Abstract
African American breast cancer genetics is less understood compared to European American breast cancer susceptibility. Despite the many advantages of gene panel screening, studies investigating African American inherited breast cancer risk and comparing variant contributions between ethnicities are infrequent. Thus, 97 breast cancer-affected individuals of African and European descent from the Alabama Hereditary Cancer Cohort were screened using the research-based gene-panel, B.O.P. (Breast, Ovarian, and Prostate cancer). Upon sequencing and bioinformatic processing, rare coding variants in 14 cancer susceptibility genes were categorized according to the American College of Medical Genetics guidelines and compared between ethnicities. Overall, 107 different variants were identified, the majority of which were benign/likely benign. A pathogenic/likely pathogenic variant was detected in 8.6% and 6.5% of African American and European American cases, respectively, which was not statistically significant. However, African Americans were more likely to have at least one variant of uncertain significance (VUS; p-value 0.006); they also had significantly more VUSs in BRCA1/2 compared to European Americans (p-value 0.015). Additionally, 51.4% of African Americans and 32.3% of European Americans harbored multiple rare variants, and African Americans were more likely to have at least one VUS and one benign/likely benign variant (p-value 0.032), as well as multiple benign/likely benign variants (p-value 0.089). Moreover, of the 15 variants detected in multiple breast cancer cases, ATM c.2289T>C (p.F763L), a VUS, along with two likely benign variants, BRCA2 c.2926_2927delinsAT (p.S976I) and RAD51D c.251T>A (p.L84H), were determined to be associated with African American breast cancer risk when compared to ethnic-specific controls. Ultimately, B.O.P. screening provides essential insight towards the variant contributions in clinically relevant cancer susceptibility genes and differences between ethnicities, stressing the need for future research to elucidate inherited breast cancer risk.
Introduction
The introduction of next-generation sequencing (NGS) and implementation of gene-panel screening have significantly reduced sequencing costs and has enabled the analysis of multiple genes-of-interest simultaneously [1, 2]. As such, gene panels can be used in both clinical or research settings to identify variants in genes known to harbor variants that cause or increase the risk of disease [3, 4]. Despite these advantages, few efforts have been published on gene-panel testing in minority populations, especially regarding the assessment of hereditary breast cancer risk. Breast cancer gene-panel screenings have focused on cohorts of mostly white, non-Hispanic individuals [2]; only a small number of studies sought to exclusively examine populations of Asian [5–7] or African [8, 9] descent. However, a few screening reports of multi-ethnic breast cancer cohorts have been published, which have compared variant contributions between ethnicities [10–13]. Even with these efforts, African American breast cancer genetics is less understood compared to the genetic susceptibility of individuals of European descent [8].
There are many breast cancer disparities between African and European Americans [14]. Despite European Americans having higher incidence rates between the ages of 65–84, African American women have higher rates before the age of 40. Knowing that early age of onset is a hallmark of hereditary breast cancer [1], genetic risk factors may be contributing to this disparity. Interestingly, African Americans have been reported to have more variants of uncertain significance (VUSs) in clinically valid breast/ovarian cancer genes [10–13, 15, 16], which warrant further investigation using NGS gene panels. Ultimately, a complete spectrum of breast cancer risk variants needs to be defined to provide greater insight towards African American breast cancer disparities.
The Alabama Hereditary Cancer Cohort (AHCC) provides an opportunity to study breast cancer genetics in underrepresented individuals [17]. Alabama is a medically underserved state and 26.8% of its population self-identify as being Black or African Americans, which is double the national percentage. African American breast cancer probands, which are seemingly unrelated cases, represent 37% of the AHCC due to the focused effort to include this minority population [17]. Thus, 97 breast cancer-affected individuals of either African or European descent from the AHCC were screened using the research-based gene-panel, B.O.P. (Breast, Ovarian, and Prostate cancer) [4, 17]. Rare variants in 14 cancer susceptibility genes were assessed and compared between ethnicities.
Materials and methods
Auburn University Institutional Review Board approved this study. Study participants were recruited and enrolled into a cancer genetic study through IRB-approved protocols, 14–232, 14–335, and 15–111. Informed consent was obtained in writing from all study participants. In total, 97 (35 African American and 62 European American) seemingly unrelated breast cancer cases were selected from the AHCC for genetic analysis based on sequential enrollment. The specific recruitment and enrollment efforts involved for the AHCC were previously described [17]. With average ages of onsets of 45.7 and 47.4 years for African Americans and European Americans, respectively, this cohort represented breast cancer-affected individuals who enrolled into the study because of a young age at diagnosis (<45 years of age) and/or a family history of the disease, which are characteristics of hereditary breast cancer [17]. Genomic DNA from each individual was screened using the custom-designed gene panel, B.O.P., which targets genes that are either clinically proven or thought to be associated with risk of breast, ovarian and/or prostate cancer [4]. DNA libraries were prepared following the HaloPlex HS Target Enrichment System For Illumina Sequencing Protocol (Version C0, December 2015) and subsequently sequenced on an Illumina HiSeq™ 2500 at the Genomic Services Laboratory at HudsonAlpha Institute for Biotechnology. Following capture and sequencing, variants were called using an in-house bioinformatics pipeline [4].
