Abstract
Aim: We sought to validate the 2010 Caprini risk assessment model (RAM) in risk stratification for deep vein thrombosis (DVT) prophylaxis among Chinese bedridden patients.
Methods: We performed a prospective study in 25 hospitals in China over 9 months. Patients were risk-stratified using the 2010 Caprini RAM.
Results: We included a total 24,524 patients. Fresh DVT was found in 221 patients, with overall incidence of DVT 0.9%. We found a correlation of DVT incidence with Caprini score according to risk stratification (χ2 = 196.308, P < 0.001). Patients in the low-risk and moderate-risk groups had DVT incidence < 0.5%. More than half of patients with DVT were in the highest risk group. Compared with the low-risk group, risk was 2.10-fold greater in the moderate-risk group, 3.34-fold greater in the high-risk group, and 16.12-fold greater in the highest-risk group with Caprini scores ≥ 9. The area under the receiver operating characteristic curve was 0.74 (95% confidence interval, 0.71–0.78; P < 0.01) for all patients. A Caprini score of ≥ 5 points was considered the criterion of a reliably increased risk of DVT in surgical patients with standard thromboprophylaxis. Predicting DVT using a cumulative risk score ≥ 4 is recommended for nonsurgical patients.
Conclusions: Our study suggested that the 2010 Caprini RAM can be effectively used to stratify hospitalized Chinese patients into DVT risk categories, based on individual risk factors. Classification of the highest risk levels using a cumulative risk score ≥ 4 and ≥ 5 provides significantly greater clinical information in nonsurgical and surgical patients, respectively.
Keywords: Caprini risk assessment model, Deep venous thrombosis, Venous thromboembolism, Validation study, Risk stratification
Introduction
The incidence of deep venous thrombosis (DVT) is increasing in Asian populations1). Emerging data on Asian patients show that the rates of DVT after major surgery and in medical patients approach rates observed in Western populations2). DVT has become a public issue that seriously threatens human health and economic development3). Fortunately, many cases of DVT are preventable. Identification of patients at risk of developing DVT allows for appropriate thromboprophylaxis to be implemented.
In recent years, great effort has been made to establish risk assessment models (RAMs) to identify patients with high and low risks for various outcomes. The 2005 Caprini RAM4) is perhaps the most widely used and well-validated risk prediction tool to date. It has been implemented and integrated into electronic medical records at many institutions5). The most recent version of the Caprini RAM was published in 2010. However, the updated 2010 version has not been formally validated in a large series of patients. In addition, many past studies used a retrospective design, which may have led to inaccurate assessments. In addition, evidence is inconsistent regarding whether the 2010 Caprini RAM is suitable for recommendation6–8). Therefore, prospective validation of this model among Chinese inpatients is needed.
In our study, we focused on Chinese bedridden patients. Bed rest is a common clinical phenomenon in hospitalized patients, and it is an independent risk factor for many complications including DVT. For patients requiring prolonged bed rest, the potential causes of DVT include reduced blood flow velocity, local blood stasis, and a hypercoagulable state. Therefore, it is vital to assess the risk of developing DVT among bedridden patients and to take appropriate preventive measures.
Aim
To the best of our knowledge, the 2010 Caprini RAM has not been validated in Chinese bedridden patients. Hence, we conducted this study to determine the incidence of DVT in Chinese bedridden patients and to assess the utility of the 2010 Caprini RAM in risk stratification for DVT prophylaxis.
