Abstract
Background:
Pain management remains an integral part of patient care after cardiac surgery, and it required proper pain assessment. The aim of the study was to assess pain perception using validated Arabic version of the short-form McGill Pain Questionnaire (SF-MPQ) and to identify analgesics prescribing patterns post cardiac surgery.
Methods:
This is a prospective study conducted in an adult cardiac critical care unit of a tertiary cardiac center from September 2018 to March 2019. The study enrolled 74 patients who underwent cardiac surgical procedures through a median sternotomy.
Results:
The mean age of our patients was 57 ± 11 years and 47 (63.5%) were males. Patients described post-cardiac surgery pain as heavy (n = 37; 50%) and tiring-exhausting (n = 49; 66%), mainly at the site of incision (n = 20; 27%). Pain intensity at day 1 according to pain rating index (PRI) and numerical rating scale (NRS) was 7 (25th, 75th percentiles: 2.8–15) and 6 (3–8), respectively. There was a significant change in pain intensity score between 2 days of assessment (PRI: 7 [2.8–15] vs 5 [2–11] P = 0.010; NRS: 6 (3–8) vs 5 (2–8), P = 0.021]). The most common analgesics prescribed were paracetamol (39%) and a combination of tramadol and paracetamol (33.8%).
Conclusion:
Pain decreased the second day after cardiac surgery compared to day 1. Paracetamol was the most prescribed analgesic; however, there was an underutilization which might be affected by insufficient pain reporting. Future improvement could focus on multimodal pain management and proper communication of pain experience.
Keywords: McGill pain questionnaire, pain assessment, post-sternotomy pain
Introduction
Pain management remains a challenging issue after cardiac surgery despite the continuous improvement of the surgical technique. Pain level is a subjective symptom that can differ significantly based on individual factors.[1] Several measuring scales were used to assess pain severity, and many barriers stand before optimal pain assessment and management.[2] According to the US Institute of Medicine, 80% of surgical patients experience acute postoperative pain; however, adequate pain control was not reported in most patients.[3]
The perception of pain is influenced by several factors, which are related to surgical trauma and patients' related factors, including psychological and ethnic elements.[4] A variety of instruments are available to evaluate pain, such as the McGill Pain Questionnaire (MPQ).[5] The MPQ provides information about pain perception, patients' reaction, and cognition, these elements are essential when deciding about the treatment strategy and evaluating its effect.[6]
Proper pain control is vital after cardiac surgery to improve the patients' experience and surgical outcome. This study aimed to evaluate pain perception using a validated Arabic version of the short-form McGill Pain Questionnaire (SF-MPQ) and to identify analgesics prescribing patterns post-cardiac surgery in a tertiary referral center.
Methods
Setting and sample
The study was conducted in the adult cardiac surgery critical care unit in a tertiary referral center. Ethics approval was granted by the hospital's research ethics committee (Reference number: R18012). A total of 74 patients were recruited over an 8-month period starting from September 2018 to March 2019. Patients who were admitted to the critical care unit following any cardiac surgery through sternotomy were included in the study. Patients who had a history of chronic pain (back pain, cancer, arthritis), or opioid use, neurological disease, psychiatric illness, alcohol, narcotics, or medication abuse were excluded.
The mean age was 57 ± 11 years and 47 patients (63.5%) were males. Thirty-seven patients (50%) underwent valvular surgery, 24 (32%) had coronary artery bypass surgery (CABG), and 9 patients (12%) had combined procedures or other cardiac surgery [Table 1].
Table 1.
