Abstract
Coronavirus disease 2019 (COVID-19) is a transmissible respiratory disease that was initially reported in Wuhan, China in December 2019. With the alarming levels of COVID-19 spread worldwide, the World Health Organization characterized COVID-19 as a pandemic. Over the past several months, chest CT has played a vital role in early identification, disease severity assessment, and dynamic disease course monitoring of COVID-19. The published data has enriched our knowledge on the etiology, epidemiology, clinical manifestations, and pathologic findings of COVID-19. Additionally, as the imaging spectrum of the disease continues to be defined, extrapulmonary infections or other complications will require further attention. This review aims to provide an updated framework and essential knowledge with which radiologists can better understand COVID-19.
Keywords: Coronavirus, Infections, Radiology, Pandemic
INTRODUCTION
Coronavirus disease 2019 (COVID-19), caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), was initially reported in Wuhan, China. Following the initial outbreak, the virus rapidly spread throughout China, before being reported by many other countries and territories worldwide (1,2,3,4). The World Health Organization (WHO) promptly declared COVID-19 a Public Health Emergency of International Concern on January 30, 2020 (5), and raised the global risk level of COVID-19 to “very high” on February 16, 2020 when a rapid worldwide spread emerged (6). To date, the epidemic progress of COVID-19 in China has come under preliminary control, whereas the alarming levels of spread and severity worldwide have caused great distress and wider public health concerns. Thereafter, the WHO characterized COVID-19 as a pandemic on March 11, 2020 (7).
During the early outbreak in China, chest CT played a key role in the detection of COVID-19, prompting rapid prevention, control, and response measures (8). However, the reference standard for diagnosis remains reverse transcription polymerase chain reaction (RT-PCR) positive for the viral RNA (9). Many published studies and case reports have shown that chest CT is also of great clinical value in the dynamic assessment of disease course and severity (10,11). Therefore, radiologists will play a key role in combating the pandemic and should keep their knowledge up to date with the newly published data. This review provides an updated framework and essential knowledge to help radiologists better understand the etiology, epidemiology, clinical manifestations, and pathology of COVID-19. Most importantly, it highlights the radiological findings and the potential effects of chest CT on the management of suspected and confirmed patients, with future challenges also discussed.
Etiology of COVID-19
The pathogen was recognized as a novel enveloped RNA beta-coronavirus sharing 96% sequence identity to the bat coronavirus RaTG13 (2), and was later officially named SARS-CoV-2 (12). Similar to severe acute respiratory syndrome coronavirus (SARS-CoV), SARS-CoV-2 infection depends on the affinity of the host cell receptor, angiotensin-converting enzyme 2, which is highly expressed in alveolar epithelial cells (13). Coronavirus spike (S) glycoproteins promote virus entry into cells, and comprise two functional subunits responsible for binding to the host cell receptor (S1subunit) and fusion of the viral and cellular membranes (S2subunit). As most glycans in the S1subunit, and all glycans in the S2subunit, are conserved among SARS-CoV-2 S and SARS-CoV S (14), SARS-CoV-2 S was also shown to be primed by TMPRSS2 as SARS-CoV (13,15). However, the SARS-CoV-2 S glycoprotein harbors a furin cleavage site at the boundary between the S1/S2subunits, which is processed during biogenesis and sets this virus apart from SARS-CoV (16). Further research speculated that the expression of furin-like proteases could participate in expanding SARS-CoV-2 in cells and tissue tropism, as well as increase its transmissibility and/or alter its pathogenicity (14).
Epidemiology of COVID-19
Since first reported in Wuhan, China, in late December 2019, COVID-19 confirmed cases grew rapidly from January 10–22, 2020. The spread from Wuhan to the whole of China peaked and plateaued between January 23 and 27, 2020. At present, China has passed the climax of the outbreak, largely due to active public health interventions, such as early detection of cases, contact tracing, and behavioral changes in the population. However, in the following weeks, the epicenter of the pandemic shifted to Europe, and new countries reported COVID-19 outbreaks on a large scale, and cases worldwide exceeded 200000 on March 19, 2020 (17). It took over 3 months to reach the first 100000 confirmed cases, and only 12 days to reach the next 100000. As of May 21, 2020, the United States of America is the worst-hit country with confirmed cases of over 1.5 million, which accounts for more than a third of global cases, followed by Spain. Until now, COVID-19 has resulted in 323256 deaths (18), which is hundreds of times more than those reported from severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome (MERS) combined (1632) (19). Figure 1 presents the epidemiology of COVID-19 outbreaks.
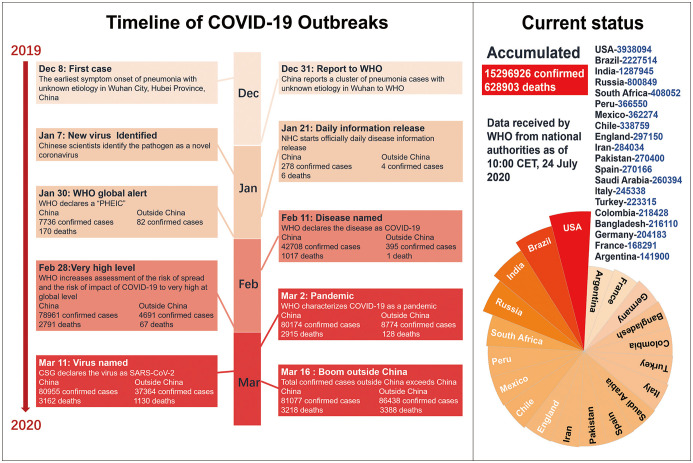
Fig. 1. Epidemiology of COVID-19 outbreaks.
Event timeline for COVID-19 outbreak from onset of symptoms in first case on December 8, 2019 to current status as of July 24, 2020 in some of most affected countries. America = United States of America, CET = Greenwich mean time, COVID-19 = coronavirus disease 2019, CSG = Coronavirus Study Group, NHC = China National Health Commission, PHEIC = Public Health Emergency of International Concern, SARS-CoV-2 = severe acute respiratory syndrome coronavirus 2, WHO = World Health Organization
Many uncertainties remain in regard to the estimated basic reproduction number, but researchers believe SARS-CoV-2 infects at least two secondary cases for each primary case. This includes a 60% transmission rate for asymptomatic or minimally symptomatic carriers, which could further lead to new outbreaks (20,21). It is worth noting that a proportion of recovered patients may still be virus carriers, but it is currently unknown whether they remain infectious at that stage (22). The primary mode of transmission of SARS-CoV-2 is via droplets and close contact, but the virus has also been found in stool and blood which has raised questions about other potential transmission routes (23). Moreover, aerosol and fomite transmission of SARS-CoV-2 has been shown to be plausible (24). The remarkable ease of human-to-human transmission led to numerous instances of clustering COVID-19 cases, with a particularly large outbreak on the Diamond Princess cruise ship as a typical example (25). In the early stage of the outbreak, researchers worked on identifying susceptible populations, but concluded that everyone was assumed to be susceptible. Some reports showed that patients in a systemic immunosuppressed state (e.g., cancer patients) were more susceptible to infection (26), while patients with inflammatory bowel disease using biologics and immunosuppressive agents did not appear to be more susceptible (27).