Methods
Study Design
Data were derived from a nationwide project aiming to evaluate the effects of a standardized nursing protocol on the quality of nursing care among bedridden patients. The standardized nursing protocol for DVT was developed based on summary evidence and expert consultation. Nurses from 25 hospitals received training in standardized nursing, which was subsequently implemented in a clinical setting. The present study was a multicenter prospective observational study conducted in 25 hospitals (6 tertiary, 12 non-tertiary, and 7 community hospitals) in China over a period of 9 months (between November 2016 and July 2017). The observational period was only during hospitalization. We recruited participants from these 25 hospitals in the departments of neuromedicine, neurosurgery, general surgery, general medicine, orthopedics, geriatric medicine, and critical care units (intensive care, coronary care, and respiratory care). These wards were chosen as investigation sites because of the high proportion of bedridden patients. All enrolled patients were stratified into different levels according to Caprini RAM score and received a standardized nursing protocol for DVT prophylaxis based on risk stratification. Low-risk patients received early ambulation; moderate-risk patients received elastic stockings (ES), intermittent pneumatic compression (IPC), low-dose unfractionated heparin (LDUH), or low-molecular-weight heparin (LWMH). In high-risk and extremely high-risk patients, the above prevention methods were used in combination, when the patient's condition permitted.
Inclusion and Exclusion Criteria
Patients were recruited from the selected wards. Inclusion criteria included age ≥ 18 years, hospitalization duration ≥ 2 days, remaining bedridden for at least 24 hours after admission to the current ward (bedridden was defined as when all of the patient's basic physiological needs were carried out with the patient remaining in bed, except for active or passive bedside standing and wheelchair transport for examination or treatment), and understanding the aims of the study and signing the consent form. All patients diagnosed with VTE at the time of admission were excluded from the study.
Data Collection
The study was conducted from November 2016 to July 2017. Each hospital appointed a coordinator who was responsible for internal logistics. At least two registered nurses in each participating hospital were appointed to perform patient data collection using a case report form (CRF). To ensure patient data collection was accurate and reliable, all investigators received training in completion of the CRF before the study began.
Measures
Risk Assessment Model (RAM)
Caprini risk scores were included in the CRF. The Caprini RAM was used to score individual patients based on comorbidities and perioperative risk factors. In this model, each independent risk factor is associated with specific points, ranging from 1 to 5, based on the risk of VTE for each factor. In the model, a total risk factor score is calculated, which corresponds to the risk of developing VTE. The most widely used and well-validated RAM is the 2005 Caprini model; the updated 2010 Caprini RAM is the latest version. Compared with the 2005 model, the 2010 model includes additional sub-categorizations for body mass index, operative time, and cancer risk factors. Super-morbid obesity and prolonged operative time are more heavily weighted (e.g., receiving additional points) than in prior versions of the model. A distinction between active cancer and a cancer history is also made, with a corresponding increase in weighting for patients with active cancer. Additionally, a personal history of superficial venous thrombophlebitis has been added as a new, distinct risk factor4, 9). Each patient may be assessed several times during hospitalization. In the present study, the results of the final assessment on study completion (achieving an endpoint, which refers to a diagnosis of VTE, being discharged from the hospital, or death) were used in the analysis.
Patient Information
Patient information was collected using a CRF, which included patient demographic characteristics (age, sex) and medical information (diagnosis, length of bed rest). DVTs were recorded according to the medical records. A 2-week pilot study was conducted in the clinic to test the applicability and clarity of the CRF, and modifications were made according to suggestions from participating nurses. This process ensured that the final version of the CRF could be understood clearly and accurately.
Diagnosis of DVT
A diagnosis of DVT refers to a medical diagnosis, and confirmation via Doppler ultrasound or venography was required. In patients with suspected pulmonary embolism (PE), computed tomographic pulmonary angiography (CTPA) or static lung perfusion scintigraphy were conducted.
Ethical Considerations
This study complied with the Declaration of Helsinki with regard to investigations in humans and was approved by the Ethical Committee of Peking Union Medical College Hospital and the local institutional review boards of the respective hospitals. Patients received verbal and written information about the study and provided their written consent to participate. If patients were unable to give written consent, their relatives were consulted regarding provision of consent. Patients were advised of their right to withdraw from the study at any time. All data were kept confidential and were processed anonymously.