Patients’ characteristics
| Variable (n=74) | Frequency (%)/mean±SD |
|---|---|
| Age (years) | 57±11 |
| Male | 47 (63.5) |
| Weight (kg) | 76±12.9 |
| Height (meter) | 1.6±0.1 |
| Body mass index (Kg/m2) | 35.5±11.6 |
| Previous cardiac surgery | 19 (25.7) |
| Heart failure | 7 (9.5) |
| Ischemic heart disease | 31 (41.9) |
| Rheumatic heart disease | 9 (12) |
| Atrial Fibrillation | 8 (10.8) |
| Hypertension | 41 (55) |
| Diabetes mellitus | 26 (35) |
| Insulin-dependent diabetes | 16 (21.6) |
| Dyslipidemia | 27 (36.5) |
| Hemoglobin (mg/dL) | 12.7±3 |
| Bilirubin (µmol/L) | 8±6 |
| Creatinine (µmol/L) | 106.6±150.8 |
| Renal impairment | |
| Moderate (CrCl >50 and <85) | 29 (39.2) |
| Severe (CrCl <50) | 8 (10.8) |
| Smoker | 8 (10.8) |
| Ex-smoker | 9 (12) |
| Surgery | |
| CABG | 24 (32.4) |
| Valves only | 37 (50) |
| CABG + valves | 9 (12) |
| Others* | 4 (5) |
Continuous variables are presented as mean and standard deviation and categorical variables as number and percent CABG: Coronary artery bypass graft; CrCl: Creatinine clearance. *Others=Pericardiectomy, repair of aortic dissection, heart transplant
Data collection
Two data collection tools were used: “A patient profile form,” which was designed for this study and was used to document the demographics, history [Table 2], and the dose and type of analgesics prescribed and administered. The second tool was “a patient interview form, which consisted of three interview tools: a validated Arabic version of the SF-MPQ, present pain intensity (PPI) index, and numerical rating scale (NRS). The information was retrieved from the patients' electronic medical records, Clinical Information System (ICIP) provided by Philips Medical System, Doctors' Portal (DORTAL), and case notes.
Table 2.
Pre-procedure medications
| Variable (n=74) | Frequency (%) |
|---|---|
| Beta-blockers | 54 (73) |
| Angiotensin receptor blockers | 10 (13.5) |
| Calcium channel blockers | 12 (16) |
| Angiotensin-converting enzyme inhibitors | 20 (27) |
| Thiazide diuretics | 3 (4) |
| Loop diuretics | 36 (48.6) |
| Digitalis | 2 (2.7) |
| Antiplatelet | 53 (71.6) |
| Anticoagulants | 16 (21.6) |
| Statins | 36 (48.6) |
Data are presented as number and percent
The SF-MPQ is a 15-item checklist assessing the sensory and affective dimensions of the pain experience. The 15 items are rated on a four-point pain intensity scale: 0 = none, 1 = mild, 2 = moderate, and 3 = sever.[5]
The sum of the intensity values for the corresponding descriptors yields the sensory (11 items), affective (4 items), and total (15 items) pain score. All 15 descriptors make a total score, ranging (0–45), which is defined as the pain rating index (PRI). A higher SF-MPQ score indicates worse pain.[6]
Patients were asked to rate the level of their pain on the PPI index: 1 = no pain, 2 = mild, 3 = discomfort, 4 = distressing, 5 = horrible, and 6 = excruciating. Patients also described whether their pain was brief, intermittent, or continuous. The SF-MPQ includes a numerical rating scale (NRS) from (0–10).
The participants were interviewed during the postoperative period from 24 to 48 h after extubation. The interview took approximately 5 min to complete and was conducted by a trained investigator. In addition, a follow-up phone call has been conducted after discharge, up to 3 months to assess the pain level and pain medication adequacy. The survey included NRS at the present time, first time experiencing pain post-discharge and after taking pain medication, if any.
