Supplemental Digital Content is available in the text
Keywords: alcohol, IDU, India, Men who have Sex with Men, MSM, oral drug, substance-use
Abstract
HIV prevalence is higher among Men who have Sex with Men (MSM), owing to their unsafe sexual behavior. Further, MSM indulge in behaviors such as consumption of alcohol/oral drugs and/or injecting during/before sex that poses the risk of unsafe behaviors, thereby increasing their vulnerability to HIV. The study aims to analyze the factors associated with HIV infection among the multi-risk MSM using any substances with those MSM who do not use substances.
Community-based cross-sectional survey design using probability-based sampling between October 2014 and November 2015.
For the nation-wide Integrated Biological and Behavioral Surveillance (IBBS), 23,081 MSM were recruited from 4067 hotspots in 108 districts across India. Information on demographics, sexual behaviors, substance use, sexual partners, and awareness on HIV and its management was collected from the consented respondents using computer-assisted personal interview (CAPI) by trained personnel. Blood samples were tested for HIV. Statistical analyses were done, to study the associations between substance use and its influence on high-risk sexual behaviors and HIV infection.
One in 3 MSM (33.88%) in India were substance users, thus exhibiting “multi-risk” (MR) behaviors. Significantly higher HIV prevalence (3.8%, P < .05) was reported among MR-MSM, despite 97.2% of them being aware of HIV. Higher HIV prevalence among MSM exhibiting homosexual behavior for ≤1 year is of specific concern, as this accounts to recent infections and indicates the increased vulnerability of the infection among the new entrants.
Substance-use resulting in high-risk sexual behavior was significantly associated with higher HIV prevalence among MR-MSM. Integrated targeted interventions focusing on safe sex and safe-IDU practices among MR-MSM are required to end the disease transmission.
1. Introduction
The national AIDS control organization (NACO) of India strives towards “AIDS-free India” through strategic HIV interventions. Female sex workers (FSW) Men who have Sex with Men (MSM), transgender (TG), and Injecting Drug Users (IDU) are the high-risk groups (HRGs) of HIV transmission in India.[1] Several interventions at national, state, and district levels including targeted interventions (TI) were formulated by NACO and implemented with the help of respective state AIDS control societies (SACS) to prevent HIV transmission among the HRGs, so as to control and halt HIV transmission among the general population. To evaluate the outcomes of the interventions, the Integrated Biological and Behavioral Surveillance (IBBS), the largest nationwide large-scale community-based bio-behavioral surveillance, was conducted among HRGs in 2014 to 2015.[2] Within the HRGs in India, HIV prevalence is generally high among FSW and MSM. In India, the prevalence of HIV among MSM in 2017 was 4.3%. MSM are most vulnerable to HIV infection via unprotected anal sex,[2,3] which explains high HIV prevalence among MSM. Apart from unsafe sexual behaviors, MSM are often indulged in other risk behaviors such as alcohol consumption and drug use that increases their risk of infection.
NACO estimates that out of the 2.1 million PLHIV in India, more than 50% were males, a considerable proportion of which are MSM.[1] Sexual behaviors of MSM, are highly indefinite. Having multiple sexual partners and indulgence in unprotected intercourse, are some of the high-risk sexual behaviors that increase the transmission risks.[4–6] In India, almost 50% percent of MSM are bisexuals, meaning they have both male and female partners, thus acting as a potential bridge population of HIV transmission to the general population.[7,8] High-risk sexual behaviors such as inconsistent condom-use during sex across different types of sex partners, social, and psychological risk behaviors such as injecting drug use for non-medical purposes, and alcohol use during or before sex seem to have a significant association with HIV infection among MSM.[9–12] Previous reports suggest substance-use to be highly associated with sexual risk behaviors such as unprotected sex, particularly insertive sex. In a study conducted by Purcell et al, the association between substance use and HIV transmission risk of HIV Positive MSM was analyzed. It was found that HIV positive MSM consumers of certain drugs were less likely to use condoms with HIV-negative or unknown status partners.[13] To understand the behavioral effects of substance use among MSM, we have compared the sexual behaviors and HIV prevalence among MSM with at least 1 substance-use practice with that of the MSM who do not use any substance such as alcohol or drug. Analyzing the effects of substance use among MSM on their sexual behaviors and HIV prevalence is essential to identify the lacunae in the current interventions and to improve them further.