Fourteen genes that were targeted on the B.O.P. panel and have National Comprehensive Cancer Network (NCCN) clinical management guidelines regarding the genetic risk of breast cancer and/or ovarian cancer [18] were selected for variant analysis: ATM (NM_000051), BARD1 (NM_000465), BRCA1 (NM_007300), BRCA2 (NM_000059), CDH1 (NM_004360), BRIP1 (NM_032043), CHEK2 (NM_001005735), NBN (NM_002485), PALB2 (NM_024675), PTEN (NM_000314), RAD51C (NM_058216), RAD51D (NM_001142571), STK11 (NM_000455), TP53 (NM_000546). The depth of coverage of each assessed gene was calculated using DepthOfCoverage tool within the GATK (v.3.4–46) and ranged from 408X-970X (S1 Table). Only variants within coding regions of the 14 genes were further investigated. Next, variants were filtered using ethnic-specific minor allele frequency (MAF) of ≤1% from controls in the National Heart, Lung, and Blood Institute (NHLBI) Exome Sequencing Project Exome Variant Server (EVS) [19]. The EVS data is publicly available and was downloaded as a merged VCF file for each assessed gene. Additionally, known sequencing artifacts from previous screening and validation were removed [4].
After filtering, true positives were identified according to criteria established through B.O.P.’s initial analytical assessment [4]. As a result, true positives included variants with high confidence calls (depth of coverage ≥100X and alternate allele frequency ≥40%), as well as variants with low confidence calls (depth of coverage <100X and alternate allele frequency <40%) that were subsequently validated through polymerase chain reactions (PCR) and Sanger sequencing. All true positive variants were organized into American College of Medical Genetics (ACMG) variant categories for clinical interpretation (pathogenic, likely pathogenic, variant of uncertain significance (VUS), benign, and likely benign) according to InterVar [20, 21]. As recommended, due to InterVar’s automated interpretation based on default parameters, some variant classifications were manually adjusted. Specifically, classifications corresponding to the most recent entries in ClinVar from reputable companies (i.e. Ambry Genetics, Invitae, GeneDx) were considered [22]. Using the Fisher’s exact test in R (v 3.5.1), the number of breast cancer-affected individuals with a particular variant, as well as variants in different categories and genes were compared between ethnicities. Furthermore, of the variants identified in more than one breast cancer-affected individual of the same ethnicity, allele frequencies were compared between cases and ethnic-specific controls from EVS [19].
Results
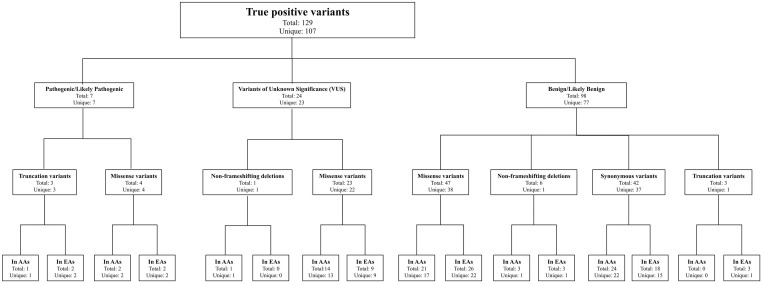
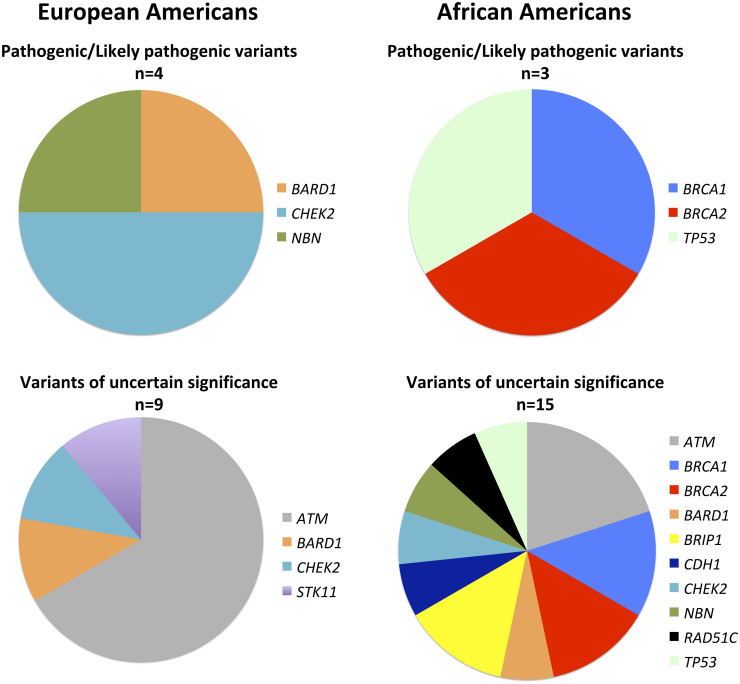
Overall, 107 different (unique), rare coding variants were classified as true positives; since 15 of the unique variants were found in multiple individuals, a total of 129 true positives were identified (Fig 1 and S2 Table). Most variants were benign/likely benign; however, a total of seven pathogenic/likely pathogenic variants were identified as well as 24 VUSs (Figs 1 and 2). The seven different pathogenic/likely pathogenic variants were each detected in one individual, three African Americans and four European Americans (Table 1). The gene distributions were vastly different for each ethnicity (Fig 2). Overall, a pathogenic/likely pathogenic variant was detected in 7.2% (7/97) of all the screened breast cancer cases, corresponding to 8.6% of African American cases and 6.5% of European American cases, which is not a statistically significant difference (Table 2).
