Abstract
This study was designed to explore the safety, feasibility, and clinical efficacy of preoperative computed tomography (CT)-guided coil localization of sub-fissural lung nodules (LNs). A total of 105 LN patients underwent CT-guided coil localization followed by video-assisted thoracoscopic surgery (VATS)-guided wedge resection at our hospital from January 2016 to December 2019. Of these patients, 4 had sub-fissural LNs and were therefore subjected to trans-fissural coil localization procedures. We analyzed data pertaining to the coil localization and VATS procedures in these patients. A total of 4 coils were used to localize 4 LNs in 4 separate patients. One of these patients suffered from parenchymal hemorrhage around the needle path, while one other patient exhibited asymptomatic pneumothorax following coil localization. A thoracoscope was able to successfully visualize the coil tails in all of these patients. There were no instances of coils having been dislodged, and wedge resection was conducted with a 100% technical success rate in these patients. These 4 LNs were subsequently diagnosed as adenocarcinomas in situ (n = 3) and benign nodules (n = 1). CT-guided coil localization can be used to safely and easily localize sub-fissural LNs in patients scheduled to undergo VATS.
Keywords: coil, localization, lung nodule, sub-fissural
1. Introduction
As the low-dose computed tomography (CT) has been widely used for screening the lung nodules (LNs), the rates of LN detection have risen.[1–5] The combination of CT-guided localization and video-assisted thoracoscopic surgery (VATS)-guided wedge resection has frequently been employed as a means of diagnosing and treating LNs owing to the minimally invasive nature of this procedure relative to more radical respective treatments.[6–14] Among the localized materials, coil localization usually yielded the lowest complication rates.[6]
Under the normal condition, most localized LNs are peripheral LNs and the coils are typically placed at the peripheral pleura.[7–14] The interlobar fissure also was routinely avoided from the needle pathway because of the following reasons: (a) the healthy lobe may be injured; (b) the incident rate of complications may increase; and (c) increased the technical failure rate of coil localization.
In some special conditions, however, some patients have the sub-fissural LNs which are localized far from the peripheral pleura (>3 cm).[15,16] Under this condition, coil localization at the peripheral pleura is not suitable because the VATS-guided wedge resection cannot be performed via the peripheral approach.[16] The VATS-guided wedge resection can only be performed via the fissural approach, and the coil must instead be placed at the fissural pleura in these patients. The technique of trans-fissural coil localization is challenging. In the previous studies regarding CT-guided localization for LNs, they may contain the patients with sub-fissural LNs.[7–14] However, there have been few studies which only focus on the preoperative localization techniques of sub-fissural LNs.[15,16]
The present analysis was designed to assess the safety, feasibility, and clinical efficacy of preoperative CT-guided coil localization of sub-fissural LNs.
2. Patients and methods
This was a retrospective analysis of patients treated at Xuzhou Central Hospital. This study received approval from the Institutional Review Board of our hospital, and the requirement for written informed consent was waived due to the retrospective nature of this analysis.
2.1. Study design
A total of 105 patients with LNs were treated via CT-guided coil localization and VATS-guided wedge resection from January 2016 to December 2019. Of these patients, 4 m (3.8%) exhibited sub-fissural LNs and underwent trans-fissural coil localization. LNs in these patients were resected following discussions with thoracic surgeons, oncologists, and radiologists in consensus.
2.2. Patients selection
Patient inclusion criteria were as follows: (a) LNs ≤30 mm in diameter; (b) a distance of ≤3 cm between the LN and fissure; (c) a distance of >3 cm between the LN and the peripheral pleura, or a LN lacking any appropriate trans-peripheral pleura-localized route; (d) LNs without a clear pathological diagnosis; and (e) LNs with a medium-to-high risk of malignancy based upon clinical and radiological findings.[1] Exclusion criteria were as follows: (a) LNs <4 mm in diameter; (b) typical benign LNs; and (c) LNs without any suitable trans-fissural localized route.
2.3. LN detection
LNs were detected by the thoracic CT scan (Fig. 1A). The size of the LNs was measured on the maximal transverse diameter. The distant from LN to peripheral and fissural pleura were measured from the CT images.
Figure 1.