2. Methods
2.1. Study population
The study participants were exclusively MSM. The inclusion criteria were being male, aged 15 years or more, who had anal, or oral sex with a male/hijra partner in the last month. A total of 23,081 MSM from 73 sampling domains or study sites across 108 districts, in 28 Indian States and Union Territories were enrolled between October 2014 and November 2015.
2.2. Study methodology
IBBS followed a community based cross-sectional survey design using the probability-based sampling method in all study sites. Socio-demographic profiles; behavioral information on number and type of sex partners and consistent condom use with different types of sex partners, HIV awareness and substance use were collected and biological variables of HIV/STI were studied. Blood samples, collected using Dried Blood Spot (DBS) method, were tested for HIV biomarkers. To identify the multi-risk behaviors of substance use among MSM, 3 specific questions were included in the questionnaire, namely,
-
1.
Have you injected drugs for non-medical reasons in the last 3 months?
-
2.
Have you consumed drugs such as Ganja (Cannabis), Heroin for pleasure in the last 12 months?
-
3.
Did you consume alcohol when you had last sex with any of your sexual partners?
Study sites are continuous geographical units for which the bio-behavioral estimates are generated. These sites were selected based on available MSM population size in a particular state and were designated as priority sites for MSM targeted intervention programs by NACO. The target sample size per sampling domain or study site was 400; however, the achieved sample size was lesser at few sites either due to the unavailability of MSM or higher refusal rates. For each study site, the survey was conducted for 3 months anytime between October 2014 and November 2015. Survey methodology, field monitoring, and supportive supervision mechanism during data collection, ethical considerations including the informed consent process, weighting procedure, laboratory methods, etc. were followed as described elsewhere.[2]
2.3. Statistical analysis