Fig 1. ACMG classifications of variants detected after B.O.P. gene panel screening, bioinformatics processing, and filtering.
(AAs) African Americans; (EAs) European Americans.
Fig 2. Genes harboring pathogenic/likely pathogenic variants and VUS.
Table 1. Pathogenic/Likely pathogenic variants detected after B.O.P. screening 97 breast cancer affected cases.
| Gene Name | Chr | Position (hg38) | Ref. Allele | Alt. Allele | Exon | DNA Change | Amino Acid Change | Protein Function | ACMG classification | Number of BC cases with variant | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| EA | AA | ||||||||||
| BARD1 | chr2 | 214728861_214728862 | TG | - | exon 11 | c.2148_2149del | p.T716fs | Truncation | Pathogenic | 1 | 0 |
| BRCA1 | chr17 | 43051071 | A | C | exon 21 | c.5387T>G | p.M1796R | Missense | Pathogenic | 0 | 1 |
| BRCA2 | chr13 | 32339966_ 32339970 | AGTAA | - | exon 11 | c.5611_5615del | p.S1871fs | Truncation | Pathogenic | 0 | 1 |
| CHEK2 | chr22 | 28725099 | A | G | exon 5 | c.599T>C | p.I200T | Missense | Pathogenic | 1 | 0 |
| 28725338 | T | C | exon 4 | c.478A>G | p.R160G | Missense | Likely Pathogenic | 1 | 0 | ||
| NBN | chr8 | 89982770 | G | - | exon 2 | c.123delC | p.I41fs | Truncation | Pathogenic | 1 | 0 |
| TP53 | chr17 | 7673776 | G | A | exon 8 | c.844C>T | p.R282W | Missense | Pathogenic | 0 | 1 |
(AA) African American; (ACMG) American College of Medical Genetics; (Alt.) Alternate; (BC) Breast cancer; (Chr) Chromosome; (EA) European American; (Ref.) Reference.
Table 2. Ethnic comparisons between different variant categories.
| Variant categories | AA BC cases | EA BC cases | Comparison of AA and EA BC cases | ||
|---|---|---|---|---|---|
| # of cases | Percentage | # of cases | Percentage | p-values* | |
| at least one variant of any category | 31 | 88.6% | 40 | 64.5% | 0.016 |
| at least one pathogenic/likely pathogenic variant | 3 | 8.6% | 4 | 6.5% | 0.700 |
| at least one VUS | 14 | 40.0% | 9 | 14.5% | 0.006 |
| at least one benign/likely benign variant | 25 | 71.4% | 36 | 58.1% | 0.274 |
| multiple variants of any category | 18 | 51.4% | 20 | 32.3% | 0.084 |
| multiple pathogenic/likely pathogenic variants | 0 | 0.0% | 0 | 0.0% | 1 |
| multiple VUS | 1 | 2.9% | 0 | 0.0% | 0.361 |
| multiple benign/likely benign variants | 13 | 37.1% | 12 | 19.4% | 0.089 |
| at least one pathogenic variant and one VUS | 1 | 2.9% | 1 | 1.6% | 1 |
| at least one pathogenic variant and one benign/likely benign variant | 1 | 2.9% | 3 | 4.8% | 1 |
| at least one VUS and one benign/likely benign variant | 9 | 25.7% | 5 | 8.1% | 0.032 |
(AA) African American; (BC) Breast cancer; (EA) European American;
*p-values generated using Fisher’s Exact Test.
African American breast cancer cases were more likely to harbor at least one rare variant in one of the 14 assessed susceptibility genes compared to European American breast cancer cases (p-value 0.016; Table 2). This finding was highly influenced by the ethnic differences in VUSs. African Americans were more likely to have at least one VUS (p-value 0.006; Table 2 and Fig 2); they also had significantly more VUSs in BRCA1/2 compared to European Americans (p-value 0.015; Table 3). Additionally, 51.4% of African American breast cancer cases and 32.3% of European American breast cancer cases harbored multiple rare variants amidst the 14 genes (Table 2). African Americans were more likely to have at least one VUS and one benign/likely benign variant (p-value 0.032); African Americans also had more breast cancer cases with multiple benign/likely benign variants, resulting in a p-value trending toward significance (p-value 0.089; Table 2).