Arabic version SF-MPQ validation
A previously validated Arabic version of SF-MPQ was used to assess pain perception in our patients. Findings indicate that the translated version of the SF-MPQ is reliable and valid for use in Arabic-speaking patients.[7]
Statistical analysis
Descriptive statistics were used to summarize surgical patients' baseline characteristics, medication history, and pain scores. Categorical variables were reported as percentages and frequencies, while continuous variables were reported as mean ± standard deviation if normally distributed; median with the interquartile range (25th and 75th percentile) if non-normally distributed. Shapiro-Wilk test was used to determine the normality of distribution. The medians of pain intensity in paired samples were compared using related samples Wilcoxon signed-rank test. Subgroup analysis of independent samples (according to gender) was done using the Mann-Whitney U Test in analyzing non-normally distributed data. The Chi-square or Fisher exact tests were used to assess the relationship between two categorical data. A statistical significance was accepted at the level of a P value of less than 0.05. All statistical analysis was done using IBM-SPSS version 25 (IBM Corp, Chicago, IL, USA).
Results
The sensory and affective subscale of pain perception
The SF-MPQ measures the PRI in two subscales: sensory subscale and affective subscale. Patients' responses for each subscales' descriptors are summarized in Table 3. Forty-eight hours post-cardiac surgery, 50% of the patients described pain perception as in the sensory subscale as heavy, and 35% as stabbing. While tiring-exhausting was the most frequently chosen descriptor of pain sensation in the affective subscale according to 66% of the patients. Further analysis revealed that there were no statistical differences in both males and females pain perception according to the sensory subscale; stabbing (males = 8 [29.6%] vs females = 18 [38%], P = 0.452]; heavy (males = 14 [51.9%] vs females = 23 [48.9%], P = 0.809] same as in the affective subscale; tiring-exhausting (male = 18 [66.7%] vs females = 31 [66%], P = 0.950).
Table 3.
Descriptors of the patient’s pain experience on the sensory and affective subscales of pain sensation
| Descriptors of pain | Severe | Moderate | Mild | Total- experience | No pain |
|---|---|---|---|---|---|
| Sensory subscale | |||||
| Throbbing | 7 (9.5) | 4 (5.4) | 2 (2.7) | 13 (17.6) | 61 (82.4) |
| Shooting | 3 (4.1) | 4 (5.4) | 1 (1.4) | 8 (10.8) | 66 (89.2) |
| Stabbing | 14 (18.9) | 8 (10.8) | 4 (5.4) | 26 (35.1) | 48 (64.9) |
| Sharp | 12 (16.2) | 8 (10.8) | 5 (6.8) | 25 (33.8) | 49 (66.2) |
| Cramping | 6 (8.1) | 8 (10.8) | 7 (9.5) | 21 (28.4) | 53 (71.6) |
| Gnawing | 0 | 4 (5.4) | 4 (5.4) | 8 (10.8) | 66 (89.2) |
| Hot-burning | 7 (9.5) | 4 (5.4) | 7 (9.5) | 18 (24.3) | 56 (75.7) |
| Aching | 11 (14.9) | 6 (8.1) | 8 (10.8) | 25 (33.8) | 49 (66.2) |
| Heavy | 17 (23) | 14 (18.9) | 6 (8.1) | 37 (50) | 37 (50) |
| Tender | 8 (10.8) | 9 (12.2) | 4 (5.4) | 21 (28.4) | 53 (71.6) |
| Splitting | 11 (14.9) | 4 (5.4) | 6 (8.1) | 21 (28.4) | 53 (71.6) |
| Affective subscale | |||||
| Tiring-exhausting | 21 (28.4) | 17 (23) | 11 (14.9) | 49 (66.2) | 25 (33.8) |
| Sickening | 7 (9.5) | 5 (6.8) | 10 (13.5) | 22 (29.7) | 52 (70.3) |
| Fearful | 5 (6.8) | 0 | 5 (6.8) | 10 (13.5) | 64 (86.5) |
| Punishing-cruel | 14 (18.9) | 7 (9.5) | 5 (6.8) | 26 (35.1) | 48 (64.9) |
Data are presented as number and percent
Pain intensity
Comparing participants' intensity score, the PRI was 7 (25th, 75th percentiles: 2.8,15) during day 1, and day 2 was 5 (25th, 75th percentiles: 2,11). Statistically significant differences in median intensity pain scores (P = 0.010), NRS, and PPI showed statistically significant differences (P = 0.021, P < 0.001, respectively) [Table 4].
