Abstract
Introduction:
Accountable care organizations (ACOs) have been successful in improving quality of care but little is known about who is benefitting from ACOs and through what mechanism. This study examines variation of potentially preventable hospitalizations (PPHs) for chronic conditions with co-existing depression in adults by hospital ACO affiliation and care coordination strategies by race/ethnicity.
Methods:
Eleven 2015 State Inpatient Databases were used to identify PPHs for chronic conditions with co-existing depression by race/ethnicity; the 2015 American Hospital Association’s Annual Survey to identify hospital ACO affiliation; and American Hospital Association’s Survey of Care Systems and Payment (collected January–August 2016) to identify hospital ACO affiliation and hospital-based care coordination strategies, such as telephonic outreach, and chronic care management. In 2019, multiple logistic regressions tested the probability of PPH by ACO-affiliation and race/ethnicity. A subsample analysis of ACO-affiliated hospitals repeated the tests by care coordination strategy.
Results:
PPHs were significantly lower among ACO-affiliated hospitals compared with ACO-unaffiliated hospitals. Lower PPH rates were observed among white, African American, Native American, and Hispanic patients. Effective care coordination strategies varied by patient race. Results also showed variation of the adoption of specific care coordination strategies among ACO-affiliated hospitals. Analysis further indicated effective care coordination strategies varied by patients’ race.
Conclusions:
ACOs and specifically designed care coordination strategies can potentially improve PPH rates and racial disparities among patients with depression. Findings support the integration of mental and physical health services and provide insights for Centers for Medicare and Medicaid Services risk adjustment efforts across race/ethnicity and SES.
INTRODUCTION
Mental health disorders are common comorbidities to heart diseases, diabetes, asthma, and hypertension.1–5 Patients with mental health disorders face higher risk for premature mortality, incur higher costs, and receive lower-quality medical care compared with those without a mental health comorbidity.6–9 Poor integration between physical and mental health sectors has contributed to challenges in meeting the complex care needs of individuals with mental health conditions.10,11 Additionally, minority populations endure systematic and social barriers to quality physical and mental health care and treatment.11–16 These inequities are exacerbated by racial and ethnic disparities in the onset and prevalence of comorbid mental and chronic conditions (e.g., hypertension and diabetes),11,17–19 resulting in higher rates of potentially preventable hospitalizations (PPHs).20
Although a major barrier to physical and mental health integration is the general lack of behavioral healthcare providers, minority populations are also less likely to seek out mental health care, even in areas with a high density of mental health specialists.21–23 This is often due to cultural stigma around seeking mental health care and instances of discrimination that have resulted in lack of trust in medical providers.24–30 However, when providers recognize the historic, systematic, and social barriers impacting access to care and implement patient-centered care coordination programs, racial/ethnic disparities are reduced.9,11,31 This occurs through relationship building, addressing access to service barriers (i.e., financial, housing, transportation, language), and providing culturally tailored communication and self-management tools.9,11,31–33 For these reasons, care coordination has been identified as a critical component of improving quality of care and patient experience within the healthcare system.9,21
An accountable care organization (ACO) is a population-based care delivery and payment model where groups of doctors, hospitals, and other providers voluntarily come together to provide high-quality care to a pre-defined patient population, and are collectively financially responsible for the costs and quality of care.34 Some ACOs were modeled on managed care settings, like HMOs, but ACOs are required to meet Centers for Medicare and Medicaid Services (CMS) quality measures and are often provider-led instead of insurance-led.35 Most importantly, ACOs encourage value-based payment to reimburse high-quality care.36 Though early evaluations of ACOs have determined that few have integrated physical and mental health care,21,37 many have adopted care coordination strategies (CCSs).38,39 Research suggests that improvements in hospital inpatient quality are due to the integrated and collaborative CCSs for individuals with chronic physical conditions, and often those with comorbid mental health conditions.9,21,39–43 Based on these early successes in quality and high adoption rates of CCSs, ACOs may potentially reduce racial/ethnic health disparities if equitably implemented. However, little is known about the association between ACOs and quality of care for minorities.44–46
Hospitals shifting to innovative delivery models like ACOs and investing in CCSs represent an important opportunity to ensure high-quality care for everyone. This study aims to examine associations between hospital ACO affiliation and PPHs for chronic conditions with co-existing depression. Chronic conditions include heart disease, asthma, diabetes, and hypertension, which are major comorbidities for people with depression. Particularly, the study examines such associations by patient’s race and ethnicity and seeks to assess specific CCSs among ACO-affiliated hospitals. The hypothesis is that ACO-affiliated hospitals and CCSs can link to reduced PPHs for all patients with comorbid physical and mental conditions, especially for racial and ethnic minority populations.
METHODS
This analysis linked 2015 data from 11 State Inpatient Databases, Healthcare Cost and Utilization Project, Agency for Healthcare Research and Quality47 with two American Hospital Association (AHA) surveys: Annual Survey (collected November 2016)48 and Survey of Care Systems and Payment (collected January–August 2016).49 The use of these databases does not involve human subjects and requires neither IRB review nor exemption. State Inpatient Databases are state-specific files that contain all inpatient records for a calendar year from participating states.47 Eleven state files (Arizona, Colorado, Florida, Kentucky, Maryland, North Carolina, New Jersey, Oregon, Rhode Island, Washington, and Wisconsin) were used based on the availability of patients’ race/ethnicity, ZIP codes, linkages to AHA surveys, and other factors.
Study Sample
The study population included adults aged ≥18 years, with either an emergency, urgent, or elective admission into a general medical/surgical hospital and discharged to home or self-care. The sample was limited to 485,979 discharges with depression as a coexisting (secondary or subsequent) diagnosis, identified using the CMS Chronic Conditions Data Warehouse algorithm.50 After excluding observations without an AHA linkage to the key independent variable (n=71,738), the sample was reduced to 414,241 observations of which 14,019 (3%) had missing variables. Missing variables were mainly patient insurance coverage and mean income by ZIP code. The final sample size includes 400,222 discharges, which included 682 hospitals in 11 states.