Table 3. Ethnic comparisons between VUS in different BC susceptibility genes.
| Genes with VUS | AA BC cases with VUS | EA BC cases with VUS | Comparison of AA and EA BC cases | ||
|---|---|---|---|---|---|
| # of cases | Percentage | # of cases | Percentage | p-values* | |
| BRCA1/2 | 4 | 11.4% | 0 | 0.0% | 0.015 |
| ATM | 3 | 8.6% | 6 | 9.7% | 1 |
| BARD1 | 1 | 2.9% | 1 | 1.6% | 1 |
| BRIP1 | 2 | 5.7% | 0 | 0.0% | 0.128 |
| CDH1 | 1 | 2.9% | 0 | 0.0% | 0.361 |
| CHEK2 | 1 | 2.9% | 1 | 1.6% | 1 |
| NBN | 1 | 2.9% | 0 | 0.0% | 0.361 |
| RAD51C | 1 | 2.9% | 0 | 0.0% | 0.361 |
| STK11 | 0 | 0.0% | 1 | 1.6% | 1 |
| TP53 | 1 | 2.9% | 0 | 0.0% | 0.361 |
(AA) African American; (BC) Breast cancer; (EA) European American;
*p-values generated using Fisher’s Exact Test.
As mentioned above, there were 15 variants detected in multiple breast cancer cases; this included five and seven variants detected solely in African American and European American breast cancer cases, respectively (S3 Table). All of those variants were classified as benign/likely benign except ATM c.2289T>C (p.F763L), which is a VUS. Interestingly, ATM c.2289T>C (p.F763L), along with two other variants currently classified as likely benign, BRCA2 c.2926_2927delinsAT (p.S976I) and RAD51D c.251T>A (p.L84H), were determined to be associated with African American breast cancer risk when compared to ethnic-specific controls (Table 4). Furthermore, comparing all 15 variants between African and European American breast cancer cases, BRCA2 c.2926_2927delinsAT (p.S976I), which was solely detected in African American cases, was the only variant statistically more likely to be observed in either ethnic group (p-value 0.044; Table 4 and S3 Table).
Table 4. Variants identified in more than one breast cancer-affected individual of the same ethnicity and associated with breast cancer risk.
| Gene Name | Chr | Start position (hg38) | Ref. Allele | Alt. Allele | Exon | DNA Change | Amino Acid Change | Protein Function | ACMG Classification | Number of BC cases with variant | Comparison between EA and AA BC cases | Population control comparison (EVS) | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| EA | AA | p-value | AA MAF (%) | AA Alt. allele count | AA WT allele count | AA BC risk p-value* |
||||||||||
| ATM | chr11 | 108257519 | T | A | exon 15 | c.2289T>A | p.F763L | Missense | VUS | 0 | 2 | 0.128 | 0.14 | 6 | 4396 | 0.006 |
| BRCA2 | chr13 | 32337281_32337282 | TC | AT | exon 11 | c.2926_2927delinsAT | p.S976I*** | Missense | Likely benign | 0 | 3 | 0.044 | 0 | 0 | 4406 | 3.67 x 10−6 |
| RAD51D | chr17 | 35116931 | A | T | exon 3 | c.251T>A | p.L84H | Missense | Likely benign | 0 | 2 | 0.128 | 0.26 | 8 | 3128 | 0.019 |
(AA) African American; (ACMG) American College of Medical Genetics; (Alt.) Alternate; (BC) Breast cancer; (Chr) Chromosome; (EA) European American; (EVS) Exome Variant Server; (Ref.) Reference;
*p-values generated using Fisher’s Exact Test.
Discussion
Involving underrepresented individuals in cancer genetics research is crucial to better understand inherited risk in different ethnicities. Herein, 97 breast cancer-affected individuals from the AHCC [17] were screened using the B.O.P. gene panel [4] to identify rare variants (MAF ≤1%) in 14 cancer susceptibility genes and compare the spectrum of variants between African and European Americans. The 14 assessed genes are clinically valid; the NCCN has established breast and/or ovarian cancer risk management guidelines regarding genetic testing results for each of the genes [18]. The variants identified during this study were categorized according to ACMG guidelines, which were established for clinical interpretation [21].
A pathogenic/likely pathogenic variant was detected in seven breast cancer cases, representing 7.2% of the total cohort and corresponding to 8.6% and 6.5% of African American and European American cases, respectively. This slightly higher frequency in African Americans was not statistically significant but was similarly observed in a recent report by Jones et al. [13]. Though it is typically reported that closer to 20% of hereditary breast cancer cases have a high-risk, pathogenic variant in a clinically relevant gene [1], the percentage of cases in this study with such variants is lower. However, it is worth noting that the 14 assessed genes only represent a fraction of the susceptibility genes listed in the NCCN breast/ovarian cancer genetic screening guidelines [18]. For instance, the Lynch syndrome genes MLH1, MSH2, MSH6, PMS2, and EPCAM are included in the guidelines to be managed based on family history [18] and are commonly screened during breast cancer genetic risk assessment [23, 24], but were not included in this analysis. Furthermore, variants in other cancer susceptibility genes (i.e., MUTYH and CDKN2A) are sometimes reported through breast cancer risk assessment [10], but were not assessed in this study. Ultimately, the assessment of this particular number and group of genes may explain the lower percentage of detected pathogenic/likely pathogenic variants. It may also simply be explained by the unique patient population. Ultimately, similar to typical breast cancer gene screening efforts, these results emphasize that the majority of African and European American individuals with familial/hereditary breast cancer remain genetically unsolved upon gene screening [1, 3, 8]; thus, pursuing discovery efforts is important.
