Abstract
Trigger finger (TF) disorder is a sudden release or locking of a finger during flexion or extension. Treatments for this disease are conservative and surgical, including NSAIDs, hand splints, corticosteroid injections, physical therapies and percutaneous or open surgery. However, the effectiveness about the optimal treatment of TF is still in lack of evidence. The aim of this study is to investigate the effectiveness of physical therapies as conservative treatment for trigger finger. A comprehensive literature search of the MEDLINE (via PubMed), Cochrane Library Databases and PEDro databases has been conducted without limits because few papers were published about this argument. The literature search identified four papers in PubMed. Two types of physical therapies were used in the conservative management of trigger finger: external shock wave therapy (ESWT) in three papers, and ultrasound therapy (UST) in one paper. ESWT is an effective and safe therapy for the conservative management of TF. It seems to reduce pain and trigger severity and to improve functional level and quality of life. UST has proven to be useful to prevent the recurrence of TF symptoms. Even if the results suggest the effectiveness of ESWT and UST for TF, future studies are necessary to understand the characteristics of the optimal treatment protocol for trigger finger.
Key words: trigger finger, physical therapy, conservative treatment
Introduction
Trigger finger (TF), also known as stenosing tenovaginitis or tenosynovitis, is an hand disorder due to hypertrophy at the intersection of the tendon with its pulley; the subsequent constriction of the tendon prevents it from gliding through ligament’s pulley, causing a sudden release or locking of a finger during flexion or extension, pain and functional limitation.1
Pinching of the tendon can lead to nodule formation and patients typically present with a locking, popping sensation as the nodule catches at the constriction.2
In some cases, it resolves spontaneously; however, if left untreated, trigger digit may gradually progress until the affected finger is permanently locked in flexion.
Histologically, the A1 pulley exhibits fibrocartilaginous metaplasia, and in the tendon tissue, areas of hyalinosis, mucoid degeneration, and chondral metaplasia are found.
TF is usually classified as an idiopathic condition, but some other etiologic hypotesis was proposed. It has been postulated that this disorder is caused by high pressure at the proximal edge of the A1 pulley and the discrepancy between the diameter of the flexor tendon and its sheath at the metacarpal head.3 Some authors argue that there is a possible correlation with hand overuse and repetitive blunt trauma. Other potential risk factors include rheumatoid arthritis, diabetes mellitus, carpal tunnel syndrome, Dupuytren’s disease, amyloidosis, hypothyroidism, mucopolysaccharide storage disorders, congestive heart failure, and genetic predisposition.4 However, the main etiology is still unclear.
TF is the most common flexor tendinopathy, with highest incidence is between 52 and 62 years and in women (75%).5 Thumb and fourth digit (ring finger) are the most commonly affected fingers, the right hand is more frequently involved compared to the left hand 6 and the dominant hand is more frequently involved compared to the non dominant hand.
Diagnosis of TF is based on history of pain, morning stiffness, and tenderness on the A1 pulley, and on clinical examination. Treatment aims to eliminate pain and stop triggering.
TF’s therapy can be divided into conservative and surgical treatment. The currently accepted conservative treatments included medications, usually oral NSAIDS and local corticosteroid injection (CI), with rehabilitative interventions, including extension splint, physiotherapy programs, with mobilization and stretching exercises and physical therapy.6 Surgical treatment involves percutaneous and open release of the A1 pulley, and it’s recommended only when TF has been unresponsive to conservative therapies. CI and surgery are reported to be effective for the remission of symptoms. CI have the greatest success rate among conservative treatments,7 but they are effective only for some patients, and could predispose to tendon rupture when repeated over time. Surgery is associated with longer recovery times and more complications including tendon bowstringing, digital ulnar drift, and nerve injuries. 6
Recently, extracorporeal shock wave therapy (ESWT) is getting popular as an alternative to surgery for the treatment of musculoskeletal disorders in patients unresponsive to conservative approach. ESWT has been reported to be effective in several tendinopathies, such as calcific tendinopathies of the shoulder.8 lateral epicondylitis of the elbow,9 patellar tendinopathy,10 hamstrings tendinopathy 11 and plantar fasciitis.12
A variety of treatments have been described in literature for TF, but the most effective treatment is still under debate.