Based on substance use, the MSM were categorized as multi-risk MSM (MR-MSM) (substance users) and MSM (substance non-users). The proportions and HIV prevalence were calculated as unweighted ones for the actual MSM sample size and are presented according to their status of substance use. Risk factors associated with HIV infection between the 2 sub-categories of MSM were compared by the Chi-Squared test. Independent risk factors significantly influencing the risk of HIV infection among the MR-MSM were determined by bivariate analysis using the logistic regression method. Variables in bivariate analysis, that were marginally significant with P < .20, were selected for multivariable analysis. IBM SPSS version 26.0[14] was used for all statistical analyses.
2.4. Ethics review and informed consent
The present study, which involves the secondary analyses of the data collected during the national IBBS, 2015, was approved by the Institutional Ethics Committee. During IBBS, a process of written informed consent was employed and all the participants were given simple and clear information regarding the risks and benefits of participating in the national IBBS through informed consent form (ICF).
3. Results
3.1. The pattern of multi-risk behaviors among MSM
The key socio-demographic profiles and other characteristics of MR-MSM and MSM are listed in Table 1. Overall, 34% of the enrolled MSM were substance users (IDU for non-medical purposes or consumers of oral drug or alcohol or combination users).
Table 1.
Demographic profile and HIV prevalence of MR-MSM and MSM: IBBS 2014-15.
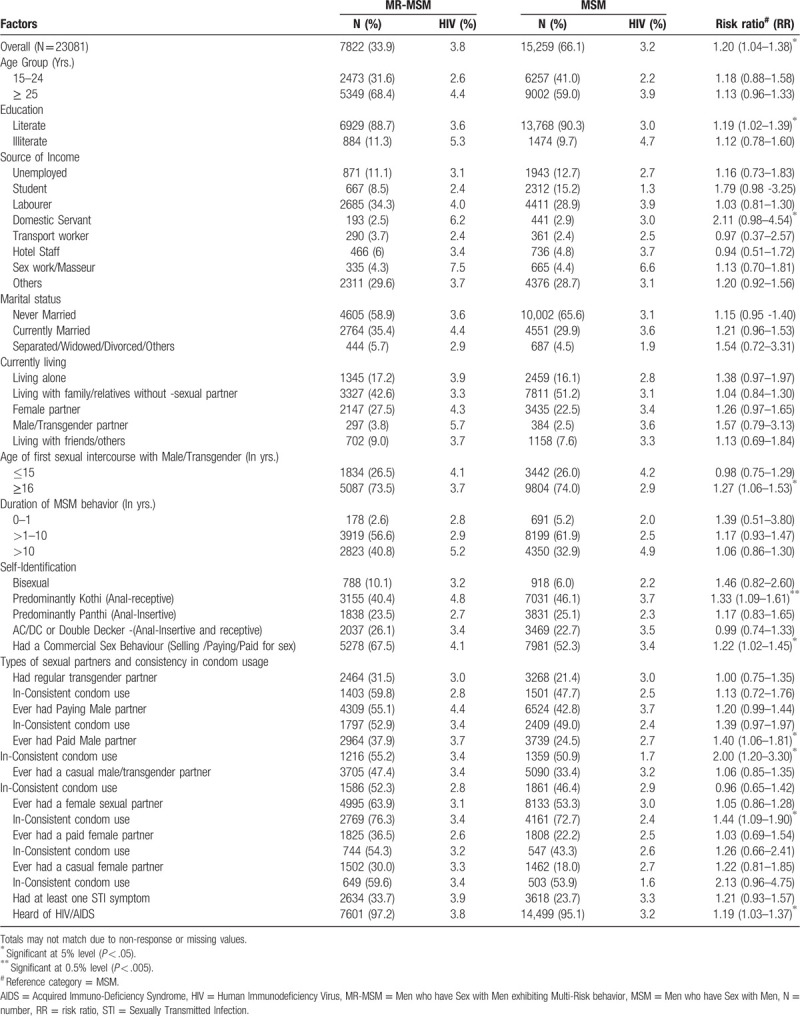
About 51.3% of MSM were alcohol consumers of which 56.2% consumed alcohol during or before sex. Moreover, 2.5% of the MSM were IDUs of which 40.8% shared their needles/syringes. Nearly 6.7% of the MSM reported that they consumed oral drugs and 1.4% were combination users of all 3.[15] In our study, we have categorized only those MSM as multi-risk MSM (MR-MSM) who consumed alcohol specifically during or before sex, who consumed oral drugs such as Heroin or Ganja (Cannabis) and who reported injecting drug use. Within the MR-MSM, 67.7% only consumed alcohol during or before sex, 8.3% were consumers of oral drugs alone and 2.9% were IDU only. On the other hand, 12.6% were both alcohol consumers during and before sex and consumers of oral drugs, 1.7% were consumers of oral/injecting drugs, 2.3% were alcohol consumers during and before sex and consumers of injecting drugs and 4.6% were users of all 3 substances (Fig. 1).
Figure 1.
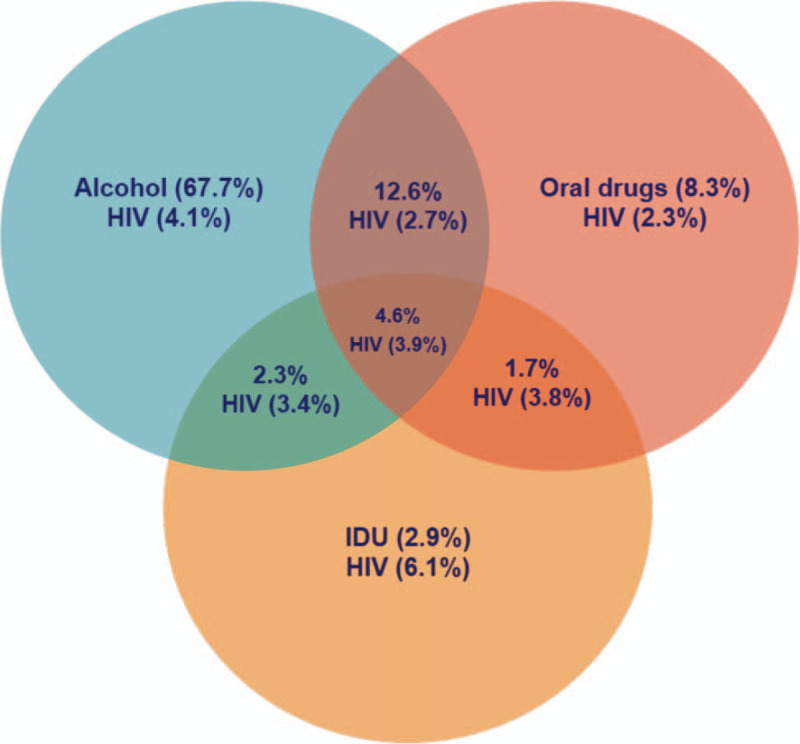
Schematic representation of multi-risk behavior patterns and the corresponding HIV prevalence within the MR-MSM.