Measures
The dependent variable was a PPH for a chronic condition as the primary diagnosis. This study focused on chronic conditions as they are common comorbidities of depression. PPHs were defined using the Agency for Healthcare Research and Quality’s Prevention Quality Indicators (PQIs),51 which were matched to chronic conditions identified in the CMS adult core set of quality care measures.52 The following chronic conditions were used: uncontrolled diabetes (PQI 14), diabetes related short-term and long-term complications (PQI 1 and PQI 3), chronic obstructive pulmonary disease or asthma (PQI 5 and PQI 15), hypertension (PQI 7), and heart failure (PQI 8). The National Quality Forum has endorsed PQIs as a measure to evaluate the quality of care for chronic conditions in the hospital setting.
The key independent variable was ACO affiliation—obtained from the AHA Annual Survey, which tracks and monitors systems of care.49 A qualified member of each hospital, responded yes or no to the question: Has your hospital or health care system established an accountable care organization (ACO)? Discharges were categorized as ACO-affiliated or ACO-unaffiliated.
This study also examined racial and ethnic disparities in PPHs with co-existing depression by hospital ACO affiliation and effectiveness of CCSs. Healthcare Cost and Utilization Project staff create a uniform value for race because of variations in state-collected race/ethnicity data, where Hispanic represents those of any race and non-Hispanic is broken out by racial groups: white, African American, Asian or Pacific Islander, Native American, and other/multi-race. Other patient characteristics controlled for included age, sex, total number of chronic conditions, expected primary payer, and the mean household income of the patient’s ZIP code.53,54 The following hospital characteristics obtained from the 2015 AHA Annual Survey were also controlled for: ownership, beds, rural, teaching status, safety net provider, state, and a fourth quarter discharge indicator to identify a possible trend shift during the conversion from ICD-9 to ICD-10.48,55,56
The AHA’s Survey of Care Systems and Payment captures 12 CCSs, including “chronic care management processes or programs to manage patients with high volume, high cost chronic diseases,” “post-hospital discharge continuity of care program,” among others. CCS adoption was evaluated based on a 5-point Likert scale from 1=not used at all to 5=used hospital-wide, where adoption was categorized as “4=used widely” or “5=used hospital-wide.” The total number of CCSs a hospital adopted was calculated.
Statistical Analysis
Using a cross-sectional study design, the basic model followed the structure: E(PQIi,h,k) = f(β0 + βiIi + βAACOh + βHHh + βSSk), where PQIi,h,k is a measure of an the outcome variable on individual i, in hospital h, and state k and f is the functional form. First, a tabulation summary of discharges with co-existing depression by hospital ACO affiliation was conducted and tested for differences between the two groups. Then, the adjusted odds of PPHs by hospital ACO affiliation was determined using a logistic regression. Additional logistic regressions were conducted for each race/ethnicity.
A subsample analysis among ACO-affiliated hospitals (86 hospitals) was performed to examine the association between CCSs and PPH. Hospital CCS adoption rates were compared across all ACOs, and then used to estimate the association between CCS and PPH for white and African American patient discharges separately—first, for the total number of CCSs using ordinary linear regressions, and then for each of the 12 CCSs individually using logistic regressions. The study was conducted in 2019 using Stata, version 15 for all analyses.
RESULTS
Of the 400,222 hospital discharges of patients aged ≥18 years with depression in 2015 in 11 states, 38,901 (10%) were potentially preventable and 47% were in ACO-affiliated hospitals (Appendix Table 1). Figure 1 presented variation of the PPH rates by hospital ACO affiliation and patient’s race and ethnicity. The highest rates of PPHs were among African American patients with depression at about 13% in ACO-affiliated hospitals and 15% in ACO-unaffiliated hospitals. By contrast, Asian patients with depression had the lowest, with a PPH rate of 7.6% in ACO-affiliated hospitals and 7.8% in ACO-unaffiliated hospitals. Overall, ACO-affiliated hospitals had significantly fewer PPHs in their white, African American, Native American, and other/multi-race patient populations compared with ACO-unaffiliated hospitals. Variation of patient and hospital characteristics by hospital ACO participation were observed (results not shown; Appendix Table 1).
Figure 1.
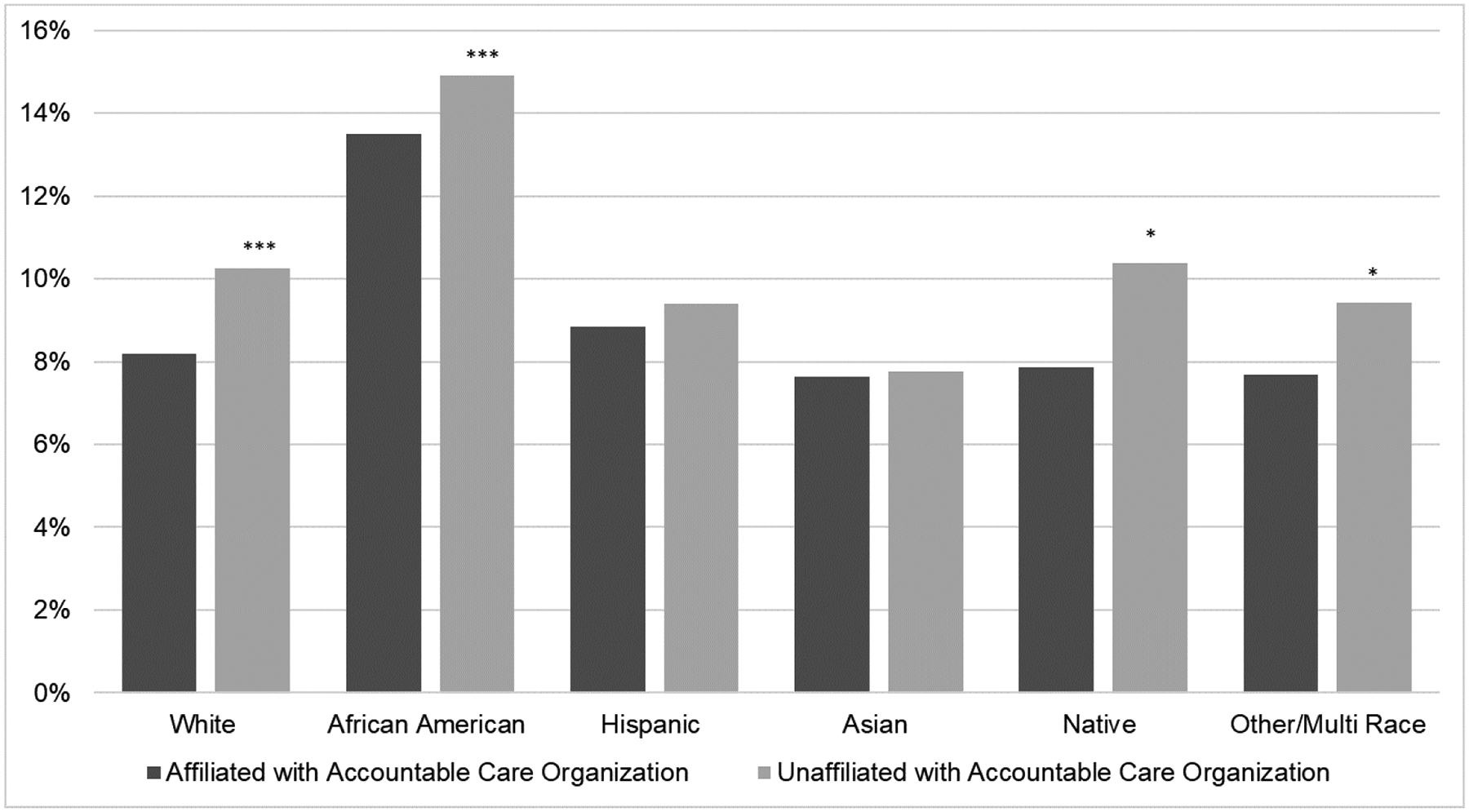
Preventable hospitalization rates among adults with depression by hospital accountable care organization affiliation, 2015.
