Abstract
Objective:
To compare the anesthetic performances of 3% prilocaine and 4% articaine when used for the extraction of the maxillary teeth.
Materials and Methods:
Ninety-five patients, aged between 16 and 70 years, were included in this study. Patients were divided into two groups. Group one received articaine 4% with 1:00.000 adrenaline. Group two received prilocaine with 3% felypressin (0.03 I.U. per ml). Onset time of anesthesia was objectively evaluated by using electronic pulp testing.
Results:
Eighty-five patients in this study had a successful local anesthetic followed by extraction within the study duration time (10 minutes). However, there were six patients with failure anesthesia (5 in prilocaine group and 1 in articaine group). By applying Person's Chi-square test (x2), there were no significant differences in the number of episodes of the anesthetic success between articaine and prilocaine groups at time intervals (P = 0.5). T-test showed that there have been no important variations within the mean onset time of anesthesia for articaine and prilocaine buccal infiltrations (P = 0.1).
Conclusions:
3% Prilocaine with felypressin is as effective as 4% articaine with adrenaline when used for the extraction of maxillary teeth. Recommendations would be given to the dental practitioners to use prilocaine more frequently than articaine because of its low toxicity.
Trial registration number:
Keywords: Carticaine, dental extraction, injections, prilocaine
Introduction
Pain associated with dental treatment is still considered as the main source of fear and anxiety in dentistry regardless of the patient's gender and age.[1,2] Local anesthetics are still the most successful agents used for controlling dental pain.[3] In the market, there are too many anesthetic drugs are available to dentists to use with different techniques.[4] The dental practitioners' point of view about the optimal local anesthetic for use in dentistry is the fastest in action and least toxic.[5,6,7,8] Choosing the best local anesthetic agents regarding safety and speed of action is still unapproachable.[2,3,4,5,6] Most of the local anesthetic agents are producing vasodilation in particular amide group. Vasodilation results in the increased rate of absorption and reduced duration of action of anesthesia and consequently, increased anesthetic blood level and risk for toxicity.[9,10,11] Prilocaine is classified as the weakest powerful vasodilator. So, it can be useful for anesthetizing the patients who are prohibited from the use of local anesthetics with adrenaline. Prilocaine (3%) with felypressin (0.03 IU/mL) is mainly used in cases when adrenaline is best avoided. Prilocaine is less toxic than articaine.[12] Metabolism of prilocaine occurs in two stages. The first stage happens in the lungs and kidneys, and it produces metabolites.[13,14] These metabolites of prilocaine are more easily breaking down by the liver than articaine.[12] So, the kidney gets rid of prilocaine faster than other amides. Felypressin is weak vasoconstriction because it constricts venous outflow.[15] However, adrenaline is strong vasoconstriction because it constricts artery inflow.[14] Felypressin is similar to oxytocin, and it can induce oxytocic action on the uterus.[10,12] Felypressin can also cause coronary artery vasoconstriction. So, felypressin is contraindicated in the late pregnancy stages and in patients with unstable angina and poorly controlled hemorrhage.[16,17]
On other hand, articaine is also an amide local anesthetic with a unique chemical structure.[18] The presence of thiophene ring in its chemical structure resulted in an increase in lipid solubility and diffusing better through soft tissues than do other anaesthetic, consequently, articaine achieves fast onset time of action along with deep nerve anesthesia.[8] Articaine is metabolized in the liver, but because of the extra ester bond, it is metabolized by cholinesterase in blood as well.[18,19] This characteristic is significant, particularly, for patients with liver disease.[19]
In light of these facts, the aim of this study was to compare the anesthetic performances of 3% prilocaine (the safest local anesthetic) with 4% articaine (the local anesthetic with fastest onset time of action) when used for the removal of the upper teeth.