Table 4.
Pain intensity as measured by the short-form McGill Pain Questionnaire (SF-MPQ)
| McGill pain questionnaire (n=74) | Day 1 | Day 2 | P |
|---|---|---|---|
| PRI | 7 IQR (2.8,15) | 5 (2,11) | 0.010 |
| NRS | 6 IQR (3,8) | 5 (2,8) | 0.021 |
| PPI | n (%) | ||
| No Pain | 5 (6.8) | 12 (16) | <0.001 |
| Mild | 16 (21.6) | 19 (25.7) | |
| Discomforting | 17 (23) | 26 (35) | |
| Distressing | 6 (8) | 4 (5) | |
| Horrible | 20 (27) | 10 (13.5) | |
| Excruciating | 10 (13.5) | 3 (4) | |
| Pain Description | n (%) | ||
| No Pain | 5 (6.8) | 11 (14.9) | 0.521 |
| Brief | 7 (9.5) | 4 (5) | |
| Intermittent | 44 (59.5) | 37 (50) | |
| Continuous | 18 (24) | 22 (29.7) |
Data are presented as number and percent. NRS: Numerical rating scale; PRI: Pain rating index
The medians and IQR (25th and 75th percentile) pain intensity scores according to gender as assessed by (A) PRI (male = 7,2,15] vs female = 12,3,15] P = 0.457), (B) PPI (male = 3,2,5] vs female = 5,2,5] P = 0.192); (C) NRS (male = 5,3,8] vs female = 8,4,10] P = 0.172) [Figure 1].
Figure 1.
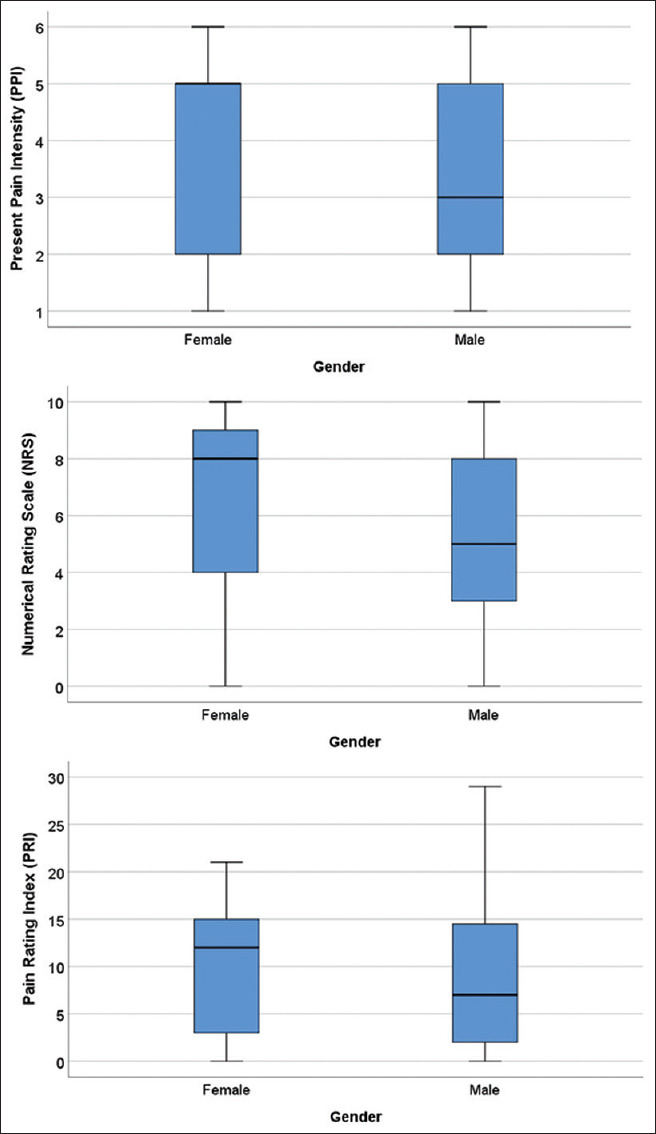
Baseline pain intensity scores of post-cardiac surgery patients according to gender
Pain location and aggregating factors
Most participants experienced bad pain sensation in the site of incision (27%), at the back and shoulders (14%), followed by pain at the site of the chest tube (7%). The aggravating factor that is most frequently associated with pain sensation was coughing (27%), and movement (18%) [Figure 2].