Data Analysis
The data were analyzed using SAS 9.4 for Windows (SAS Institute, Inc., Cary, NC, USA). Continuous variables with a normal distribution are summarized as mean and standard deviation (SD). Categorical data are reported as frequency and percentage. Group comparisons were analyzed using the chisquare test, and single-factor binary logistic regression was also used. A receiver operating characteristic (ROC) curve was plotted for sensitivity and specificity, and the area under the ROC curve (AUC) was calculated. All statistical tests were two-sided. P-values < 0.05 were taken to indicate statistical significance.
Results
Participant Characteristics
Patients' characteristics are presented in Table 1. A total 24,524 bedridden patients were enrolled in the analysis. Most participants were surgical patients (72.5%) and were admitted to a tertiary hospital (81.4%). Patients had a mean age 56.6 years; most patients (39.5%) were in the age group 41–60 years, with only 14.2% over 74 years of age. The sex distribution was 43.2% female and 56.8% male patients. Most patients (95.5%) were in the body mass index (BMI) category of ≤ 30 kg/m2. A total 0.2% of patients had a history of DVT/PE and 2.4% had a cancer history. The number of surgical patients with active cancer (6.9%) was higher than that among nonsurgical patients (1.7%). In terms of length of the bedridden period, 72.3% of patients were bedridden for ≤ 7 days.
Table 1. Characteristics of patients (N = 24,524).
| Variables | Total | Surgical patients (n = 17,774) |
Nonsurgical patients (n = 6,750) |
|---|---|---|---|
| Hospital type | |||
| Tertiary hospital | 19,957 (81.4%) | 15,413 (86.7%) | 4,544 (67.3%) |
| Nontertiary hospital | 4,328 (17.7%) | 2,327 (13.1%) | 2,001 (29.6%) |
| Community hospital | 239 (0.9%) | 34 (0.2%) | 205 (3.0%) |
| Age | |||
| < 41 | 4,119 (16.8%) | 3,454 (19.4%) | 665 (9.9%) |
| 41–60 | 9,676 (39.5%) | 7,645 (43.0%) | 2,031 (30.1%) |
| 61–74 | 7,256 (29.6%) | 5,062 (28.5%) | 2,194 (32.5%) |
| ≥ 75 | 3,473 (14.2%) | 1,613 (9.1%) | 1,860 (27.6%) |
| Gender | |||
| Females | 10,598 (43.2%) | 7,852 (44.2%) | 2,746 (40.7%) |
| Males | 13,926 (56.8%) | 9,922 (55.8%) | 4,004 (59.3%) |
| BMI (kg/m2) | |||
| ≤ 30 | 23,415 (95.5%) | 16,950 (95.4%) | 6,465 (95.8%) |
| > 30 | 1,073 (4.4%) | 804 (4.5%) | 269 (4.0%) |
| > 40 | 30 (0.1%) | 17 (0.1%) | 13 (0.2%) |
| > 50 | 6 (0.02%) | 3 (0.02%) | 3 (0.04%) |
| History of DVT/PE | |||
| No | 24,470 (99.8%) | 17,745 (99.8%) | 6,725 (99.6%) |
| Yes | 54 (0.2%) | 29 (0.2%) | 25 (0.4%) |
| History of cancer | |||
| No | 23,936 (97.6%) | 17,324 (97.5%) | 6,612 (98.0%) |
| Yes | 588 (2.4%) | 450 (2.5%) | 138 (2.0%) |
| Active cancer | |||
| No | 23,188 (94.6%) | 16,552 (93.1%) | 6,636 (98.3%) |
| Yes | 1,336 (5.4%) | 1,222 (6.9%) | 114 (1.7%) |
| Length of bedridden period (days) | |||
| ≤ 7 | 17,722 (72.3%) | 13,162 (74.1%) | 4,560 (67.6%) |
| 8–14 | 3,993 (16.3%) | 2,717 (15.3%) | 1,276 (18.9%) |
| ≥ 14 | 2,809 (11.5%) | 1,895 (10.7%) | 914 (13.5%) |
BMI, body mass index; DVT, deep vein thrombosis; PE, pulmonary embolism.