Material and Methods
This randomized clinical study was conducted at the Taibah College of Dentistry in November 2017 to compare the effectiveness of 4% articaine with 3% prilocaine for the extraction of the maxillary teeth. After finishing the whole study, statistical analysis was carried out to compare the anesthesia onset time for articaine and prilocaine groups. The main protocol of the study was approved by the Taibah Dental College Research Ethics Committee. Recruitment of patients for this study was carried out at the Department of Oral and Maxillofacial Surgery in the Taibah University College of Dentistry. A total number of 95 patients were assigned to the articaine and prilocaine groups. Inclusion criteria consisted of: Patients having one or two upper teeth for extraction, subject tooth or its adjacent must be vital, healthy patient or patient with mild systemic diseases (class I or II according to the American Society of Anesthesiology). Patients excluded from this study if they had allergy to local anesthetic agents or needed surgical or multiple teeth extraction. Patients were randomly allocated to the study groups by a researcher who printed out a certain number of pieces of paper with 3% prilocaine and 4% articaine. Randomization was done by a secretary of the department who mixed up the pieces of paper and placed them in the opaque envelopes along with a copy of datasheet. After that, the envelopes were sealed and numbered in sequence. In clerking sessions, if a patient was included in the study a numbered envelope was hooked up to the patient's dental record.
On the dental chair, the envelope was opened by a dental assistant who reads the piece of paper and loaded the dental syringe with the appropriate local anesthetic cartilage. Before the administration of LA, a patient was asked to read the information sheet and sign the consent form. The dental assistant who prepared the local anesthetic cartridges was fully unaware of the whole process. Regardless of the group to which the patient belongs, the buccal infiltration technique was applied by inserting a short needle at the height of buccal sulcus along the long axis of the subject tooth for extraction. The depth of penetration was from 4 to 7 mm to deposit 1.4 ml of the anesthetic solution around the apex of the subject tooth. The palatal infiltrative injection was administered by inserting the needle 5 mm far from the gingival margin of the subject tooth and deposing the remaining 0.4 ml of local anesthetic solution. The success of anesthesia was checked objectively by using electronic pulp tester. Interval time of 2 minutes was set out to examine the anesthetic success of the subject tooth throughout the study duration of 10 minutes. Anesthesia was considered successful if the examined tooth did not release any painful sensation when exposed to a stimulating force of 64 mV. Extraction was carried out at any point of the trial (10 minutes), on condition that the anesthetized tooth becomes unresponsive for the highest pulp stimulation (64 reading). Ten minutes after the injection, the anesthetized tooth was still responsive to electrical pulp tester, then the second cartridge of LA was given. The patient and the researcher were unaware of the type of LA that was injected. All anesthesia injections were given by the same surgeon. Standard aspirating dental cartridge syringes (USA: ATI) fitted with 27 gauge, 21 mm short needles (C-K Ject [27 gauge] 0.4 mm × 21 mm, Korea) were used for buccal and palatal infiltrations.
Statistical analysis
The sample size for this study was calculated based on a study by Nydegger et al.[11] A number of 90 participants would have 90% power to detect the differences in the mean onset time of two anesthetic agents assuming a significance level of 5%. So, 95 patients were recruited in this study and Statistical Package for the Social Sciences (SPSS 20) was used to carry out descriptive, crosstabs analysis, and independent sample t-test.
Results
Ninety-five patients enrolled in this study. Four patients were excluded because they fainted after the administration of local anesthetics. The final sample size included 91 patients with an age range from 16 to 70 years (mean 36 years, standard deviation 12.5).
Anesthetic success
Within the study duration of 10 minutes, 85 patients in articaine and prilocaine groups achieved successful pulpal anesthesia and extraction. However, six patients (five in prilocaine group and one in articaine group) failed to secure anesthetic success for their upper teeth and extra local anesthesia was given to accomplish the dental extraction. Nonparametric test was used to calculate the number of episodes with anesthetic success when maximal pulp stimulation (64 reading) was applied with no positive responses. Table 1 summarizes the success of anesthesia in the upper teeth of 91 patients who took part in this study. In this table, “no response to maximal electronic pulp stimulation (64 reading)” means successful anesthesia, and “positive response to electronic pulp stimulation” means failed anesthesia. By applying Person's Chi-square test (x2), there were no significant differences in the number of episodes of the anesthetic success for patients in articaine and prilocaine groups on time intervals (P = 0.5).