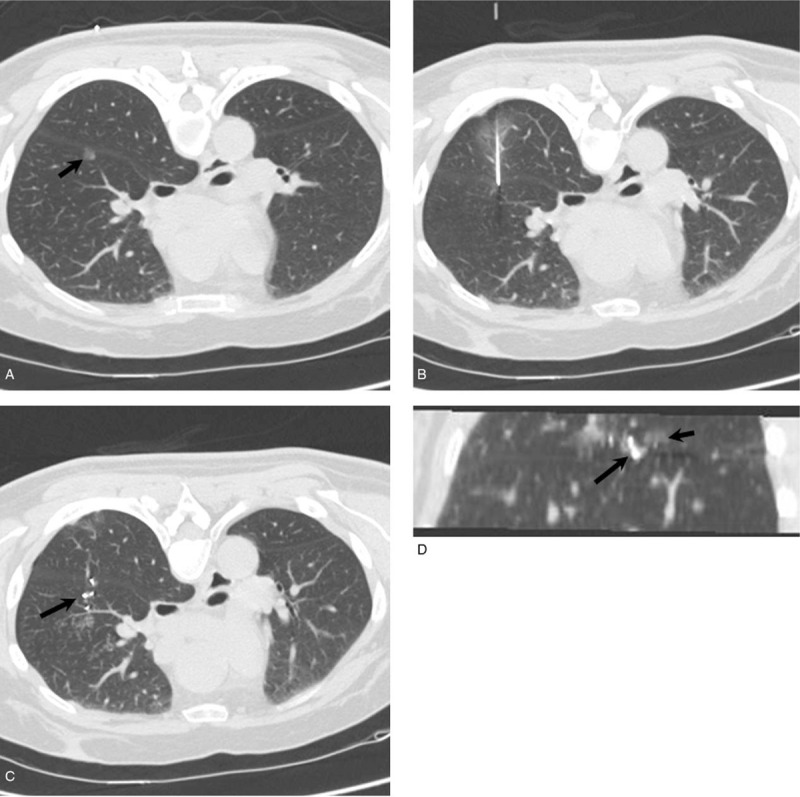
(A) As sub-fissural LN as detected via CT (arrow). (B) A trans-fissural approach was used to guide needle puncture. (C) The coil tail (arrow) remained above the fissural pleura. (D) The relationship between the coil (long arrow) and the LN (short arrow) are represented by this multiple-planar reconstruction.
2.4. CT-guided coil localization
All procedures were conducted with a 16-slice CT (Philips, OH, USA) instrument, with the tube voltage set to 120 kV, the current set to 150 mAs, and the scanning thickness set to 2 mm.
Patients were positioned so as to allow for the shortest necessary needle pathway to be used. The peripheral and fissural pleura was then punctured using an 18 G coaxial needle (Precisa, Roma, Italy) from the neighboring lobe (Fig. 1B). The needle tip was then maintained within 10 mm of the lesion, with a coil that was 0.038 inches in diameter and 50 mm in length (Cook, Bjaeverskov, Denmark) being partially inserted into the lung in this region. The needle was then carefully removed, with the coil tail remaining visible between the fissural pleura of the two contiguous lung lobes (Fig. 1C, D).
Following localization, an additional CT scan was conducted as a means of checking for any procedure-related complications.
2.5. VATS-guided wedge resection
VATS wedge resection was typically conducted within 24 hours following localization in patients. Visualization of the coil tail was used to guide the wedge resection procedure, with the edge of the resected area being 2 cm or more from the coil. In cases where the coil was not visible, efforts were made to locate it via palpation. When these efforts failed, lobectomy was instead conducted.
A rapid pathological assessment of the resected lesion was conducted by the Department of Pathology at our hospital. In any patients with LNs that had advanced beyond the mini-invasive adenocarcinoma (MIA) stage, additional lobectomy and lymph node dissection were performed.
2.6. Definition
Coil localization was considered successful if the coil was found to be localized on the fissural pleura during the VATS. Wedge resection was considered successful if the LN was identified in the wedge-shaped lung tissue.
3. Results
3.1. Baseline data
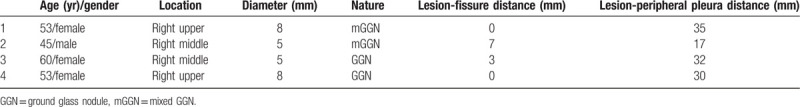
Baseline data for the 4 patients treated via this approach are compiled in Table 1. Each patient exhibited a single LN, and none had any history of prior malignancies.
Table 1.
Baseline data of the 4 patients.