Clinical Features of COVID-19
The report from the Chinese Center for Disease Control and Prevention (China CDC) showed that 87% patients were 30 years to 79 years, only 1% were 9 years or younger, and only 3% were 80 years or older (28). The median incubation period is estimated to be 5.1 days (29), and patients tend to have fever and cough on admission, with a median duration of 12.0 days (8.0–13.0) and 19.0 days (12.0–23.0), respectively. These symptoms are generally followed by continued sputum production and fatigue (30). A recent study reported that 32% (12/38) of patients demonstrated ocular manifestations, such as epiphora, conjunctival congestion, or chemosis; these symptoms were especially prominent in patients with more severe systemic manifestations (31). Common laboratory findings included lymphopenia, prolonged prothrombin time, and elevated lactate dehydrogenase.
Two summaries of a report including 44672 cases from China CDC, and a report including 22512 cases from Italy (28,32) reported that no deaths occurred in the group aged 9 years and younger. However, those aged 80 years and older had a case-fatality rate of approximately 15% to 20% (28,32). This data corroborates other recent studies that suggested that increased age may be a risk factor for poor clinical outcomes (33,34). Moreover, it is speculated that for patients with underlying comorbidities, such as cardiovascular disease, diabetes, or chronic respiratory disease, SARS-CoV-2 infection might act as a precipitating factor to worsen the condition and lead to death (35,36). Certain complications (acute cardiac injury and acute respiratory distress syndrome), and the rise of biochemical indicators indicating disease progression (neutrophils, serum amyloid A, procalcitonin, C-reactive protein, serum hypersensitive troponin I, D-dimer, and lactate dehydrogenase) were shown to be factors that predispose affected individuals to adverse clinical outcomes (33,37,38,39).
To date, an increasing number of studies put an emphasis on pediatric infection. The two initial studies produced very different results with small samples (40,41), while the latter study showed that most infected children appear to have a milder clinical course and 16% (27/171) were asymptomatic (42). This finding concurred with another study with a sample size of 731 laboratory-confirmed cases that showed that over 90% of all patients were asymptomatic, mild, or moderate cases. Children at all ages appeared susceptible to COVID-19, but young children, particularly infants, were more vulnerable to infection (43).
Pathological Findings of COVID-19
There was limited data available on the pathological findings of COVID-19 at the time of this writing. Only one study of a patient who died of severe infection with COVID-19 pathologically showed hyaline membrane formation and bilateral diffuse alveolar damage with cellular fibromyxoid exudates (44), which is similar to that described in SARS. Interstitial mononuclear inflammatory infiltrates, dominated by lymphocytes and multinucleated syncytial cells in the intra-alveolar spaces, were also observed (6,44).
Chest CT vs. RT-PCR Testing in the Fight Against COVID-19
RT-PCR remains the reference standard for the diagnosis of COVID-19; however, insufficient availability and relatively low sensitivity of RT-PCR in the early stage of the initial outbreak were detrimental to the control of the pandemic. Some early reports showed that 3% (5/167) and 29% (15/51) of patients presented with an initially abnormal chest CT with ground-glass opacities (GGO) but negative RT-PCR results (45,46). Caruso et al. (47) and Ai et al. (48) reported that chest CT had the same sensitivity, i.e., 97%, for detecting COVID-19; hence, CT was suggested to be used as an important complement to RT-PCR assay due to its wide availability and relatively consistent, albeit non-specific, CT imaging patterns of COVID-19 lung involvement (49). A recent meta-regression analysis demonstrated that the pooled sensitivity was 94% for chest CT and 89% for RT-PCR, while the pooled specificity was 37% for chest CT. Specifically, in countries with a prevalence less than 10%, the positive predictive value of RT-PCR was more than 10-fold higher than that of CT scans (50). These results implied that the use of chest CT scans in low-prevalence regions could induce a large number of false-positive results, which coincided with the statements from the Society of Thoracic Radiology and American Society of Emergency Radiology that routine CT screening was not recommended for the diagnosis of COVID-19 (51). The Fleischner Society also published a multinational consensus statement that highlighted that CT was mainly indicated for patients with moderate to severe features of COVID-19, regardless of RT-PCR test results, as well as for patients with COVID-19 and evidence of worsening respiratory status. RT-PCR testing is indicated in patients who were incidentally found to have findings suggestive of COVID-19 on a chest CT scan (52).
Chest CT Features of COVID-19
Chest CT Findings at Baseline
It is important to be aware of the imaging findings of COVID-19 that can trigger a timely response of prevention and control, especially for asymptomatic patients. As previously described (7,47,53,54,55,56,57,58,59), the most common CT findings of COVID-19 include bilateral lung involvement, GGO, and consolidative pulmonary opacities, which are mainly located peripherally (Fig. 2). Lung alveoli filled with blood, pus, water, or cells is recognized as the pathological basis of GGO, which are observed in 65–90% of confirmed COVID-19 patients (Table 1), while the appearance of consolidation indicates that the alveoli are completely filled with inflammatory exudate (59). The features of the opacities are also diverse, including rounded and linear morphology, a “crazy-paving” pattern, and the reverse CT halo sign. Pleural effusion, pericardial effusion, air bronchogram, and lymphadenopathy were initially reported but later found in only a very small number of cases with disease progression (55,56,57,58). Pulmonary fibrosis, cavitation, and calcification have not been reported. Furthermore, most pulmonary lesions of COVID-19 involve bilateral lungs and multiple lung lobes, which is different from SARS which typically demonstrates a unifocal opacity (60). Chest CT findings also showed a posterior and peripheral predominant distribution (55), with the right lower lobes most commonly affected due to the shortness and straightness of the right bronchus.