Table 1.
Number and percentages of anaesthetic successes at time interval for upper teeth pulp anaesthesia following prilocaine and articaine buccal infiltration in 91 adult patients
| Anaesthetic success at time interval | 2 min n (%) | 4 min n (%) | 6 min n (%) | 8 min n (%) | 10 min n (%) | >10 min n (%) | Total n (%) |
|---|---|---|---|---|---|---|---|
| Prilocaine regimen | 27 (58) | 10 (22) | 4 (9) | 0 (0.0) | 0 (0) | 5 (11) | 46 (100) |
| Articaine regimen | 32 (71) | 8 (18) | 3 (7) | 1 (2) | 0 (0) | 1 (2) | 45 (100) |
| Person’s Chi- square test (χ2) | 4.578 | ||||||
| P | 0.5 |
Onset time of anesthesia
The speed of action of anesthesia and the start of extraction ranged from 2 to 14 minutes. Table 2 shows that the mean time for starting anesthesia and removal of the teeth in the upper jaw for the patients in the articaine group (articaine regimen: 3 min, SD, 2.1 min) was clinically faster than those who were in prilocaine group [prilocaine regimen: Mean 4 min, standard deviation (SD) 3.3 min]. The application of independent samples t-test revealed that there were no significant differences in the mean onset time of anesthesia for articaine and prilocaine buccal infiltrations (P = 0.0.1). The results are listed in Table 2. Figure 1 outlines the number of patients who achieved anesthetic successes on time interval for both prilocaine and articaine groups. The average time of anesthesia and dental extraction for patients in the articaine group was faster than patients in the prilocaine group but the differences were not significant.
Table 2.
Comparisons between mean onset time of pulpal anaesthesia and extraction of the patients for articaine and prilocaine infiltration groups
| Groups | n | Number of volunteers | Mean (min) | SD | t-test (df=89 | P |
|---|---|---|---|---|---|---|
| Anaesthesia and extraction onset time | Articaine regimen | 45 | 3 | 2.1 | -1.65 | 0.1 |
| Prilocaine regimen | 46 | 4 | 3.3 |
Figure 1.
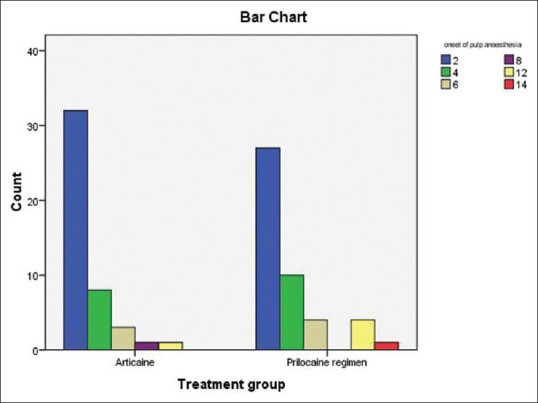
Representing the number of patients who achieved anaesthetic successes at time interval for both prilocaine and articaine groups
Discussion
This study was designed to weigh the advantages and disadvantages of clinical performances of 4% articaine with epinephrine (1:100,000) and 3% prilocaine with felypressin (0.03 I.U. per ml) for the extraction of the maxillary teeth. The findings of this study revealed that there were no significant differences in the onset time of action and the depth of anesthesia for 4% articaine and 3% prilocaine when used for the extraction of the maxillary teeth. However, clinically, injected teeth by articaine was anesthetized faster than injected ones by prilocaine. In light of these findings, the author (GG) believes that prilocaine can be the best local anesthetic agent for use in dentistry. Prilocaine is as effective as lidocaine and articaine for use in dentoalveolar surgery.[1,15,20] Prilocaine is safer than lidocaine and articaine because it is considered as the least vasodilator agent.[20] So, it has less toxicity and few hemodynamic effects making it a good choice for use in children, elderly people, and patients who have contraindications to the use of local anesthesia with adrenaline.[19,20,21,22] In other words, prilocaine has good efficacy and an excellent safety profile compared with other amides. Although articaine has a fast onset time of action amongst the amide local anesthetic agent, it is not recommended to use for inferior alveolar nerve block.[23] It has been associated with a higher risk of nerve damage (permanent lower lip paraesthesia) when used as a block technique. So, articaine can only be used for infiltration injections.