Acknowledging the possible complications associated with surgery, the fact that guidelines recommend surgery only when conservative treatments have failed, the aim of this review was to investigate the effectiveness of physical therapies as conservative treatment for trigger finger.
Materials and Methods
A comprehensive literature search of the MEDLINE (via PubMed), Cochrane Library Databases and PEDro databases was conducted using the following search terms: “trigger finger” OR “physical therapy” OR “external shock wave therapy” OR “ therapeutic ultrasound” OR “ conservative treatment “. The review included English articles published up to March 2020. Articles were selected by two reviewers (SC, PEF).
They decided to include all papers, due to the small amount of scientific evidence in literature and they excluded all those articles not connected with human medicine, and subsequently with rehabilitation, keeping only articles about health conditions relevant to rehabilitation.
They selected independently the articles eligible for inclusion in the review in order to reduce the risk of inter-observer bias.
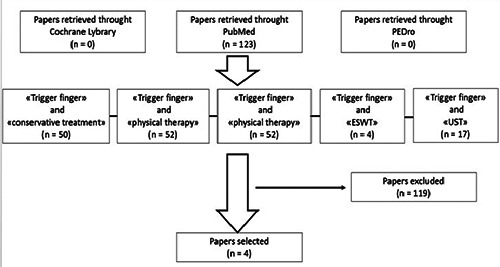
Any study not approved by both of the reviewers was discarded (Figure 1). Afterwards, the same reviewers extrapolated from the articles the characteristics of the sample, the devices, the trial procedures and the outcome indexes (Table 1).
Results
The literature search identified 123 papers published in PubMed as described in algoritm (Figure 1). We excluded n° 119 papers because only four papers studied physical therapies in TF. Any papers were selected in PEDro and Cochrane Library Databases. Of the four total papers one is an interventional study,13 one is a retrospective cohort study,14 and two are prospective RCTs.7,15
Two types of physical therapies were found to be used in the conservative management of trigger finger: external shock wave therapy (ESWT) in three papers,13-15 and ultrasound therapy (UST) in one papers.7
Extracorporeal shock wave therapy and trigger finger
The recent interventional study of Vahdatpour et al.13 recruited 19 subjects with trigger finger disorder. Each patient was treated with ESWT in three sessions with a 1-week interval. The treatment protocol for each session consisted in two parts: radial extracorporeal shock wave therapy (rESWT) with 1000 shocks, at an energy flux density of 2.1 bar and a frequency of 15 Hz, followed by focused shock wave therapy (fESWT) with 500 shocks, at an energy flux density of 0.1 bar and a frequency of 4 Hz. Focused shock waves were used directly on the nodule and the maximum tenderness site, while radial shock wave therapy was used on the peripheral tissues of the nodule. Evaluation of pain severity, severity of triggering, and functional impact of triggering was carried out using the Visual Analogue Scale (VAS), Trigger Finger Score suggested by Quinnell, Quick-Disabilities of the Arm, Shoulder, and Hand questionnaire (Quick-DASH), respectively, before intervention, immediately after intervention, and in 6 and 18 weeks after intervention. There were statistically significant differences with regard to reduction of the pain severity, severity of triggering, and functional impact of triggering before intervention, immediately after intervention, and in 6 and 18 weeks after intervention.
Figure 1.
Study selection process.
Table 1.
Characteristics of the selected articles.