Figure 2.
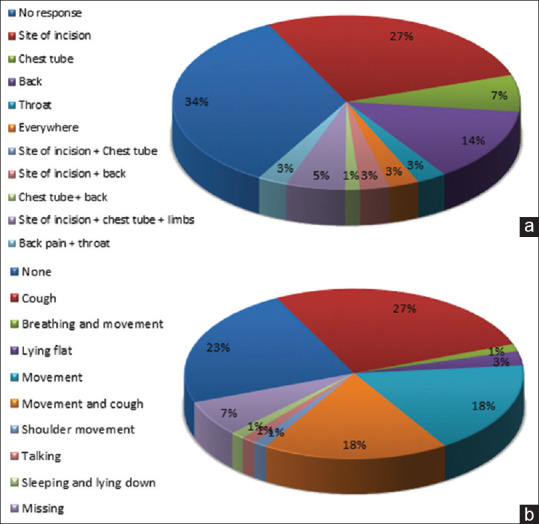
(a) Pain location and (b) pain aggregating factors of patients post-surgery
Pain medication administration patterns
The majority of the sample (39%) were prescribed 1 g of intravenous (IV) paracetamol, and 33.8% were prescribed a combination of 50 mg of IV Tramadol plus 1 g of IV paracetamol every 6 h. Analgesic medication with the lowest prescribing frequency was oral naproxen 250 mg (4%). Paracetamol was administered most frequently using the IV route.
The most frequent pain analgesic modality used on day 1 was multimodal, which includes two pain medications administered either orally or parenterally (49.6%), while the single parenteral drug was frequently used on day 2 (48.9%) [Table 5].
Table 5.
Pain medication administration pattern
| Pain medication strategy | Frequency and percentage of patients per pain management strategy | |
|---|---|---|
| Day 1 | Day 2 | |
| No pain medications | 7 (9.5) | 10 (13.5) |
| Single drug (oral) | 2 (2.7) | 8 (10.8) |
| Single drug (parenteral) | 31 (41.9) | 31 (41.9) |
| Multimodal (2 medications) | 33 (44.6) | 25 (33.8) |
| Multimodal (3 medications) | 1 (1.4) | 0 |
Data are presented as number and percent
Follow-up
Forty-five patients were followed up 1-month post-cardiac surgery to evaluate their pain level, description, location, and to observe any aggravating factors. Patients were evaluated if they are still taking their pain medications. Statistical significance reduction in numerical rating scores at the 30 days follow up (P = 0.003). 38% of the patients were taking their post-discharge pain medication, reasons for not taking pain medications were fear of side effects (n = 3; 9.1%), careless (n = 2; 6.1%), tolerable pain (n = 1; 3%), no pain (n = 6; 18.2%), and no pain medication prescribed (n = 6; 18.2%).
Discussion
Pain management after surgery involving sternotomy is an integral part of patients' care, which enhances the overall patients' experience and improves the outcomes. Mechanisms of post-cardiac surgery pain are complex, and the inflammatory response contributes to pain, in addition to the direct tissue trauma.[8] Pain is associated with unfavorable physical and psychological outcomes, in addition to the impaired quality of life and slow recovery.[9]
A variety of instruments are available to evaluate pain, such as the chronic pain grade scale (CPGS), pain catastrophizing scale, and the MPQ. The standard tool to measure pain in our institution was Wong-Baker Faces; however, it does not provide a thorough evaluation of pain. Therefore, we used the McGill pain questionnaire. Since the original form of MPQ is time-consuming, and it might be irritating to the patients, we used the SF-MPQ. The SF-MPQ is a widely used tool for qualitative and quantitative pain assessment that is suitable to assess sensory, affective, and evaluative dimensions of pain. It is easy to administer, and it usually takes about 5 min to complete.[7,10]
The pain intensity score of the patient's post-cardiac surgery was assessed and reported according to the following: PRI, NRS, and PPI. Results showed that there were differences in the intensity of pain according to the different measures used throughout the postoperative stay of the patients.