Note: Total sample (N=400,222) includes discharges for adult adults with depression from 682 hospitals in 11 states (Arizona, Colorado, Florida, Kentucky, Maryland, North Carolina, New Jersey, Oregon, Rhode Island, Washington, and Wisconsin). Potentially preventable hospitalizations were measured using the AHRQ algorithm for any of the following chronic condition Prevention Quality Indicators (PQIs): uncontrolled diabetes (PQI 14), diabetes related short-term and long-term complications (PQI 1, PQI 3); chronic obstructive pulmonary disease or asthma (PQI 5 and PQI 15), hypertension (PQI 7), and heart failure (PQI 8). Statistical significance (***p<0.001; **p<0.01; *p<0.05) between hospital ACO affiliation by race.
Sources: 2015 HCUP SID, 2015 AHA annual survey; and the 2015 AHA Care Systems and Payment Survey.
AHRQ, Agency for Healthcare Research and Quality; HCUP, Healthcare Cost and Utilization Project; SID, State Inpatient Databases; AHA, American Hospital Association.
Regression results showed that ACO-affiliated hospitals had lower odds of PPH (OR=0.89, 95% CI=0.86, 0.91) compared with ACO-unaffiliated hospitals (Table 1). The odds of a PPH were greater for African American (OR=1.60, 95% CI=1.55, 1.66) and Hispanic (OR=1.11, 95% CI=1.06, 1.16) patients with depression compared with their white counterparts. Greater odds of a PPH were observed in patients who were aged 18–24 years, female, had multiple chronic conditions, had government or no insurance, and with ZIP codes with a median income <$44,000 in for-profit, small, rural, non-teaching hospitals. Compared with Florida, Rhode Island and New Jersey were the only states that had significantly greater odds of a PPH, whereas Arizona, Colorado, North Carolina, Oregon, Washington, and Wisconsin had significantly lower odds of a PPH.
Table 1.
Adjusted Odds of Potentially Preventable Hospitalizations With Co-Existing Depression by Hospital ACO Affiliation, 2015
| Variable | OR (95% CI) |
|---|---|
| Hospital affiliation | |
| ACO-unaffiliated | ref |
| ACO-affiliated | 0.89 (0.87, 0.91) |
| Individual characteristics | |
| Race/Ethnicity | |
| NH white | ref |
| NH African American | 1.60 (1.55, 1.66) |
| NH Asian or Pacific Islander | 1.10 (0.96, 1.26) |
| NH Native American | 0.95 (0.84, 1.08) |
| NH other/multi-race | 1.12 (1.00, 1.25) |
| Hispanic (any race) | 1.11 (1.06, 1.16) |
| Age, years | |
| 18–24 | ref |
| 25–34 | 0.60 (0.56, 0.65) |
| 35–44 | 0.68 (0.63, 0.73) |
| 45–54 | 0.85 (0.80, 0.91) |
| 55–64 | 0.89 (0.83, 0.95) |
| 65–74 | 0.85 (0.80, 0.92) |
| ≥75 | 0.91 (0.85, 0.98) |
| Sex | |
| Male | ref |
| Female | 1.10 (1.08, 1.13) |
| Chronic conditions | 1.16 (1.16, 1.17) |
| Payer | |
| Medicare | ref |
| Medicaid | 1.06 (1.02, 1.09) |
| Private insurance | 0.68 (0.66, 0.70) |
| Self-pay | 1.22 (1.15, 1.30) |
| No charge | 1.09 (0.95, 1.26) |
| Other | 0.71 (0.66, 0.76) |
| Median income of ZIP code | |
| $1-$41,999 | ref |
| $42,000-$51,999 | 0.93 (0.90, 0.96) |
| $52,000-$67,999 | 0.87 (0.85, 0.90) |
| ≥$68,000 | 0.78 (0.75, 0.81) |
| 4th quarter discharge | 1.12 (1.09, 1.15) |
| Hospital characteristics | |
| Hospital ownership | |
| For-profit | ref |
| Non-for-profit | 0.91 (0.87, 0.94) |
| Government | 0.91 (0.87, 0.96) |
| Bed size | |
| Small ≤50 | ref |
| Medium 51–200 | 0.78 (0.73, 0.83) |
| Large >200 | 0.61 (0.58, 0.65) |
| Teaching status | |
| Non-teaching | ref |
| Teaching | 0.76 (0.74, 0.79) |
| Safety net provider | |
| No | ref |
| Yes | 0.98 (0.94, 1.01) |
| Geography | |
| Urban | ref |
| Rural | 1.27 (1.22, 1.33) |
| State | |
| Florida | ref |
| Arizona | 0.77 (0.73, 0.81) |
| Colorado | 0.66 (0.62, 0.69) |
| Kentucky | 0.98 (0.94, 1.02) |
| Maryland | 1.00 (0.96, 1.05) |
| North Carolina | 0.95 (0.92, 0.99) |
| New Jersey | 1.35 (1.28, 1.42) |
| Oregon | 0.71 (0.67, 0.74) |
| Rhode Island | 1.37 (1.25, 1.50) |
| Washington | 0.78 (0.74, 0.82) |
| Wisconsin | 0.73 (0.70, 0.77) |
| Constant | 0.07 (0.06, 0.08) |
Notes: Total sample (N=400,222) includes discharges for adult adults with depression from 682 hospitals in 11 states (Florida, Arizona, Colorado, Kentucky, Maryland, North Carolina, New Jersey, Oregon, Rhode Island, Washington, and Wisconsin). Potentially preventable hospitalizations were measured using the AHRQ algorithm for any of the following chronic condition Prevention Quality Indicators (PQIs): uncontrolled diabetes (PQI 14), diabetes related short-term and long-term complications (PQI 1, PQI 3); chronic obstructive pulmonary disease or asthma (PQI 5 and PQI 15), hypertension (PQI 7), and heart failure (PQI 8). The 4th quarter indicator attempts to capture the possible trend shift due to the implementation of ICD10 codes in October 2015. ICD9 codes were used for discharges in quarter 1–quarter 3 and ICD10 for quarter 4 in 2015. Boldface indicates statistical significance (p<0.05).
