment in OR (for example: Glidescope or laryngoscope)
In rare scenario, oral fiberoptic intubation is required and often used in children after deep anesthesia with maintenance of spontaneous ventilation and vocal cord topicalization with lidocaine through the pharyngeal cavity, oral cavity, and airway catheter surface
Depth of anesthesia should be insured to decrease the chance of child coughing during airway topicalization
This situation is similar to that for the care of an ordinary patient, however, the preparation should be more robust as help is limited, equipping personal protective equipment is time-consuming, besides, obtaining a clear view of the glottis is extremely challenging due to vapor condensation on the eye shield or goggles[29]
These units should plan and follow infection prevention and control recommendations, and intubation should be done in a negative pressure room if available.
Anesthesia Emergence
The extubation should be performed while the HEPA filter is ON[26]
The muscle relaxant reversal should be given, anti-emetic should be considered to reduce vomiting and forceful retching, and deep extubation should be considered as a first option whenever possible
Surgeons and other nurses should be as far as possible, recovery will be in OR by a single PACU nurse with similar PPE precautions, if help is needed, the nurse will ask the assigned anesthesiologist, and if kept intubated, transfer directly to PICU
The assigned anesthesiologist should determine the proper time for discharge from OR.
Remote Area (Interventional Radiology MRI/CT Scan)
Despite the elective nature of these interventions, children with COVID-19 might come in a situation of difficult IV access or need long term access, urgent CT scan, imaging or other interventional radiology procedures for other urgent reasons is expected to require Pediatric Anesthesia Care
These allocations carry inherited risk of the remote area, including unfamiliar environment, personnel, and lack of help during a crisis
When a patient with suspected COVID-19 is imaged, during scanning of the patient with suspected airborne or droplet precautions, up to three staff members may be occupied with scanning the patient. Appropriate cleaning and disinfection must be enforced between patients, according to ICP, the scanner may be unusable for up to 90 minutes to perform terminal cleaning
CT should not be used to screen as the first-line test to diagnose COVID 19, for patients with known COVID-19 requiring imaging for other indications; the reason for the study should be discussed with the radiologist on service. If the clinical question can be answered by utilizing a portable modality (portable X-ray, portable ultrasound), then these should be used instead of computed tomography (CT) or magnetic resonance imaging (MRI)
Patients will be scheduled towards the end of the workday or off-peak hours to reduce the chances of infecting other patients
If a patient needs anesthesia support and intubation, then it will be performed in designated OR rooms, with all precautions, prior transportation to MRI/CT, and upon completion of imaging, the patient will be taken back to same designated OR rooms for extubation with airborne precautions. Disinfection of designated OR room should be performed following the extubation
For interventional radiology procedures requiring anesthesia support, it will be performed in the designated OR rooms if agreed by radiologist. Otherwise, it will be done in angiography- suite with all precautions of airborne isolation and disinfection.
Transport Measures
During the transfer, the circulating nurse and anesthesiologist should wear proper PPE outside OR, the patient should be covered with one disposable operating sheet and then transferred to the negative-pressure or isolation ward through a dedicated lobby and elevator
The patient must wear a surgical mask during transfer. The surfaces of passageways and the elevator should be cleaned and covered.[30] If the patient is kept intubated, then a single-patient-use Ambu bag must be used during the transfer. It is not recommended to use a ventilator during transfer.[29]
Post-operative Strategies
Equipment care and operating room disinfection
Equipment, supplies, and medications must be used for one patient only
Anesthesia supplies that directly contact the patient’s skin or mucosa should be single-use as possible
All anesthesia equipment should be cleaned and disinfected, according to hospital infection control protocol
The carbon dioxide absorber is recommended to be replaced between cases as it provides a large surface area in the anesthesia machine. The breathing circuit within the anesthesia machine should be disinfected between cases and at the end of the shift. The surface of the anesthesia machine, laryngoscope handles, and other non-disposable equipment should be cleaned and disinfected after the completion of each case and again at the end of the shift, according to infection control protocol[29]
Contamination should be wiped off with a damp disposable cloth. When using alcohol, a solution diluted to 40% should be used
The disinfectant should not be directly sprayed on the touch screen. The cleaning agent must first be transferred to a cloth or towel
Patient cables and blood pressure cuff can be disinfected with a cloth soaked in diluted alcohol or aldehyde-based disinfectant then dried thoroughly with a lint-free cloth.