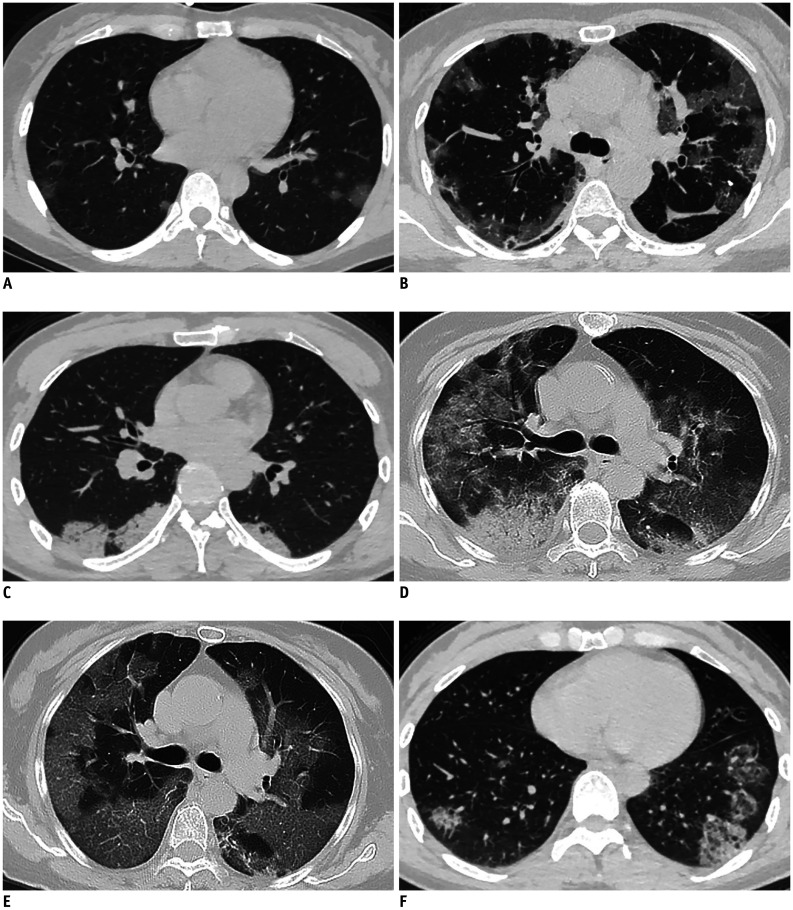
Fig. 2. Chest CT findings of COVID-19.
(A) Multifocal GGO with subpleural distribution, (B) patchy GGO with subpleural bands, (C) multifocal subpleural consolidations, (D) diffuse GGO and consolidation, (E) crazy-paving pattern, and (F) reversed halo sign. GGO = ground-glass opacities
Table 1. Summary of Chest CT Imaging Features of Coronavirus Disease 2019.
| Literature Presentation | Total | |||||||
|---|---|---|---|---|---|---|---|---|
| Ng et al. (53), n = 21 | Chung et al. (54), n = 21 | Pan et al. (10), n = 21 | Shi et al. (56), n = 81 | Bernheim et al. (57), n = 121 | Xu et al. (58), n = 90 | Wu et al. (59), n = 80 | ||
| Most common CT characteristic, n (%) | ||||||||
| Ground-glass opacification | 18 (86) | 18 (86) | 18 (75) | 53 (65) | 91 (75) | 65 (72) | 73 (91) | 336 (77) |
| Consolidation | 13 (62) | 6 (29) | 10 (42) | 14 (17) | 52 (43) | 12 (13) | 50 (63) | 157 (36) |
| Crazy-paving pattern | N/A | 4 (19) | 6 (25) | 8 (10) | 6 (5) | 11 (12) | 23 (29) | 58 (14) |
| Less common CT characteristic, n (%) | ||||||||
| Normal | 2 (10) | 3 (14) | 4 (17) | 0 (0) | 24 (20) | 21 (23) | 4 (5) | 58 (13) |
| Lymphadenopathy | 0 (0) | 0 (0) | 0 (0) | 5 (6) | 0 (0) | 1 (1) | 3 (4) | 9 (2) |
| Pleural effusion | 0 (0) | 0 (0) | N/A | 4 (5) | 1 (1) | 4 (4) | 5 (6) | 14 (3) |
| Predominant distribution, n (%) | ||||||||
| Bilateral | N/A | 16 (76) | 10 (42) | 64 (79) | 73 (60) | 53 (59) | N/A | 216 (65) |
| Peripheral | 18 (86) | 7 (33) | 13 (54) | 44 (54) | 63 (52) | 46 (51) | N/A | 191 (54) |
N/A = unavailable
Some reports showed that younger adults tended to have more GGO, while older adults tended to have more areas of lung involvement and more consolidation (55,61). Compared to adults, pediatric patients showed fewer CT findings with a relatively small and limited distribution, but a higher frequency of bronchial wall thickening and peribronchial distribution (41,42). Table 1 summarizes the characteristic chest CT features of COVID-19. However, these CT features of COVID-19 are nonspecific, and the diagnosis should depend on epidemiological history, clinical, imaging, and etiological findings (62,63).
In patients suspicious for COVID-19 with sudden onset of dyspnea and hypoxemia, respiratory deterioration with other clinical evidence of venous thrombosis should raise suspicion for pulmonary embolism (64,65). As patients are admitted for treatment and isolation, prophylactic measures for avoiding venous thromboembolism should be taken. Mediastinal emphysema, giant bulla, and pneumothorax have also been shown to develop during the course of COVID-19 pneumonia (11,66). Extrapulmonary infections or complications also need to be taken into account. Indeed, Poyiadji et al. (67) recently reported the first case of presumptive COVID-19-associated acute necrotizing hemorrhagic encephalopathy. Images from brain MRI demonstrated hemorrhagic rim enhancing multifocal lesions with bilateral thalamic involvement (67). While it is a rare encephalopathy, clinicians and radiologists should be watching for this presentation among patients presenting with COVID-19 and altered mental status, as the number of patients with COVID-19 increases worldwide.
Evaluation of Disease Severity
CT can evaluate the disease severity and provide prognostic information. Chang et al. (68) initially proposed a CT severity score system during the outbreak of SARS, which was assigned on the basis of all abnormal lung areas involved; this has now been adopted to semi-quantitatively estimate the pulmonary involvement of COVID-19. Many studies (10,69) have shown that the CT severity score was significantly higher in severe/critical COVID-19 patients or patients in the peak course stage, suggesting that a higher CT severity score on admission may be an independent predictor for progression in severely ill patients. Yang et al. (70) further confirmed that the optimal threshold of the CT severity score for identifying at-risk COVID-19 patients was 19.5 with 83.3% sensitivity, 94% specificity, and an area under the curve of 0.892. Furthermore, compared to moderately ill patients, severe/critical patients had a higher rate of bilateral pulmonary involvement (29,71). In addition to the degree of lung involvement, some CT imaging patterns could also indicate disease severity. Indeed, Guan et al. (29) found that severely ill patients demonstrated a higher rate of interstitial abnormalities than non-severe patients on chest CT. Currently accumulated data show that consolidation, linear opacities, a crazy-paving pattern, bronchial wall thickening, and extrapulmonary lesions are imaging features of severely and critically ill COVID-19 patients (69). Incidences of lymphadenopathy, pleural effusion, and pericardial effusion in severe/critical patients were also higher than those with moderate disease, which is consistent with the previous MERS, SARS, and H5N1 studies showing that the presence of pleural effusion or lymphadenopathy were poor prognostic indicators (72,73).