| References | N. Subjects | N. Controls | Physical therapy | Parameters | Outcomes | Timing | Main results | |||
|---|---|---|---|---|---|---|---|---|---|---|
| Shocks (n) | Frequency (Hz) | Flux density (bar) | N. sessions/weeks | T0: baseline T1: 3 weeks | Significant reduction of VAS and QD at T1, T2 and T3 | |||||
| Vahdatpour et al., 2020 | 19 | - | rESWT | 1000 | 15 | 2,1 | 3 /1 week interval | VAS QD | T2: 6 weeks T3: 18 weeks | |
| fESWT | 500 | 4 | 0.1 | |||||||
| Malliaropoulos et al., 2016 | 44s/49 | - | rESWT | 2000 | 5-6 | 1-3 | 3-8 | VAS RM | T0: baseline T1: 4 weeks T2: 12 weeks T3: 1 year | Significant reduction of VAS and better RM at T1, T2 and T3 |
| Yldirim et al., 2016 | 20 | 20 | ESWT vs CI | 1000 | 15 | 2,1 | 3 /1week interval | VAS trigger finger assessment scale QD | T0: baseline T1: 4 weeks T2: 12 weeks T3: 24 weeks | Significant reduction of VAS, QD and TFAS at T1, T2 and T3 in both groups |
| Salim et al., 2012 | 35 | 39 | PT + UST vs CI | - | - | - | - | VAS, n.TFAS hand grip, satisfaction, complication and recurrence. | T0: baseline T1: 12 weeks T2: 24 weeks | Significant reduction of all outcomes in CI at T1. PT + UST no recurrence of symptoms until T2 |
QD: Quick DASH; RM: Roles and Maudsley score; TFAS: trigger finger assessment scale.
Malliaropoulos et al.14 published a retrospective cohort study of 44 patients (49 fingers) treated with an individually adapted protocol of rESWT. According to the authors’ knowledge, this is the first study conducted to assess the effectiveness of rESWT for trigger digit. At each session, 2,000 impulses were applied to the painful area overlying the pathological flexor tendon at a frequency of 5-6 Hz. The device pressure varied from 1 to 3 bars depending on the patient’s individual pain tolerance. The number of weekly rESWT sessions ranged from 3 to 8 with an average of 6±1.3, until symptoms subsided. Primary outcome measures were functional improvement and pain reduction at 1, 3, and 12 months posttreatment compared with baseline. The Roles and Maudsley score was used to assess functional and pain severity was measured using VAS. Recurrence of symptoms was defined as a 1-year follow-up VAS score of ≥2. The individualized protocols were also retrospectively analyzed in terms of the number of sessions required and the pressure used (bars). Therefore, the functional improvement and mean pain reduction over a 1-year follow up period were assessed. In addition, the individualised treatment protocol was retrospectively analysed to look for correlations between pre-treatment symptom duration, the number of rESWT sessions required until recovery, and the 1- year post-treatment visual analog scale score.
To do this, additional outcome measures were used to assess correlations, first, between pretreatment symptom duration and the number of rESWT sessions required until recovery and, second, between pretreatment symptom duration and the 1-year posttreatment VAS score. A statistically significant reduction in VAS scores and functional improvement were found between baseline and 1, 3 and 12 months posttreatment. Notably, in the present study, pain reductions continuously increased over the entire 1-year follow-up period. At 1 month post-treatment, the mean VAS score had reduced by 67% from baseline and at 12 months, it had reduced by 91%, providing excellent long-term efficacy of rESWT.
Only one RCT was found about this argument; Yldirim et al.15 compared the efficiencies of ESWT therapy and corticosteroid injection in the conservative management of trigger finger. In this prospective randomized clinical trial, 40 patients with TF were randomly assigned to ESWT or injection groups. Regarding shock wave, each patient received 1000 shocks at an energy flux density of 2.1 bar (frequency 15 Hz) for three sessions (1-week interval between the sessions). All the clinical outcomes were assessed before treatment and after 1, 3, and 6 months. Pain was measured using VAS. Because of the lack of universally accepted instruments to measure frequency of triggering (FT), the authors used a 0 to 10 point to evaluate this parameter according to an earlier study.16 This scale was also used to score the severity of triggering and the functional impact of triggering. Functional status was assessed using QuickDASH. The definition of cure rate was based on the Quinnell classification.
There were statistically significant differences between baseline and at 1, 3, and 6 months after treatment in terms of all clinical (pain, severity and frequency of triggering) and functional assessments intergroups, but not between groups.
Ultrasound therapy and trigger finger
One paper about the use of ultrasound therapy for TF was found. This RCT 7 compared for the first time the effectiveness of physiotherapy (PT: 35 patients) and corticosteroid injection (CI: 39 patients) treatment in the management of mild trigger fingers.