Anesthesia machine and ventilator must be sent to central sterile services department (CSSD) for thermal disinfection
The breathing circuit is for single use. An appropriate filter should be placed between the patient and the breathing circuit. A new filter should be utilized for each patient
Sampling lines for sidestream gas analysis, carbon dioxide absorber, and water trap must be replaced
The anesthesia cart and other anesthesia facilities must be cleaned and disinfected according to infection control protocol. The infection control team of the operating room should keep a checklist and track the cleaning and disinfection of equipment and facilities in a timely fashion
The operating room used for patients with ARI or confirmed or suspected COVID-19 pneumonia should be thoroughly disinfected. The cleaning personnel should complete sufficient training on cleaning, disinfection, and self-protection before working in the dedicated operating room
The transfer bed used for patients with COVID-19 should be cleaned and disinfected according to infection control protocol.[29]
Disposal of Medical Waste
Medical waste should be disposed of immediately. All the medical waste should be double-bagged and labeled along with the name of the department, date and time, and the category
Before being taken out of the contaminated area, all the packing bags should be sealed and sprayed with a disinfectant or covered with an additional bag and sealed according to infection control protocol. Medical waste produced in the clean area can be treated routinely[29]
All health-care workers participating in the surgery should remove their PPE and place the PPE in a designated waste bag. PPEs should be removed in the following order: shoe covers → gloves → hand hygiene → goggles/face shield → hand hygiene → the gown → hand hygiene → the protective mask → hand hygiene → the headcover → hand hygiene → shower and change into personal clothing.[29]
Management of Health-care worker after Caring for Infected/Suspected Patients
In case of any staff has an unprotected exposure to a confirmed or suspected case while not wearing proper PPE or used PPE improperly, he must inform the Infection control department, stop performing duties, visit the flu clinic and do testing for COVID 19 preferably after more than 24 hours of exposure, stay in home isolation and he will not resume his duties until he is cleared
If he is COVID19 positive and does not need admission, then he will stay in home isolation until cleared, if he is COVID19 negative, he will stay in home isolation 14 days and he will not resume his duties until he is cleared
Clearance criteria include all the following: no symptoms for 48 hours, the 14 days postexposure observation period is over, and he had at least one negative PCR for COVID-19
If our staff has a protected exposure to a confirmed case while wearing proper PPE, and he is not symptomatic, he will continue duties, testing COVID-19 is not recommended, but he will be assessed daily for 14 days post exposure for development of symptoms
If he was symptomatic, then he must inform the Infection control department, stop performing duties, visit the flu clinic and do testing for COVID 19 preferably after more than 24 hours of exposure, stay in home isolation, and he will not resume his duties until he is cleared
If he is COVID19 positive and does not need admission, then he will stay in home isolation until cleared. If he is COVID19 negative, then he will stay in home isolation until resolution of symptoms and he will not resume his duties until he is cleared. All clearance criteria must be met.[30]
In conclusion, COVID-19 is evolving acute viral respiratory disease with a lot of knowledge and lessons need to be learn. We present here a summary of recommendations adapted in our tertiary institution. We believe this guidance might help in other similar population and work condition.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Coronavirus Disease 2019 (COVID-19) [Internet]. CDC. Available from: https://wwwcdcgov/coron avirus/2019-ncov/indexhtml . Last cited on 2020 Mar 30.
- 2.Q&A on coronaviruses (COVID-19) [Internet]. WHO. Available from: https://wwwwhoint/news-roo m/q-a-detail/q-a-coronaviruses . Last cited on 2020 Mar 30.