Sources: 2015 HCUP SID, 2015 AHA annual survey, and the 2015 AHA Care Systems and Payment Survey.
ACO, accountable care organization; NH, Non-Hispanic; AHRQ, Agency for Healthcare Research and Quality; HCUP, Healthcare Cost and Utilization Project; SID, State Inpatient Databases; AHA, American Hospital Association.
After controlling for patient and hospital characteristics, ACO-affiliated hospitals continued to be associated with statistically significantly lower PPH rates for white (OR=0.88, 95% CI=0.85, 0.90), African American (OR=0.88, 95% CI=0.82, 0.94), Native American (OR=0.69, 95% CI=0.51, 0.93), and Hispanic (OR=0.88, 95% CI=0.80, 0.98) patients compared with their counterparts in ACO-unaffiliated hospitals (Table 3). Identifying as other/multi-race was still associated with lower odds of PPH, but this was not statistically significant, and neither were the higher odds in Asian or Pacific Islander patients.
Table 3.
Exposure and Effect of Care Coordination Strategies on Preventable Hospitalizations and Depression in ACOs, 2015
| Variable | All (N=73,690) Mean (SD) | NH white (N=55,148) OR (p-value) | NH African American (N=9,373) OR (p-value) |
|---|---|---|---|
| Total care coordination strategies (0–12) Individual care coordination strategies | 5.84 (3.21) | 1.01 (0.403) | 0.98 (0.089) |
| Hospitalists for medical/surgical inpatients | 0.98 (0.15) | 0.76 (0.008) | 0.72 (0.197) |
| Medication reconciliation as part of an established plan of care | 0.89 (0.31) | 1.02 (0.74) | 0.96 (0.719) |
| Provision of visit summaries to patients as part of all outpatient encounters and scheduling of follow up visit and/or specialty referrals at the time of the initial encounter | 0.56 (0.5) | 1 (0.911) | 0.9 (0.202) |
| Telephonic outreach to discharged patients within 72 hours of discharge | 0.55 (0.5) | 0.99 (0.685) | 0.77 (0.001) |
| Disease management programs for one or more chronic care conditions (e.g., asthma, diabetes, COPD) | 0.46 (0.5) | 1.13 (0.001) | 1.08 (0.369) |
| Chronic care management processes or programs to manage patients with high volume, high cost chronic diseases | 0.43 (0.5) | 1.09 (0.017) | 0.81 (0.01) |
| Post-hospital discharge continuity of care program with scaled intensiveness based upon a severity or risk profile for adult medical-surgical patients in defined diagnostic categories or severity profiles | 0.4 (0.49) | 0.94 (0.116) | 0.78 (0.008) |
| Prospective management of patients at high risk for poor outcomes or extraordinary resource use by experienced case managers | 0.35 (0.48) | 1.08 (0.039) | 1.03 (0.704) |
| Nurse case managers whose primary job is to improve the quality of outpatient care for patients with chronic diseases (e.g., asthma, CHF, depression, diabetes) | 0.33 (0.47) | 0.95 (0.207) | 0.8 (0.004) |
| Assignment of case managers for outpatient follow-up to patients at risk for hospital admission or readmission | 0.32 (0.47) | 1.02 (0.692) | 0.99 (0.93) |
| Arrangement of home visits by physicians, advanced practice nurses, or other professionals for homebound and complex patients for whom office visits constitute a physical hardship | 0.31 (0.46) | 1.03 (0.48) | 1.11 (0.262) |
| Use of predictive analytic tools to identify individual patients at high risk for poor outcomes or extraordinary resource use | 0.27 (0.45) | 1.01 (0.869) | 0.93 (0.411) |
Notes: Total sample (N=73,690) includes discharges for adult adults with depression from 86 hospitals affiliated with an accountable care organization (ACO) in 11 states (Florida, Arizona, Colorado, Kentucky, Maryland, North Carolina, New Jersey, Oregon, Rhode Island, Washington, and Wisconsin). Potentially preventable hospitalizations were measured using the AHRQ algorithm for any of the following chronic condition Prevention Quality Indicators (PQIs) : uncontrolled diabetes (PQI 14), diabetes related short-term and long-term complications (PQI 1, PQI 3); chronic obstructive pulmonary disease or asthma (PQI 5 and PQI 15), hypertension (PQI 7), and heart failure (PQI 8). Comparison group is all other patients. Boldface indicates statistical significance (p<0.05).
Sources: 2015 HCUP SID, 2015 AHA annual survey; and the 2015 AHA Care Systems and Payment Survey.
ACO, accountable care organization; NH, non-Hispanic; COPD, chronic obstructive pulmonary disease; CHF, congestive heart failure; AHRQ, Agency for Healthcare Research and Quality; HCUP, Healthcare Cost and Utilization Project; SID, State Inpatient Databases; AHA, American Hospital Association.
Results of the subsample analysis of CCSs on PPHs by race/ethnicity in ACO-affiliated hospitals are presented in Table 3. Hospitals adopted an average of six CCSs. The two most adopted common strategies were: (1) hospitalists for medical/surgical inpatients and (2) medication reconciliation as part of an established plan of care. The two strategies adopted least were: (1) arrangement of home visits by physicians, advanced practice nurses, or other professionals for homebound and complex patients for whom office visits constitute a physical hardship and (2) use of predictive analytic tools to identify individual patients at high risk for poor outcomes or extraordinary resource use.