Incidence Rate of DVT and Risk Stratification According to Caprini RAM Score
Of the 24,524 included patients, fresh DVT was found in 221 patients and the overall incidence of DVT was 0.9%. PE was found in 10 surgical patients, all of which developed from DVT. The incidence of DVT was 0.8% for surgical patients and 1.1% for nonsurgical patients. The duration between the onset of DVT and admission date was 16.3 ± 12.8 days for surgical patients and 14.7 ± 14.9 days for nonsurgical patients. The incidence of proximal DVT was 62 (42.5%) surgical patients and that of distal DVT was 84 (57.5%) surgical patients. Risk stratification according to score of the 2010 Caprini RAM is shown in Table 2. In terms of total Caprini score, 28.9% of patients were in the group with a low risk of DVT (Caprini score 0–1), 20.2% were in the moderate-risk group (Caprini score 2), 20.9% were in the high-risk group (Caprini score 3–4), and 30.0% were in the highest-risk group (Caprini score ≥ 5).
Table 2. Risk stratification according to Caprini RAM score and binary logistic regression for risk level (N = 24,524).
| Risk level | N | DVT Incidence | OR | 95% CI | P |
|---|---|---|---|---|---|
| Low risk (0–1) | 7,089 (28.9%) | 15 (0.2%) | 1 | ||
| Moderate risk (2) | 4,946 (20.2%) | 22 (0.4%) | 2.10 | 1.09–4.07 | 0.026* |
| High risk (3–4) | 5,126 (20.9%) | 36 (0.7%) | 3.34 | 1.82–6.10 | < 0.001*** |
| Highest risk with Score 5–6 | 3,161 (12.9%) | 43 (1.4%) | 6.50 | 3.61–11.72 | < 0.001*** |
| Highest risk with Score 7–8 | 2,689 (11.0%) | 55 (2.1%) | 9.85 | 5.56–17.46 | < 0.001*** |
| Highest risk with Score ≥ 9 | 1,513 (6.2%) | 50 (3.3%) | 16.12 | 9.03–28.78 | < 0.001*** |
| P trend | < 0.001*** |
DVT, deep vein thrombosis; CI, confidence interval; OR, odds ratio; RAM, risk assessment model.
The incidence rates of DVT among the different risk groups are presented in Fig. 1 and Table 2. Patients in the low- and moderate-risk groups had an incidence of DVT < 0.5%. More than half of patients with DVT were from the highest-risk group. The incidence of DVT increased dramatically with increased Caprini score. Further disaggregating patients in the highest-risk category, the increase in incidence of acquired DVT appeared to accelerate according to cumulative risk score (Fig. 1). Chi-square tests suggested differences in DVT incidence among the six groups. That is to say, there was a correlation between the incidence of DVT and Caprini score in risk stratification (χ2 = 196.308, P < 0.001). A binary logistic regression revealed that the risk of developing DVT was significantly higher in the highest-risk group (P < 0.001). Compared with the low-risk group, risk was 2.10-fold greater in the moderate-risk group, 3.34-fold greater in the high-risk group, and 16.12-fold greater in the highest-risk group with scores ≥ 9 (Table 2).
Fig. 1.
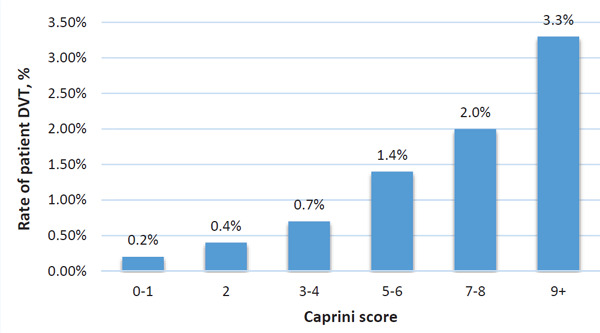
Caprini scores and incidence rates of deep vein thrombosis (DVT)
ROC Curves
For all patients (Fig. 2), analyses of the ROC curves showed that the AUC was 0.74 (95% confidence interval (CI), 0.71–0.77; P < 0.001); a Caprini score of 3.5 was the cutoff point providing the highest sensitivity and specificity (sensitivity, 0.75; specificity, 0.62). Thus, the 2010 Caprini RAM showed satisfactory accuracy for predicting DVT using a cumulative risk score of ≥ 4.