- 3.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chen ZM, Fu JF, Shu Q, Chen YH, Hua CZ, Li FB, et al. Diagnosis and treatment recommendations for pediatric respiratory infection caused by the 2019 novel coronavirus. World J Pediatr. 2020 doi: 10.1007/s12519-020-00345-5. doi: 101007/s12519-020-00345-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.MOH Command and Control Center COVID-19 Virus [Internet]. MOH. Available from: https://wwwmohgovsa/e n/CCC/Pages/defaultaspx . Last cited on 2020 Mar 30.
- 6.Infection Prevention and Control of Epidemic-and Pandemic-Prone Acute Respiratory Infections in Health Care WHO Guidelines[Internet]. WHO. Available from: https://appswhoint/iris/bitstream/ha ndle/10665/112656/9789241507134_en gpdfsequence=1 . Last cited on cited 2020 Mar 30. [PubMed]
- 7.Chee VW Ter, Khoo ML, Lee SF, Lai YC, Chin NM. Infection control measures for operative procedures in severe acute respiratory syndrome–related patients. Anesthesiol J Am Soc Anesthesiol. 2004;100:1394–8. doi: 10.1097/00000542-200406000-00010. [DOI] [PubMed] [Google Scholar]
- 8.Park J, Yoo SY, Ko JH, Lee SM, Chung YJ, Lee JH, et al. Infection prevention measures for surgical procedures during a middle east respiratory syndrome outbreak in a tertiary care hospital in South Korea. Sci Rep. 2020;10:325. doi: 10.1038/s41598-019-57216-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sun P, Lu X, Xu C, Sun W, Pan B. Understanding of COVID-19 based on current evidence. J Med Virol. 2020 doi: 10.1002/jmv.25722. doi: 101002/jmv 25722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cao Q, Chen YC, Chen CL, Chiu CH. SARS-CoV-2 infection in children: Transmission dynamics and clinical characteristics. J Formos Med Assoc. 2020;119:670–3. doi: 10.1016/j.jfma.2020.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lu Q, Shi Y. Coronavirus disease (COVID-19) and neonate: What neonatologist need to know. J Med Virol. 2020 doi: 10.1002/jmv.25740. doi: 101002/jmv25740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Peng PWH, Wong DT, Bevan D, Gardam M. Infection control and anesthesia: Lessons learned from the Toronto SARS outbreak. Can J Anesth. 2003;50:989–97. doi: 10.1007/BF03018361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Scales DC, Green K, Chan AK, Poutanen SM, Foster D, Nowak K, et al. Illness in intensive care staff after brief exposure to severe acute respiratory syndrome. Emerg Infect Dis. 2003;9:1205–10. doi: 10.3201/eid0910.030525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Loeb M, McGeer A, Henry B, Ofner M, Rose D, Hlywka T, et al. SARS among critical care nurses, Toronto. Emerg Infect Dis. 2004;10:251–5. doi: 10.3201/eid1002.030838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rothe C, Schunk M, Sothmann P, Ofner M, Rose D, Hlywka T, et al. Transmission of 2019-NCOV infection from an asymptomatic contact in Germany. N Engl J Med. 2020;382:970–1. doi: 10.1056/NEJMc2001468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wax RS, Christian MD. Practical recommendations for critical care and anesthesiology teams caring for novel coronavirus (2019-nCoV) patients TT-Directives concrètes à l'intention des équipes de soins intensifs et d'anesthésiologie prenant soin de patients atteints du coronav. Can J Anaesth. 2020;67:568–76. doi: 10.1007/s12630-020-01591-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Perioperative Considerations for the 2019 Novel Coronavirus (COVID-19) [Internet] Anesthesia Patient Safety Foundation. Available from: https://wwwapsforg/news-updates/periope rative-considerations-for-the-2019-no vel-coronavirus-covid-19/ Last cited on 2020 Mar 30.
- 18.How Coronavirus Spreads [Internet]. CDC. Available from: https://wwwcdcgov/corona virus/2019-ncov/prevent-getting- sick/how-co vid-spreadshtmlCDC_AA_ref Val=https%3A%2F%2Fwwwcdcgov%2Fcoro navirus%2F2019-ncov%2Fprepare%2Ftran smissionhtml . Last cited on 2020 Jan 04.