The total number of adopted CCSs was not significantly associated with PPH rates for white or African American patients, two major racial groups in the study. However, results varied widely for each CCS. Among white patient groups, lower ORs were observed in hospitals with hospitalists for medical/surgical inpatients (OR=0.76, p=0.008), but higher odds for disease management programs (OR=1.13, p<0.001), chronic care management (OR=1.10, p=0.017), and prospective management of patients at high risk (OR=1.08, p=0.039). Meanwhile, African American patients significantly benefited from four strategies: chronic care management (OR=0.81, p=0.01), post-hospital discharge continuity of care program (OR=0.77, p=0.008), nurse case managers (OR=0.80, p=0.004), and telephonic outreach to discharged patients within 72 hours of discharge (OR=0.77, p=0.001).
DISCUSSION
The results of this study demonstrate that hospital ACO affiliation is associated with a lower rate of PPHs for heart disease, asthma, diabetes, and hypertension among patients with co-existing depression. White, African American, Native American, and Hispanic patients all had lower rates of PPHs in ACO-affiliated hospitals than unaffiliated hospitals. These findings were expected given hospital utilization of CCS and the ACO payment model incentives to improve quality of care and health outcomes.21,39,42 Hence, the study further sought to determine how each CCS made a difference. The outcomes for African American and white patients varied for each of the 12 CCSs examined in ACO-affiliated hospitals. Lower odds of PPH in white patients was only significantly associated with one strategy, whereas three strategies were associated with higher odds of PPH. Meanwhile, lower PPH odds were significantly associated with African American patients in four strategies.
There is no one-size-fits-all solution, but these results suggest that CCSs might work differently across racial groups, thus demonstrating a need for patient-centered design.9,11,31,42 To the authors’ knowledge, this study is the first to show variation in PPHs for chronic conditions with co-existing depression by race/ethnicity across specific CCSs. These findings support other studies demonstrating that patient-centered design and care coordination can effectively improve racial/ethnic disparities in depression treatment9 and hypertension.31 The observed variation could be associated with the historic, systemic, and social barriers that African American patients face around discrimination, access to quality care, trust in the healthcare system, and the cultural stigma around mental illness.9,18,22,53,57 This effect may also be due to ACO patient selection bias and survey response bias, as hospital ACOs are larger and located in higher-income areas than the full study sample.38,58
Results support the ACO payment model as a mechanism to improve the quality of care for adults with comorbid physical and mental conditions.9,31,39,41–43 As more hospitals become ACO-affiliated and specific patient populations are targeted, ACOs should seek out best practices from other ACO-affiliated hospitals, strengthen community partnerships, and include patients from their target population in the design and evaluation of the CCSs employed.16 Additionally, by integrating mental and physical health care, minority patient populations may further benefit from CCSs.21,39,54
Limitations
This study has several limitations. First, this analysis was based on a cross-sectional study design that explores the association between hospital ACO-affiliation and PPHs by race/ethnicity, not the impact of patient affiliation with an ACO. Second, the measure of hospital ACO affiliation was utilized given data availability. It is likely that this measure of ACO-affiliated hospitals contained a mix of patients who were enrolled or not enrolled in the ACOs. Literature on the taxonomy of ACOs has demonstrated that hospital-led ACOs have weaker incentives to prevent hospitalizations as compared with physician- or co-led ACOs59–61; thus, these findings may be conservative. Future studies should explore the effects of ACO affiliation on PPHs in other types of ACOs, utilizing data that can identify patient-level ACO affiliation. Third, the study used administrative data, which are vulnerable to coding errors, have limited patient demographic variables, and limited ability to determine the severity of depression and if CCSs were offered/utilized at the patient level. Despite controlling for hospital and community factors, there is insufficient information on the driving forces that support ACO affiliation or hospital application of CCSs for their patient populations, which may differentially effect PPH rates.62–64 Fourth, these data are not nationally representative, nor generalizable as the availability of race/ethnicity, ZIP code, and linkage files restricted the sample to 11 states.
The subsample analyses among ACO-affiliated hospitals have other limitations. The CCSs were obtained from a supplemental AHA survey. Hospitals that participated in the CCS survey tend to be more well-resourced hospitals,65 which may have a longer history of implementing CCSs.38 Additionally, racial and ethnic minority patients and other underserved populations were less likely to have access to such hospitals.66 Thus, results of the variation of the PPHs by ACO and CCS even among these well-resourced hospitals may be a conservative estimate among minorities. There was limited analytical power to compare other racial/ethnic populations among the 86 ACO-affiliated hospitals. Furthermore, CCSs can depend heavily on hospital/unit-level leadership and other available resources,64 and be implemented differently depending on the needs, risk profile, and patient mix of a given population.67 Given the fragmented nature of mental health care and the poor integration between physical and mental health care, it is not clear whether a different set of CCSs more often employed in the outpatient setting (and thus not currently assessed by the AHA survey instrument) might be more effective in decreasing PPHs among patients experiencing co-occurring physical and mental conditions. These limitations could possibly be explored through an integrated data system with comprehensive measures of all types of healthcare utiliations.68 Data sets with detailed measures of individual socioeconomic characteristics and social determinants of health will be helpful to further investigate racial and ethnic disparities.
CONCLUSIONS
The ACO model incentivizes hospitals to integrate CCSs to improve quality of care. This study found lower odds of PPHs with co-existing depression in ACO-affiliated hospitals compared with ACO-unaffiliated hospitals. This was especially true for white, African American, Native American, and Hispanic patients. Additionally, results showed variation of the adoption of specific CCSs among ACO-affiliated hospitals and that the effectiveness of each CCS varies by patients’ race. These results highlight the importance of tailoring ACOs to fit the needs of specific patient populations and suggest that ACOs could be designed to improve health disparities and support the need to integrate physical and mental health. A common barrier to integration is mental health provider shortages; however, hospitals can leverage community resources and develop cross-sector partnerships to strengthen their care coordination services and focus on care across the continuum. Lastly, these findings may help inform CMS and other payers establish risk adjustment payment algorithms for patient race/ethnicity and SES.
Supplementary Material
Table 2.