[5,24,25,26] The author's judgment is sported by the U.S. Food and Drug Administration (FDA), which reported that lidocaine and prilocaine have the best ranking to be used as local anesthetic agents for special patient populations.[7] Our findings are consistent with a result of a recent study conducted by Alsharif et al.[20] comparing the onset time of action of 2% lidocaine and 3% prilocaine for upper teeth extractions. They found that both prilocaine and lidocaine possess a similar potency and onset time of action.[20] A review Cochrane study carried out by St George G, et al.[1] to compare the success of anesthesia amongst different local anesthetic agents used for various dental procedures. The results of this review showed that there is weak evidence that recommends that 4% articaine, 1: 100,000 epinephrine was better than 2% lidocaine, 1: 100,000 epinephrine for endodontic therapy. However, 2% lidocaine, 1: 100,000 epinephrine was stronger than 4% prilocaine plain when used for the anesthesia of surgical procedures.[1] Moreover, a clinical trial was conducted in volunteers by Hass et al.[15] to compare the anesthetic efficacy of 4% articaine and 4% prilocaine when injected by infiltration technique to anesthetize the upper and lower teeth. The outcome of the study by Hass et al. reported that articaine was equivalent to prilocaine with respect to the ability to induce anesthesia of labial, lingual, and pulpal tissues when administered by labial infiltration.[15] Articaine has gained popularity among dentists because of its superior onset, duration, potency, and tissue diffusion properties.[27,28] However, mepivacaine and prilocaine are the only local anesthetics in dentistry formulated without a vasoconstrictor and have played a role in treating medically compromised patients who may not tolerate a local anesthetic containing adrenaline.[27,29]
In light of these facts, this study provided strong evidence for using prilocaine with felypressin as a good choice in the dentistry in particular with children, elderly patients, patients with cardiovascular impairment and other medically compromised patients who may not tolerate lidocaine/articaine with adrenaline.
Conclusions
Prilocaine (3%) with felypressin is as effective as 4% articaine with adrenaline when used for the extraction of maxillary teeth. Recommendations would be given to the dental practitioners to use prilocaine more frequently than articaine because of its low toxicity.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
The author would like to thank all dental surgeons and assistants in the Oral and Maxillofacial department.
References
- 1.St George G, Morgan A, Meechan J, Moles DR, Needleman I, Ng YL, et al. Injectable local anaesthetic agents for dental anaesthesia. Cochrane Database Syst Rev. 2018;7:CD006487. doi: 10.1002/14651858.CD006487.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gheisari R, Resalati F, Mahmoudi S, Golkari A, Mosaddad SA. Do different modes of delivering postoperative instructions to patients help reduce the side effects of tooth extraction? A randomized clinical trial. J Oral Maxillofac Surg. 2018;76:1652. doi: 10.1016/j.joms.2018.04.019. e1-e7. [DOI] [PubMed] [Google Scholar]
- 3.Alzahrani F, Duggal MS, Munyombwe T, Tahmassebi JF. Anaesthetic efficacy of 4% articaine and 2% lidocaine for extraction and pulpotomy of mandibular primary molars: An equivalence parallel prospective randomized controlled trial. Int J Paediatr Dent. 2018;28:335–44. doi: 10.1111/ipd.12361. [DOI] [PubMed] [Google Scholar]