The common words used to describe surgical pain include sharp, stabbing, aching, dull, and tender.[11,12] However, these descriptions were not commonly used to express pain post-sternotomy in our study. Patients in this study found their pain to be predominately heavy (50%) and stabbing (35%). For the effective subscale pain perception, participants in this study were predominantly described as being tiring/exhausting (66%).
In this study, participants experienced higher pain scores in the first 48 h after extubation compared to other studies.[11] The highest pain score was observed after extubation, and the median NRS was 6 on day 1. The pain level was reduced over time, and the median NRS was 5 on day 2. The most common aggravation factors for the pain experience, according to patients, were coughing (27%) and movement (18%). Another study showed that coughing had the highest percentage as an aggravating factor; thus, the patient was directed to place a pillow at the site of the incision to minimize the pain.
Several management strategies are available for reducing postoperative pain, including opioids, anticonvulsants,[9] continuous local anesthetic infiltration, nerve blocks, intrapleural local anesthetics, alpha-adrenergic agonists, intrathecal techniques, and epidural techniques.[13] Multimodal analgesia offers a synergistic effect that maximizes pain relief at a lower analgesic dose.
In this study, paracetamol was the most commonly used therapy, followed by a combination of paracetamol and tramadol. While the most frequently used analgesics in other studies were morphine and dexmedetomidine.[14]
Regarding the discharge medications, 46% of patients have not prescribed any pain medications, and this might lead to several complications. Prescribing privilege is considered to be one of the obstacles to adequate pain control. Furthermore, the prescription was affected by the fear of acquiring physical dependence, tolerance, addiction, and side effects. Nurses may fail to routinely assess pain due to some barriers, including the language barrier, workload, and the defect of patients' ability to express their level of pain, and that might be due to religious and cultural beliefs.[15] It is crucial for health care professionals to understand the patients' experience and suffering and mitigate this with appropriate measures whenever possible.[4]
Limitation and recommendation
The study has several limitations; the SF-MPQ was conducted at a fixed time, so the effect before and after analgesic administration was not investigated nor the length of the analgesic effect. Because of the multicultural patients and health care practitioners, we recommend establishing a multilingual pain management team; its job is concerned in assessing the pain and managing it properly. We recommend obtaining a baseline pain score to compare it to the pain score for each patient as the standard of care and evaluate the postoperative change in pain perception rather than a fixed number for each patient.