Evaluation of Disease Course
Some reports have illustrated the disease course of COVID-19, which has helped in elucidating the natural history of the disease. For discharged patients, the most common pattern of disease evolution on chest CT is an initial progression from an early, mild stage to a peak level, followed by radiological improvement (10,56). Typical mild COVID-19 pneumonia generally starts as unilateral or bilateral multifocal GGO distributed peripherally in the lower lobes. However, some patients demonstrated an initially normal chest CT, with imaging findings that subsequently became increasingly apparent as the course of infection progressed. The progression of disease always presented as greater lung involvement, increased density, and new onset lesions. GGO quickly coalesced into dense consolidative opacities and then progressively evolved to interstitial septal thickening, a crazy-paving pattern and/or the reverse CT halo sign (74), which serves as an indicator of disease progression. The peak level is generally reached around 10 days after the onset of symptoms, with the coexistence of mixed imaging patterns, but without obvious progression (10,75). As the disease progresses into the recovery stage and the infection becomes controlled, lesions are gradually absorbed with residual GGO, fibrous stripes, bronchial wall thickening, and interlobular septal thickening. These findings are considered to represent imaging evidence of improvement (55,56,57,76). Wang et al. (75) found that 94% (66/70) of patients discharged with residual disease on final chest CT scans had GGO as the predominant pattern. Figure 3 shows the disease recovery course of one representative case with confirmed COVID-19 who was safely discharged.
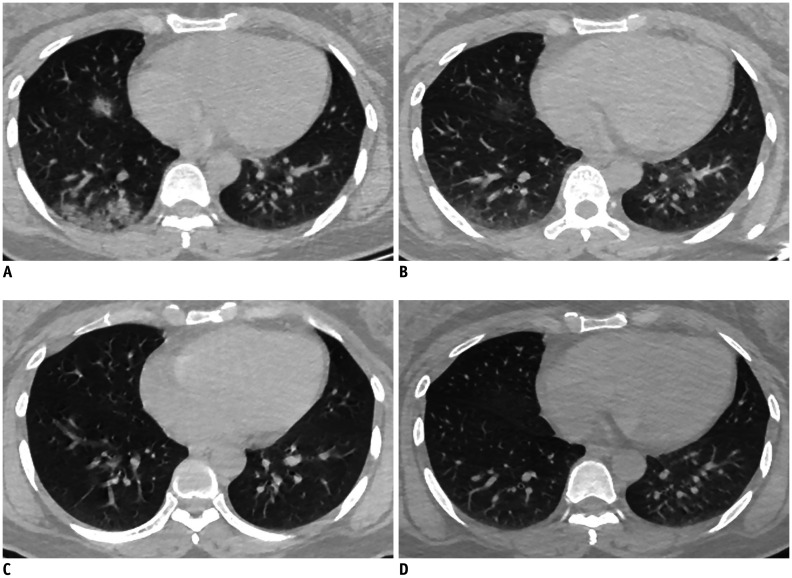
Fig. 3. Confirmed COVID-19 in 37-year-old woman with fever and fatigue.
A. Chest CT study obtained 7 days after symptom onset (2020-1-29) shows multiple consolidations in right lung. B. Chest CT image obtained 10 days later (2020-2-8) shows resolution of consolidation. C, D. Chest CT images obtained 6 days (2020-2-14) and 10 days (2020-2-18) later showing recovery from disease. Patient was discharged 2 days after second CT scan.
For a proportion of patients with worsening disease, patients tended to demonstrate progressive radiographic deterioration without any sign of improvement (56). Lesions rapidly evolved to bilateral, diffuse heterogeneous consolidations, and GGO with air-bronchogram sign and bronchiectasis, instead of a variable degree of resolution of opacification and thickened interlobular septa (56). In the later stages of the disease, large lobular and subsegmental areas of consolidation with increased opacity presented as “white lung,” and the incidence of pleural effusion was common (74). If treatment was not received promptly, or if immunity failed to fight off the virus, the patient's condition became life-threatening, especially for those with multiple comorbidities. Figure 4 shows the progressive radiographic deterioration process in one patient who died of COVID-19.
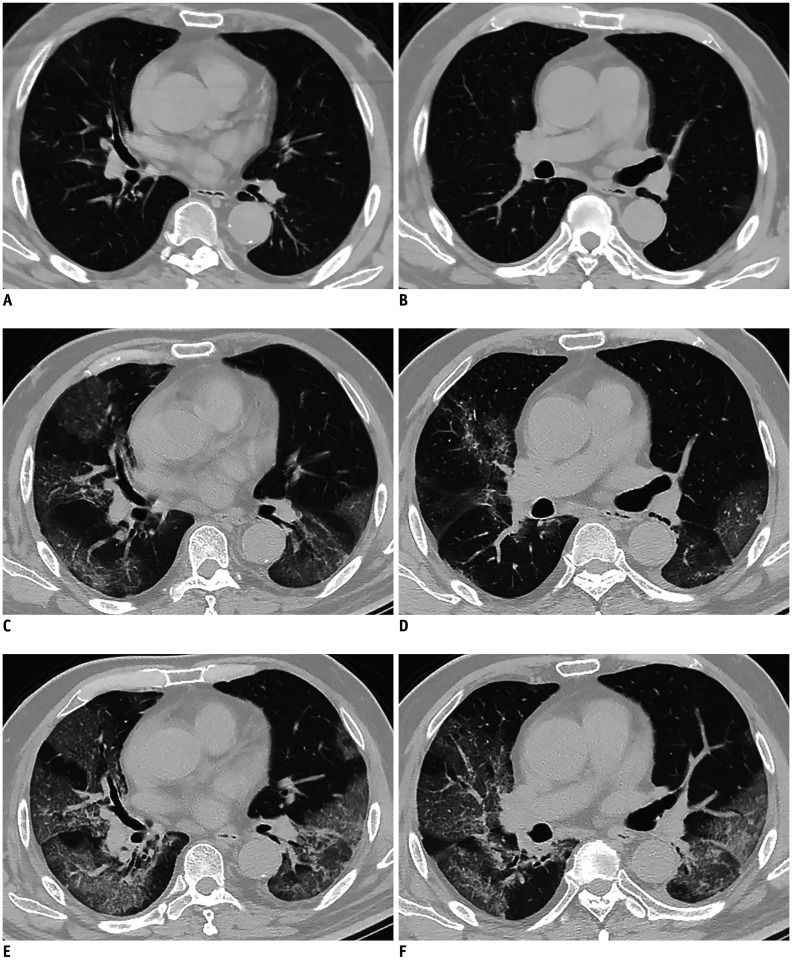
Fig. 4. Confirmed COVID-19 in 63-year-old man with fever, cough, and diarrhea.
