Abstract
Aims
Inflammation plays a pivotal role in atherothrombosis. Colchicine is an anti-inflammatory drug that may attenuate this process. Cardiovascular protective effects of anti-inflammatory drugs, however, seem to be limited to patients with a biochemical response. We therefore investigated whether short-term exposure to colchicine reduced inflammatory markers and whether additional laboratory changes occur in patients with chronic coronary artery disease.
Methods & results
In 138 consecutive patients with chronic coronary artery disease and a high sensitivity C-reactive Protein (hs-CRP) ≥ 2 mg/L, inflammatory markers, lipids, haematologic parameters and renal function were measured at baseline and after 30 days exposure to colchicine 0.5mg once daily. Hs-CRP decreased from baseline 4.40 mg/L (interquartile range [IQR] 2.83–6.99 mg/L) to 2.33 mg/L (IQR 1.41–4.17, median of the differences -1.66 mg/L, 95% confidence interval [CI] -2.17 – -1.22 mg/L, p-value <0.01), corresponding to a median change from baseline of -40%. Interleukin-6 decreased from 2.51 ng/L (IQR 1.59–4.32 ng/L) to 2.22 ng/L (median of the differences -0.36 ng/L, 95%CI -0.70 – -0.01 ng/L, p-value 0.04), corresponding to a median change from baseline of -16%. No clinically relevant changes in lipid fractions were observed. Both leukocyte and thrombocyte count decreased (median change from baseline -7% and -4% respectively). Estimated glomerular filtration rate decreased with a mean change from baseline of -2%.
Conclusion
In patients with chronic coronary artery disease and elevated hs-CRP, one-month exposure to colchicine 0.5 mg once daily was associated with a reduction of inflammatory markers. A small effect was seen on white blood cell count and platelet count, as well as a small decrease in estimated glomerular filtration rate.
Introduction
Inflammation plays a pivotal role in the complex pathophysiology of atherothrombosis [1,2]. Part of the inflammatory response may be initiated by the crystallization of cholesterol in the lipid pool of the atheroma. Leukocyte chemotaxis and inflammatory response can compromise stability of thin capped fibroatheromata. In addition, the cholesterol crystals may pierce through the plaque cap causing direct disruption of the cap [3]. Important chemokines in these processes are interleukin (IL)– 1 and cytosolic multimeric protein complexes called inflammasomes [4–6].
Dampening the inflammatory response in atherosclerosis with anti-inflammatory drugs has yielded contradictory results. Anti-inflammatory treatment with canakinumab, a therapeutic monoclonal antibody targeting interleukin-1β, resulted in a detectable anti-inflammatory biochemical response and was associated with beneficial effects on major clinical outcomes in cardiovascular disease. Treatment with low-dose methotrexate however, did not show biochemical or clinical response [7,8]. Colchicine is an anti-inflammatory drug highly effective in reducing crystal induced inflammation in gout [9]. It is currently investigated as a potential anti-inflammatory drug in several atherosclerotic vascular disease states [10]. Although there is some evidence on its clinical efficacy in cardiovascular disease, the effects on downstream markers of inflammation may vary, and have not yet been investigated in patients with chronic coronary artery disease [11–14].
Colchicine has a narrow therapeutic index. First, competition with Cytochrome P450 3A4 (CYP3A4) or P-glycoprotein metabolizing drugs may lead to decreased clearance of colchicine or alter pharmacodynamics of CYP3A4 substrates such as statins. Second, colchicine in high dose can modulate myeloid cell lines due to its anti-proliferative properties [15,16]. Third, colchicine is relatively contra-indicated in patients with advanced renal insufficiency, although possible reno-protective properties of the drug are increasingly investigated in patients with renal disease [17].
The aim of this study was to investigate whether 30 days exposure to colchicine 0.5mg once daily leads to a reduction in inflammatory biomarkers in patients with chronic coronary artery disease and to investigate effects of treatment on lipid fractions, blood indices, and renal function.
Methods
Design and population
We conducted a prospective, open-label, clinical study with pre- and post-exposure blood testing. Accordingly, adult patients with chronic coronary artery disease were recruited from three Dutch hospitals. Recruitment took place from May 1st, 2017 to December 4th, 2018. Patients were eligible for participation if they had coronary artery disease proven by either invasive coronary angiography or computed tomography coronary angiography with an Agatston calcium score > = 400 units, a high sensitivity [hs]-CRP ≥2 mg/L and if they were considered clinically stable to the discretion of the caregiver. This cut-off value for hs-CRP was chosen to select patients with a pro-inflammatory status and to optimize comparability to prior clinical studies [7,18]. Exclusion criteria were an estimated glomerular filtration rate [eGFR] < 30 ml/min/1,73m2) or a serum creatinine > 150 μmol/L, the necessity to take colchicine for any other indication or concomitant drug use of strong CYP3A4 inhibiting drugs (verapamil, azithromycine, clarithromycin). Patients had to be treated for chronic coronary artery disease without active intercurrent illnesses, frailty or a limited life expectancy according to the discretion of their treating physician. Treatment with other anti-inflammatory drugs was permitted. Obesity was defined as a body mass index of 25 kg/m2 or more. Diabetes was defined by use of oral or parenteral glucose level modifying drugs. Statin intensity was categorized in accordance with the guidelines of the American College of Cardiology and American Heart Association, and high dose statin was defined as atorvastatin 40mg or 80mg dose equivalent [19].
Exposure and outcome
Patients were supplied with colchicine 0.5mg once daily to be taken orally at the same time of the day. The pre-specified primary outcome of the present study was change of hs-CRP and IL-6 after 30 days of exposure to colchicine. Secondary outcomes were change in lipids, leukocyte count, thrombocyte count, red blood cell parameters, creatinine, and estimated renal function using the Chronic Kidney Disease–Epidemiology Collaboration (CKD-EPI) formula. Follow-up took place from May 1st, 2017 to February 1st, 2019.
Laboratory assessment
Blood samples were taken before and after 30 days of exposure to colchicine. All samples were centrifuged (1500xg at 4°C for 15 minutes) and serum was kept stored at -80°C in separate containers. Levels of CRP and IL-6 were measured in a central core laboratory. Hs-CRP was measured using a research hs-CRP Elisa kit (Hycult Biotech #HK369, Uden, the Netherlands). The lower detection limit of this assay was 0.4ng/L and the inter- and intra-assay coefficients of variation were <6.9% and <6.3% respectively. IL-6 levels were measured by highly sensitive human IL-6 immunoassay (R&D Systems #D6050, Minneapolis, MN, USA) for which intra-assay and inter-assay coefficients of variation ranged from 4.2% to 6.4%. This assay had a sensitivity of 0.7 pg/mL.