- 4.Gazal G, Alharbi R, Fareed WM, Omar E, Alolayan AB, Al-Zoubi H, et al. Comparison of onset anesthesia time and injection discomfort of 4% articaine and 2% mepivacaine during teeth extractions. Saudi J Anaesth. 2017;11:152–7. doi: 10.4103/1658-354X.203017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gazal G, Fareed WM, Zafar MS. Role of intraseptal anaesthesia for pain-free dental treatment. Saudi J Anaesth. 2016;10:81–6. doi: 10.4103/1658-354X.169482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gazal G, Alharbi AM, Al-Samadani KH, Kanaa MD. Articaine and mepivacaine buccal infiltration in securing mandibular first molar pulp anesthesia following mepivacaine inferior alveolar nerve block: A randomized, double-blind crossover study. Saudi J Anaesth. 2015;9:397–403. doi: 10.4103/1658-354X.159463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Li J, Wei W, Yang W, Li J, Gao Y, Qian Y. Comparison of clinical efficacy and safety between articaine and lidocaine in the anaesthesia management of tooth pulp disease. Pak J Pharm Sci. 2018;31:2303–6. [PubMed] [Google Scholar]
- 8.Shahi S, Rahimi S, Yavari HR, Ghasemi N, Ahmadi F. Success rate of 3 injection methods with articaine for mandibular first molars with symptomatic irreversible pulpitis: A CONSORT randomized double-blind. Clinical Trial J Endod. 2018;44:1462–6. doi: 10.1016/j.joen.2018.07.010. [DOI] [PubMed] [Google Scholar]
- 9.Karm MH, Kim M, Park FD, Seo KS, Kim HJ. Comparative evaluation of the efficacy, safety, and hemostatic effect of 2% lidocaine with various concentrations of epinephrine. J Dent Anesth Pain Med. 2018;18:143–9. doi: 10.17245/jdapm.2018.18.3.143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mishra A, Lalani Z, Kalakonda B, Krishnan P, Pandey R, Reddy K. Comparative evaluation of hemodynamic, vasoconstrictive, and SpO2 variability during different stages of periodontal surgery performed using 0.5% ropivacaine or 2% lignocaine HCl (1:80,000 adrenaline) local anesthesia: A randomized, double-blind, split-mouth pilot study. J Indian Soc Periodontol. 2018;22:243–8. doi: 10.4103/jisp.jisp_18_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nydegger B, Nusstein J, Reader A, Drum M, Beck M. Anaesthetic comparisons of 4% concentrations of articaine, lidocaine, and prilocaine as primary buccal infiltrations of the mandibular first molar: A prospective randomized, double-blind study. J Endod. 2014;40:1912–6. doi: 10.1016/j.joen.2014.08.001. [DOI] [PubMed] [Google Scholar]
- 12.Katz S, Drum M, Reader A, Nusstein J, Beck M. A prospective, randomized, double-blind comparison of 2% lidocaine with 1: 100,000 epinephrine, 4% prilocaine with 1: 200,000 epinephrine, and 4% prilocaine for maxillary infiltrations. Anesth Prog. 2010;57:45–51. doi: 10.2344/0003-3006-57.2.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pool SM, Struys MM, van der Lei B. A randomised double-blinded crossover study comparing pain during anaesthetising the eyelids in upper blepharoplasty: First versus second eyelid and lidocaine versus prilocaine. J Plast Reconstr Aesthet Surg. 2015;68:1242–7. doi: 10.1016/j.bjps.2015.04.021. [DOI] [PubMed] [Google Scholar]
- 14.Shinzaki H, Sunada K. Advantages of anterior inferior alveolar nerve block with felypressin-propitocaine over conventional epinephrine-lidocaine: An efficacy and safety study. J Dent Anesth Pain Med. 2015;15:63–8. doi: 10.17245/jdapm.2015.15.2.63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Haas DA, Harper DG, Saso MA, Young ER. Comparison of articaine and prilocaine anesthesia by infiltration in maxillary and mandibular arches. Anesth Prog. 1990;37:230–7. [PMC free article] [PubMed] [Google Scholar]