A, B. Chest CT images obtained 8 days after symptom onset (2020-2-7) show multifocal hazy GGO in both lungs. C, D. Chest CT images obtained 3 days later (2020-2-10) show expansion of bilateral pulmonary lesions with subpleural consolidation and peripheral GGO. E, F. Chest CT images obtained 2 days later (2020-2-12) show disease progression, with more extensive and more dense pulmonary consolidations, with interlobular and intralobular septal thickening. Patient died 12 days after final CT scan.
Chest Radiographic Findings of COVID-19
There is an abundance of literature describing CT findings in the preliminary stage of COVID-19 infection, due to the preferential use of chest CT over chest X ray (CXR) in China, which may be the result of the limited sensitivity of CXR in the diagnosis of infection and the relatively easy access to CT in China. However, CXR is still given priority in many countries experiencing the current pandemic (77,78). Wong et al. (78) reviewed 64 patients and found that the sensitivity of baseline CXR was 69% (44/64), lower than that of initial RT-PCR (91%); however, six patients (9%) demonstrated CXR abnormalities prior to eventual positive RT-PCR results. Different to chest CT with GGO as the predominant feature, current studies show that on CXR, consolidation is the most common pattern, followed by GGO. Nevertheless, the lesions also tended to have a peripheral, bilateral, and lower zone distribution on CXR, which is consistent with CT. Furthermore, pleural effusion could be seen but is uncommon, only was found in 3% cases (2/64) (77,78,79). To quantify the extent of infection, a severity score of 0–4 was assigned to each lung depending on the extent of involvement by consolidation or GGO (0 = no involvement; 1 ≤ 25%; 2 = 25–50%; 3 = 50–75%; 4 ≥ 75% involvement). The scores for each lung were summed to produce the final severity score. CXR severity scores changed over time and peaked at 10–12 days from symptom onset on CXR, at which the median CXR severity score was 3 (78).
Artificial Intelligence can Assist with Combatting COVID-19
During the early stages of the pandemic, when it was a priority to control the spread of the outbreak, fast, safe, and accurate CT, aimed to detect large numbers of suspected cases for appropriate quarantine and treatment measures. However, the number of radiologists available for such a task was not sufficient to meet the needs of incoming patients. Artificial intelligence (AI) could complete the diagnosis in a few seconds, and shows great potential to accelerate detection and provide a mechanism of workload relief. By extracting both 2D local and 3D global representative features to provide a clinical diagnosis, Li et al. (80) developed a robust deep learning (DL) model, of which the pre-exam sensitivity and specificity for detecting COVID-19 was 90% and 96%, respectively. More importantly, the robust diagnostic performance of DL was helpful in differentiating COVID-19 and community acquired pneumonia (CAP) on chest CT images. The corresponding area under the curve values were 0.96 (95% confidence interval [CI]: 0.94, 0.99) for COVID-19 and 0.95 (95% CI: 0.93, 0.97) for CAP (80). Although CXR may be more available in less developed parts of the world, CXR is less sensitive than CT. DL approaches to augment radiographs with a color probability have been proposed to identify COVID-19-associated pneumonia/acute lung injury, highlighting subtle abnormalities that may be missed by less experienced radiologists, and triage patients for CT (81,82). These results provide evidence that AI could be a powerful tool to combat the outbreak, but further studies are still necessary to determine its performance in this scenario.
Future Challenges
Although chest CT is important during COVID-19 management, some challenges remain. Firstly, chest CT is not sufficiently reliable to be used as a standalone tool to diagnose COVID-19, and a better workflow is required to select patients for CT examination to overcome this diagnostic dilemma. Secondly, regarding the premise of meeting patients' needs, low radiation dose methods, and techniques to minimize radiation dosage should always be applied. Finally, as the outbreak has spread rapidly worldwide, international multicenter studies with larger sample sizes are needed to further reveal prognostic differences between ethnicities and populations and the natural history of COVID-19.
CONCLUSIONS
In conclusion, CT plays an important role in the early detection of COVID-19 infection, especially in appropriate settings of patient exposure or in areas of endemic disease. Bilateral distribution of GGO and consolidation are typical hallmarks of chest CT for COVID-19. Considering that CT could also help to evaluate the disease severity and course, combining AI with the power of CT for containing COVID-19 is expected to become more apparent. With enormous efforts from medical professionals, substantial public health prevention measures, and accelerated research, we hope that the day that brings the outbreak to a close will arrive soon.
Footnotes
Supported by The National Key Research and Development Program of China (2017YFC0113400 for L.J.Z.).
Conflicts of Interest: The authors have no potential conflicts of interest to disclose.
References
- 1.Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhou P, Yang XL, Wang XG, Hu B, Zhang L, Zhang W, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579:270–273. doi: 10.1038/s41586-020-2012-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Holshue ML, DeBolt C, Lindquist S, Lofy KH, Wiesman J, Bruce H, et al. First case of 2019 novel coronavirus in the United States. N Engl J Med. 2020;382:929–936. doi: 10.1056/NEJMoa2001191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Phan LT, Nguyen TV, Luong QC, Nguyen TV, Nguyen HT, Le HQ, et al. Importation and human-to-human transmission of a novel coronavirus in Vietnam. N Engl J Med. 2020;382:872–874. doi: 10.1056/NEJMc2001272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.World Health Organization. Statement on the second meeting of the International Health Regulations (2005) Emergency Committee regarding the outbreak of novel coronavirus (2019-nCoV) [Accessed March 18, 2020]. Available at: https://www.who.int/news-room/detail/30-01-2020-statement-on-the-second-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-outbreak-of-novel-coronavirus-(2019-ncov)
- 6.World Health Organization. WHO / COVID-19 UPDATE. [Accessed March 18, 2020]. Available at: https://www.unmultimedia.org/tv/unifeed/asset/2536/2536753/
- 7.World Health Organization. WHO Director-general's opening remarks at the media briefing on COVID-19 - 11 March 2020. [Accessed March 18, 2020]. Available at: https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020.