Fig. 2.
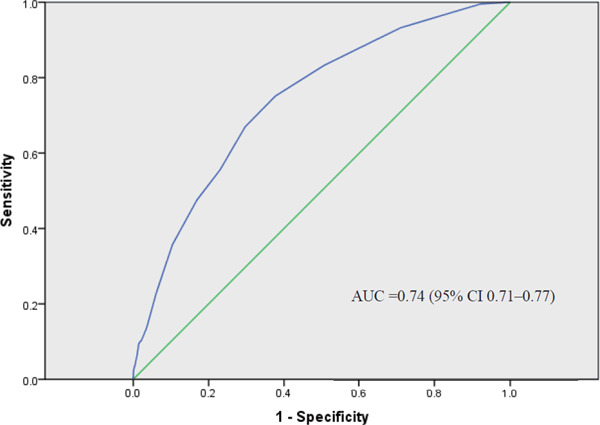
Receiver operating characteristic (ROC) curve of Caprini scores for all patients AUC, area under the ROC curve.
For surgical patients (Fig. 3), analyses of the ROC curves showed that the AUC was 0.77 (95% CI, 0.74–0.81; P < 0.001); a cutoff point of Caprini score 4.5 reliably predicted the onset of DVT (sensitivity, 0.71; specificity, 0.72). Therefore, a Caprini score ≥ 5 was accepted as the criterion of a reliably increased risk of DVT among surgical patients with standard thromboprophylaxis in place.
Fig. 3.
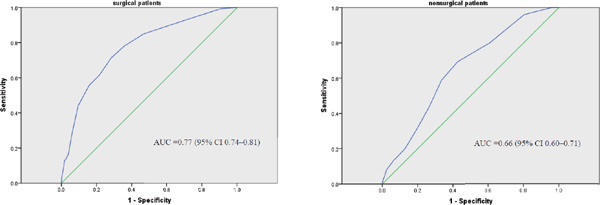
Receiver operating characteristic (ROC) curves for surgical patients and nonsurgical patients AUC, area under the ROC curve.
For nonsurgical patients (Fig. 3), the AUC was 0.66 (95% CI, 0.60–0.71; P < 0.001) and a Caprini score of 3.5 was the cutoff point providing the highest sensitivity and specificity (sensitivity, 0.69; specificity, 0.57). The 2010 Caprini RAM showed lower accuracy for predicting DVT in nonsurgical patients than surgical patients. Predicting DVT using a cumulative risk score of ≥ 4 is recommended.
Discussion
Awareness of the risks related to bed rest is high among clinicians, and immobility is one of the main determinants of prescribing thromboprophylaxis in clinical practice10). Thus, it is vital to assess the risk of developing DVT among bedridden patients, to implement appropriate preventive measures. We sought to determine the incidence of DVT among Chinese bedridden patients and to validate the 2010 Caprini RAM, to stratify the risk of developing DVT among hospitalized patients based on their individual risk factors.