Summary of Adjusted Odds of PPH by Hospital ACO Affiliation for Each Race/Ethnicity, 2015
| Race/Ethnicity | Count, N | OR (95% CI |
|---|---|---|
| NH white | 320,665 | 0.88 (0.85, 0.90) |
| NH African American | 43,733 | 0.88 (0.82, 0.94) |
| NH Asian or Pacific Islander | 2,983 | 1.22 (0.85, 1.79) |
| NH Native American | 3,087 | 0.69 (0.51, 0.93) |
| NH other/multi-race | 4,015 | 0.81 (0.61, 1.06) |
| Hispanic (any race) | 25,739 | 0.88 (0.8, 0.98) |
Notes: Total sample (N=400,222) includes discharges for adult adults with depression from 682 hospitals in 11 states (Florida, Arizona, Colorado, Kentucky, Maryland, North Carolina, New Jersey, Oregon, Rhode Island, Washington, and Wisconsin). Potentially preventable hospitalizations were measured using the AHRQ algorithm for any of the following chronic condition Prevention Quality Indicators (PQIs): uncontrolled diabetes (PQI 14), diabetes related short-term and long-term complications (PQI 1, PQI 3); chronic obstructive pulmonary disease or asthma (PQI 5 and PQI 15), hypertension (PQI 7), and heart failure (PQI 8). Comparison group per row is the patient population in ACO-unaffiliated hospitals. Boldface indicates statistical significance (p<0.05). Contact the author for full results by race.
Sources: 2015 HCUP SID, 2015 AHA annual survey; and the 2015 AHA Care Systems and Payment Survey.
PPH, potentially preventable hospitalization; ACO, accountable care organization; NH, non-Hispanic; AHRQ, Agency for Healthcare Research and Quality; HCUP, Healthcare Cost and Utilization Project; SID, State Inpatient Databases; AHA, American Hospital Association.
ACKNOWLEDGMENTS
This research was supported by NIH, National Institute on Minority Health and Health Disparities, Grant R01MD011523; National Institute on Aging, Grant R56AG062315; and National Institute on Minority Health and Health Disparities, Grant R01MD011523-03S1 awarded to Jie Chen. Funding is also award to Deanna Barath from the Robert Wood Johnson Foundation’s Health Policy Research Scholars program. None of the funding bodies played a role in the design of the study; data collection, analysis, or interpretation; manuscript writing; or the decision to submit this manuscript for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
No financial disclosures were reported by the authors of this paper.
REFERENCES
- 1.Bodenheimer T, Wang MC, Rundall TG, et al. What are the facilitators and barriers in physician organizations’ use of care management processes? Jt Comm J Qual Saf. 2004;30(9):505–514. 10.1016/s1549-3741(04)30059-6. [DOI] [PubMed] [Google Scholar]
- 2.Li Y, Glance LG, Cai X, Mukamel DB. Mental illness and hospitalization for ambulatory care sensitive medical conditions. Med Care. 2008;46(12):1249–1256. 10.1097/mlr.0b013e31817e188c. [DOI] [PubMed] [Google Scholar]
- 3.Goodell S, Druss B, Walker E. Mental Disorders and Medical Comorbidity. The Synthesis Project Princeton, NJ: The Robert Wood Johnson Foundation; 2011. [PubMed] [Google Scholar]
- 4.Rugulies R Depression as a predictor for coronary heart disease: a review and meta-analysis. Am J Prev Med. 2002;23(1):51–61. 10.1016/s0749-3797(02)00439-7. [DOI] [PubMed] [Google Scholar]
- 5.Han YY, Forno E, Marsland AL, Miller GE, Celedon JC. Depression, asthma, and bronchodilator response in a nationwide study of US adults. J Allergy Clin Immunol Pract. 2016;4(1):68–73.e1. 10.1016/j.jaip.2015.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cook BL, McGuire T, Miranda J. Measuring trends in mental health care disparities, 2000–2004. Psychiatr Serv. 2007;58(12):1533–1540. 10.1176/ps.2007.58.12.1533. [DOI] [PubMed] [Google Scholar]
- 7.Walker ER, McGee RE, Druss BG. Mortality in mental disorders and global disease burden implications: a systematic review and meta-analysis. JAMA Psychiatry. 2015;72(4):334–341. 10.1001/jamapsychiatry.2014.2502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.de Oliveira C, Cheng J, Vigod S, Rehm J, Kurdyak P. Patients with high mental health costs incur over 30 percent more costs than other high-cost patients. Health Aff (Millwood). 2016;35(1):36–43. 10.1377/hlthaff.2015.0278. [DOI] [PubMed] [Google Scholar]
- 9.Angstman KB, Phelan S, Myszkowski MR, et al. Minority primary care patients with depression: outcome disparities improve with collaborative care management. Med Care. 2015;53(1):32–37. 10.1097/mlr.0000000000000280. [DOI] [PubMed] [Google Scholar]
- 10.Horvitz-Lennon M, Kilbourne AM, Pincus HA. From silos to bridges: meeting the general health care needs of adults with severe mental illnesses. Health Aff (Millwood). 2006;25(3):659–669. 10.1377/hlthaff.25.3.659. [DOI] [PubMed] [Google Scholar]
- 11.Adams AS, Soumerai SB, Zhang F, et al. Effects of eliminating drug caps on racial differences in antidepressant use among dual enrollees with diabetes and depression. Clin Ther. 2015;37(3):597–609. 10.1016/j.clinthera.2014.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Alegria M, Chatterji P, Wells K, et al. Disparity in depression treatment among racial and ethnic minority populations in the United States. Psychiatr Serv. 2008;59(11):1264–1272. 10.1176/ps.2008.59.11.1264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.O’Neil SS, Lake T, Merrill A, Wilson A, Mann DA, Bartnyska LM. Racial disparities in hospitalizations for ambulatory care-sensitive conditions. Am J Prev Med. 2010;38(4):381–388. 10.1016/j.amepre.2009.12.026. [DOI] [PubMed] [Google Scholar]
- 14.Institute of Medicine, Board on Health Sciences Policy, Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care. Unequal treatment: Confronting racial and ethnic disparities in health care. Washington, DC: National Academies Press; 2003. 10.17226/10260. [DOI] [PubMed] [Google Scholar]
- 15.Sorkin DH, Ngo-Metzger Q, De Alba I. Racial/ethnic discrimination in health care: impact on perceived quality of care. J Gen Intern Med. 2010;25(5):390–396. 10.1007/s11606-010-1257-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chen J, Mortensen K, Bloodworth R. Exploring contextual factors and patient activation: evidence from a nationally representative sample of patients with depression. Health Educ Behav. 2014;41(6):614–624. 10.1177/1090198114531781. [DOI] [PubMed] [Google Scholar]
- 17.Puckrein GA, Egan BM, Howard G. Social and medical determinants of cardiometabolic health: the big picture. Ethn Dis. 2015;25(4):521–524. 10.18865/ed.25.4.521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Agyemang AA, Mezuk B, Perrin P, Rybarczyk B. Quality of depression treatment in black Americans with major depression and comorbid medical illness. Gen Hosp Psychiatry. 2014;36(4):431–436. 10.1016/j.genhosppsych.2014.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Geronimus AT, Hicken M, Keene D, Bound J. “Weathering” and age patterns of allostatic load scores among blacks and whites in the United States. Am J Public Health. 2006;96(5):826–833. 10.2105/ajph.2004.060749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pezzin LE, Bogner HR, Kurichi JE, et al. Preventable hospitalizations, barriers to care, and disability. Medicine (Baltimore). 2018;97(19):e0691 10.1097/md.0000000000010691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fullerton CA, Henke RM, Crable EL, Hohlbauch A, Cummings N. The impact of Medicare ACOs on improving integration and coordination of physical and behavioral health care. Health Aff (Millwood). 2016;35(7):1257–1265. 10.1377/hlthaff.2016.0019. [DOI] [PubMed] [Google Scholar]