The hematology parameters were determined with the XN9000 of Sysmex (Sysmex, Kobe, Japan). The serum LDL cholesterol was determined with the third-generation homogeneous enzymatic colorimetric assay, the serum creatinine with the second-generation enzymatic assay. These analyses were carried out in a routine setting under ISO15189 compliance.
Statistical analysis
We estimated that using a sample size of 130 subjects would provide 80% power to detect a mean of the differences of -1 mg/dl in hs-CRP concentration, assuming a standard deviation of 4 mg/dl. Due to the expected non-normal distribution of differences, the minimal number of participants was extended with 15% to increase discriminative power in non-parametric testing [20].
Central tendencies and distribution of continuous parameters were displayed using mean or median with standard deviation or 25th and 75th percentile in case of normally and non-normally distributed variables respectively. Categorical variables were presented as proportions. Paired differences of parameters were evaluated and provided using the mean or median of the differences and the corresponding 95% confidence interval (CI). Standard errors and confidence intervals for medians in non-parametric distributions were computed using bias-corrected and accelerated bootstrapping. A Hodges–Lehmann estimator was used to provide a pseudo-median and confidence interval of the differences between non-parametric distributions. Formal hypothesis testing was done using a paired sample T–test for normally distributed differences and the Wilcoxon Signed Rank Test with continuity correction for non-normally distributed differences. The linear relationship of two continuous parameters was calculated using the Spearman's rank correlation coefficient.
For exploratory purposes, interaction of the estimated treatment effect in selected subgroups was tested using a mixed effects model with random intercepts and slopes with log transformation of outcome data. All subgroups were included in the final model to adjust for confounding.
All calculations were done with R (The R Foundation for Statistical Computing, version 3.6.0. using the packages “LMER” and “boot”).
Ethical approval and funding
The study was approved by a central ethics committee (MEC-U, Nieuwegein, the Netherlands). All patients signed informed consent prior to participation. This work was supported by a governmental grant from The Netherlands Organisation for Health Research and Development [grant number 848015014]. The drug was supplied free of charge by TioPharma (Oud-Beijerland, the Netherlands). The funders and drug supplier had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. The authors confirm that all ongoing and related trials for this drug/intervention are registered and the main trial is registered in the Australian Clinical Trials Registry (ACTRN12614000093684). There are no conflicts of interests by the authors.
Results
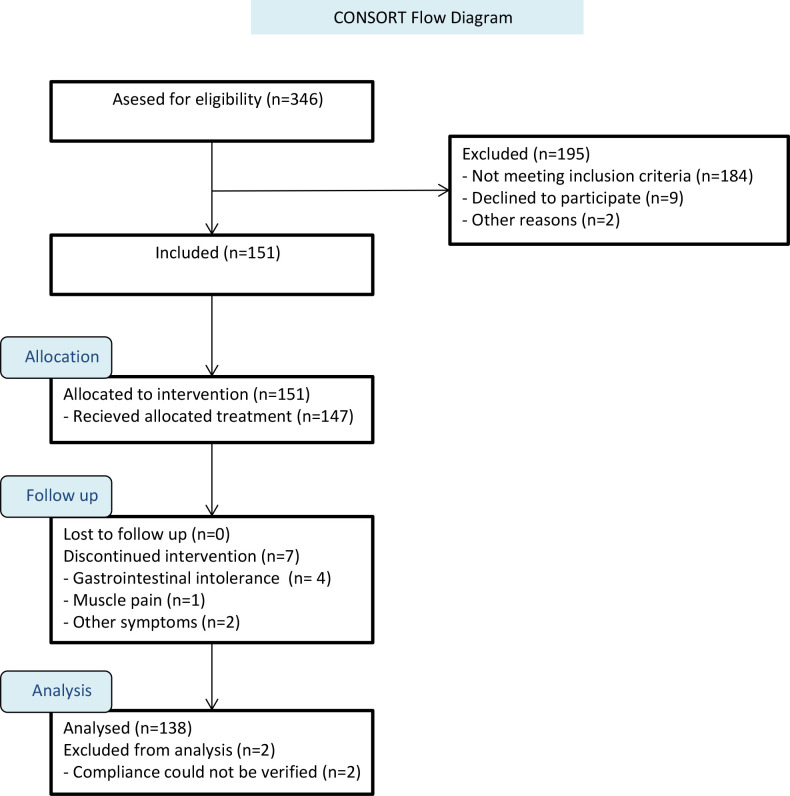
Blood samples were available in 337 patients. Major reasons for exclusion where hs-CRP <2 (n = 184) or intolerance to the drug (n = 7), mainly in the form of gastro-intestinal upset (Fig 1). 138 patients were included in the final analysis.
Fig 1. Flowchart of study.
The figure shows selection of subjects and reason for exclusion. Abbreviation: hs-CRP: High sensitivity C-reactive Protein.
Median age was 65 years and 82% were male (Table 1). Of these, 115 (83%) had a previous acute coronary syndrome with the last event occurring a median of 23 months prior to inclusion (interquartile range [IQR] 9–76 months). Active smokers comprised 14% of the cohort and 20% had diabetes. All had single or dual antiplatelet therapy or anticoagulants, 88% were treated with statins and 59% with high dose statins.