3.2. Distribution of MR-MSM and MSM based on their demographics and sexual behaviors
Within the MR-MSM, a larger proportion was over 25 years of age (68.4%), literates (88.7%), laborers (34.3%), never married (58.9%), and were living with the family without a sexual partner (42.6%). About 26.5% of the MSM had their first MSM sexual activity within 15 years of age while the new entrants (duration of MSM behavior ≤ 1 year) accounted for about 2.6%. Around 40.4% of the MSM were predominantly Kothis while 67.5% of the MR-MSM involved in commercial sex. Similar patterns were reflected in the substance non-users MSM group. Nevertheless, compared to that of MSM, the proportion of MR-MSM who were above 25 years (68.4 vs 59.0), illiterates (11.3 vs 9.7), laborers (34.3 vs 28.9) or transport workers (3.7 vs 2.4) or hotel staff (6.0 vs 4.8) were higher. Likewise, the proportion of married MR-MSM (35.4 vs 29.9) and those living with a female partner (27.5% vs 22.5%) was higher than that of the MSM. The proportion of men exhibiting MSM behavior over 10 years was comparatively higher among MR-MSM than MSM (40.8% vs 32.9%).
Similarly, the proportion involved in commercial sex behavior was higher among MR-MSM and were less likely to be consistent in their condom usage than MSM. Specifically, MSM who do not use substances were less likely to have casual or paid female partners. Nevertheless, the inconsistent condom usage was invariably higher with regular female partners among both MR-MSM and MSM. A higher proportion of MR-MSM was symptomatic of any STIs (33.7 vs 23.7), while the awareness of the term HIV was above 95% in both categories.
3.3. HIV Prevalence
HIV prevalence based on the demographics and the sexual behavior of MR-MSM and MSM and their risk ratio is presented in Table 1. HIV prevalence among MR-MSM was 3.8%, which was 17 times higher than that of the general population.[15–17] Overall, HIV prevalence among MR-MSM was significantly higher when compared to MSM (3.8% vs 3.2%, P < .05) and in particular, MR-MSM were 1.2 times at a higher risk of acquiring the infection than the MSM. Risk-specific HIV prevalence within the MR-MSM shows the highest prevalence among IDU-MSM (6.1%), followed by consumers of alcohol before or during sex (4.1%) (Fig. 1).
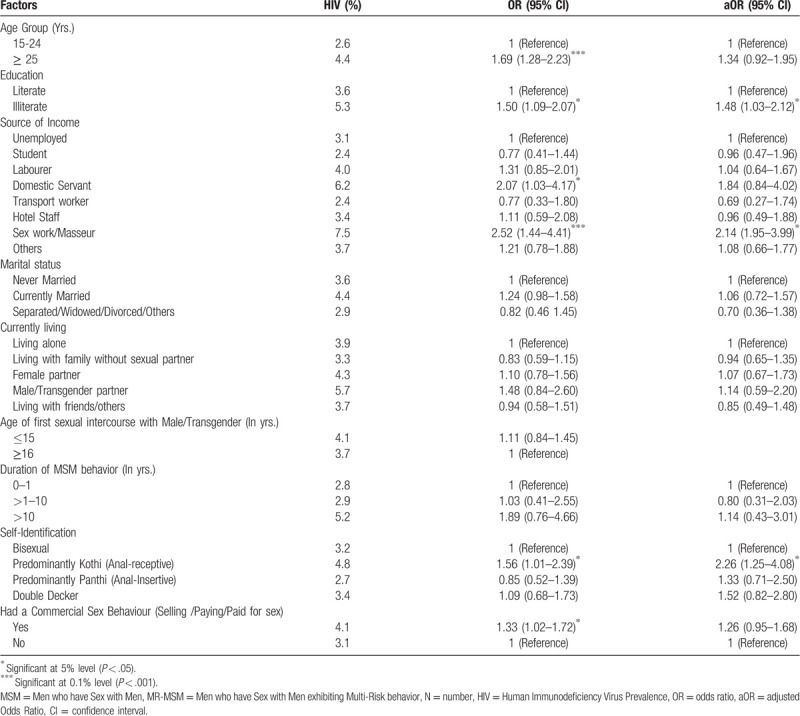
MR-MSM who were literates, were or domestic servants, have had their first sexual intercourse with a male/TG partner, self-identified themselves as predominantly Kothi, had commercial sex behavior, who had regular/paid male sexual partners and who had inconsistent condom usage with their regular female partner had a significantly higher prevalence of HIV. Therefore, factors significantly associated with a higher risk of HIV infection among MR-MSM were education, source of income, sexual identity, commercial sexual behavior, type of sexual partner, and inconsistent condom usage (Table 1). The independent risk factors associated with HIV infection among the MR-MSM identified by the logistic regression method are presented in Table 2. Factors significantly associated with HIV infection were identified as age, education, source of income, marital status, sexual identity, commercial sex behavior, and paying male sexual partner. The multivariable analysis revealed illiterate MR-MSM were more likely to be infected by HIV than the literates (aOR 1.48, 95% CI: 1.03–2.12, P = .036). Likewise, self-identified Kothi behavior (aOR 2.26, 95% CI: 1.25–4.08, P = .007) and reliance on sex work for main source of income (aOR 2.14, 95% CI:1.15–3.99, P = .017) were independent risk factors for HIV infection among MR-MSM.