- 22.Cook BL, Doksum T, Chen C-N, Carle A, Alegría M. The role of provider supply and organization in reducing racial/ethnic disparities in mental health care in the U.S. Soc Sci Med. 2013;84:102–109. 10.1016/j.socscimed.2013.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cook BL, Zuvekas SH, Chen J, Progovac A, Lincoln AK. Assessing the individual, neighborhood, and policy predictors of disparities in mental health care. Med Care Res Rev. 2017;74(4):404–430. 10.1177/1077558716646898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nadeem E, Lange JM, Edge D, Fongwa M, Belin T, Miranda J. Does stigma keep poor young immigrant and U.S.-born black and Latina women from seeking mental health care? Psychiatr Serv. 2007;58(12):1547–1554. 10.1176/ps.2007.58.12.1547. [DOI] [PubMed] [Google Scholar]
- 25.Gary FA. Stigma: barrier to mental health care among ethnic minorities. Issues Ment Health Nurs. 2005;26(10):979–999. 10.1080/01612840500280638. [DOI] [PubMed] [Google Scholar]
- 26.Brandon DT, Isaac LA, LaVeist TA. The legacy of Tuskegee and trust in medical care: is Tuskegee responsible for race differences in mistrust of medical care? J Natl Med Assoc. 2005;97(7):951–956. [PMC free article] [PubMed] [Google Scholar]
- 27.Thornicroft G. Stigma and discrimination limit access to mental health care. Epidemiol Psychiatr Sci. 2008;17(1):14–19. . [DOI] [PubMed] [Google Scholar]
- 28.Canales MK, Weiner D, Samos M, Wampler NS. Multi-generational perspectives on health, cancer, and biomedicine: Northeastern Native American perspectives shaped by mistrust. J Health Care Poor Underserved. 2011;22(3):894–911. 10.1353/hpu.2011.0096. [DOI] [PubMed] [Google Scholar]
- 29.Henderson RC, Williams P, Gabbidon J, et al. Mistrust of mental health services: ethnicity, hospital admission and unfair treatment. Epidemiol Psychiatr Sci. 2015;24(3):258–265. 10.1017/s2045796014000158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kim PY, Kendall DL, Cheon HS. Racial microaggressions, cultural mistrust, and mental health outcomes among Asian American college students. Am J Orthopsychiatry. 2017;87(6):663–670. 10.1037/ort0000203. [DOI] [PubMed] [Google Scholar]
- 31.Bartolome RE, Chen A, Handler J, Platt ST, Gould B. Population care management and team-based approach to reduce racial disparities among African Americans/blacks with hypertension. Perm J. 2016;20(1):53–59. 10.7812/tpp/15-052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Garrison GM, Angstman KB, O’Connor SS, Williams MD, Lineberry TW. Time to remission for depression with collaborative care management (CCM) in primary care. J Am Board Fam Med. 2016;29(1):10–17. 10.3122/jabfm.2016.01.150128. [DOI] [PubMed] [Google Scholar]
- 33.Weech-Maldonado R, Elliott M, Pradhan R, Schiller C, Hall A, Hays RD. Can hospital cultural competency reduce disparities in patient experiences with care? Med Care. 2012;50(suppl):S48–S55. 10.1097/mlr.0b013e3182610ad1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Burwell SM. Setting value-based payment goals--HHS efforts to improve U.S. health care. New Engl J Med. 2015;372(10):897–899. 10.1056/nejmp1500445. [DOI] [PubMed] [Google Scholar]
- 35.Burns LR, Pauly MV. Accountable care organizations may have difficulty avoiding the failures of integrated delivery networks of the 1990s. Health Aff (Millwood). 2012;31(11):2407–2416. 10.1377/hlthaff.2011.0675. [DOI] [PubMed] [Google Scholar]
- 36.Benjenk I, Chen J. Managed Care and Aging In: Gu D, Dupre ME, eds. Encyclopedia of Gerontology and Population Aging. Cham: Springer International Publishing; 2019:1–5. 10.1007/978-3-319-69892-2_992-1. [DOI] [Google Scholar]
- 37.Lewis VA, Colla CH, Tierney K, Van Citters AD, Fisher ES, Meara E. Few ACOs pursue innovative models that integrate care for mental illness and substance abuse with primary care. Health Aff (Millwood). 2014;33(10):1808–1816. 10.1377/hlthaff.2014.0353. [DOI] [PubMed] [Google Scholar]
- 38.Anderson AC, Chen J. ACO Affiliated hospitals increase implementation of care coordination strategies. Med Care. 2019;57(4):300–304. 10.1097/mlr.0000000000001080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Counts NZ, Wrenn G, Muhlestein D. Accountable care organizations’ performance in depression: lessons for value-based payment and behavioral health. J Gen Intern Med. 2019;34:2898–2900. 10.1007/s11606-019-05047-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Busch AB, Huskamp HA, McWilliams JM. Early efforts By Medicare accountable care organizations have limited effect on mental illness care and management. Health Aff (Millwood). 2016;35(7):1247–1256. 10.1377/hlthaff.2015.1669. [DOI] [PubMed] [Google Scholar]
- 41.Chukmaitov A, Harless DW, Bazzoli GJ, Muhlestein DB. Preventable hospital admissions and 30-day all-cause readmissions: does hospital participation in accountable care organizations improve quality of care? Am J Med Qual. 2019;34(1):14–22. 10.1177/1062860618778786. [DOI] [PubMed] [Google Scholar]
- 42.Ivey SL, Shortell SM, Rodriguez HP, Wang YE. Patient engagement in ACO practices and patient-reported outcomes among adults with co-occurring chronic disease and mental health conditions. Med Care. 2018;56(7):551–556. 10.1097/mlr.0000000000000927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kaufman BG, Spivack BS, Stearns SC, Song PH, O’Brien EC. Impact of accountable care organizations on utilization, care, and outcomes: a systematic review. Med Care Res Rev. 2019;76(3):255–290. 10.1177/1077558717745916. [DOI] [PubMed] [Google Scholar]
- 44.Lewis VA, Fraze T, Fisher ES, Shortell SM, Colla CH. ACOs serving high proportions of racial and ethnic minorities lag in quality performance. Health Aff (Millwood). 2017;36(1):57–66. 10.1377/hlthaff.2016.0626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hartzman A, Rhodes K. Accountable care organizations and disparities. Health Aff (Millwood). 2017;36(5):960 10.1377/hlthaff.2017.0236. [DOI] [PubMed] [Google Scholar]
- 46.Lewis VA, Fisher ES, Colla CH. ACOs and disparities: the authors reply. Health Aff (Millwood). 2017;36(5):960 10.1377/hlthaff.2017.0237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Healthcare Cost and Utilization Project (HCUP). Rockville, MD: Agency for Healthcare Research and Quality; 2015. [PubMed] [Google Scholar]
- 48.American Hospital Association. AHA Annual Survey. Published 2015.