Table 1. Baseline characteristics.
| Demographics | n = 138 | |
|---|---|---|
| Age, years | Mean (SD) | 65.1 (9.4) |
| Male | 113 (81.9%) | |
| Smoker | ||
| Active smoker | 19 (13.8%) | |
| Former smoker | 88 (63.8%) | |
| BMI, kg/m2 | Mean (SD) | 28.7 (4.3) |
| Cardiovascular medical history | ||
| Hypertension | 80 (58.0%) | |
| Diabetes | 27 (19.6%) | |
| Diabetes on insulin | 11 (8.0%) | |
| Prior acute coronary syndrome | 115 (83.3%) | |
| Time since last acute coronary syndrome, months | Median (IQR) | 22.8 (9.3–75.8) |
| Prior percutaneous coronary stenting | 124 (89.9%) | |
| Left ventricular ejectionfraction, % | Mean (SD) | 54.1 (9.9) |
| Cardiovascular drug use | ||
| Dual antiplatelet therapy | 57 (41.3%) | |
| Any antiplatelet therapy or oral anticoagulants | 138 (100.0%) | |
| Betablocker or calciumchannelblocker | 108 (78.3%) | |
| ACE inhibitors or angiotensin receptor blockers | 93 (67.4%) | |
| Any of the above mentioned anti-hypertensives | 125 (90.58%) | |
| Statin | 121 (87.7%) | |
| High dose statin | 71 (58.7%) | |
| Any lipid lowering drug: | 132 (95.7%) |
Statin intensity was categorized in accordance with the guidelines of the American College of Cardiology and American Heart Association, and high dose statin was defined as a atorvastatin 40mg or 80mg dose equivalent [19]. Abbreviations: ACE, angiotensin converting enzyme; BMI, body mass index; IQR, inter quartile range; kg, kilogram; SD, standard deviation.
Inflammatory biomarkers
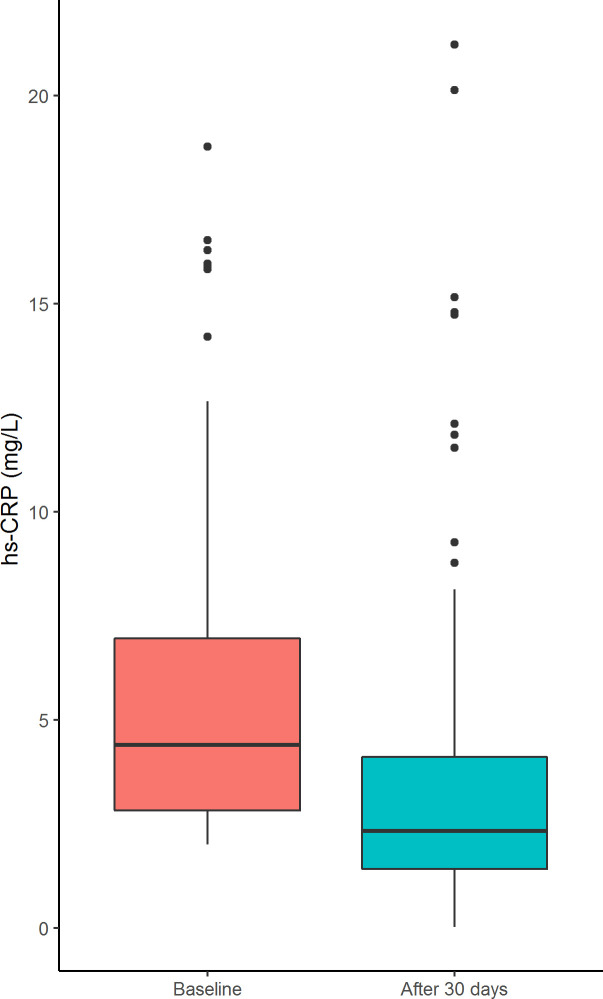
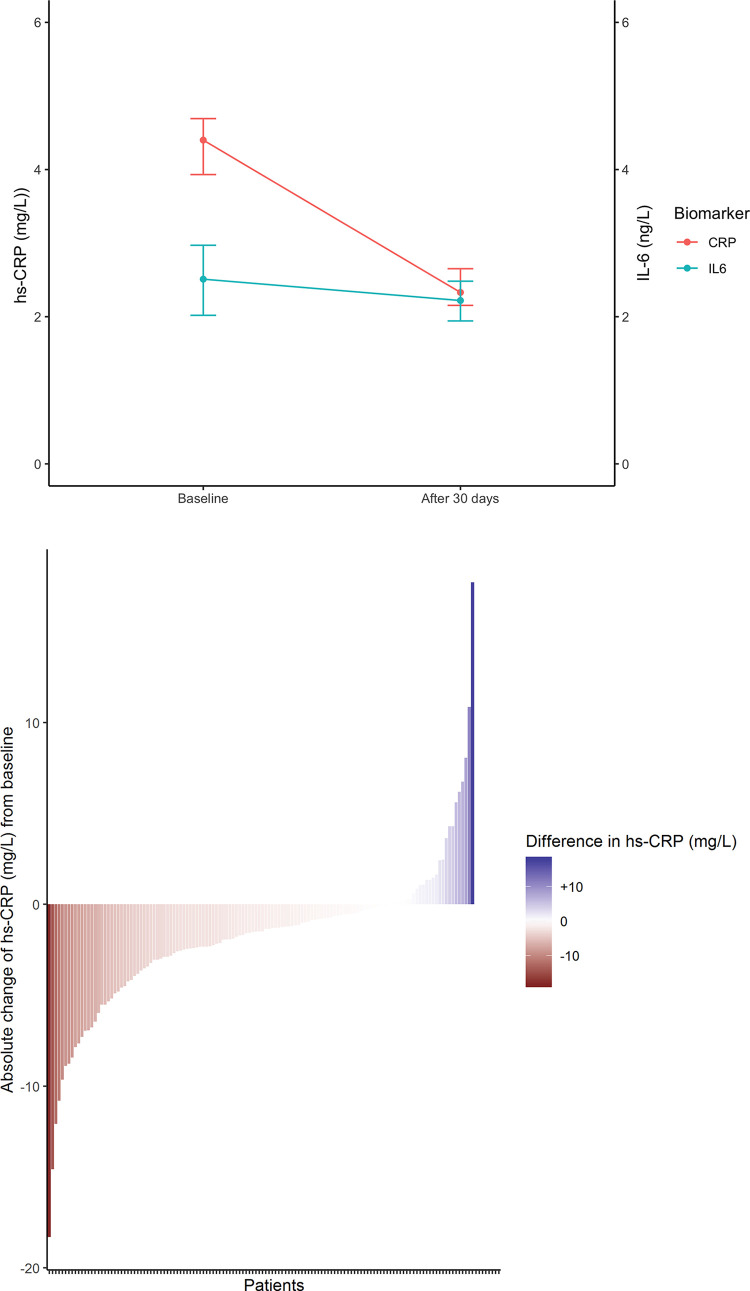
Median baseline hs-CRP was 4.40 mg/L (IQR 2.83–6.99 mg/L). After one month hs-CRP was 2.33 mg/L (IQR 1.41–4.17, median of the differences -1.66 mg/L, 95%CI -2.17 –-1.22 mg/L, p-value <0.01, Fig 2) corresponding to a median change from baseline of -40% (Table 2, Fig 3A). In 81% of patients hs-CRP decreased, with 36% of patients reaching a hs-CRP <2 (Fig 3B).