Table 2.
Risk factors associated with HIV infection among MR-MSM by multivariable analysis: IBBS 2014-15.
4. Discussion
The data collected from the IBBS 201415 shows that 1 in 3 MSM were consumers of alcohol/oral drug or injecting drug users or combination substance users. Previous reports suggest an association between alcohol/polydrug consumption with a higher prevalence of HIV infection among substance users,[18,19] due to the increased probability of unsafe sexual behaviors among MSM.[20] Possible explanations for high-risk sexual behaviors under the influence of alcohol/drugs could be either due to the effect of alcohol/drugs causing behavioral disinhibition or impaired immune system regulation.[21]
Our study discusses the non-sexual high-risk behaviors among the MSM that influences sexual risk behaviors, eventually leading to HIV transmission. Alcohol consumption during or before sex, consumption of oral drugs such as Ganja (Cannabis) or Heroin, injecting drug usage, and sharing of needles or syringes are identified as the multi-risk behaviors among the MSM. The demographic and behavioral factors significantly associated with higher HIV prevalence among MR-MSM are discussed in brief.
4.1. Age and duration of MSM behavior
HIV prevalence was higher among older MSM irrespective of their status of substance usage. This could be attributed to their duration of MSM behavior; longer the duration of MSM activity, higher is the risk of HIV infection.[22] Correspondingly, the prevalence of HIV was higher among MSM aged above 25 years, given that their duration of MSM behavior being more than 10 years (Table 2). More specifically, HIV prevalence was comparatively higher among older MR-MSM exhibiting MSM behavior for more than 10 years when compared to that of younger MSM (4.9% vs 1.9%). Contrastingly, prevalence among those exhibiting MSM behavior for less than a year (6.1%) indicates new infections among the new entrants and was particularly higher among MSM of younger age (6.4%), marking them as a vulnerable population (Supplementary Table 1). Strikingly, the prevalence was higher among those MSM/ MR-MSM who had their first sexual intercourse below 15 years of age. Hence, higher prevalence among older MSM/MR-MSM can also be attributed to unsafe sexual practices at a younger age, longer duration of MSM behavior, or child sexual abuse rather than to substance abuse, nevertheless, older men can avail the drugs/alcohol more easily.
4.2. Education and source of income
Among the MR-MSM, the illiterates were 1.5 times at a higher risk of infection. Although education is not directly related to HIV infection, illiteracy is widely associated with ignorance of HIV, means of transmission, consequences of unsafe anal sex, and the long-term effects of the disease. More often, illiterates stay uninformed about their disease-status or are indifferent about HIV-testing and management.[23] Within the MR-MSM, HIV prevalence was significantly higher among domestic servants (6.2%) and sex workers (7.5%). Relatively, relying on sex work for their main source of income presents a higher risk of infection among all MSM. However, substance usage contributed to over 2 times higher odds of infection among domestic servants (OR: 2.07 95% CI: 1.03–4.17, P < .05) and sex workers (OR: 2.52 95% CI: 1.44–4.41, P < .001). The association of substance usage with HIV infection was more evident among the domestic servants; the prevalence was comparatively lower among domestic servants who did not use any substances (Table 1).