- 49.American Hospital Association. AHA Survey of Care Systems and Payment. Published 2015.
- 50.Centers for Medicare and Medicaid Services. CCW Chronic Condition Algorithms. Chronic Conditions Data Warehouse; Published 2019. [Google Scholar]
- 51.Agency for Healthcare Research and Quality. Prevention Quality Indicators Technical Specifications Updates. Published 2018.
- 52.Centers for Medicare & Medicaid Services. 2015 Annual Reporting on the Quality of Care for Adults in Medicaid Medicaid Quality Measurement Program. Adult Health Care Quality Measures Washington, DC: Centers for Medicare & Medicaid Services; 2019. [Google Scholar]
- 53.Nuru-Jeter AM, Michaels EK, Thomas MD, Reeves AN, Thorpe RJ Jr., LaVeist TA. Relative roles of race versus socioeconomic position in studies of health inequalities: a matter of interpretation. Annu Rev Public Health. 2018;39:169–188. 10.1146/annurev-publhealth-040617-014230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Maust DT, Oslin DW, Marcus SC. Mental health care in the accountable care organization. Psychiatr Serv. 2013;64(9):908–910. 10.1176/appi.ps.201200330. [DOI] [PubMed] [Google Scholar]
- 55.McDowell MJ, Busch AB, Sen AP, et al. Participation in accountable care organizations among hospitals offering substance use disorder and mental health services. Psychiatr Serv. 2018;69(11):1131–1134. 10.1176/appi.ps.201800248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43(11):1130–1139. 10.1097/01.mlr.0000182534.19832.83. [DOI] [PubMed] [Google Scholar]
- 57.Fiscella K, Sanders MR. Racial and ethnic disparities in the quality of health care. Annu Rev Public Health. 2016;37:375–394. 10.1146/annurev-publhealth-032315-021439. [DOI] [PubMed] [Google Scholar]
- 58.Colla CH, Lewis VA, Tierney E, Muhlestein DB. Hospitals participating in ACOs tend to be large and urban, allowing access to capital and data. Health Aff (Millwood). 2016;35(3):431–439. 10.1377/hlthaff.2015.0919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Bleser WK, Muhlestein D, Saunders RS, McClellan MB. Half a decade in, Medicare accountable care organizations are generating net savings: part 1. Health Affairs Blog. September 20, 2018. [Google Scholar]
- 60.Bleser WK, Saunders RS, Muhlestein DB, McClellan M. Why do accountable care organizations leave the Medicare shared savings program? Health Aff (Millwood). 2019;38(5):794–803. 10.1377/hlthaff.2018.05097. [DOI] [PubMed] [Google Scholar]
- 61.Zhang H, Cowling DW, Graham JM, Taylor E. Five-year impact of a commercial accountable care organization on health care spending, utilization, and quality of care. Med Care. 2019;57(11):845–854. 10.1097/mlr.0000000000001179. [DOI] [PubMed] [Google Scholar]
- 62.Bazzoli GJ, Harless DW, Chukmaitov AS. A taxonomy of hospitals participating in Medicare accountable care organizations. Health Care Manage Rev. 2019;44(2):93–103. 10.1097/hmr.0000000000000159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Shortell SM, Wu FM, Lewis VA, Colla CH, Fisher ES. A taxonomy of accountable care organizations for policy and practice. Health Serv Res. 2014;49(6):1883–1899. 10.1111/1475-6773.12234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Lewis VA, D’Aunno T, Murray GF, Shortell SM, Colla CH. The hidden roles that management partners play in accountable care organizations. Health Aff (Millwood). 2018;37(2):292–298. 10.1377/hlthaff.2017.1025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Benjenk I, Franzini L, Chen J. Evidence of the linkage between hospital-based care coordination strategies and hospital overall (star) ratings. Med Care. 2020;58(1):18–26. 10.1097/mlr.0000000000001226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Chen J, DuGoff EH, Novak P, Wang MQ. Variation of hospital-based adoption of care coordination services by community-level social determinants of health. Health Care Manage Rev. In press. Online November 27, 2018 10.1097/hmr.0000000000000232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Ouayogode MH, Mainor AJ, Meara E, Bynum JPW, Colla CH. Association between care management and outcomes among patients with complex needs in Medicare accountable care organizations. JAMA Netw Open. 2019;2:e196939 10.1001/jamanetworkopen.2019.6939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.CMS Office of Minority Health. Part C and D Performance Data Stratified by Race, Ethnicity, and Gender. Baltimore, MD: U.S. Centers for Medicare & Medicaid Services; 2019. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