Conclusion
Pain decreased on the second day after cardiac surgery compared to day 1. Paracetamol was the most prescribed analgesic; however, there was an underutilization which might be affected by insufficient pain reporting. There are few areas requiring improvements such as the use of a multimodal strategy to manage pain and proper communication of pain experience between patients and healthcare professionals.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Jensen MP, Tome-Pires C, de la Vega R, Galan S, Sole E, Miro J. What determines whether a pain is rated as mild, moderate, or severe? The importance of pain beliefs and pain interference. Clin J Pain. 2017;33:414–21. doi: 10.1097/AJP.0000000000000429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hjermstad MJ, Fayers PM, Haugen DF, Caraceni A, Hanks GW, Loge JH, et al. Studies comparing numerical rating scales, verbal rating scales, and visual analogue scales for assessment of pain intensity in adults: A systematic literature review. J Pain Symptom Manage. 2011;41:1073–93. doi: 10.1016/j.jpainsymman.2010.08.016. [DOI] [PubMed] [Google Scholar]
- 3.Chou R, Gordon DB, de Leon-Casasola OA, Rosenberg JM, Bickler S, Brennan T, et al. Management of postoperative pain: A clinical practice guideline from the American Pain Society, the American Society of Regional Anesthesia and Pain Medicine, and the American Society of Anesthesiologists' Committee on Regional Anesthesia, executive commi. J Pain. 2016;17:131–57. doi: 10.1016/j.jpain.2015.12.008. [DOI] [PubMed] [Google Scholar]
- 4.Krupic F, Custovic S, Jasarevic M, Sadic S, Fazlic M, Grbic K, et al. Ethnic differences in the perception of pain: A systematic review of qualitative and quantitative research. Med Glas (Zenica) 2019;16:108–14. doi: 10.17392/966-19. [DOI] [PubMed] [Google Scholar]
- 5.Melzack R. The short-form McGill Pain Questionnaire. Pain. 1987;30:191–7. doi: 10.1016/0304-3959(87)91074-8. [DOI] [PubMed] [Google Scholar]
- 6.Strand LI, Ljunggren AE, Bogen B, Ask T, Johnsen TB. The short-form McGill pain questionnaire as an outcome measure: Test-retest reliability and responsiveness to change. Eur J Pain. 2008;12:917–25. doi: 10.1016/j.ejpain.2007.12.013. [DOI] [PubMed] [Google Scholar]
- 7.Terkawi AS, Tsang S, Abolkhair A, Alsharif M, Alswiti M, Alsadoun A, et al. Development and validation of Arabic version of the short-form McGill pain questionnaire. Saudi J Anaesth. 2017;11(Suppl 1):S2–10. doi: 10.4103/sja.SJA_42_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Huang APS, Sakata RK. [Pain after sternotomy-review] Rev Bras Anestesiol. 2016;66:395–401. doi: 10.1016/j.bjan.2014.09.003. [DOI] [PubMed] [Google Scholar]
- 9.Cogan J. Pain management after cardiac surgery. Semin Cardiothorac Vasc Anesth. 2010;14:201–4. doi: 10.1177/1089253210378401. [DOI] [PubMed] [Google Scholar]
- 10.Wright KD, Asmundson GJ, McCreary DR. Factorial validity of the short-form McGill pain questionnaire (SF-MPQ) Eur J Pain. 2001;5:279–84. doi: 10.1053/eujp.2001.0243. [DOI] [PubMed] [Google Scholar]
- 11.Menda F, Koner O, Sayin M, Ergenoglu M, Kucukaksu S, Aykac B. Effects of single-dose gabapentin on postoperative pain and morphine consumption after cardiac surgery. J Cardiothorac Vasc Anesth. 2010;24:808–13. doi: 10.1053/j.jvca.2009.10.023. [DOI] [PubMed] [Google Scholar]
- 12.Swaika S, Parta N, Chattopadhyay S, Bisui B, Banarjee SS, Chattarjee S. A comparative study of the efficacy of intravenous Paracetamol and Dexmedetomidine on peri-operative hemodynamics and post-operative analgesia for patients undergoing laparoscopic cholecystectomy. Anesth Essays Res. 2013;7:331–5. doi: 10.4103/0259-1162.123225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Smith LM, Barrington MJ. Ultrasound-guided blocks for cardiovascular surgery: Which block for which patient? Curr Opin Anaesthesiol. 2020;33:64–70. doi: 10.1097/ACO.0000000000000818. [DOI] [PubMed] [Google Scholar]
- 14.Brock L. Dexmedetomidine in adult patients in cardiac surgery critical care: An evidence-based review. AACN Adv Crit Care. 2019;30:259–68. doi: 10.4037/aacnacc2019888. [DOI] [PubMed] [Google Scholar]
- 15.Sinatra R. Causes and consequences of inadequate management of acute pain. Pain Med. 2010;11:1859–71. doi: 10.1111/j.1526-4637.2010.00983.x. [DOI] [PubMed] [Google Scholar]