4.3. Marital status
The proportion of married MSM with substance usage was higher than married MSM without substance usage. Similar was the trend among separated/widowed/divorced MSM. Incidentally, the odds of HIV infection among the married MR-MSM was 1.24 times higher than never-married MR-MSM. Concurrently, the highest proportion of MR-MSM exhibits inconsistent condom usage with their regular female partner, most likely to be their wife. This is of special concern as the married MSM population, if involved in an unprotected heterosexual act, have higher chances of horizontal and vertical transmission of the infection. Forced heterosexual marriage, depression, social stigma could be attributed to increased substance usage among married MSM, eventually leading to increased infection risk. It is essential to address the effects of marriage on the psychological and sexual behavior changes of MSM and its correlation with their substance usage.
4.4. Sexual identity and commercial sex behavior
Unprotected anal receptive intercourse (UARI) is a predominant risk factor for HIV transmission among MSM. As expected, MR-MSM self-identified as Kothi are at a higher risk (OR: 1.56; 95% CI: 1.01–2.39; P < .05). Likewise, commercial sex behavior and inconsistent condom usage with paying sexual partners increased the odds of infection. With those MR-MSM involved in commercial sex, the odds of not knowing the HIV status of their clients is high. Synergistically, substance usage can also increase the odds of unsafe sexual behaviors, thus posing a high risk of disease transmission.
4.5. Multiple sexual partners and condom usage
Predominantly, compared to MSM, MR-MSM were less likely to be consistent in their condom usage. More than half of the MR-MSM had inconsistent condom usage with different sexual partners, although, the inconsistency of their condom usage varied between sexual partners, it was more pronounced with female sexual partners. (Table 1). For instance, 63.9% of the MR-MSM had had regular female sexual partners, of which only 23.7% were consistent in condom usage. Inconsistent condom usage with regular or paid female partners was associated with HIV infection. However, a reverse association was found between condom usage with male/TG partners and HIV prevalence. While it is evident that unprotected sex is a risk factor for HIV infection, the reverse association could be because the infected MSM with known HIV positivity status are being consistent in their condom usage. The proportion of MR-MSM having paid/casual female partners/ TG partners was much higher than that of MSM. Multiple sexual partners and inconsistent condom usage are notable risk factors for HIV infection among MR-MSM. Safe sex practice is the most effective method to prevent HIV transmission.[4] Creating awareness about HIV transmission modes and advocating safe-sex practices especially among male sex workers and bisexual, alongside substance-abuse preventive measures are required.
4.6. Injecting drug usage
While oral drug consumption poses similar risks as that of alcohol consumption, injecting drug usage poses a greater threat of transmission through shared needles or syringes. TI has been formulated for the IDU community separately; however, integrated TI that focuses on IDUs within the MSM community is less known. Hence, upgraded integrated-targeted interventions are highly recommended to connect the missing linkages within the HRGs for enhanced HIV management.
One of the strategies of the targeted interventions among MSM is to identify bisexuals and promote protected sexual practices with their female partners to prevent HIV transmission among the general population through vaginal sex. Correspondingly, MSM involved in injecting drug use may not be accessible to TIs of the IDU cluster and hence will be “bridge population” within the HRGs (MSM-IDU↔IDU→ General Population). Moreover, in our study, the prevalence was invariably higher among MSM using any of the substances (alcohol, oral/injecting drug) compared to substance non-users MSM. Hence, an integrated targeted intervention within the high-risk communities (MSM + IDU or MSM + BS + IDU), along with preventive interventions that focus on substance abuse that influence high-risk sexual behaviors simultaneously, will be insightful in effective HIV management.
5. Conclusion
Oral consumption of addictive substances such as alcohol, Ganja (Cannabis), or Heroin does not transmit HIV directly, whereas injecting drugs for non-medical purposes increases the risk of infection through needle/syringe sharing. Nonetheless, the intake of narcotics, especially during or before sex, inflicts unsafe sexual behavior, thereby increasing the risk of HIV infection. Identifying such multi-risk behaviors within the high-risk population and developing integrated interventions will accelerate HIV preventive measures. Such integrated measures must address alcohol /drugs related issues besides promoting safe-sex practices among MSM. Awareness through IEC activities on the adverse effects of alcohol/drug addiction, providing sterile needles to IDU-MSM, and advocating protected sex with female partners are some of the recommended measures. Priority lies in prompt behavioral changes and sensible utilization of HIV-related community services to break the disease transmission linkages. If not intervened now, the MR-MSM community poses serious transmission risks, eventually leading to unmanageable HIV outcomes.
