Abstract
The epidemic of 2019 novel coronavirus, later named as coronavirus disease (COVID-19), began in Wuhan, China in December 2019 and has spread rapidly worldwide. Early diagnosis is crucial for the management of the patients with COVID-19, but the gold standard diagnostic test for this infection, the reverse transcriptase polymerase chain reaction, has a low sensitivity and an increased turnaround time. In this scenario, chest computed tomography (CT) could play a key role for an early diagnosis of COVID-19 pneumonia. Here, we have reported a confirmed case of COVID-19 with an atypical CT presentation showing a “double halo sign,” which we believe represents the pathological spectrum of this viral pneumonia.
Keywords: COVID-19 pneumonia, SARS-CoV-2, Chest CT, Atypical CT manifestation, Case report
INTRODUCTION
Coronavirus disease (COVID-19) originated in Wuhan, Hubei Province of China in December 2019 and has spread rapidly worldwide, starting from Italy where more than 220000 confirmed cases and more than 32000 deaths have been registered to date (1,2,3). In February 2020, the World Health Organization named this new coronavirus as severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and the resulting disease as COVID-19 (4,5).
Reverse transcriptase polymerase chain reaction (RT-PCR), which is usually performed on the oropharyngeal swab, is the gold standard test for the diagnosis of COVID-19, but it has a low sensitivity and an increased turnaround time (approximately 24–48 hours). Hence, several studies have highlighted the role and usefulness of chest computed tomography (CT) for an early diagnosis of COVID-19 pneumonia (6,7,8).
We present a case of COVID-19 pneumonia with an atypical and never described CT presentation pattern. Since no personal identifiable data were reported, this study was exempted from the Institutional Review Board approval; however, we obtained written informed consent from the patient.
CASE REPORT
A 55-year-old woman with a history of cough, fever, and worsening dyspnea for 7 days, was referred to the emergency department of the Imola City Hospital.
She had no relevant medical history, except for mild arterial hypertension, which was been treated with amlodipine (5 mg/day) and valsartan/hydrochlorothiazide (160/12.5 mg/day). On admission, her body temperature was slightly elevated (38.2℃) and oxygen saturation was 93%. An arterial blood gas analysis showed the arterial partial pressure of oxygen and the fraction of inspired oxygen ratio of 301. Laboratory studies showed a normal neutrophil count (68.2%; normal range: 42.0–77.0%), mild lymphopenia (18.1%; normal range: 20.0–40.0%), an increased erythrocyte sedimentation rate (76 mm/h; normal range: < 36 mm/h), and elevated C-reactive protein level (5.77 mg/dL; normal range: < 0.50 mg/dL).
Based on an oropharyngeal swab, the patient tested positive for SARS-CoV-2 by the RT-PCR test.
Unenhanced high-resolution chest CT revealed multiple consolidations in both the lungs, mostly with nodular morphology (approximately 1–1.5 cm), but some consolidations were larger in size (the largest approximately 5 cm) with prevalent peripheral and subpleural distribution and without a clear predominance for upper or lower lung fields. All of these consolidations were surrounded by a well-defined ground-glass opacity, the “halo sign” (9,10) (Fig. 1). Numerous recent publications reporting COVID-19 pneumonia have indicated that the “halo sign” is atypical and infrequent, but not an entirely rare finding in this infection (11,12). In the right lower lobe (RLL), these consolidations showed a tendency toward confluence and at least three of them had peculiar CT features, with an organizing pneumonia (OP) like pattern represented by a rounded area of normal parenchyma or rounded ground-glass opacity surrounded by a complete ring of consolidation, known as “reversed halo sign” or “atoll sign,” a well-known pattern of OP (9,13). This was surrounded in turn by another peripheral ground-glass halo (identical to the “halo sign” of the other consolidations) that gave these lesions a peculiar target-like appearance, which we defined as “double halo sign” (Figs. 2, 3).