- 8.Xiang KY, Zu ZY, Lu GM, Zhang LJ. Coronavirus disease 2019 (COVID-19): Chinese radiologists are acting. J Thorac Imaging. 2020 May 01; doi: 10.1097/RTI.0000000000000528. [Epub] [DOI] [PubMed] [Google Scholar]
- 9.General Office of National Health Committee. [Notice on the issuance of a programme for the diagnosis and treatment of novel coronavirus (2019-nCoV) infected pneumonia (trial fifth edition)] [Accessed February 5, 2020]. Available at: http://www.nhc.gov.cn/yzygj/s7653p/202002/3b09b894ac9b4204a79db5b8912d4440.shtml.
- 10.Pan F, Ye T, Sun P, Gui S, Liang B, Li L, et al. Time course of lung changes at chest CT during recovery from coronavirus Disease 2019 (COVID-19) Radiology. 2020;295:715–721. doi: 10.1148/radiol.2020200370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lei P, Mao J, Huang Z, Liu G, Wang P, Song W. Key considerations for radiologists when diagnosing the novel coronavirus disease (COVID-19) Korean J Radiol. 2020;21:625–626. doi: 10.3348/kjr.2020.0190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Coronaviridae Study Group of the International Committee on Taxonomy of Viruses. The species severe acute respiratory syndrome-related coronavirus: classifying 2019-nCoV and naming it SARS-CoV-2. Nat Microbiol. 2020;5:536–544. doi: 10.1038/s41564-020-0695-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yan R, Zhang Y, Li Y, Xia L, Guo Y, Zhou Q. Structural basis for the recognition of SARS-CoV-2 by full-length human ACE2. Science. 2020;367:1444–1448. doi: 10.1126/science.abb2762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Walls AC, Park YJ, Tortorici MA, Wall A, McGuire AT, Veesler D. Structure, function, and antigenicity of the SARS-CoV-2 spike glycoprotein. Cell. 2020;181:281–292.e6. doi: 10.1016/j.cell.2020.02.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hoffmann M, Kleine-Weber H, Schroeder S, Krüger N, Herrler T, Erichsen S, et al. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell. 2020;181:271–280.e8. doi: 10.1016/j.cell.2020.02.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wrapp D, Wang N, Corbett KS, Goldsmith JA, Hsieh CL, Abiona O, et al. Cryo-EM structure of the 2019-nCoV spike in the prefusion conformation. Science. 2020;367:1260–1263. doi: 10.1126/science.abb2507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.World Health Organization. Coronavirus disease 2019 (COVID-19): situation report - 59. [Accessed March 22, 2020]. Available at: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200319-sitrep-59-covid-19.pdf?sfvrsn=c3dcdef9_2.
- 18.World Health Organization. Coronavirus disease (COVID-19): situation report - 122. [Accessed May 22, 2020]. Available at: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200521-covid-19-sitrep-122.pdf?sfvrsn=24f20e05_4.
- 19.Mahase E. Coronavirus covid-19 has killed more people than SARS and MERS combined, despite lower case fatality rate. BMJ. 2020;368:m641. doi: 10.1136/bmj.m641. [DOI] [PubMed] [Google Scholar]
- 20.Zou L, Ruan F, Huang M, Liang L, Huang H, Hong Z, et al. SARS-CoV-2 viral load in upper respiratory specimens of infected patients. N Engl J Med. 2020;382:1177–1179. doi: 10.1056/NEJMc2001737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Qiu J. Covert coronavirus infections could be seeding new outbreaks. nature; [Accessed March 22, 2020]. Available at: https://www.nature.com/articles/d41586-020-00822-x. [DOI] [PubMed] [Google Scholar]
- 22.Lan L, Xu D, Ye G, Xia C, Wang S, Li Y, et al. Positive RT-PCR test results in patients recovered from COVID-19. JAMA. 2020;323:1502–1503. doi: 10.1001/jama.2020.2783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wang W, Xu Y, Gao R, Lu R, Han K, Wu G, et al. Detection of SARS-CoV-2 in different types of clinical specimens. JAMA. 2020;323:1843–1844. doi: 10.1001/jama.2020.3786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.van Doremalen N, Bushmaker T, Morris DH, Holbrook MG, Gamble A, Williamson BN, et al. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med. 2020;382:1564–1567. doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rocklöv J, Sjödin H, Wilder-Smith A. COVID-19 outbreak on the Diamond Princess cruise ship: estimating the epidemic potential and effectiveness of public health countermeasures. J Travel Med. 2020;27:taaa030. doi: 10.1093/jtm/taaa030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Liang W, Guan W, Chen R, Wang W, Li J, Xu K, et al. Cancer patients in SARS-CoV-2 infection: a nationwide analysis in China. Lancet Oncol. 2020;21:335–337. doi: 10.1016/S1470-2045(20)30096-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mao R, Liang J, Shen J, Ghosh S, Zhu LR, Yang H, et al. Implications of COVID-19 for patients with pre-existing digestive diseases. Lancet Gastroenterol Hepatol. 2020;5:425–427. doi: 10.1016/S2468-1253(20)30076-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020 Feb 24; doi: 10.1001/jama.2020.2648. [Epub] [DOI] [PubMed] [Google Scholar]
- 29.Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wu P, Duan F, Luo C, Liu Q, Qu X, Liang L, et al. Characteristics of ocular findings of patients with coronavirus disease 2019 (COVID-19) in Hubei Province, China. JAMA Ophthalmol. 2020;138:575–578. doi: 10.1001/jamaophthalmol.2020.1291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Livingston E, Bucher K. Coronavirus disease 2019 (COVID-19) in Italy. JAMA. 2020 Mar 17; doi: 10.1001/jama.2020.4344. [Epub] [DOI] [PubMed] [Google Scholar]
- 33.Li X, Wang L, Yan S, Yang F, Xiang L, Zhu J, et al. Clinical characteristics of 25 death cases with COVID-19: a retrospective review of medical records in a single medical center, Wuhan, China. Int J Infect Dis. 2020;94:128–132. doi: 10.1016/j.ijid.2020.03.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Onder G, Rezza G, Brusaferro S. Case-fatality rate and characteristics of patients dying in relation to COVID-19 in Italy. JAMA. 2020 Mar 23; doi: 10.1001/jama.2020.4683. [Epub] [DOI] [PubMed] [Google Scholar]