Fig 2. Boxplot representing change of hs-CRP levels after 30 days of colchicine exposure.
The figure shows the change in median hs-CRP levels after 30 days of colchicine exposure. Abbreviation: hs-CRP: High sensitivity C-reactive Protein.
Table 2. Inflammatory markers and lipids.
| Visit 1 | Visit 2 | Mean or median of differences | 95% CI | P-value | % change from baseline | |||
| Inflammatory Markers | ||||||||
| Interleukin-6 | ng/L | median | 2.51 | 2.22 | -0.36 | (-0.70 to -0.01) | 0.04 | -16% |
| hs-CRP | mg/L | median | 4.40 | 2.33 | -1.66 | (-2.17 to -1.22) | <0.01 | -40% |
| Lipids | Visit 1 | Visit 2 | Mean or median of differences | 95% CI | % change from baseline | |||
| Total Cholesterol | mmol/l | Mean | 4.07 | 3.96 | -0.07 | (-0.16 to 0.01) | 0.091 | NS |
| HDL Cholesterol | mmol/l | Mean | 1.16 | 1.13 | -0.03 | (-0.05 to -0.01) | <0.01 | -3% |
| LDL cholesterol | mmol/l | Mean | 2.38 | 2.24 | -0.07 | (-0.13 to 0.00) | 0.04 | -2% |
| Triglycerides | mmol/l | Mean | 2.04 | 2.13 | 0.08 | (-0.05 to 0.21) | 0.21 | NS |
Abbreviations: CI, confidence interval; HDL, high density lipid; hs, high sensitivity; LDL, low density lipid; NS, not significant.
Fig 3.
a. Median change in hs-CRP. The figure shows the median change in hs-CRP and IL-6 levels after 30 days of colchicine exposure. Horizontal lines represent 95% confidence intervals. Abbreviations: hs-CRP, High sensitivity C-reactive Protein; IL-6, interleukin-6. b. Absolute change in hs-CRP & IL-6. The figure shows a waterfall plot of change in hs-CRP from baseline to 30 days after colchicine exposure. Vertical bars in the plot represent individual patients. Abbreviations: hs-CRP, high sensitivity C-Reactive Protein; IL-6, interleukin-6.
Median baseline IL-6 was 2.51 ng/L (IQR 1.59–4.32 ng/L) and after one month 2.22 ng/L (median of the differences -0.36 ng/L, 95%CI -0.70 –-0.01 ng/L, p-value 0.01), corresponding to a median change from baseline of -16% (Fig 3A).
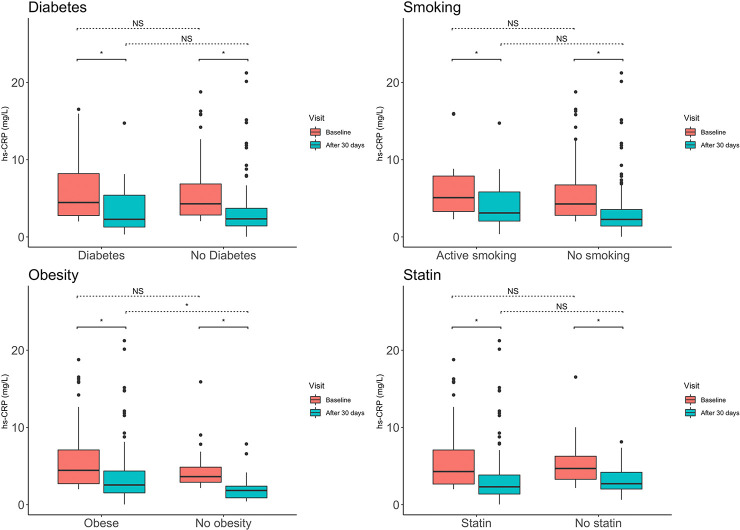
In 57% of patients hs-CRP decrease showed concordance with IL-6 decrease. Overall, a change in hs-CRP showed a moderate correlation with change in IL-6 (R = 0.41, p <0.001). The median decrease of hs-CRP and IL6 was consistent among various pro-inflammatory phenotypes such as diabetes, smoking, obesity and independent of statin use. There were no significant differences in baseline level of hs-CRP or IL-6 between these groups. (Table 3 and Fig 4).
Table 3. Differences in inflammatory markers between subgroups.
| Visit 1 hs-CRP [IQR] | Visit 2 hs-CRP [IQR] | P-value for interaction | Visit 1 IL6 [IQR] | Visit 2 IL6 [IQR] | P-value for interaction | |
|---|---|---|---|---|---|---|
| Clinical subgroup | ||||||
| Diabetes | 4.46 [2.56–8.42] | 2.28 [1.23–5.53] | 0.329 | 2.96 [1.97–4.72] | 3.09 [1.75–3.67] | 0.743 |
| No diabetes | 4.29 [2.83–6.86] | 2.34 [1.42–3.77] | 2.40 [1.49–4.10] | 2.13 [1.38–3.39] | ||
| P-value for within differences | 0.723 | 0.896 | 0.147 | 0.115 | ||
| Active smoking | 5.08 [2.83–8.33] | 3.10 [2.05–5.83] | 0.893 | 2.45 [1.50–3.74] | 2.48 [1.90–4.62] | 0.084 |
| No active smoking | 4.27 [2.76–6.86] | 2.27 [1.41–3.56] | 2.62 [1.59–4.56] | 2.17 [1.37–3.25] | ||
| P-value for within differences | 0.256 | 0.087 | 0.753 | 0.160 | ||
| Obesity | 4.45 [2.67–7.10] | 2.55 [1.52–4.48] | 0.156 | 2.70 [1.76–4.53] | 2.30 [1.45–3.58] | 0.063 |
| No obesity | 3.63 [2.86–4.99] | 1.84 [0.69–2.46] | 1.76 [0.97–3.44] | 1.76 [0.82–3.01] | ||
| P-value for within differences | 0.304 | 0.010 | 0.060 | 0.173 | ||
| Statin | 4.29 [2.67–7.08] | 2.31 [1.38–3.91] | 0.097 | 2.64 [1.55–4.53] | 2.26 [1.45–3.58] | 0.483 |
| No statin | 4.69 [3.29–6.27] | 2.72 [2.02–4.21] | 1.97 [1.64–3.44] | 1.77 [0.57–2.69] | ||
| P-value for within differences | 0.551 | 0.274 | 0.403 | 0.145 |
Abbreviations: hs-CRP, high sensitive C Reactive Protein; IL, interleukin; IQR, interquartile range.