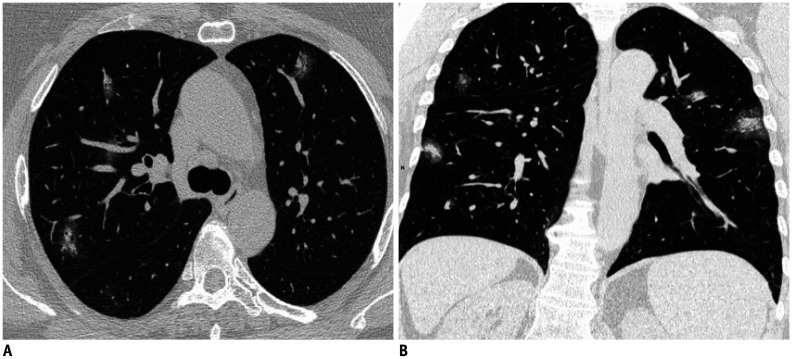
Fig. 1. Chest-CT on hospital admission.
Axial (A) and coronal (B) images show multiple bilateral rounded consolidations with surrounding well-defined ground-glass opacities (“halo sign”).
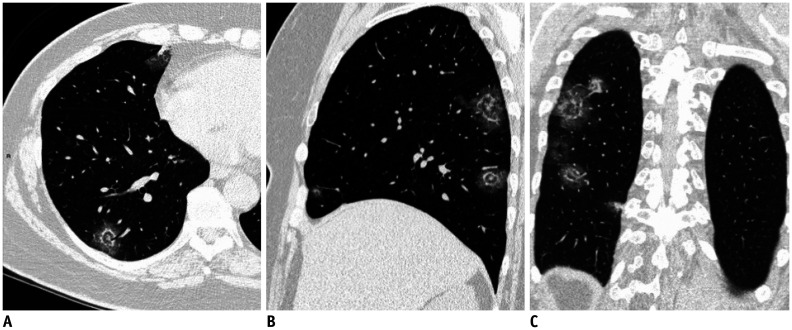
Fig. 2. Chest-CT multi-planar reconstructions of the “double halo sign.”.
Axial (A), sagittal (B), and coronal (C) images show rounded areas of normal parenchyma or rounded ground-glass opacities surrounded by a more or less complete ring of consolidation surrounded in turn by another peripheral ground-glass halo with a final target-like appearance that we defined as “double halo sign.”
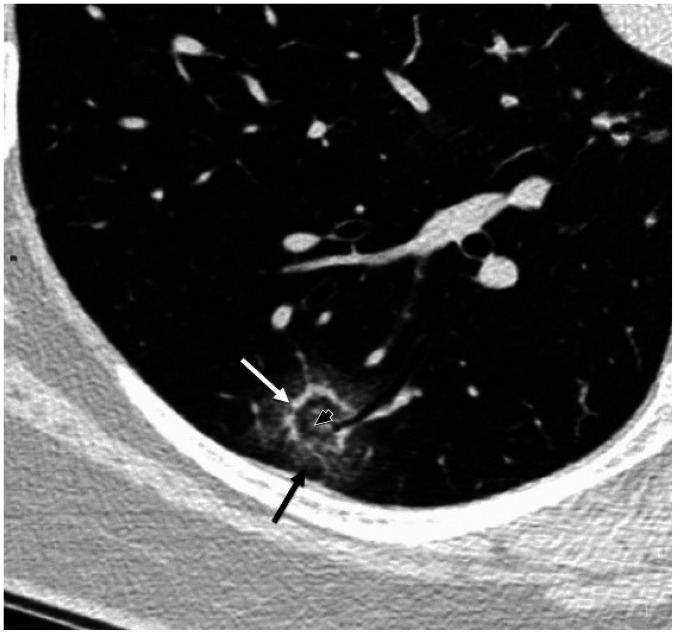
Fig. 3. Magnified view of “double halo sign,” consisting of rounded area of normal parenchyma or rounded ground-glass opacity (black arrowhead) surrounded by internal thin rim of consolidation (white arrow) and outer thick rim of ground-glass opacity (black arrow) with final target-like appearance.