3.2. Localization procedures
A total of 4 coils were used to localize the 4 LNs in these 4 patients (Table 2). Patients were placed in the prone (n = 3) and supine (n = 1) position during localization. CT-guided procedures had a median duration of 15 minutes, with a median intrapulmonary needle path distance of 36.5 mm. Of these 4 patients, 1 suffered from parenchymal hemorrhage around the needle path, and 1 suffered from asymptomatic pneumothorax following coil localization. None of these complications influenced the following VATS procedure.
Table 2.
Details of localization and VATS.
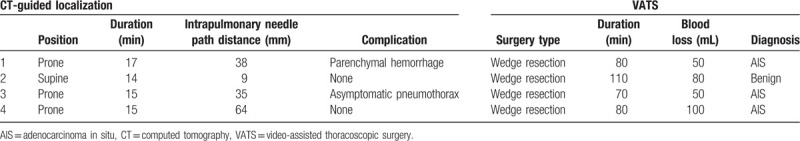
3.3. VATS procedures
A thoracoscope allowed for the successful visualization of coil tails in all patients, with no instances of coils having been dislodged. Wedge resection had a 100% technical success rate in these patients (Table 2). Following rapid pathological analysis, these 4 LNs were diagnosed as adenocarcinomas in situ (n = 3) and benign nodule (n = 1). We would perform lobectomy and later lymph node dissection, if required, but it was not necessary. The total median VATS duration was 80 minutes, with a 65 mL median intraoperative blood loss volume.
4. Discussion
Several previous studies have demonstrated that VATS wedge resection procedures can be safely and effectively guided via a preoperative CT-guided coil localization approach in patients with single, multiple, or ground-glass LNs.[2–8] In the majority of these patients, however, it is important to note that these LNs are most often localized proximal to the peripheral pleura.[8] When these nodules are instead located >3 cm from the peripheral pleura, it is typically necessary for a segmentectomy to be conducted to treat these patients.[9] In such patients, however, LN localization proximal to the fissural pleura can enable preoperative trans-fissural coil localization as an ideal localization strategy.
In the present study, a thoracoscope was able to visualize the coil tails in all 4 studied patients, indicating a 100% localization success rate. This is consistent with a prior study that achieved a 91% technical success rate when employing a trans-fissural short hook-wire approach to preoperatively localize LNs.[10] This result indicated that trans-fissural coil localization for LNs is also technically feasible.
Unlike such hook-wires, the coils used in the present study typically remain in a circular shape following insertion. As such, the coil localization procedure requires additional skill to execute successfully. The high technical success rate observed in the present study may be attributable to the following: (a) the coil was 50 mm long, ensuring that a portion of it could be inserted into the lung while allowing the coil tail to remain on the fissural pleura; and (b) the majority of the coil was inserted into the target lung wherein it adopted a circular configuration. This configuration, together with the fiber coating of the coil, have the potential to enhance coil stability within the lung parenchyma. Even when lungs collapse during the VATS procedure, these coils are resistant to being dislodged.
In this study, we observed a 50% complication rate associated with the trans-fissural coil localization procedure, which was higher than that (12.5%–27.1%) observed in prior studies of LN coil localization.[2–8] This is mainly likely attributable to the long intrapulmonary needle path distance employed in our study. In addition, compared to the conventional route, trans-fissural route creates three holes in the visceral pleura, this is another risk factor of complications. However, none of these complications influenced the following VATS procedure. This finding is comparable to that in the previous studies regarding trans-fissural hook-wire or coil localization for sub-fissural LNs.[10,11]
We were able to successfully conduct VATS wedge resection via the fissural pleura in 100% of patients in the present study. As such, our localization approach led to a significant reduction in the resected lung volume relative to a traditional segmentectomy. Importantly, as all 4 nodules were of a pathological stage lower than MIA, this wedge resection strategy was able to significantly improve the preservation of lung functionality in all treated patients. In addition, the wedge resection instead of lobectomy is performed for patients with lung metastasis.[10] The median blood loss in this study was only 65 mL, which is comparable to that (50 mL) in a previous study regarding of trans-fissural coil localization for sub-fissural LNs.[11]
There are certain limitations to the present analysis. For one, this study is retrospective in nature. In addition, our study size was relatively small. However, as the coil localization of sub-fissural LNs is only conducted in a select subset of patients, our results nonetheless provide important insights into the safety and feasibility of such an approach. Lastly, no control group was included in the present study.
In summary, CT-guided coil localization can be safely and readily conducted prior to VATS wedge resection in certain patients with sub-fissural LNs.
Author contributions
Data curation: Yu Li.
Methodology: Miao Zhang.