Fig 4. Subgroup changes in hs-CRP.
The figure shows the median change in hs-CRP after 30 days of colchicine exposure in four subgroups. An asterisk depicts p-values < 0.05 for the paired and non-paired comparisons. In all subgroups hs-CRP decreased significantly. There was no significant interaction of the subgroups and change in hs-CRP. Abbreviations: hs-CRP, high sensitivity C-Reactive Protein; NS, not significant.
Lipids
At baseline mean LDL cholesterol level was 2.38 mmol/L. No significant changes were observed in levels of LDL cholesterol, total cholesterol and triglycerides (Table 2). HDL cholesterol decreased from a mean of 1.16 mmol/L to 1.13 mmol/L (median of the differences -0.03 mmol/L, 95% CI -0.05 to -0.01 mmol/L, p-value <0.01), corresponding with a median change from baseline of -3%.
Hematologic markers
No change was seen in concentration of hemoglobin, hematocrit or erythrocytes (Table 4). The mean corpuscular volume of the erythrocytes went from baseline 91.47 to 91.17 femtoliter (mean of the differences -0.35 femtoliter, 95%CI -0.68 to -0.03, p-value 0.03).
Table 4. Haematology and renal function.
| Visit 1 | Visit 2 | Mean or median of differences | 95% CI | P-value | % change from baseline | |||
| Haematology | ||||||||
| Hemoglobine | (mmol/L) | Mean | 9.08 | 9.09 | 0.02 | (-0.05 to 0.09) | 0.59 | NS |
| Hematocrit | L/L | Mean | 0.44 | 0.44 | 0.00 | (-0.01 to 0.00) | 0.28 | NS |
| Erytrocytes | (x 10^12/L) | Mean | 4.87 | 4.87 | 0.00 | (-0.04 to 0.04) | 0.93 | NS |
| MCV | (fl) | Mean | 91.47 | 91.17 | -0.35 | (-0.68 to -0.03) | 0.03 | 0% |
| Leukocytes | (x 10^9/L) | Median | 6.99 | 6.62 | -0.47 | (-0.74 to -0.19) | <0.01 | -7% |
| Trombocytes | (x 10^9/L) | Median | 237.50 | 231.00 | -11.50 | (-16.50 to -6.50) | <0.01 | -4% |
| Renal function | Visit 1 | Visit 2 | Mean or median of differences | 95% CI | P-value | % change from baseline | ||
| eGFR | (ml/min/1,73m2) | Mean | 76.81 | 74.99 | -1.94 | (-3.46 to -0.42) | 0.01 | -2% |
| Creatinine | (μmol/L) | Mean | 87.90 | 89.53 | 1.69 | (0.10 to 3.28) | 0.04 | 1% |
Abbreviations: CI, confidence interval; eGFR, estimated glomerular filtration rate; MCV, mean corpuscular volume; NS, not significant.
The number of leukocytes decreased from a median of 6.99 to 6.62 x 10^9/l (mean of the differences -0.47 x 10^9/l, 95% CI –0.47 to -0.74, p-value <0.01), corresponding to a median change from baseline of -7%. The number of thrombocytes decreased from a median of 237.50 to 231.00 x 10^9/l (median of the differences -11.50 x 10^9/l, 95%CI -16.50 to -6.50, p-value <0.01), corresponding to a median change from baseline of -4%. Leukocyte changes were significantly correlated with changes in hs-CRP (R = 0.23, p < 0.001).
Renal function
Creatinine increased from a mean of 87.90 to 89.53 μmol/L (mean of the differences 1.69 μmol/L, 95%CI 0.10 to 3.28 μmol/L, p-value 0.01), corresponding to a mean change from baseline of 1% (Table 3). Derived mean eGFR was 76.81 ml/min/1.73m2 at baseline and decreased to 74.99 ml/min/1.73m2 after 30 days (mean of the differences -1.94 ml/min/1.73m2, 95%CI -3.28 to -0.42, p-value 0.01), corresponding to a mean change from baseline of -2%. Mild or moderate renal impairment (eGFR 30 to 60 ml/min/1.73m2) was seen in 11% of patients at baseline and 14% of patients at follow-up. Change in eGFR did not correlate significantly with the change in hs-CRP (R 0.07, p = 0.435).
Discussion
This study showed that patients with chronic coronary artery disease and a pro-inflammatory state defined by hs-CRP ≥ 2 mg/L, had a significant decrease in both hs-CRP and IL-6 after one month of colchicine exposure. No clinically relevant changes in lipid spectrum were observed. A small decrease in mean corpuscular volume was observed, as well as a decrease in leukocyte and thrombocyte number and a small decrease in estimated glomerular filtration rate. The present study extends our knowledge of the anti-inflammatory effect of 0.5mg colchicine once daily to patients with chronic coronary artery disease.
Anti-inflammatory effects
The direction and extent of the change in inflammatory markers after exposure to colchicine in this pro-inflammatory population with coronary artery disease compares to observations from previous studies in heart failure and patients with metabolic syndrome. Although absolute reduction of hs-CRP and IL-6 were larger in these studies in which baseline levels were higher, the relative reduction was similar. The reduction in the current study was achieved with a lower dose of colchicine [21,22]. Systemic hs-CRP and IL-6 reduction have not been observed when administrating colchicine directly after acute myocardial infarction [14,23,24]. This may represent limitations in the anti-inflammatory effect of the drug in highly inflammatory conditions such a reperfusion injury and extended necrosis following acute myocardial infarction [25,26].
The magnitude of hs-CRP and IL-6 reduction found in the current study is similar to the effect of canakinumab used in the Canakinumab Antiinflammatory Thrombosis Outcome Study (CANTOS) [7]. Although hs-CRP <2 mg/L is associated with a lower risk for future cardiovascular events, hs-CRP itself carries no causal relationship to such incidents [18]. Inference to the magnitude of any clinical effect based on the current observations is thus explorative. Other surrogate markers for clinical outcomes are suggested to have a directly proportional relationship with hs-CRP concentration. For example, a change in hs-CRP has been shown to be associated in a linear manner with low attenuation plaque volume, a radiologic marker of plaque stability [27].