The patient was treated by antiretroviral therapy with ritonavir (100 mg/day), darunavir (800 mg/day), hydroxychloroquine (200 mg twice/day), and piperacillin-tazobactam (4.5 g four times/day). Because of the progressive improvement of the patient, and to minimize radiation exposure, a follow-up chest CT was not advised and the patient was discharged after 10 days of hospitalization in a stable condition.
DISCUSSION
The gold standard test for the diagnosis of COVID-19 is RT-PCR, as described previously. However, this test has several limitations, including a low and extremely variable sensitivity depending on many factors, such as the site and quality of sampling, duration of disease, patient's immune status, or degree of viral multiplication and an increased turnaround time (at least 24 hours), which can delay the patient isolation and the proper clinical interventions. In this scenario, CT imaging plays a key role in the diagnosis and management of these patients, and several studies have reported a high sensitivity of chest CT not only in patients with confirmed COVID-19 infection, but also in asymptomatic patients with known exposure or in patients with high clinical suspicion but inconclusive laboratory test results (6,7,8,14,15,16).
Based on the current literature, typical CT manifestations of COVID-19 include diffuse or patchy ground-glass opacities, with or without consolidations or thickening of intralobular septa (“crazy paving” pattern), with prevalent peripheral distribution (involving the outer third of the lung) and with multifocal and bilateral involvement. However, the CT findings can change drastically depending on factors, such as duration of the infection and stage of disease, patient's age, and/or pre-existing lung disease (14,15,16,17).
All the CT signs detected in this case (the “halo sign,” “reversed halo sign,” or “atoll sign”) are reported with variable, but not negligible frequency in COVID-19 pneumonia (11,12,14,15,16). However, to the best of our knowledge, the CT presentation pattern with areas of OP consisting of a double halo (one solid, the “reversed halo sign” and another of pure ground-glass halo, the “halo sign”) has never been described in the literature pertaining to COVID-19 or in other lung pathologies. We believe this sign represents the pathological spectrum of COVID-19 pneumonia. In fact, as highlighted in some recent studies based on the pathological findings (18,19,20), it is possible to find not only areas of OP in the lungs of these patients corresponding to consolidations with a “reversed halo sign” in CT images, but also extensive thrombotic damage of the pulmonary microcirculation, which can explain both the “halo sign” of the bilateral consolidations and the second ground-glass halo of the lesions in the RLL.
In conclusion, large-scale studies focusing on atypical CT manifestations of COVID-19 pneumonia could offer new perspectives for a better understanding of this infection that has rapidly spread worldwide.
Footnotes
Conflicts of Interest: The authors have no potential conflicts of interest to disclose.
References
- 1.Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Holshue ML, DeBolt C, Lindquist S, Lofy KH, Wiesman J, Bruce H, et al. First case of 2019 novel coronavirus in the United States. N Engl J Med. 2020;382:929–936. doi: 10.1056/NEJMoa2001191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Covid-19, situation report update at 22 May 2020. Ministero della salute della Repubblica Italiana Web site. 2020. May 22, [Accessed June 3, 2020]. http://www.salute.gov.it/portale/news/p3_2_1_1_1.jsp?lingua=italiano&menu=notizie&p=dalministero&id=4801.
- 4.WHO director-general's remarks at the media briefing on 2019-nCoV on 11 February 2020. World Health Organization Web site. 2020. Feb 11, [Accessed May 10, 2020]. www.who.int/dg/speeches/detail/who-director-general-s-remarks-at-the-media-briefing-on-2019-ncov-on-11-february-2020.
- 5.Naming the 2019 coronavirus. International Committee on Taxonomy of Viruses (ICTV) Web site. 2020. Feb 11, [Accessed May 10, 2020]. https://talk.ictvonline.org/?Redirected=true.