- 16.Oliver G, David DA, Bell C, Robb N. An investigation into dental local anaesthesia teaching in United Kingdom dental schools. SAAD Dig. 2016;32:7–13. [PubMed] [Google Scholar]
- 17.Hashemi SH, Ladez SR, Moghadam SA. Comparative assessment of the effects of three local anaesthetics: Lidocaine, prilocaine, and mepivacaine on blood pressure changes in patients with controlled hypertension. Glob J Health Sci. 2016;8:54157. doi: 10.5539/gjhs.v8n10p227. [DOI] [PubMed] [Google Scholar]
- 18.Gazal G. Is articaine more potent than mepivacaine for use in oral surgery? J Oral Maxillofac Res. 2018;9:e5. doi: 10.5037/jomr.2018.9305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gazal G. Is prilocaine safe and potent enough for use in the oral surgery of medically compromised patients. Saudi Med J. 2019;40:97–100. doi: 10.15537/smj.2019.1.23475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Alsharif A, Omar E, Alolayan AB, Bahabri R, Gazal G. 2% lidocaine versus 3% prilocaine for oral and maxillofacial surgery. Saudi J Anaesth. 2018;12:571–7. doi: 10.4103/sja.SJA_259_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Byakodi S, Gurjar V, Soni S. Glucose levels and hemodynamic changes in patients submitted to routine dental extraction under local anesthesia with and without adrenaline. J Contemp Dent Pract. 2017;18:57–9. doi: 10.5005/jp-journals-10024-1989. [DOI] [PubMed] [Google Scholar]
- 22.Torres-Lagares D, Serrera-Figallo MÁ, Machuca-Portillo G, Corcuera-Flores JR, Machuca-Portillo C, Castillo-Oyagüe R, et al. Cardiovascular effect of dental anesthesia with articaine (40 mg with epinefrine 0,5 mg% and 40 mg with epinefrine 1 mg%) versus mepivacaine (30 mg and 20 mg with epinefrine 1 mg%) in medically compromised cardiac patients: A cross-over, randomized, single blinded study. Med Oral Patol Oral Cir Bucal. 2012;17:e655–60. doi: 10.4317/medoral.17892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bonar T, Nusstein J, Reader A, Drum M, Fowler S, Beck M. Anaesthetic efficacy of articaine and lidocaine in a primary intraseptal injection: A prospective, randomized double-blind study. Anesth Prog. 2017;64:203–11. doi: 10.2344/anpr-64-04-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ghadimi S, Shahrabi M, Khosravi Z, Behroozi R. Efficacy of articaine infiltration versus lidocaine inferior alveolar nerve block for pulpotomy in mandibular primary second molars: A randomized clinical trial. J Dent Res Dent Clin Dent Prospects. 2018;12:97–101. doi: 10.15171/joddd.2018.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rayati F, Noruziha A, Jabbarian R. Efficacy of buccal infiltration anaesthesia with articaine for extraction of mandibular molars: A clinical trial. Br J Oral Maxillofac Surg. 2018;56:607–10. doi: 10.1016/j.bjoms.2018.06.012. [DOI] [PubMed] [Google Scholar]
- 26.Sawadogo A, Coulibaly M, Quilodran C, Bationo R, Konsem T, Ella B. Success rate of first attempt 4% articaine para-apical anesthesia for the extraction of mandibular wisdom teeth. J Stomatol Oral Maxillofac Surg. 2018;119:486–8. doi: 10.1016/j.jormas.2018.06.005. [DOI] [PubMed] [Google Scholar]
- 27.Moore PA. Innovations in local anesthesia are easing the pain of dentistry. Compend Contin Educ Dent. 2018;39:256–7. [PubMed] [Google Scholar]
- 28.Gazal G. Overcoming the failure of anesthesia in the mandibular teeth. Saudi Med J. 2019;40:425. doi: 10.15537/smj.2019.5.24078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gazal G, Omar E, Fareed WM, Alsharif A, Bahabri R. Impact of maxillary teeth morphology on the failure rate of local anesthesia. Saudi J Anaesth. 2020;14:57–62. doi: 10.4103/sja.SJA_542_19. [DOI] [PMC free article] [PubMed] [Google Scholar]