In contrast to hs-CRP, the evidence for a causal relation to levels of IL-6 and in particular IL– 1 beta and atherothrombosis has become more rigid after observational Mendelian randomization studies and results of the CANTOS trial [7,28–30]. A causative role for these two cytokines in disease progression is further implied by the absence of clinical benefit using the anti-inflammatory drug methotrexate, which did not yield a change in hs-CRP or IL-6 levels [8].
IL– 1 beta is an upstream biomarker of IL-6 and there are data suggesting that high doses of colchicine can reduce IL– 1 beta release. However, such an effect has not been described in patients with chronic coronary artery disease [31]. The absence of a clinical effect in the low dose canakinumab arm with the smallest change in inflammatory biomarkers may suggest a certain biomarker threshold to reach clinical effect. This hypothesis is further substantiated by the absence of clinical effect in patients not reaching below-median levels of IL-6 in the CANTOS trial [32].
Blood count effects
A small reduction in leukocyte and thrombocyte count was observed during one month of colchicine exposure. This finding is not unexpected. Colchicine affects leukocyte adhesion and chemotaxis and also has an anti-proliferative effect on leukocytes, mediated by the ability to disrupt the cytoskeleton. Colchicine irreversibly binds with tubulin to form an intracellular tubulin complex preventing the formation of microtubules [33,34]. In high doses the drug will arrest mitosis in metaphase as it precludes chromosome separation [15]. Data in acute myocardial infarction, gout or Familial Mediterranean Fever do not support the possibility that these changes translate into clinically relevant adverse effect such as increased likelihood of bleeding [14,35]. In patients with recent myocardial infarction, no numerical differences in total white blood count or lymphocytes between active and placebo drugs were seen twelve months after treatment initiation, and similar rates of infection in general were seen, but higher incidences of pneumonia (0.9% versus 0.4% in patients on placebo (p = 0.03) [14]. Treatment with canakinumab resulted in a small increase in the incidence of fatal infection, albeit with a low absolute risk (0.31 versus 0.18 events per 100 person years) [7].
Renal effects
A small increase in serum creatinine and a corresponding decrease of eGFR was observed. Excretion of colchicine takes place mainly via the enterohepatic circulation (80%) and in part via renal excretion (20%) [9,36]. Whether current observations are a direct drug effect on glomerular filtration should be investigated further. Future analysis should include to what extent renal function is affected during long-term administration. The absence of correlation between change in eGFR and magnitude of hs-CRP reduction suggests that the effect of colchicine on eGFR is different from the anti-inflammatory effects of colchicine and may be due to a direct hemodynamic effect on the glomerulus [37,38]. Another effect could be the Hawthorne effect, i.e. an indirect effect of trial participation. Whether the patients increased their compliance with drugs affecting glomerular hemodynamics such as angiotensin converting enzyme inhibitors was not be assessed in the current study setup, but is a known effect in trial participants [39,40].
Limitations
A methodological limitation of our study is the paired testing with the absence of a parallel control group. This is inherent to the design of the study as it was part of the run-in phase prior to randomization of three sites in a clinical trial. Due to the selection of hs-CRP ≥2, part of the change in hs-CRP may be explained by regression to the mean or natural course. However, changes in hs-CRP are more pronounced than those observed in the placebo arm of the similar CANTOS population (change of -40% in this cohort versus -17% in CANTOS), suggesting the CRP decrease is perhaps only partially influenced by preselection and natural course. In addition, no change in IL-6 was seen in the placebo arm of CANTOS [7].
Finally, the subgroup analyses have an exploratory purpose only. Since the study was not designed to assess differences between subgroups, the limited sample size increases risk for type 2 errors in these observations.
Conclusion
One-month exposure to low-dose colchicine was associated with a reduction of the inflammatory markers hs-CRP and IL-6 in patients with chronic coronary artery disease and baseline hs-CRP ≥2 mg/L. An effect was seen on estimated glomerular filtration rate, leukocyte and thrombocyte cell count, which warrants placebo-controlled and longer follow-up of these parameters. Whether the anti-inflammatory and other effects observed in this study are solely contributable to colchicine should be confirmed in placebo-controlled assessment. Whether this effect translates into a clinical benefit has to be awaited. Observations thus far support ongoing clinical research in colchicine as anti-inflammatory drug in atherosclerosis.
Supporting information
(DOC)
(DOCX)
Acknowledgments
The help of the research personnel (Ms Hanneke Bakker, Ms Petra Bunschoten, Ms Marjan van Doorn, Ms Coriet Hobé, Ms Hilde Giezen) at the involved sites and the laboratory staff (Ms Marjet Klein Avink) was highly appreciated.
Data Availability
Data are not publicly available because the research and funding is part of a larger, multi-center and currently still ongoing clinical drug trial sponsored by a governmental grant from The Netherlands Organisation for Health Research and Development. These restrictions are described in the data management plan that was designed by The Netherlands Organisation for Health Research and Development, the ethics committee and the steering committee. However, the complete de-identified data set used in this analysis is available for sharing on request to authors who meet the criteria for access to confidential data. All data access request may be directed to a.schut@wcn.life, or to the authors (JanHein.Cornel@radboudumc.nl, a.t.l.fiolet@umcutrecht.nl, or a.mosterd@meandermc.nl). The authors of the present study had no special access privileges in accessing data from this study which other interested researchers would not have. Additional data acquired after this study concerning subsequent studies will also be shared when the multi-center and currently still ongoing clinical drug trial has finished, in accordance to the prerequisites of the governmental grant (The Netherlands Organization for Health Research and Development, grant number 848015014, registered in the Australian Clinical Trials Registry ACTRN12614000093684).
Funding Statement
This work was supported by a governmental grant from The Netherlands Organisation for Health Research and Development [grant number 848015014]. The drug was supplied free of charge by TioPharma (Oud-Beijerland, the Netherlands). The funders and drug supplier had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. There are no conflicts of interests by the authors.