Acknowledgments
The authors wish to thank the Project Directors of all the State AIDS Control Societies, Referral Laboratories, State Surveillance Team members, and sentinel site personnel for their support in completing the surveillance activities on time. The authors also express their special gratitude to Dr. Sanjay Madhav Mehendale, former Additional Director General, Indian Council of Medical Research, New Delhi; Prof. DCS Reddy, Former Professor and Head, Department of PSM, Banaras Hindu University, Varanasi; Dr. Arvind Pandey, Former Director, ICMR-National Institute of Medical Statistics, New Delhi; Prof. Shashi Kant, Professor and Head, Department of Community Medicine, AIIMS, New Delhi for their immense contribution and technical inputs towards establishing a robust HIV Sentinel Surveillance system in India.
Author contributions
Conceptualization: Arumugam Elangovan, Pradeep Kumar, Aridoss Santhakumar.
Data curation: Aridoss Santhakumar, Joseph K. David.
Data analysis: Jaganathasamy Nagaraj.
Writing: Mathiyazhakan Malathi, Arumugam Elangovan.
Review & editing: Shobini Rajan, Balasubramanian Ganesh, Rajatashuvra Adhikary, Natesan Manikandan, V.M. Padmapriya.
Supplementary Material
Footnotes
Abbreviations: AIDS = Acquired Immuno Deficiency Syndrome, BS = Bi-sexual, CAPI = Computer Assisted Personal Interview, DBS = Dried Blood Spot, FSW = Female Sex Worker, HIV = Human Immunodeficiency Virus, HRG = High-Risk Group, IBBS = Integrated Biological and Behavioral Surveillance, IDU = Injecting Drug User, MR-MSM = Men who have Sex with Men exhibiting Multi-Risk behavior, MSM = Men who have Sex with Men, NACO = National AIDS Control Organization, PLHIV = People Living with HIV, SACS = State AIDS Control Society, STI = Sexually Transmitted Infection, TG = Transgender, TI = Targeted Interventions, UARI = Unprotected anal receptive intercourse.
How to cite this article: Kumar P, Aridoss S, Mathiyazhakan M, Balasubramanian G, Jaganathasamy N, Natesan M, V.M. P, David JK, Rajan S, Adhikary R, Arumugam E. Substance use and risk of HIV infection among Men who have Sex with Men in India: Analysis of National IBBS data, India. Medicine. 2020;99:35(e21360).
The Corresponding author received funding from the National AIDS Control Organization, Government of India for conducting the National Integrated Biological and Behavioral surveillance, especially for 7 southern states of India. NACO Grant No. T-11020/36/09-NACO (Surveillance).
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
- [1]. National AIDS Control Organization. National Strategic Plan for HIV/AIDS and STI 2017–2024. “Paving Way for an AIDS Free India”. New Delhi: NACO, Ministry of Health and Family Welfare, Government of India. December 1, 2017; http://naco.gov.in/sites/default/files/Paving%20the%20Way%20for%20an%20AIDS%2015122017.pdf. Accessed December 10, 2019. [Google Scholar]
- [2]. National AIDS Control Organization. National Integrated Biological and Behavioral Surveillance (IBBS), India 2014–15. New Delhi: NACO, Ministry of Health and Family Welfare, Government of India. December 2015; http://naco.gov.in/sites/default/files/IBBS%20Report%202014-15.pdf. Accessed December 10, 2019. [Google Scholar]
- [3].Narayanan P, Das A, Morineau G, et al. An exploration of elevated HIV and STI risk among male sex workers from India. BMC Public Health 2013;13:1059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Abara WE, Oraka E, Jeffries WL, et al. Prevalence and correlates of condom use among sexually active men who have sex with men in the United States: findings from the National Survey of Family Growth, 2002, 2006-2010 and 2011-2013. Sex Health 2017;14:363–71.. [DOI] [PubMed] [Google Scholar]