BRCA1/2 are recognized as the most commonly mutated genes in hereditary breast cancer cases [1]. Yet, there were no BRCA1/2 pathogenic/likely pathogenic variants detected in European American cases in this study. This finding is contrary to the results of African Americans for which BRCA1/2 variants represented 67% of the detected pathogenic/likely pathogenic variants. Even though it was unexpected to not observe any BRCA1/2 variants in European Americans, our results corroborate a recent study by Kurian et al. that reported more BRCA1 pathogenic variants in African American compared to European American breast cancer cases [12]. Kurian et al. also reported that CHEK2 pathogenic variants were more common in European Americans compared to other minorities. We observed similar results, detecting pathogenic/likely pathogenic CHEK2 variants solely in European Americans. Overall, with African Americans reported to have high genetic diversity and a unique spectrum of variants [25], it is not surprising that no pathogenic/likely pathogenic variants overlapped between ethnicities. In fact, each pathogenic/likely pathogenic variant was unique to an individual.
Previously, in our initial publication describing the B.O.P. panel, we assessed coding variants (in a subset of clinically valid breast/ovarian cancer genes) with MAFs ≤2% in cancer-affected cases from the AHCC and identified a significant difference in the number of African Americans with at least one variant compared to European Americans (p-value 2.71 X 10−3) [4]. Similarly, this study revealed that significantly more African American breast cancer cases had at least one rare variant (MAF ≤1%) in the 14 assessed genes compared to European American breast cancer cases (89% versus 65%, respectively; p-value 0.016). This occurrence was primarily a result of the difference in VUSs, being in 40% and 14.5% of African Americans and European Americans, respectively (p-value 6.45 X 10−3). Even though VUSs were identified in 11 of the 14 assessed genes, there were significantly more BRCA1/2 VUSs in African Americans compared to European Americans. Such differences have been reported since some of the earliest multi-ethnic BRCA1/2 screening studies [15, 16] and continue to be reiterated in multi-ethnic gene panel studies [10, 12, 13]. Thus, in conjunction with those studies, our findings not only reinforce that more inclusive research studies need to be carried out but emphasize the need to investigate this class of variants further. Functional studies, family segregation analyses, and large association studies are pertinent for determining the actual pathogenicity of each identified VUS, which will ultimately result in variant reclassification [3, 26, 27]. This is essential because clinical management does not change with the identification of a VUS [18], and African Americans are disparately receiving such inconclusive results.
Even though ACMG guidelines have been developed for the clinical interpretation of genetic variants in clinically valid susceptibility genes [21], in reality, classification still varies amongst different clinical laboratories, and variant reclassification is an issue [27, 28]. In addition to VUSs, which most frequently undergo reclassifications, the clinical impact of variants in other categories can be downgraded or upgraded [27]. Even though over ~90% of variant reclassifications are downgrades and less than 10% of reclassifications result in a change of actionability, it has been demonstrated that of variants that undergo a change in actionability, 64% are upgrades and 34% are downgrades [27]. Thus, in other words, the majority of variant reclassifications that result in a change in actionability reclassify benign/likely benign variants or VUSs to pathogenic/likely pathogenic. In saying that, it is important to note that there were three variants in this study that were associated with African American breast cancer risk, ATM c.2289T>C (p.F763L), which is a VUS, and two other variants currently classified as likely benign, BRCA2 c.2926_2927delinsAT (p.S976I) and RAD51D c.251T>A (p.L84H). Considering that reclassification rates vary by ancestry and are highest in ethnic minorities [29], these variants could eventually undergo an upgrade in clinical impact; thus, further investigation is warranted. However, similar to BRCA2 c.9976A>T; p.K3326X, they may be low-risk variants, which are currently not clinically relevant [18, 30, 31]. BRCA2 c.9976A>T; p.K3326X, which we identified in three European American breast cancer cases, is classified as likely benign according to the ACMG guidelines. Ultimately, to truly understand risk, all risk variants will need to be considered, no matter where they fall on the spectrum.