In this study, we finally identified 221 (0.9%) patients with fresh DVT among 24,525 patients who were bedridden for at least 24 hours after admission and who received standard VTE prophylaxis. Interestingly, the incidence of DVT among nonsurgical patients (1.1%) was higher than that among surgical patients (0.8%). We found that the DVT incidence was much lower than in previous reports. A retrospective study analyzed 8,216 inpatients who underwent general, vascular, and urologic surgery between 2001 and 2008. The overall incidence of VTE within 30 days was 1.4%; by risk level, the incidence was as follows: highest, 1.94%; high, 0.97%; moderate, 0.70%; and low, 0%9). There are several possible reasons for the lower incidence of DVT among Chinese patients. First, our findings indicated that our standardized nursing protocol for DVT prophylaxis was effective. In our study, low-risk patients received early ambulation; moderate-risk patients received ES, IPC, LDUH, or LWMH. In high-risk and extremely high-risk patients, the above prevention methods were used in combination, when the patient's condition permitted. Second, the lower incidence of DVT in our study may be partly owing to differences in ethnicity. Third, most of our patients had symptomatic DVT; thus, it was difficult to compare our findings with previously reported data. As for the higher incidence of DVT among nonsurgical patients, this is consistent with existing findings. Although historically considered a complication of surgical admission, it is now recognized that up to 70% of thromboembolic events and almost two-thirds of fatal PE among hospitalized patients occur among nonsurgical patients11, 12). DVT occurs in hospitalized non-surgical as well as surgical patients, and the risk of DVT is as high in some nonsurgical patients as in those who undergo surgery. Therefore, all hospitalized patients should receive appropriate prophylaxis.
In the original Caprini RAM, all patients with a score > 5 were placed in the same group4). Bahl et al. modified the Caprini RAM and added a separate “super high risk” group (score > 8) and also recommended an extended duration of chemoprophylaxis in these patients9). By further dividing the highest-risk category in our study, we observed that the difference in DVT incidence among the six groups was statistically significant (P < 0.001). This indicated that the Caprini score and cumulative risk level were associated with an increased risk of DVT. An increase in the odds ratio for DVT was noted in patients with increased cumulative risk scores. A higher-risk patient had a higher incidence of DVT despite receiving standardized nursing protocol for DVT prophylaxis. Compared with the low-risk group, risk was 2.10-fold greater in the moderate-risk group, 3.34-fold greater in the high-risk group, and 16.12-fold greater in the highest-risk group (scores ≥ 9). These findings are consistent with the results of a study published by Bilgi et al. in surgical patients13). Zhou also found similar results and preliminarily suggested that the 2010 Caprini RAM is a practical and effective tool for assessing the risk of DVT among unselected Chinese inpatients, and that it may also be useful in predicting the risk of VTE recurrence6, 14). The findings of the present study are consistent with these observations and suggest that further stratification of the highest risk category is necessary to determine the exact extent of risk.
For all patients, analyses of ROC curves showed that the AUC was 0.74 (95% CI, 0.71–0.77; P < 0.001). This indicated satisfactory accuracy for predicting DVT using a cumulative risk score of ≥ 4. One study recommended a cumulative risk score of ≥ 5 to predict risk of DVT, but ROC curves were not used in the analysis in that previous study; its retrospective design also included several limitations that precluded identification of all patient risk factors. In addition, screening hospitalized patients for asymptomatic DVT was not routinely performed in the hospital in that past study14). Kirill et al. conducted a validation study of the Caprini RAM in high-risk surgical patients under a background of standard prophylaxis15); the AUC in that study was 0.87 (95% CI, 0.81–0.93; P < 0.001). A Caprini score of ≥ 11 can be used identify a subgroup of patients at extremely high risk. The results of our ROC analysis reconfirmed the high predictive power of the model with respect to DVT.