- 6.Watson J, Whitining PF, Brush JE. Interpreting a COVID-19 test result. BMJ. 2020;369:m1808. doi: 10.1136/bmj.m1808. [DOI] [PubMed] [Google Scholar]
- 7.Chen D, Jiang X, Hong Y, Wen Z, Wei S, Peng G, et al. Can chest CT features distinguish patients with negative from those with positive initial RT-PCR results for coronavirus disease (COVID-19)? AJR Am J Roentgenol. 2020 May 05; doi: 10.2214/AJR.20.23012. [Epub] [DOI] [PubMed] [Google Scholar]
- 8.Fang Y, Zhang H, Xie J, Lin M, Ying L, Pang P, et al. Sensitivity of chest CT for COVID-19: comparison to RT-PCR. Radiology. 2020 Feb 19; doi: 10.1148/radiol.2020200432. [Epub] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hansell DM, Bankier AA, MacMahon H, McLoud TC, Müller NL, Remy J. Fleischner Society: glossary of terms for thoracic imaging. Radiology. 2008;246:697–722. doi: 10.1148/radiol.2462070712. [DOI] [PubMed] [Google Scholar]
- 10.Primack SL, Hartman TE, Lee KS, Müller NL. Pulmonary nodules and the CT halo sign. Radiology. 1994;190:513–515. doi: 10.1148/radiology.190.2.8284408. [DOI] [PubMed] [Google Scholar]
- 11.Chung M, Bernheim A, Mei X, Zhang N, Huang M, Zeng X, et al. CT imaging features of 2019 novel coronavirus (2019-nCoV) Radiology. 2020;295:202–207. doi: 10.1148/radiol.2020200230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lei J, Li J, Li X, Qi X. CT imaging of the 2019 novel coronavirus (2019-nCoV) pneumonia. Radiology. 2020;295:18. doi: 10.1148/radiol.2020200236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zompatori M, Poletti V, Battista G, Diegoli M. Bronchiolitis obliterans with organizing pneumonia (BOOP), presenting as a ring-shaped opacity at HRCT (the atoll sign). A case report. Radiol Med. 1999;97:308–310. [PubMed] [Google Scholar]
- 14.Ye Z, Zhang Y, Wang Y, Huang Z, Song B. Chest CT manifestations of new coronavirus disease 2019 (COVID-19): a pictorial review. Eur Radiol. 2020 Mar 19; doi: 10.1007/s00330-020-06801-0. [Epub] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kanne JP, Little BP, Chung JH, Elicker BM, Ketai LH. Essentials for radiologists on COVID-19: an update-radiology scientific expert panel. Radiology. 2020 Feb 27; doi: 10.1148/radiol.2020200527. [Epub] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Salehi S, Abedi A, Balakrishnan S, Gholamrezanezhad A. Coronavirus disease 2019 (COVID-19) imaging reporting and data system (COVID-RADS) and common lexicon: a proposal based on the imaging data of 37 studies. Eur Radiol. 2020 Apr 28; doi: 10.1007/s00330-020-06863-0. [Epub] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bernheim A, Mei X, Huang M, Yang Y, Fayad ZA, Zhang N, et al. Chest CT findings in coronavrus disease-19 (COVID-19): relationship to duration of infection. Radiology. 2020;295:200463. doi: 10.1148/radiol.2020200463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Xu Z, Shi L, Wang Y, Zhang J, Huang L, Zhang C, et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir Med. 2020;8:420–422. doi: 10.1016/S2213-2600(20)30076-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tian S, Hu W, Niu L, Liu H, Xu H, Xiao SY. Pulmonary pathology of early-phase 2019 novel coronavirus (COVID-19) pneumonia in two patients with lung cancer. J Thorac Oncol. 2020;15:700–704. doi: 10.1016/j.jtho.2020.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhang H, Zhou P, Wei Y, Yue H, Wang Y, Hu M, et al. Histopathologic changes and SARS-CoV-2 immunostaining in the lung of a patient with COVID-19. Ann Intern Med. 2020;172:629–632. doi: 10.7326/M20-0533. [DOI] [PMC free article] [PubMed] [Google Scholar]