NGS, including gene panel screening, detects the full spectrum of variants in the targeted region(s) for each individual screened, which provides an opportunity to explore how combinations of variants contribute towards polygenic risk [32]. Although recent efforts examining polygenic risk of breast cancer have focused on common variants [31], rare variants that modify risk in BRCA1 and BRCA2 mutation carriers have been identified [33, 34]. Considering this, assessing combinations of rare variants is likely a vital missing component for polygenic breast cancer risk assessment. In our study, 51.4% of African American breast cancer cases and 32.3% of European American cases had multiple rare variants in the 14 clinically relevant cancer susceptibility genes (p-value 0.084). This overall difference seemed to be specifically related to more African Americans having multiple benign/likely benign variants (p-value 0.089), as well as at least one VUS and one benign/likely benign variant (p-value 0.032), the latter being statistically significant. Despite that some of the VUSs could eventually be re-classified as pathogenic/likely pathogenic and associated with high risk, overall these variants may individually only slightly elevate risk and specific combinations of these variants may multiplicatively influence risk of developing breast cancer. Therefore, comparing such rare variant combinations between cases and ethnic-specific controls using NGS approaches will provide essential insight towards polygenic breast cancer risk, particularly in African Americans [3]. This effort requires having individual sequencing files from each assessed control, which were not available for this study.
Lastly, with the launch of NGS, several whole-exome sequencing investigations have been carried out to identify novel breast cancer risk variants; however, the majority of those studies were relatively unsuccessful due to the heterogeneity of breast cancer genetics [1]. Noteworthy, the successful whole-exome sequencing studies focused on relatively homogeneous populations [1, 35], suggesting that investigating homogeneous cohorts is a useful approach to enhance our understanding of breast cancer genetics. By screening cancer cases from the AHCC, which was established through strategic recruitment mechanisms that involved traveling to isolated and rural communities in Alabama, the detection of ancestral mutations in seemingly unrelated individuals was anticipated [17]. Overall, this B.O.P. screening suggests that the AHCC is relatively homogeneous since a total of 15 rare variants in the 14 cancer susceptibility genes were detected in multiple seemingly unrelated breast cancer cases. This occurrence likely facilitated the African American breast cancer associations regarding ATM c.2289T>C (p.F763L), BRCA2 c.2926_2927delinsAT (p.S976I) and RAD51D c.251T>A (p.L84H). Additionally, while this study focused on variants with ethnic-specific MAF≤1%, a previous B.O.P. analysis identified a slightly more common, synonymous variant (STK11 c.369G>A;p.Q123Q) associated with African American breast cancer (p-value 8.50 X 10−4) when compared to ethnic-specific controls (MAF of 1.5%) [4]. Nonetheless, the publicly available controls used in this study are not the ideal comparison, being a compilation of cohorts that were sequenced on a different NGS platform [19], and screening larger cohorts including both affected cases as well as internal controls is required to validate these preliminary findings, considering the small sample size in this study. Overall, this study provides insight towards the variant contributions in clinically relevant cancer susceptibility genes and the differences between European and African Americans. Future research should broaden the search for potential genetic risk factors to include all variant types and combinations. Expanding the scope will elucidate breast cancer genetics and potentially identify the hereditary factors that play a role in the disparate number of early-onset breast cancers observed in African American women.
Supporting information
(XLSX)
(XLSX)
(AA) African American; (Alt.) Alternate; (BC) Breast cancer; (Chr) Chromosome; (EA) European American; (#) esp6500siv2; (Het) Heterozygous; (MAF) minor allele frequency; (Ref.) Reference; (VUS) Variant of Uncertain Significance.
(XLSX)
Acknowledgments
Our work would not be possible without the generous involvement and contributions of many people. We are deeply grateful for our study participants who made possible the establishment of the Alabama Hereditary Cancer Cohort. We remain indebted to our community partners and patient advocates for their continued support. We would like to acknowledge the Spencer Cancer Center at East Alabama Medical Center in Opelika, Alabama. Their partnership and efforts towards hospital recruitment on our behalf have been essential. Lastly, we would like to acknowledge the Office of Information Technology at Auburn University for their dedicated support and provision of compute time on the Hopper High-Performance Computing Cluster.
Data Availability
All relevant data are within the manuscript and its Supporting Information files.