Mild trigger finger is characterized by mild crepitus, uneven finger movements and actively correctable triggering. PT was a multimodal rehabilitative strategy with ten sessions of wax therapy, ultrasound, stretching muscle exercises and massage. Outcome measurements were based on pain relief (VAS), number of triggering events, hand function, hand grip, patients satisfaction (measured as a decrease in severity of pain and triggering), complication and recurrence. Number of triggering events was assessed by recording the number of triggering events that occurred in 10 active composite flexion/extension movements and the hand grip was assessed based on a dynamometer (JAMAR grip). Hand function was assessed by restriction or pain during buttoning/unbuttoning shirt, pain during opening jars/cans, ability to fully grip the hand and pain during washing clothes/ dishes. Success rate was measured by absence of pain and triggering after completion of treatment at 3 months. Recurrence was assessed by telephone interview at 6 months recording symptoms of pain and triggering. CI treatment had higher rate of improvement in terms of pain score, mean amount of triggering, hand grip and patients’s satisfaction compared to physiotherapy at 3 months post treatment. However, the recurrence rate was significant for pain in the CI group but not in the PT group. Interestingly, there was no recurrence of pain or triggering at all in patients who were successfully treated with physiotherapy even 6 months post-treatment.
Discussion
Trigger finger, also known as stenosing tenovaginitis, is common tenosynovitis characterized by triggering or locking on flexion of the involved metacarpophalangeal joint. A variety of conservative and surgical treatments have been described, but none the most effective treatment for trigger finger is still under debate. Recently, ESWT is getting popular as an alternative to surgery for the treatment of tendinopathies8-12 in patients unrensponsive to traditional conservative treatment.
The biological mechanisms by which ESWT induces therapeutic effects on pathological tendon tissue are not completely elucidated, although the following ipothesis about how shockwaves may facilitate the healing process have been suggested: 8,11
promoting catabolic processes with the disruption and removal of damaged matrix tissues;
stimulating growth factors release and stem cell recruitment
producing neoangiogenesis through an increase in the angiotensin factor, that gives the bloody supply to the injured tendon necessary to its repair
stimulating the synthesis of nitric oxide which will suppress the progression of inflammation.
The clinical studies of Vahdatpour et al.,13 Malliaropoulos et al.14 and Yildrim at al.15 showed the effectiveness of shock wave therapy in reducing pain and triggering severity and in improving finger’s functioning.
Although multiple high-quality studies have demonstrated that ESWT is safe and effective in the treatment of various tendinopathies,8-12 the parameters of the optimal treatment protocol for TF, haven’t been yet established. They include shock wave type (focal or radial), number of shocks, energy flux density, frequency, pressure, number of sessions.
About shock waves generation, Malliaropoulos et al.14 choose to use radial shockwaves because they allow the treatment of a larger tissue volume compared to the focal one; in fact the pathological hypertrophyc area in TF is wider than those involved in insertional tendinopathies, for which focal ESWT is usually used. rESWT is also less painful than focused ESWT. This makes local anesthetic unnecessary and potentially improves treatment outcome as concomitant local anesthesia showed to reduce ESWT efficacy.
About the total number of shocks of each session, it ranges from 500 to 2000 shocks. Two studies13,14 performed 1000 shocks instead, and one14 used a number of 2000 shocks. Only in Vahdatpour et al study 13 has been specified the number of impulses related to the type of device: 1000 shocks for rESWT and 500 shocks for fEWST.
The flux density ranged from 0,1 bar to 3 bar, with two studies using 2,1 bar, considering previous studies using EWST in tendinopathies. For the fESWT a flux density of 0,1 bar was setted. About frequency, the most used value was of 15 Hz (13,15); also frequency of 5-6 Hz 14 and 4 Hz for fESWT were found.
Vahdatpour et al. 13 performed sessions composed by one phase of radial ESWT followed by a second phase of focal ESWT. In Yildrim study 15 shock wave’s type wasn’t indicated.
It has been demonstrated that pressure and number of sessions are inversely proportional: the higher the pressure, the greater the treatment effects; thus, less sessions are required, the lower the pressure, the more sessions are required to have a therapeutic effect. But ESWT at high pressure is very painful, so the right compromise between patient tolerability and therapeutic results must be found. Compared to other tendinopathies treated with rESWT, the finger is a rather painful area to treat. This might explain why comparatively low pressures have to be used.