Writing – original draft: Er-Liang Li.
Writing – review & editing: Er-Liang Li.
Footnotes
Abbreviations: CT = computed tomography, LN = lung nodule, MIA = mini-invasive adenocarcinoma, VATS = video-assisted thoracoscopic surgery.
How to cite this article: Li EL, Cao W, Li Y, Zhang M. Computed tomography-guided coil localization for sub-fissural lung nodules. Medicine. 2020;99:35(e22030).
The authors have no funding and conflicts of interest to disclose.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
- [1].Winer-Muram HT. The solitary pulmonary nodule. Radiology 2006;239:34–49.. [DOI] [PubMed] [Google Scholar]
- [2].Cruickshank A, Stieler G, Ameer F. Evaluation of the solitary pulmonary nodule. Intern Med J 2019;49:306–15.. [DOI] [PubMed] [Google Scholar]
- [3].Alpert JB, Ko JP. Management of incidental lung nodules: current strategy and rationale. Radiol Clin North Am 2018;56:339–51.. [DOI] [PubMed] [Google Scholar]
- [4].Ko JP, Azour L. Management of incidental lung nodules. Semin Ultrasound CT MR 2018;39:249–59.. [DOI] [PubMed] [Google Scholar]
- [5].Penn A, Ma M, Chou BB, et al. Inter-reader variability when applying the 2013 Fleischner guidelines for potential solitary subsolid lung nodules. Acta Radiol 2015;56:1180–6.. [DOI] [PubMed] [Google Scholar]
- [6].Park CH, Han K, Hur J, et al. Comparative effectiveness and safety of preoperative lung localization for pulmonary nodules: a systematic review and meta-analysis. Chest 2017;151:316–28.. [DOI] [PubMed] [Google Scholar]
- [7].Fu YF, Zhang M, Wu WB, et al. Coil localization-guided video-assisted thoracoscopic surgery for lung nodules. J Laparoendosc Adv Surg Tech A 2018;28:292–7.. [DOI] [PubMed] [Google Scholar]
- [8].Su TH, Fan YF, Jin L, et al. CT-guided localization of small pulmonary nodules using adjacent microcoil implantation prior to video-assisted thoracoscopic surgical resection. Eur Radiol 2015;25:2627–33.. [DOI] [PubMed] [Google Scholar]
- [9].Finley RJ, Mayo JR, Grant K, et al. Preoperative computed tomography-guided microcoil localization of small peripheral pulmonary nodules: a prospective randomized controlled trial. J Thorac Cardiovasc Surg 2015;149:26–31.. [DOI] [PubMed] [Google Scholar]
- [10].Teng F, Wang ZS, Wu AL, et al. Computed tomography-guided coil localization for video-assisted thoracoscopic surgery of sub-solid lung nodules: a retrospective study. ANZ J Surg 2019;89:E514–8.. [DOI] [PubMed] [Google Scholar]
- [11].Yang ZJ, Liang YH, Li M, et al. Preoperative computed tomography-guided coil localization of lung nodules. Minim Invasive Ther Allied Technol 2020;29:28–34.. [DOI] [PubMed] [Google Scholar]
- [12].Refai M, Andolfi M, Barbisan F, et al. Computed tomography-guided microcoil placement for localizing small pulmonary nodules before uniportal video-assisted thoracoscopic resection. Radiol Med 2020;125:24–30.. [DOI] [PubMed] [Google Scholar]
- [13].Liu L, Zhang LJ, Chen B, et al. Novel CT-guided coil localization of peripheral pulmonary nodules prior to video-assisted thoracoscopic surgery: a pilot study. Acta Radiol 2014;55:699–706.. [DOI] [PubMed] [Google Scholar]
- [14].Zhang M, Wang T, Wang H. A segmental labeling technique for non-intubated thoracoscopic anatomical segmentectomy. J Thorac Dis 2017;9:1648–50.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Iguchi T, Hiraki T, Gobara H, et al. Transfissural route used for preoperative localization of small pulmonary lesions with a short hook wire and suture system. Cardiovasc Intervent Radiol 2015;38:222–6.. [DOI] [PubMed] [Google Scholar]
- [16].Xia FF, Shi YB, Wang T, et al. Computed tomography-guided transfissural coil localization of lung nodules. Thorac Cardiovasc Surg 2019;[published online ahead of print, 2019 Aug 26]. doi: 10.1055/s-0039-1695759. [DOI] [PubMed] [Google Scholar]