Funding Statement
This research was supported by the American Association of Colleges of Pharmacy (AACP) New Investigator Award, AU Research Initiative in Cancer (AURIC) Seed Grant, the Joy to Life Foundation Grant, and the AU Innovative Research grant through the Internal Grant Program with matching funds provided by AURIC and the Joy to Life Foundation (N.D.M). This research was also supported by the AURIC Graduate Fellowship Program (to M.R.B. and A.L. W.H.), the AU Cellular and Molecular Biosciences (CMB) Peaks of Excellence Research Fellowship (to M.R.B. and A.L.W.H.; NSF-EPS-1158862, grant G00006750), the Department of Drug Discovery and Development in the AU Harrison School of Pharmacy, the Department of Pathobiology in the AU College of Veterinary Medicine, and the AU College of Sciences and Mathematics. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Chandler MR, Bilgili EP, Merner ND. A Review of Whole-Exome Sequencing Efforts Toward Hereditary Breast Cancer Susceptibility Gene Discovery. Hum Mutat. 2016;37(9):835–46. 10.1002/humu.23017 [DOI] [PubMed] [Google Scholar]
- 2.Shah PD, Nathanson KL. Application of Panel-Based Tests for Inherited Risk of Cancer. Annu Rev Genomics Hum Genet. 2017;18:201–27. 10.1146/annurev-genom-091416-035305 [DOI] [PubMed] [Google Scholar]
- 3.Easton DF, Pharoah PD, Antoniou AC, Tischkowitz M, Tavtigian SV, Nathanson KL, et al. Gene-panel sequencing and the prediction of breast-cancer risk. N Engl J Med. 2015;372(23):2243–57. 10.1056/NEJMsr1501341 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bishop MR, Huskey ALW, Hetzel J, Merner ND. A research-based gene panel to investigate breast, ovarian and prostate cancer genetic risk. PLoS One. 2019;14(8):e0220929 10.1371/journal.pone.0220929 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lin PH, Kuo WH, Huang AC, Lu YS, Lin CH, Kuo SH, et al. Multiple gene sequencing for risk assessment in patients with early-onset or familial breast cancer. Oncotarget. 2016;7(7):8310–20. 10.18632/oncotarget.7027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mannan AU, Singh J, Lakshmikeshava R, Thota N, Singh S, Sowmya TS, et al. Detection of high frequency of mutations in a breast and/or ovarian cancer cohort: implications of embracing a multi-gene panel in molecular diagnosis in India. J Hum Genet. 2016;61(6):515–22. 10.1038/jhg.2016.4 [DOI] [PubMed] [Google Scholar]
- 7.Ng PS, Wen WX, Fadlullah MZ, Yoon SY, Lee SY, Thong MK, et al. Identification of germline alterations in breast cancer predisposition genes among Malaysian breast cancer patients using panel testing. Clin Genet. 2016;90(4):315–23. 10.1111/cge.12735 [DOI] [PubMed] [Google Scholar]
- 8.Churpek JE, Walsh T, Zheng Y, Moton Z, Thornton AM, Lee MK, et al. Inherited predisposition to breast cancer among African American women. Breast Cancer Res Treat. 2015;149(1):31–9. 10.1007/s10549-014-3195-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ricks-Santi L, McDonald JT, Gold B, Dean M, Thompson N, Abbas M, et al. Next Generation Sequencing Reveals High Prevalence of BRCA1 and BRCA2 Variants of Unknown Significance in Early-Onset Breast Cancer in African American Women. Ethn Dis. 2017;27(2):169–78. 10.18865/ed.27.2.169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Maxwell KN, Wubbenhorst B, D'Andrea K, Garman B, Long JM, Powers J, et al. Prevalence of mutations in a panel of breast cancer susceptibility genes in BRCA1/2-negative patients with early-onset breast cancer. Genet Med. 2015;17(8):630–8. 10.1038/gim.2014.176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shimelis H, LaDuca H, Hu C, Hart SN, Na J, Thomas A, et al. Triple-Negative Breast Cancer Risk Genes Identified by Multigene Hereditary Cancer Panel Testing. J Natl Cancer Inst. 2018;110(8):855–62. 10.1093/jnci/djy106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kurian AW, Ward KC, Howlader N, Deapen D, Hamilton AS, Mariotto A, et al. Genetic Testing and Results in a Population-Based Cohort of Breast Cancer Patients and Ovarian Cancer Patients. J Clin Oncol. 2019;37(15):1305–15. 10.1200/JCO.18.01854 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jones T, Trivedi MS, Jiang X, Silverman T, Underhill M, Chung WK, et al. Racial and Ethnic Differences in BRCA1/2 and Multigene Panel Testing Among Young Breast Cancer Patients. J Cancer Educ. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.American Cancer Society: Breast Cancer Facts and Figures 2019–2020 [Internet]. 2019. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/breast-cancer-facts-and-figures/breast-cancer-facts-and-figures-2019-2020.pdf.
- 15.Haffty BG, Silber A, Matloff E, Chung J, Lannin D. Racial differences in the incidence of BRCA1 and BRCA2 mutations in a cohort of early onset breast cancer patients: African American compared to white women. J Med Genet. 2006;43(2):133–7. 10.1136/jmg.2005.034744 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nanda R, Schumm LP, Cummings S, Fackenthal JD, Sveen L, Ademuyiwa F, et al. Genetic testing in an ethnically diverse cohort of high-risk women: a comparative analysis of BRCA1 and BRCA2 mutations in American families of European and African ancestry. JAMA. 2005;294(15):1925–33. 10.1001/jama.294.15.1925 [DOI] [PubMed] [Google Scholar]
- 17.Bishop MR, Shah A, Shively M, Huskey ALW, Omeler SM, Bilgili EP, et al. Establishment of the Alabama Hereditary Cancer Cohort—strategies for the inclusion of underrepresented populations in cancer genetics research. Mol Genet Genomic Med. 2018;6(5):766–78. 10.1002/mgg3.443 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.National Comprehensive Cancer Network. Genetic/Familial High-Risk Assessment: Breast and Ovarian (Version 3.2019) 2019 https://www.nccn.org/professionals/physician_gls/pdf/genetics_screening.pdf.