References
- 1.Ross R. Atherosclerosis—An Inflammatory Disease. N Engl J Med. 1999;340(2):115–26. 10.1056/NEJM199901143400207 [DOI] [PubMed] [Google Scholar]
- 2.Libby P, Ridker PM, Hansson GK. Inflammation in Atherosclerosis: From Pathophysiology to Practice. J Am Coll Cardiol. 2009. December 1;54(23):2129–38. 10.1016/j.jacc.2009.09.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Abela GS. Cholesterol crystals piercing the arterial plaque and intima trigger local and systemic inflammation. J Clin Lipidol. 2010;4(3):156–64. 10.1016/j.jacl.2010.03.003 [DOI] [PubMed] [Google Scholar]
- 4.Janoudi A, Shamoun FE, Kalavakunta JK, Abela GS. Cholesterol crystal induced arterial inflammation and destabilization of atherosclerotic plaque. Eur Heart J. 2016. December 24;37(25):1959–67. 10.1093/eurheartj/ehv653 [DOI] [PubMed] [Google Scholar]
- 5.Duewell P, Kono H, Rayner KJ, Sirois CM, Vladimer G, Bauernfeind FG, et al. NLRP3 inflammasomes are required for atherogenesis and activated by cholesterol crystals. Nature. 2010;464(7293):1357–61. 10.1038/nature08938 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Broz P, Dixit VM. Inflammasomes: mechanism of assembly, regulation and signalling. Nat Rev Immunol. 2016;16(7):407 10.1038/nri.2016.58 [DOI] [PubMed] [Google Scholar]
- 7.Ridker PM, Everett BM, Thuren T, MacFadyen JG, Chang WH, Ballantyne C, et al. Antiinflammatory Therapy with Canakinumab for Atherosclerotic Disease. N Engl J Med. 2017. September;377(12):1119–31. 10.1056/NEJMoa1707914 [DOI] [PubMed] [Google Scholar]
- 8.Ridker PM, Everett BM, Pradhan A, MacFadyen JG, Solomon DH, Zaharris E, et al. Low-Dose Methotrexate for the Prevention of Atherosclerotic Events. N Engl J Med. 2019. February 21;380(8):752–62. 10.1056/NEJMoa1809798 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nuki G. Colchicine: its mechanism of action and efficacy in crystal-induced inflammation. Curr Rheumatol Rep. 2008;10(3):218–27. 10.1007/s11926-008-0036-3 [DOI] [PubMed] [Google Scholar]
- 10.Fiolet ATL, Nidorf SM, Mosterd A, Cornel JH. Colchicine in Stable Coronary Artery Disease. Clin Ther. 2019. January;41(1):30–40. 10.1016/j.clinthera.2018.09.011 [DOI] [PubMed] [Google Scholar]
- 11.Crittenden DB, Lehmann RA, Schneck L, Keenan RT, Shah B, Greenberg JD, et al. Colchicine use is associated with decreased prevalence of myocardial infarction in patients with gout. J Rheumatol. 2012. July;39(7):1458–64. 10.3899/jrheum.111533 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Solomon DH, Liu CC, Kuo IH, Zak A, Kim SC. Effects of colchicine on risk of cardiovascular events and mortality among patients with gout: a cohort study using electronic medical records linked with Medicare claims. Ann Rheum Dis. 2015. November 18;75(9):1674–9. 10.1136/annrheumdis-2015-207984 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nidorf SM, Eikelboom JW, Budgeon CA, Thompson PL. Low-dose colchicine for secondary prevention of cardiovascular disease. J Am Coll Cardiol. 2013;61(4):404–10. 10.1016/j.jacc.2012.10.027 [DOI] [PubMed] [Google Scholar]
- 14.Tardif J-C, Kouz S, Waters DD, Bertrand OF, Diaz R, Maggioni AP, et al. Efficacy and Safety of Low-Dose Colchicine after Myocardial Infarction. N Engl J Med. 2019;381(26):2497–505. 10.1056/NEJMoa1912388 [DOI] [PubMed] [Google Scholar]
- 15.Niel E, Scherrmann J-M. Colchicine today. Jt Bone Spine. 2006;73(6):672–8. [DOI] [PubMed] [Google Scholar]
- 16.Terkeltaub RA. Colchicine update: 2008. Semin Arthritis Rheum. 2009;38(6):411–9. 10.1016/j.semarthrit.2008.08.006 [DOI] [PubMed] [Google Scholar]
- 17.Solak Y, Atalay H, Biyik Z, Alibasic H, Gaipov A, Guney F, et al. Colchicine Toxicity in End-Stage Renal Disease Patients. Am J Ther. 2014;21(6):e189–95. 10.1097/MJT.0b013e31825a364a [DOI] [PubMed] [Google Scholar]
- 18.(CCGCC Reactive Protein Coronary Heart Disease Genetics Collaboration), Wensley F, Gao P, Burgess S, Kaptoge S, Di Angelantonio E, et al. Association between C reactive protein and coronary heart disease: mendelian randomisation analysis based on individual participant data. BMJ. 2011. February 15;342:d548 10.1136/bmj.d548 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Stone NJ, Robinson JG, Lichtenstein AH, Merz CNB, Blum CB, Eckel RH, et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63(25 Part B):2889–934. [DOI] [PubMed] [Google Scholar]
- 20.Lehmann EL. Nonparametrics: Statistical Methods Based on Ranks, Revised. Springer-Verlag; New York; 1998. pages 76–81. [Google Scholar]
- 21.Deftereos S, Giannopoulos G, Panagopoulou V, Bouras G, Raisakis K, Kossyvakis C, et al. Anti-inflammatory treatment with colchicine in stable chronic heart failure: a prospective, randomized study. JACC Hear Fail. 2014;2(2):131–7. [DOI] [PubMed] [Google Scholar]
- 22.Demidowich AP, Levine JA, Onyekaba GI, Khan SM, Chen KY, Brady SM, et al. Effects of colchicine in adults with metabolic syndrome: A pilot randomized controlled trial. Diabetes, Obes Metab. 2019. April 2;21(7):1642–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Raju NC, Yi Q, Nidorf M, Fagel ND, Hiralal R, Eikelboom JW. Effect of colchicine compared with placebo on high sensitivity C-reactive protein in patients with acute coronary syndrome or acute stroke: a pilot randomized controlled trial. J Thromb Thrombolysis. 2012;33(1):88–94. 10.1007/s11239-011-0637-y [DOI] [PubMed] [Google Scholar]
- 24.Hennessy T, Soh L, Bowman M, Kurup R, Schultz C, Patel S, et al. The low dose colchicine after myocardial infarction (LoDoCo-MI) study: A pilot randomized placebo controlled trial of colchicine following acute myocardial infarction. Am Heart J. 2019. June 14;215:62–9. 10.1016/j.ahj.2019.06.003 [DOI] [PubMed] [Google Scholar]