- 35.Guan WJ, Liang WH, Zhao Y, Liang HR, Chen ZS, Li YM, et al. Comorbidity and its impact on 1590 patients with COVID-19 in China: a nationwide analysis. Eur Respir J. 2020;55:2000547. doi: 10.1183/13993003.00547-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.CDC COVID-19 Response Team. Preliminary estimates of the prevalence of selected underlying health conditions among patients with coronavirus disease 2019 - United States, February 12-March 28, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:382–386. doi: 10.15585/mmwr.mm6913e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Guo T, Fan Y, Chen M, Wu X, Zhang L, He T, et al. Cardiovascular implications of fatal outcomes of patients with Coronavirus Disease 2019 (COVID-19) JAMA Cardiol. 2020 Mar 27; doi: 10.1001/jamacardio.2020.1017. [Epub] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Yang X, Yu Y, Xu J, Shu H, Xia J, Liu H, et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020;8:475–481. doi: 10.1016/S2213-2600(20)30079-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Shi S, Qin M, Shen B, Cai Y, Liu T, Yang F, et al. Association of cardiac injury with mortality in hospitalized patients with COVID-19 in Wuhan, China. JAMA Cardiol. 2020 Mar 25; doi: 10.1001/jamacardio.2020.0950. [Epub] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Liu W, Zhang Q, Chen J, Xiang R, Song H, Shu S, et al. Detection of Covid-19 in children in early January 2020 in Wuhan, China. N Engl J Med. 2020;382:1370–1371. doi: 10.1056/NEJMc2003717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Xu Y, Li X, Zhu B, Liang H, Fang C, Gong Y, et al. Characteristics of pediatric SARS-CoV-2 infection and potential evidence for persistent fecal viral shedding. Nat Med. 2020;26:502–505. doi: 10.1038/s41591-020-0817-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lu X, Zhang L, Du H, Zhang J, Li YY, Qu J, et al. SARS-CoV-2 infection in children. N Engl J Med. 2020;382:1663–1665. doi: 10.1056/NEJMc2005073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Dong Y, Mo X, Hu Y, Qi X, Jiang F, Jiang Z, et al. Epidemiology of COVID-19 among children in China. Pediatrics. 2020;145:e20200702. doi: 10.1542/peds.2020-0702. [DOI] [PubMed] [Google Scholar]
- 44.Xu Z, Shi L, Wang Y, Zhang J, Huang L, Zhang C, et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir Med. 2020;8:420–422. doi: 10.1016/S2213-2600(20)30076-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Xie X, Zhong Z, Zhao W, Zheng C, Wang F, Liu J. Chest CT for typical 2019nCoV pneumonia: relationship to negative RT-PCR testing. Radiology. 2020 Feb 12; doi: 10.1148/radiol.2020200343. [Epub] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Fang Y, Zhang H, Xie J, Lin M, Ying L, Pang P, et al. Sensitivity of chest CT for COVID-19: comparison to RT-PCR. Radiology. 2020 Feb 19; doi: 10.1148/radiol.2020200432. [Epub] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Caruso D, Zerunian M, Polici M, Pucciarelli F, Polidori T, Rucci C, et al. Chest CT features of COVID-19 in Rome, Italy. Radiology. 2020 Apr 03; doi: 10.1148/radiol.2020201237. [Epub] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ai T, Yang Z, Hou H, Zhan C, Chen C, Lv W, et al. Correlation of chest CT and RT-PCR testing in coronavirus disease 2019 (COVID-19) in China: a report of 1014 cases. Radiology. 2020 Feb 26; doi: 10.1148/radiol.2020200642. [Epub] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kanne JP, Little BP, Chung JH, Elicker BM, Ketai LH. Essentials for radiologists on COVID-19: an update-radiology scientific expert panel. Radiology. 2020 Feb 27; doi: 10.1148/radiol.2020200527. [Epub] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kim H, Hong H, Yoon SH. Diagnostic performance of CT and reverse transcriptase-polymerase chain reaction for coronavirus disease 2019: a meta-analysis. Radiology. 2020 Apr 17; doi: 10.1148/radiol.2020201343. [Epub] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Society of Thoracic Radiology. STR/ASER COVID-19 position statement March 11, 2020. [Accessed May 11, 2020]. Available at: https://thoracicrad.org/
- 52.Rubin GD, Ryerson CJ, Haramati LB, Sverzellati N, Kanne JP, Raoof S, et al. The role of chest imaging in patient management during the COVID-19 pandemic: a multinational consensus statement from the Fleischner Society. Radiology. 2020 Apr 07; doi: 10.1148/radiol.2020201365. [Epub] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ng MY, Lee EY, Yang J, Yang F, Li X, Wang H, et al. Imaging profile of the COVID-19 infection radiologic findings and literature review. Radiology: Cardiothoracic Imaging. 2020 Feb 13; doi: 10.1148/ryct.2020200034. [Epub] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Chung M, Bernheim A, Mei X, Zhang N, Huang M, Zeng X, et al. CT imaging features of 2019 novel coronavirus (2019-nCoV) Radiology. 2020;295:202–207. doi: 10.1148/radiol.2020200230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Song F, Shi N, Shan F, Zhang Z, Shen J, Lu H, et al. Emerging 2019 novel coronavirus (2019-nCoV) pneumonia. Radiology. 2020;295:210–217. doi: 10.1148/radiol.2020200274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Shi H, Han X, Jiang N, Cao Y, Alwalid O, Gu J, et al. Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: a descriptive study. Lancet Infect Dis. 2020;20:425–434. doi: 10.1016/S1473-3099(20)30086-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Bernheim A, Mei X, Huang M, Yang Y, Fayad ZA, Zhang N, et al. Chest CT findings in coronavirus disease-19 (COVID-19): relationship to duration of infection. Radiology. 2020;295:200463. doi: 10.1148/radiol.2020200463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Xu X, Yu C, Qu J, Zhang L, Jiang S, Huang D, et al. Imaging and clinical features of patients with 2019 novel coronavirus SARS-CoV-2. Eur J Nucl Med Mol Imaging. 2020;47:1275–1280. doi: 10.1007/s00259-020-04735-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Wu J, Wu X, Zeng W, Guo D, Fang Z, Chen L, et al. Chest CT findings in patients with coronavirus disease 2019 and its relationship with clinical features. Invest Radiol. 2020;55:257–261. doi: 10.1097/RLI.0000000000000670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Paul NS, Roberts H, Butany J, Chung T, Gold W, Mehta S, et al. Radiologic pattern of disease in patients with severe acute respiratory syndrome: the Toronto experience. Radiographics. 2004;24:553–563. doi: 10.1148/rg.242035193. [DOI] [PubMed] [Google Scholar]