- 19.Exome Variant Server. NHLBI GO Exome Sequencing Project (ESP) Seattle, WA2019 http://evs.gs.washington.edu/EVS/.
- 20.Li Q, Wang K. InterVar: Clinical Interpretation of Genetic Variants by the 2015 ACMG-AMP Guidelines. Am J Hum Genet. 2017;100(2):267–80. 10.1016/j.ajhg.2017.01.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Richards S, Aziz N, Bale S, Bick D, Das S, Gastier-Foster J, et al. Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet Med. 2015;17(5):405–24. 10.1038/gim.2015.30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Landrum MJ, Lee JM, Benson M, Brown G, Chao C, Chitipiralla S, et al. ClinVar: public archive of interpretations of clinically relevant variants. Nucleic acids research. 2016;44(D1):D862–8. 10.1093/nar/gkv1222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Desmond A, Kurian AW, Gabree M, Mills MA, Anderson MJ, Kobayashi Y, et al. Clinical Actionability of Multigene Panel Testing for Hereditary Breast and Ovarian Cancer Risk Assessment. JAMA Oncol. 2015;1(7):943–51. 10.1001/jamaoncol.2015.2690 [DOI] [PubMed] [Google Scholar]
- 24.Tung N, Battelli C, Allen B, Kaldate R, Bhatnagar S, Bowles K, et al. Frequency of mutations in individuals with breast cancer referred for BRCA1 and BRCA2 testing using next-generation sequencing with a 25-gene panel. Cancer. 2015;121(1):25–33. 10.1002/cncr.29010 [DOI] [PubMed] [Google Scholar]
- 25.Olopade OI, Fackenthal JD, Dunston G, Tainsky MA, Collins F, Whitfield-Broome C. Breast cancer genetics in African Americans. Cancer. 2003;97(1 Suppl):236–45. 10.1002/cncr.11019 [DOI] [PubMed] [Google Scholar]
- 26.Calo V, Bruno L, La Paglia L, Perez M, Margarese N, Di Gaudio F, et al. The Clinical Significance of Unknown Sequence Variants in BRCA Genes. Cancers (Basel). 2010;2(3):1644–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Slavin TP, Manjarrez S, Pritchard CC, Gray S, Weitzel JN. The effects of genomic germline variant reclassification on clinical cancer care. Oncotarget. 2019;10(4):417–23. 10.18632/oncotarget.26501 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yorczyk A, Robinson LS, Ross TS. Use of panel tests in place of single gene tests in the cancer genetics clinic. Clin Genet. 2015;88(3):278–82. 10.1111/cge.12488 [DOI] [PubMed] [Google Scholar]
- 29.Slavin TP, Van Tongeren LR, Behrendt CE, Solomon I, Rybak C, Nehoray B, et al. Prospective Study of Cancer Genetic Variants: Variation in Rate of Reclassification by Ancestry. J Natl Cancer Inst. 2018;110(10):1059–66. 10.1093/jnci/djy027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Meeks HD, Song H, Michailidou K, Bolla MK, Dennis J, Wang Q, et al. BRCA2 Polymorphic Stop Codon K3326X and the Risk of Breast, Prostate, and Ovarian Cancers. J Natl Cancer Inst. 2016;108(2). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mavaddat N, Pharoah PD, Michailidou K, Tyrer J, Brook MN, Bolla MK, et al. Prediction of breast cancer risk based on profiling with common genetic variants. J Natl Cancer Inst. 2015;107(5). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chatterjee N, Shi J, Garcia-Closas M. Developing and evaluating polygenic risk prediction models for stratified disease prevention. Nat Rev Genet. 2016;17(7):392–406. 10.1038/nrg.2016.27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sokolenko AP, Bulanova DR, Iyevleva AG, Aleksakhina SN, Preobrazhenskaya EV, Ivantsov AO, et al. High prevalence of GPRC5A germline mutations in BRCA1-mutant breast cancer patients. Int J Cancer. 2014;134(10):2352–8. 10.1002/ijc.28569 [DOI] [PubMed] [Google Scholar]
- 34.Thiffault I, Hamel N, Pal T, McVety S, Marcus VA, Farber D, et al. Germline truncating mutations in both MSH2 and BRCA2 in a single kindred. British journal of cancer. 2004;90(2):483–91. 10.1038/sj.bjc.6601424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cybulski C, Carrot-Zhang J, Kluzniak W, Rivera B, Kashyap A, Wokolorczyk D, et al. Germline RECQL mutations are associated with breast cancer susceptibility. Nat Genet. 2015;47(6):643–6. 10.1038/ng.3284 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(XLSX)
(XLSX)
(AA) African American; (Alt.) Alternate; (BC) Breast cancer; (Chr) Chromosome; (EA) European American; (#) esp6500siv2; (Het) Heterozygous; (MAF) minor allele frequency; (Ref.) Reference; (VUS) Variant of Uncertain Significance.
(XLSX)
Data Availability Statement
All relevant data are within the manuscript and its Supporting Information files.