- 25.Ikonomidis I, Athanassopoulos G, Lekakis J, Venetsanou K, Marinou M, Stamatelopoulos K, et al. Myocardial Ischemia Induces Interleukin-6 and Tissue Factor Production in Patients With Coronary Artery Disease. Circulation. 2005. November 22;112(21):3272–9. 10.1161/CIRCULATIONAHA.104.532259 [DOI] [PubMed] [Google Scholar]
- 26.Orn S, Manhenke C, Ueland T, Damas JK, Mollnes TE, Edvardsen T, et al. C-reactive protein, infarct size, microvascular obstruction, and left-ventricular remodelling following acute myocardial infarction. Eur Heart J. 2009. May 2;30(10):1180–6. 10.1093/eurheartj/ehp070 [DOI] [PubMed] [Google Scholar]
- 27.Vaidya K, Arnott C, Martínez GJ, Ng B, McCormack S, Sullivan DR, et al. Colchicine Therapy and Plaque Stabilization in Patients With Acute Coronary Syndrome: A CT Coronary Angiography Study. JACC Cardiovasc Imaging. 2018;11(2):305–16. [DOI] [PubMed] [Google Scholar]
- 28.Libby P. Interleukin-1 Beta as a Target for Atherosclerosis Therapy. J Am Coll Cardiol. 2017. October 31;70(18):2278–89. 10.1016/j.jacc.2017.09.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Consortium I 1 G. Cardiometabolic effects of genetic upregulation of the interleukin 1 receptor antagonist: a Mendelian randomisation analysis. Lancet Diabetes Endocrinol. 2015;3(4):243–53. 10.1016/S2213-8587(15)00034-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Consortium I-6 RMRA (IL6R M. The interleukin-6 receptor as a target for prevention of coronary heart disease: a mendelian randomisation analysis. Lancet. 2012;379(9822):1214–24. 10.1016/S0140-6736(12)60110-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Martinez GJ, Robertson S, Barraclough J, Xia Q, Mallat Z, Bursill C, et al. Colchicine Acutely Suppresses Local Cardiac Production of Inflammatory Cytokines in Patients With an Acute Coronary Syndrome. J Am Heart Assoc. 2015. August 24;4(8):e002128 10.1161/JAHA.115.002128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ridker PM, Libby P, MacFadyen JG, Thuren T, Ballantyne C, Fonseca F, et al. Modulation of the interleukin-6 signalling pathway and incidence rates of atherosclerotic events and all-cause mortality: analyses from the Canakinumab Anti-Inflammatory Thrombosis Outcomes Study (CANTOS). Eur Heart J. 2018. October 7;39(38):3499–507. 10.1093/eurheartj/ehy310 [DOI] [PubMed] [Google Scholar]
- 33.Ben-Chetrit E, Levy M. Colchicine: 1998 update. Semin Arthritis Rheum. 1998;28(1):48–59. 10.1016/s0049-0172(98)80028-0 [DOI] [PubMed] [Google Scholar]
- 34.Phelps P. Polymorphonuclear leukocyte motility in vitro. IV. colchicine inhibition of chemotactic activity formation after phagocytosis of urate crystals. Arthritis Rheum. 1970;13(1):1–9. 10.1002/art.1780130101 [DOI] [PubMed] [Google Scholar]
- 35.Levy M, Eliakim M. Long-term colchicine prophylaxis in familial Mediterranean fever. Br Med J. 1977;2(6090):808 10.1136/bmj.2.6090.808 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rudi J, Raedsch R, Gerteis C, Schlenker T, Plachky J, Walter-Sack I, et al. Plasma kinetics and biliary excretion of colchicine in patients with chronic liver disease after oral administration of a single dose and after long-term treatment. Scand J Gastroenterol. 1994;29(4):346–51. 10.3109/00365529409094847 [DOI] [PubMed] [Google Scholar]
- 37.Platts SH, Falcone JC, Holton WT, Hill MA, Meininger GA. Alteration of microtubule polymerization modulates arteriolar vasomotor tone. Am J Physiol Circ Physiol. 1999;277(1):100–6. [DOI] [PubMed] [Google Scholar]
- 38.Guan T, Gao B, Chen G, Chen X, Janssen M, Uttarwar L, et al. Colchicine attenuates renal injury in a model of hypertensive chronic kidney disease. Am J Physiol Physiol. 2013;305(10):1466–76. [DOI] [PubMed] [Google Scholar]
- 39.McCambridge J, Witton J, Elbourne DR. Systematic review of the Hawthorne effect: new concepts are needed to study research participation effects. J Clin Epidemiol. 2014. March;67(3):267–77. 10.1016/j.jclinepi.2013.08.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Brinker S, Pandey A, Ayers C, Price A, Raheja P, Arbique D, et al. Therapeutic Drug Monitoring Facilitates Blood Pressure Control in Resistant Hypertension. J Am Coll Cardiol. 2014. March 4;63(8):834–5. 10.1016/j.jacc.2013.10.067 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOC)
(DOCX)
Data Availability Statement
Data are not publicly available because the research and funding is part of a larger, multi-center and currently still ongoing clinical drug trial sponsored by a governmental grant from The Netherlands Organisation for Health Research and Development. These restrictions are described in the data management plan that was designed by The Netherlands Organisation for Health Research and Development, the ethics committee and the steering committee. However, the complete de-identified data set used in this analysis is available for sharing on request to authors who meet the criteria for access to confidential data. All data access request may be directed to a.schut@wcn.life, or to the authors (JanHein.Cornel@radboudumc.nl, a.t.l.fiolet@umcutrecht.nl, or a.mosterd@meandermc.nl). The authors of the present study had no special access privileges in accessing data from this study which other interested researchers would not have. Additional data acquired after this study concerning subsequent studies will also be shared when the multi-center and currently still ongoing clinical drug trial has finished, in accordance to the prerequisites of the governmental grant (The Netherlands Organization for Health Research and Development, grant number 848015014, registered in the Australian Clinical Trials Registry ACTRN12614000093684).