Dear Editor,
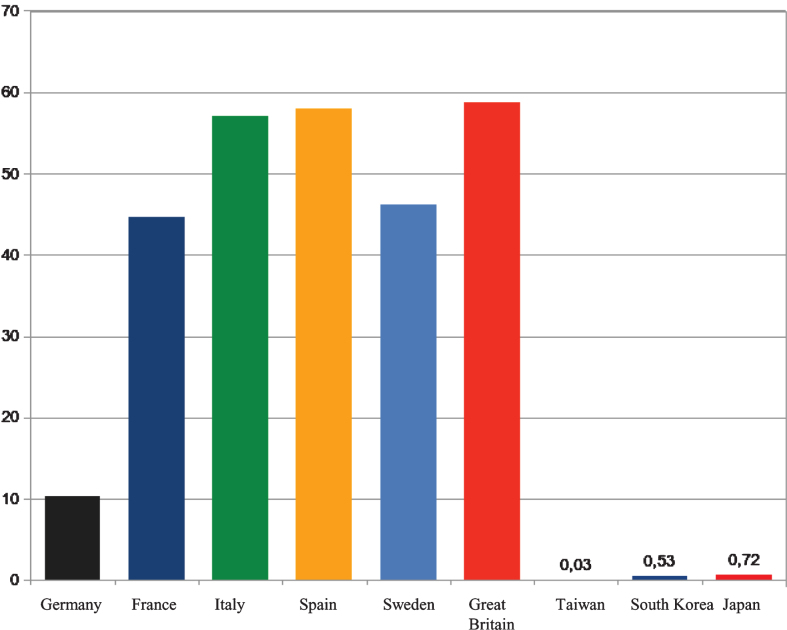
The COVID-19 global pandemic caused by infection with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) remains a significant issue for global health, economics and society. Recent results show a wide variation between countries of per-capita mortality by the disease COVID-19 caused by the virus SARS-CoV-2. For reasons that are not completely understood, the per-capita mortality from COVID-19 varies by several orders of magnitude between countries [1]. Accurate diagnoses, early detection and the management of severe cases differ between the countries as well as the restrictions for the societies and the lock-down of the economy [2]. While in the Western countries after initial hesitation a nation-wide lock-down of the economy became necessary, this was not the case in Taiwan, Japan or South Korea. Figure 1 shows mortality rates per-capita (in relation to 100.000 inhabitants).
Fig.1.
Mortality rates per capita in some European and Asian countries (data of June 8, 2020; data source: https://www.ecdc.europa.eu/en/publications-data/download-todays-data-geographic-distribution-covid-19-cases-worldwide).
Although most people still went to work in those Asian countries, Covid-19-related mortality rates are generally smaller in Asia than in European countries. The biggest difference seems to be that in the Asian countries the wearing of face masks is already common in influenza epidemics and this is also widely practiced by the populations in COVID-19 pandemic. This is unusual in western countries and even at the times of highest infection rates, this was not recommended by the governing authorities, even not by the WHO. It was only on June 1 that the WHO changed its recommendation to wear face masks after all. To contain infections, they are now recommended for use in crowded public places, said the WHO General Director in Geneva.
Infections occur through the airborne transmission of virus-containing droplets (5 to 10μm) and aerosols (≤5μm) exhaled from infected individuals during breathing, speaking, coughing, and sneezing. The spread of COVID-19 is assumed to be occurring through aerosols produced by asymptomatic individuals during breathing and speaking [3, 4]. Droplet size, inertia, gravity, and evaporation determines how far emitted droplets or aerosols remain suspended in the air for minutes-to-hours after a cough or sneeze [5–7]. Droplets sediment fast, contaminate surfaces and lead to contact transmission while aerosols accumulate in indoor air for hours, remain infectious and can be inhaled deep into the lungs. Thus, two respiratory virus transmission pathways exist: contact (between people and with contaminated surfaces) and airborne inhalation.
The transmission of the SARS-Cov2 virus is discussed to occur largely via large cough or sneeze droplets, which comprise the vast portion of the sprayed liquid in cough/sneeze and will land in the nasopharynx due to their size — precisely where the receptors for the virus are present, allowing viral attachment and entry into the host cells. Obviously, this route of transmission could be effectively blocked by simple physical barrier like face masks [8].
Therefore, the wearing of face masks might reduce virus infection induced by: i.) direct contact with respiratory secretions such as on hands and surfaces, ii.) the infection of other persons through speaking, coughing, and sneezing, and 3.) the inhalation of aerosols.