Currently, there are no standardized guidelines for the number of ESWT sessions required, although studies have suggested that multiple applications provide superior long-term results compared to a single application. Clinical trials analyzed in this review showed a total number of 3 sessions 13,15 and a range of 3-8 sessions, suggesting individualized treatment protocols according to each patient’s tolerance and response to treatment. 14 Data from Yildrim et.al 15 RCT showed that 3 sessions of ESWT treatment could be as effective as a corticosteroid injection for improving symptom severity and functional status in patients with a classification of grade 2 according to the Quinnell classification.
Also duration of pretreatment symptoms could influence session’s number: shorterterm cases required fewer sessions then patients with a longer history of symptoms.14
Results showed that ESWT is an effective and safe therapy for the conservative management of TF. It seemed to reduce pain and trigger severity and improves functional level. No side effects were reported. Notably, excellent long-term efficacy of rESWT was found: pain reductions continuously increased over entire 1-year follow-up period, and at 1- month post-treatment, the mean VAS score had reduced by 67% from baseline and at 12 months, it had reduced by 91%.14
In In the RCT of Yildrim at al.15 about ESWT versus CI, both treatments was found to relieve symptoms, but CI was more effective than ESWT. However, ESWT is recommend for patients who reject corticosteroid injections because of their potential complications, or allergic patients to local anaesthetics, as well as in patients with an intense and persistent fear of injections. Even though no deleterious effect of corticosteroid injection was seen in the study analyzed,15 there have been previous studies reporting dermal or subcutaneous atrophy, transient hyperglycaemia, hypopigmentation of the skin, infection, and rupture of the flexor digitorum profundus tendon in rare cases of CI.17
Only one paper was found about the effectiveness of UST for TF,7 that for the first time compared the success rate of physiotherapy, including therapeutic ultrasound, or corticosteroid injection in managing trigger finger.
In patients with TF the tendon becomes extensile, undergoes plastic deformation and passes more easily through the stenotic A1 pulley.
Therapeutic heat includes superficial (depths of 2-3cm) and deep (up to 5cm) modalities. Superficial modalities include hot packs, hot wax and paraffin baths whilst deep modalities include ultrasound and diathermy. Heat increases blood flow and extensibility of collagen tissue assisting in resolution of edema. Additionally, heat also decreases joint stiffness and pain. A combination of heat and stretching is even more effective as it capitalizes on the extensibility of collagen producing plastic deformation, e.g. bandage wraps of a joint in flexion prior to application of hot packs.18 Additionally, joint mobilization helps increase joint and soft tissue mobility via a slow, passive therapeutic traction and translational gliding. Finally, massaging can ‘soften’ or remodel tendons reducing tissue bulk at the pulleys.
The study7 concursed with studies about other tendinopathies with a high success rate, measured as the absence of pain and triggering, of corticosteroid compared to physiotherapy at 3 months after treatment. The corticosteroid group also shows a significant increase in grip strength compared to physiotherapy.
Therapeutic ultrasound was less effective in reducing pain and in improving function immediately post treatment compared to corticosteroid injection, but interestingly have proven to be useful to prevent the recurrence of symptoms (pain or triggering) after 3 and 6 months posttreatment. In fact there was no recurrence of pain or triggering in the UST group.
Both treatments are safe as there were no complications seen. So ultrasound therapy could be used for patients who dislike or are uncomfortable with needles and injections.
Limitations of the study
Some potential limitations of our study should be mentioned. The literature search was done screening the papers listed in only three databases and only English articles were included. Moreover, studies are few and heterogeneous, with poor sample size and with different outcome mesaures. So even if the results suggest the effectiveness of ESWT and UST for TF, future studies are necessary to understand the characteristics of the optimal treatment protocol for trigger finger.
Conclusions
This narrative review provides a synthesis of the scientific literature available about physical therapies for trigger finger. Results showed that ESWT is an effective and safe therapy for the conservative management of TF. It seems to reduce pain and trigger severity and to improve functional level and quality of life. UST has proven to be useful to prevent the recurrence of TF symptoms. However further studies are necessary to clarify the efficacy of physical therapies in the conservative treatment of TF. In addiction the best treatment energy set-up and protocol for TF are still left to be found.