- [5].Alam SJ, Romero SE, Kim JH, et al. Dynamic sex roles among men who have sex with men and transmissions from primary HIV infection. Epidemiology 2010;21:669–75.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Beyrer C, Baral SD, van Griensven F, et al. Global epidemiology of HIV infection in men who have sex with men. Lancet 2012;380:367–77.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7]. National AIDS Control Organisation. State Epidemiological Fact Sheets, Volume I. New Delhi: NACO, Ministry of Health and Family Welfare, Government of India. August 2017; http://naco.gov.in/sites/default/files/Final%20North-East%20Region%20-%20Vol%201_Final.pdf. Accessed December 10, 2019. [Google Scholar]
- [8].Choi KH, Gibson DR, Han L, et al. High levels of unprotected sex with men and women among men who have sex with men: a potential bridge of HIV transmission in Beijing, China. AIDS Educ Prev 2004;16:19–30.. [DOI] [PubMed] [Google Scholar]
- [9].Colfax G, Coates TJ, Husnik MJ, et al. Longitudinal patterns of methamphetamine, popper (amyl nitrite), and cocaine use and high-risk sexual behavior among a cohort of San Francisco men who have sex with men. J Urban Health 2005;82: 1 Suppl 1: i62–70.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Guadamuz TE, McCarthy K, Wimonsate W, et al. Psychosocial health conditions prevalence incidence cohort men who sex men sex men syndemiceffect. AIDS Behav 2014;18:2089–96.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Holtz TH, Pattanasin S, Chonwattana W, et al. Longitudinal analysis of key HIV-risk behavior patterns and predictors in men who have sex with men, bangkok, thailand. Arch Sex Behav 2015;44:341–8.. [DOI] [PubMed] [Google Scholar]
- [12].Li A, Varangrat A, Wimonsate W, et al. Sexual behavior and risk factors for HIV infection among homosexual and bisexual men in Thailand. AIDS Behav 2009;13:318–27.. [DOI] [PubMed] [Google Scholar]
- [13].David W, Purcell JT, Parsons, et al. Substance use and sexual transmission risk behavior of HIV-positive men who have sex with men. J Substance Abuse 2001;13:185–200.. [DOI] [PubMed] [Google Scholar]
- [14]. IBM Corp. Released 2019. IBM SPSS Statistics for Windows, Version 26.0. IBM Corp., Armonk, NY: IBM Corp. [Google Scholar]
- [15]. National AIDS Control Organisation. State Epidemiological Fact Sheets, Volume II. New Delhi: NACO, Ministry of Health and Family Welfare, Government of India. September 2017; http://naco.gov.in/sites/default/files/Western%20Region%20-%20Vol%202%20revised.pdf. Accessed December 10, 2019. [Google Scholar]
- [16]. NACOHIV Sentinel Surveillance: Technical Brief, India 2016-17. New Delhi: NACO, Ministry of Health and Family Welfare, Government of India. December 2017; http://naco.gov.in/sites/default/files/HIV%20SENTINEL%20SURVEILLANCE_06_12_2017_0.pdf. Accessed December 10, 2019. [Google Scholar]
- [17]. National AIDS Control Organisation. HIV Sentinel Surveillance 2014-15: A Technical Brief. New Delhi: NACO, Ministry of Health and Family Welfare, Government of India. 2015; http://naco.gov.in/sites/default/files/HIV_Sentinel_Surveillance_report.pdf. Accessed December 10, 2019. [Google Scholar]
- [18].Irwin TW, Morgenstern J, Parsons JT, et al. Alcohol and sexual HIV risk behavior among problem drinking men who have sex with men: an event level analysis of timeline followback data. AIDS and Behav 2006;10:299–307.. [DOI] [PubMed] [Google Scholar]
- [19].McCarty-Caplan D, Jantz I, Swartz J. MSM and drug use: a latent class analysis of drug use and related sexual risk behaviors. AIDS Behav 2014;18:1339–51.. [DOI] [PubMed] [Google Scholar]
- [20].Yadav D, Chakrapani V, Goswami P, et al. Association between alcohol use and HIV-related sexual risk behaviors among men who have sex with men (MSM): findings from a multi-site bio-behavioral survey in India. AIDS Behav 2014;18:1330–8.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Zablotska IB, Gray RH, Serwadda D, et al. Alcohol use before sex and HIV acquisition: a longitudinal study in Rakai, Uganda. AIDS 2006;20:1191–6.. [DOI] [PubMed] [Google Scholar]
- [22].Mansergh G, Marks G. Age and risk of HIV infection in men who have sex with men. AIDS 1998;12:1119–28.. [DOI] [PubMed] [Google Scholar]
- [23]. Medel-Anonuevo C, Cheick DM. Making the Connections: Why Literacy Matters for HIV Prevention. Hamburg: UIL; 2007.1-16. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