Indeed, face mask usage has been shown to decrease infection and was successfully implemented during former coronavirus outbreaks (i.e. SARS and MERS [9]). Asian countries demonstrate that – among continual isolation, prompt identification of cases and contacts, strict quarantines, travel restrictions, social distancing, and personal hygiene - wearing a mask when on public transit or shopping might help to limit the spread of SARS-COV-2 [10–12].
The findings of a systematic review of 172 studies on COVID-19, SARS, and MERS provide the best available evidence that wearing face masks protects people against infection by coronaviruses (and that eye protection could confer additional benefit) [13]. However, none of these interventions afforded complete protection from infection. Assuming that masks would only reduce transmissions by 22%, then after 10 cycles of the infection, mask-wearing would reduce the level of infection in the population by 91.7%, as compared with a non-mask wearing population [1].
It is highly unlikely that entire countries or populations will ever be randomized to either wear, or not wear, face masks. Therefore, there is not enough data to quantify risk reduction from the use of masks and it is not possible to establish the evidence for wearing masks with certainty. Though masks alone cannot stop the pandemic, studies might indicate that mask wearing should be implemented as early as possible and, especially indoors, should be maintained until the end of the pandemic to successfully combat mortality from SARS-COV-2. The Asian states show that this is possible without a general lock-down.
Conflict of interest
The authors have no conflict of interest to declare.
References
- [1]. Leffler CT, Ing E, McKeown CA, Pratt D, Grzybowski A. Final Country-wide Mortality from the Novel Coronavirus (COVID-19) Pandemic and Notes Regarding Mask Usage by the Public. April 4, 2020. Available from: https://www.researchgate.net/publication/340438732_Country-wide_Mortality_from_the_Novel_Coronavirus_COVID-19_Pandemic_and_Notes_Regarding_Mask_Usage_by_the_Public Accessed: May 20, 2020.
- [2]. Jung F, Krieger V, Hufert FT, Küpper J-H. Herd immunity or suppression strategy to combat COVID-19. Clin Hemorheol Microcirc. 2020. DOI: 10.3233/CH-209006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3]. Morawska L, Cao J. Airborne Transmission of SARS-CoV-2: The World Should Face the Reality. Environ. Int. 2020;139:105730 DOI: 10.1016/j.envint.2020.105730pmid:32294574 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4]. Anderson EL, Turnham P, Griffin JR, Clarke CC. Consideration of the Aerosol Transmission for COVID-19 and Public Health. Risk Anal. 2020;40:902 DOI: 10.1111/risa.13500pmid:32356927 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5]. Tellier R, Li Y, Cowling BJ, Tang W. Recognition of aerosol transmission of infectious agents: A commentary. BMC Infect. Dis. 2019;19,101 DOI: 10.1186/s12879-019-3707-ypmid:30704406 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6]. Mittal R, Ni R, Seo J-H. The flow physics of COVID-19. J. Fluid Mech. 2020. DOI: 10.1017/jfm.2020.330 [DOI] [Google Scholar]
- [7]. Diaz-Quijano F, Rodriguez-Morales AJ, Waldman EA. Translating transmissibility measures into recom-mendations for coronavirus prevention. Rev Saude Publica. 2020;54:43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8]. van der Sande M, Teunis P, Sabel R. Professional and Home-Made Face Masks Reduce Exposure to Respiratory Infections among the General Population. PLoS ONE. 20083(7):e2618 DOI: 10.1371/journal.pone.0002618 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9]. Syed Q, Sopwith W, Regan M, Bellis MA. Behind the mask. Journey through an epidemic: some observations of contrasting public health responses to SARS. Journal of Epidemiology & Community Health. 2003;57(11):855–856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].WHO, Interim Guidance, Advice of the use of masks in the contect of COVID-19, Geneva, June 5, 2020. https://www.who.int/publications/i/item/advice-on-the-use-of-masks-in-the-community-during-home-care-and-in-healthcare-settings-in-the-context-of-the-novel-coronavirus-(2019-ncov)-outbreak.
- [11]. Leung NHL, Chu DKW, Shiu EYC, Chan KH, McDevitt JJ, Hau BJP, Yen HL, Li Y, Ip DKM, Peiris JSM, Seto WH, Leung GM, Milton DK, Cowling BJ. Respiratory virus shedding in exhaled breath and efficacy of face masks. Nat Med. 2020;26:676–680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12]. Prather KA, Wang CC, Schooley RT. Reducing transmission of SARS-CoV-2. Science. 2020. DOI: 10.1126/science.abc6197 [DOI] [PubMed] [Google Scholar]
- [13]. Chu DK, Akl EA, Duda S, Solo K, Yaacoub S, Schünemann HJ. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a systematic review and meta-analysis. Lancet. 2020. doi: 10.1016/S0140-6736(20)31142-9 [DOI] [PMC free article] [PubMed] [Google Scholar]