- 19.Ti LK, Ang LS, Foong TW, Ng BSW. What we do when a COVID-19 patient needs an operation: Operating room preparation and guidance. Can J Anaesth. 2020 doi: 10.1007/s12630-020-01617-4. doi: 101007/s12630-020-01617-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wong J, Goh QY, Tan Z, Lie SA, Tay YC, Ng SY, et al. Preparing for a COVID-19 pandemic: A review of operating room outbreak response measures in a large tertiary hospital in Singapore Se préparer pour la pandémie de COVID-19: Revue des moyens déployés dans un bloc opératoire d'un grand hôpital tertiaire au. S Can J Anesth Can d'anesthésie. 2020 doi: 10.1007/s12630-020-01620-9. doi: 101007/s12630-020-01620-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kurup V, Matei V, Ray J. Role of in-situ simulation for training in healthcare: Opportunities and challenges. Curr Opin Anaesthesiol. 2017;30:755–60. doi: 10.1097/ACO.0000000000000514. [DOI] [PubMed] [Google Scholar]
- 22.Patterson MD, Geis GL, Falcone RA, LeMaster T, Wears RL. In situ simulation: Detection of safety threats and teamwork training in a high risk emergency department. BMJ Qual Saf. 2013;22:468–77. doi: 10.1136/bmjqs-2012-000942. [DOI] [PubMed] [Google Scholar]
- 23.Mastoras G, Poulin C, Norman L, Weitzman B, Pozgay A, Frank JR, et al. Stress testing the resuscitation room: Latent threats to patient safety identified during interprofessional in situ simulation in a Canadian academic emergency department. AEM Educ Train. 2019 doi: 10.1002/aet2.10422. doi: 101002/aet210422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fent G, Blythe J, Farooq O, Purva M. In situ simulation as a tool for patient safety: A systematic review identifying how it is used and its effectiveness. BMJ Simul Technol Enhanc Learn. 2015 doi: 10.1136/bmjstel-2015-000065. doi: 101136/bmjstel-2015-000065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wong JEL, Leo YS, Tan CC. COVID-19 in Singapore-current experience: Critical global issues that require attention and action. JAMA - J Am Med Assoc. 2020 doi: 10.1001/jama.2020.2467. doi: 101001/jama20202467. [DOI] [PubMed] [Google Scholar]
- 26.Tompkins, Bonnie M, Kerchberger, John P. Personal Protective Equipment for Care of Pandemic Influenza Patients: A Training Workshop for the Powered Air Purifying Respirator. Anesth Analg. 2010;111:933–45. doi: 10.1213/ANE.0b013e3181e780f8. [DOI] [PubMed] [Google Scholar]
- 27.Tan TK. How severe acute respiratory syndrome (SARS) affected the Department of Anaesthesia at Singapore General Hospital. Anaesth Intensive Care. 2004;32:394–400. doi: 10.1177/0310057X0403200316. [DOI] [PubMed] [Google Scholar]
- 28.Tran K, Cimon K, Severn M, Pessoa-Silva CL, Conly J. Generating procedures and risk of transmission of acute respiratory infections to healthcare workers: A systematic review. PLoS One. 2012;7:e35797. doi: 10.1371/journal.pone.0035797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chen X, Liu Y, Gong Y, Guo X, Zuo M, Li J, et al. Perioperative management of patients infected with the novel coronavirus: Recommendation from the Joint Task Force of the Chinese Society of Anesthesiology and the Chinese Association of Anesthesiologists. Anesthesiol J Am Soc Anesthesiol. 2020 doi: 10.1097/ALN.0000000000003301. doi: 101097/ALN0000000000003301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kamming D, Gardam M, Chung FI. Anaesthesia and SARS. Br J Anaesth. 2003;90:715–8. doi: 10.1093/bja/aeg173. [DOI] [PMC free article] [PubMed] [Google Scholar]