- 61.Zhu T, Wang Y, Zhou S, Zhang N, Xia L. A comparative study of chest computed tomography features in young and older adults with corona virus disease (COVID-19) J Thorac Imaging. 2020;35:W97–W101. doi: 10.1097/RTI.0000000000000513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Chen A, Huang J, Liao Y, Liu Z, Chen D, Yang C, et al. Differences in clinical and imaging presentation of pediatric patients with COVID-19 in comparison with Adults. Radiology: Cardiothoracic Imaging. 2020;2:e200117. doi: 10.1148/ryct.2020200117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Zu ZY, Jiang MD, Xu PP, Chen W, Ni QQ, Lu GM, et al. Coronavirus disease 2019 (COVID-19): a perspective from China. Radiology. 2020 Feb 21; doi: 10.1148/radiol.2020200490. [Epub] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Xie Y, Wang X, Yang P, Zhang S. COVID-19 complicated by acute pulmonary embolism. Radiology: Cardiothoracic Imaging. 2020 Mar 16; doi: 10.1148/ryct.2020200067. [Epub] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Ullah W, Saeed R, Sarwar U, Patel R, Fischman DL. COVID-19 complicated by acute pulmonary embolism and right-sided heart failure. JACC Case Rep. 2020 Apr 17; doi: 10.1016/j.jaccas.2020.04.008. [Epub] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Sun R, Liu H, Wang X. Mediastinal emphysema, giant bulla, and pneumothorax developed during the course of COVID-19 pneumonia. Korean J Radiol. 2020;21:541–544. doi: 10.3348/kjr.2020.0180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Poyiadji N, Shahin G, Noujaim D, Stone M, Patel S, Griffith B. COVID-19-associated acute hemorrhagic necrotizing encephalopathy: CT and MRI features. Radiology. 2020 Apr 17; doi: 10.1148/radiol.2020201187. [Epub] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Chang YC, Yu CJ, Chang SC, Galvin JR, Liu HM, Hsiao CH, et al. Pulmonary sequelae in convalescent patients after severe acute respiratory syndrome: evaluation with thin-section CT. Radiology. 2005;236:1067–1075. doi: 10.1148/radiol.2363040958. [DOI] [PubMed] [Google Scholar]
- 69.Li K, Wu J, Wu F, Guo D, Chen L, Fang Z, et al. The clinical and chest CT features associated with severe and critical COVID-19 pneumonia. Invest Radiol. 2020;55:327–331. doi: 10.1097/RLI.0000000000000672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Yang R, Li X, Liu H, Zhen YL, Zhang XX, Xiong QX, et al. Chest CT severity score an imaging tool for assessing severe COVID-19. Radiology: Cardiothoracic Imaging. 2020 Mar 30; doi: 10.1148/ryct.2020200047. [Epub] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Mo P, Xing Y, Xiao Y, Deng L, Zhao Q, Wang H, et al. Clinical characteristics of refractory COVID-19 pneumonia in Wuhan, China. Clin Infect Dis. 2020 Mar 16; doi: 10.1093/cid/ciaa270. [Epub] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Das KM, Lee EY, Enani MA, AlJawder SE, Singh R, Bashir S, et al. CT correlation with outcomes in 15 patients with acute Middle East respiratory syndrome coronavirus. AJR Am J Roentgenol. 2015;204:736–742. doi: 10.2214/AJR.14.13671. [DOI] [PubMed] [Google Scholar]
- 73.Qureshi NR, Hien TT, Farrar J, Gleeson FV. The radiologic manifestations of H5N1 avian influenza. J Thorac Imaging. 2006;21:259–264. doi: 10.1097/01.rti.0000213573.94032.53. [DOI] [PubMed] [Google Scholar]
- 74.Pan Y, Guan H, Zhou S, Wang Y, Li Q, Zhu T, et al. Initial CT findings and temporal changes in patients with the novel coronavirus pneumonia (2019-nCoV): a study of 63 patients in Wuhan, China. Eur Radiol. 2020;30:3306–3309. doi: 10.1007/s00330-020-06731-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Wang Y, Dong C, Hu Y, Li C, Ren Q, Zhang X, et al. Temporal changes of CT findings in 90 patients with COVID-19 pneumonia: a longitudinal study. Radiology. 2020 Mar 19; doi: 10.1148/radiol.2020200843. [Epub] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Sun Q, Xu X, Xie J, Li J, Huang X, et al. Evolution of computed tomography manifestations in five Patients who recovered from coronavirus disease 2019 (COVID-19) pneumonia. Korean J Radiol. 2020;21:614–619. doi: 10.3348/kjr.2020.0157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Bandirali M, Sconfienza LM, Serra R, Brembilla R, Albano D, Pregliasco FE, et al. Chest radiograph findings in asymptomatic and minimally symptomatic quarantined patients in Codogno, Italy during COVID-19 Pandemic. Radiology. 2020;295:E7. doi: 10.1148/radiol.2020201102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Wong HYF, Lam HYS, Fong AH, Leung ST, Chin TW, Lo CSY, et al. Frequency and distribution of chest radiographic findings in COVID-19 positive patients. Radiology. 2019 Mar 27; doi: 10.1148/radiol.2020201160. [Epub] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Yoon SH, Lee KH, Kim JY, Lee YK, Ko H, Kim KH, et al. Chest radiographic and CT findings of the 2019 novel coronavirus disease (COVID-19): analysis of nine patients treated in Korea. Korean J Radiol. 2020;21:494–500. doi: 10.3348/kjr.2020.0132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Li L, Qin L, Xu Z, Yin Y, Wang X, Kong B, et al. Artificial intelligence distinguishes COVID-19 from community acquired pneumonia on chest CT. Radiology. 2020 Mar 19; doi: 10.1148/radiol.2020200905. [Epub] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Yi PH, Kim TK, Lin CT. Generalizability of deep learning tuberculosis classifier to COVID-19 chest radiographs: new tricks for an old algorithm? J Thorac Imaging. 2020;35:W102–W104. doi: 10.1097/RTI.0000000000000532. [DOI] [PubMed] [Google Scholar]
- 82.Hurt B, Kligerman S, Hsiao A. Deep learning localization of pneumonia: 2019 coronavirus (COVID-19) outbreak. J Thorac Imaging. 2020;35:W87–W89. doi: 10.1097/RTI.0000000000000512. [DOI] [PMC free article] [PubMed] [Google Scholar]