The current strategy in risk assessment among inpatients is to use different RAMs based on the department in which patients are currently hospitalized; this is inconvenient and time-consuming in a general hospital where patients are moved to different departments relatively frequently16). Validation of the 2010 Caprini RAM in nonsurgical patients is rare because it originated from a surgical population. From the AUC in our study, we can conclude that the 2010 Caprini RAM was much more effective in assessing DVT risk among surgical patients than nonsurgical ones. For surgical patients in this study, we can regard patients with a Caprini score of ≥ 5 as having the highest-level risk of developing DVT. In nonsurgical patients, predicting DVT using a cumulative risk score of ≥ 4 is recommended. A retrospective case-control study among medical inpatients admitted to a large general hospital in China included 902 patients with confirmed VTE during hospitalization; 902 controls were randomly selected and matched with cases. Analyses of ROC curves showed that the AUC was 0.71 (95% CI, 0.69–0.73) and a Caprini score of 4 was the cutoff point providing the highest sensitivity and specificity16). These results are similar to our findings among nonsurgical patients. Thus, we can conclude that the universal 2010 Caprini RAM could be used to effectively stratify hospitalized Chinese patients according to DVT risk categories in a general hospital, to simplify the process of risk assessment for DVT. However, different standards of assessing the risk of DVT can be applied and appropriate precautions should be taken according to whether patients are surgical or nonsurgical patients.
This is the first large-scale multicenter study to validate the 2010 Caprini RAM among hospitalized patients in China to date. However, our study has several limitations. We only chose to validate the updated version of the Caprini RAM; it was thus difficult to determine the best version or tool without the ability to make comparisons among them. The 2010 version has not been formally validated in a large series of patients. Some studies have compared the 2010 and 2005 versions7), with controversial results. Moreover, our results indicated that the 2010 Caprini RAM is less effective in assessing DVT risk among nonsurgical patients than surgical ones. Further investigation of the 2010 Caprini RAM should be conducted, or some items revised, to improve its accuracy and validity among non-surgical patients. In addition, some researchers have rightfully criticized the Caprini RAM for its complexity and the time required to query patients regarding all of its included factors. In the future, additional data must be collected and analyzed to provide generalizable conclusions, to help determine the most suitable RAM for predicting VTE risk in the Chinese population17).
Conclusion
To the best of our knowledge, this is the first large-scale multicenter study to validate the 2010 Caprini RAM among hospitalized patients in China. Our study findings suggest that the 2010 Caprini RAM can be effectively used to stratify hospitalized Chinese patients according to DVT risk categories, based on individual risk factors. Classification of the highest risk level using a cumulative risk score of ≥ 4 and ≥ 5 provides significantly more clinical information in nonsurgical patients and surgical patients, respectively.
Acknowledgements and Notice of Grant Support
This study was supported by the National Health and Family Planning Commission (Beijing, China) [grant numbers 201502017]. We sincerely acknowledge the collaboration and support received from the staff and patients of the 25 included hospitals. We also thank Analisa Avila, ELS, of Liwen Bianji, Edanz Group China (www.liwenbianji.cn/ac), for editing the English text of a draft of this manuscript.
Conflict of Interest
None.
References