Funding Statement
Funding: None
References
- 1.Huisstede BM, Hoogvliet P, Coert JH, Fridén J. Multidisciplinary consensus guideline for managing trigger finger: results from the european HANDGUIDE study. Phys Ther 2014;94:1421-33. [DOI] [PubMed] [Google Scholar]
- 2.Farnebo S, Chang J. Practical management of tendon disorders in the hand. Plast Reconstr Surg 2013;132:841e-53e [DOI] [PubMed] [Google Scholar]
- 3.Frontera WR, Silver JK, Rizzo TD. Essentials of Physical Medicine and Rehabilitation: Musculoskeletal Disorders, Pain, and Rehabilitation. Saunders/Elsevier; 2008. [Google Scholar]
- 4.Blyth MJ, Ross DJ. Diabetes and trigger finger. J Hand Surg Br 1996;21:244-5 [DOI] [PubMed] [Google Scholar]
- 5.Fleisch SB, Spindler KP, Lee DH. Corticosteroid injections in the treatment of trigger finger: a level I and II systematic review. J Am Acad Orthop Surg 2007;15:166-71 [DOI] [PubMed] [Google Scholar]
- 6.Ryzewicz M, Wolf JM. Trigger digits: principles, management, and complications. J Hand Surg Am 2006; 31:135-46. [DOI] [PubMed] [Google Scholar]
- 7.Salim N, Abdullah S, Sapuan J, Haflah NH. Outcome of corticosteroid injection versus physiotherapy in the treatment of mild trigger fingers. J Hand Surg Eur Vol 2012;37:27-34 [DOI] [PubMed] [Google Scholar]
- 8.Avancini-Dobrovic V, Frlan-Vrgoc L, Stamenkovic D. Pavlovic I Radial extracorporeal shock wave therapy in the treatment of shoulder calcific tendinitis. Coll Antropol. 2011. [PubMed] [Google Scholar]
- 9.Pettrone FA, McCall BR. Extracorporeal shock wave therapy without local anesthesia for chronic lateral epicondylitis. J Bone Joint Surg Am 2005;87:1297-304. [DOI] [PubMed] [Google Scholar]
- 10.van Leeuwen MT, Zwerver J, van den Akker-Scheek I. Extracorporeal shockwave therapy for patellar tendinopathy: a review of the literature. Br J Sports Med 2009;43:163-8 [DOI] [PubMed] [Google Scholar]
- 11.Cacchio A, Rompe JD, Furia JP, Susi P, et al. Shockwave therapy for the treatment of chronic proximal hamstring tendinopathy in professional athletes. Am J Sports Med 2011;39:146-53 [DOI] [PubMed] [Google Scholar]
- 12.Lohrer H, Nauck T, Dorn-Lange NV, Scholl J, et al. Comparison of radial versus focused extracorporeal shock waves in plantar fasciitis using functional measures. Foot Ankle Int 2010;31:1-9 [DOI] [PubMed] [Google Scholar]
- 13.Vahdatpour B, Momeni F, Tahmasebi A, Taheri P. The Effect of Extracorporeal Shock Wave Therapy in the Treatment of Patients with Trigger Finger. J Sports Med 2020;11:85-91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Malliaropoulos N, Jury R, Pyne D, et al. Radial extracorporeal shockwave therapy for the treatment of finger tenosynovitis (trigger digit). Open Access J Sports Med 2016;7:143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yildirim P, Gultekin A, Yildirim A, Karahan A, et al. Extracorporeal shock wave therapy versus corticosteroid injection in the treatment of trigger finger: a randomized controlled study. J Hand Surg Eur Vol 2016;41:977-83. [DOI] [PubMed] [Google Scholar]
- 16.Tarbhai K, Hannah S, von Schroeder HP. Trigger finger treatment: a comparison of 2 splint designs. J Hand Surg Am 2012;37:243-9. [DOI] [PubMed] [Google Scholar]
- 17.Akhtar S, Bradley MJ, Quinton DN, Burke FD. Management and referral for trigger finger/thumb. BMJ 2005;331:30-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Knight CA, Rutledge CR, Cox ME, Acosta M, et al. Effect of superficial heat, deep heat, and active exercise warmup on the extensibility of the plantar flexors. Phys Ther 2001;81: 1206-14. [PubMed] [Google Scholar]