- 1). Lee WS, Kim KI, Lee HJ, Kyung HS, Seo SS: The incidence of pulmonary embolism and deep vein thrombosis after knee arthroplasty in Asians remains low: a meta-analysis. Clin Orthop Relat Res, 2013; 471: 1523-1532 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2). Angchaisuksiri P: Venous thromboembolism in Asia--an unrecognised and under-treated problem? Thromb Haemost, 2011; 106: 585-590 [DOI] [PubMed] [Google Scholar]
- 3). Aggarwal A, Fullam L, Brownstein AP, Maynard GA, Ansell J, Varga EA, Friedman RJ, Rickles FR: Deep vein thrombosis (DVT) and pulmonary embolism (PE): awareness and prophylaxis practices reported by patients with cancer. Cancer Invest, 2015; 33: 405-410 [DOI] [PubMed] [Google Scholar]
- 4). Caprini JA: Thrombosis risk assessment as a guide to quality patient care. Dis Mon, 2005; 51: 70-78 [DOI] [PubMed] [Google Scholar]
- 5). Caprini JA: Risk assessment as a guide for the prevention of the many faces of venous thromboembolism. Am J Surg, 2010; 199: S3-10 [DOI] [PubMed] [Google Scholar]
- 6). Zhou HX, Peng LQ, Yan Y, Yi Q, Tang YJ, Shen YC, Feng YL, Wen FQ: Validation of the Caprini risk assessment model in Chinese hospitalized patients with venous thromboembolism. Thromb Res, 2012; 130: 735-740 [DOI] [PubMed] [Google Scholar]
- 7). Jacobs B, Pannucci C: Scoring Systems for Estimating Risk of Venous Thromboembolism in Surgical Patients. Semin Thromb Hemost, 2017; 43: 449-459 [DOI] [PubMed] [Google Scholar]
- 8). Pannucci CJ, Barta RJ, Portschy PR, Dreszer G, Hoxworth RE, Kalliainen LK, Wilkins EG: Assessment of postoperative venous thromboembolism risk in plastic surgery patients using the 2005 and 2010 Caprini Risk score. Plast Reconstr Surg, 2012; 130: 343-353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9). Bahl V, Hu HM, Henke PK, Wakefield TW, Campbell DA, Jr., Caprini JA: A validation study of a retrospective venous thromboembolism risk scoring method. Ann Surg, 2010; 251: 344-350 [DOI] [PubMed] [Google Scholar]
- 10). Gussoni G, Campanini M, Silingardi M, Scannapieco G, Mazzone A, Magni G, Valerio A, Iori I, Ageno W, Group GS: In-hospital symptomatic venous thromboembolism and antithrombotic prophylaxis in Internal Medicine. Findings from a multicenter, prospective study. Thromb Haemost, 2009; 101: 893-901 [PubMed] [Google Scholar]
- 11). Barbar S, Prandoni P: Scoring Systems for Estimating Risk of Venous Thromboembolism in Hospitalized Medical Patients. Semin Thromb Hemost, 2017; 43: 460-468 [DOI] [PubMed] [Google Scholar]
- 12). Cohen AT, Tapson VF, Bergmann JF, Goldhaber SZ, Kakkar AK, Deslandes B, Huang W, Zayaruzny M, Emery L, Anderson FA, Jr., Investigators E : Venous thromboembolism risk and prophylaxis in the acute hospital care setting (ENDORSE study): a multinational cross-sectional study. Lancet, 2008; 371: 387-394 [DOI] [PubMed] [Google Scholar]
- 13). Bilgi K, Muthusamy A, Subair M, Srinivasan S, Kumar A, Ravi R, Kumar R, Sureshkumar S, Mahalakshmy T, Kundra P, Kate V: Assessing the risk for development of Venous Thromboembolism (VTE) in surgical patients using Adapted Caprini scoring system. Int J Surg, 2016; 30: 68-73 [DOI] [PubMed] [Google Scholar]
- 14). Zhou H, Wang L, Wu X, Tang Y, Yang J, Wang B, Yan Y, Liang B, Wang K, Ou X, Wang M, Feng Y, Yi Q: Validation of a venous thromboembolism risk assessment model in hospitalized chinese patients: a case-control study. J Atheroscler Thromb, 2014; 21: 261-272 [DOI] [PubMed] [Google Scholar]
- 15). Lobastov K, Barinov V, Schastlivtsev I, Laberko L, Rodoman G, Boyarintsev V: Validation of the Caprini risk assessment model for venous thromboembolism in highrisk surgical patients in the background of standard prophylaxis. J Vasc Surg Venous Lymphat Disord, 2016; 4: 153-160 [DOI] [PubMed] [Google Scholar]
- 16). Zhou H, Hu Y, Li X, Wang L, Wang M, Xiao J, Yi Q: Assessment of the Risk of Venous Thromboembolism in Medical Inpatients using the Padua Prediction Score and Caprini Risk Assessment Model. J Atheroscler Thromb, 2018; 25: 1091-1104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17). Wang CL, Cui FP, Li JQ, Yuan XZ, Wang J, Liu LY, Wang MX: Risk Factors for Venous Thromboembolism in Hospitalized Patients in the Chinese Population. Open Life Sciences, 2018; 13: 82-89 [DOI] [PMC free article] [PubMed] [Google Scholar]


