Abstract
Total knee arthroplasty (TKA) is a highly successful operation that improves patients’ quality of life and functionality. Yet, up to 20% of TKA patients remain unsatisfied with the functional outcomes. Robotic TKA has gained increased attention and popularity in order to improve patient satisfaction and implant survivorship by increasing accuracy and precision of component implantation. The current systematic review was run in order to compare implant survivorship, complication rates, clinical outcomes, and radiological outcomes between robotic-assisted TKA (RA) and conventional manual TKA (CM). Articles were referenced from the US National Library of Medicine (PubMed/MEDLINE), EMBASE, and the Cochrane Database of Systematic Reviews. Nine comparative studies with 1199 operated knees in 1159 patients were included, 614 underwent active or semiactive robotic-assisted TKA compared to 585 CM-TKA. Improvements in the RA group were reported for early functional outcomes, radiographic outliers (RA 16% vs CM 76%) and radiolucent lines (RA 0% vs CM 35%). No significant differences between the two groups were reported in overall survivorship (RA 98.3% vs CM 97.3%), complication rate (RA 2.4% vs CM 1.4%) and operative time (RA 88 min vs CM 79 min). Despite higher costs, roboticassisted TKA offers better short-term clinical outcomes when compared to conventional manual technique with reduction in radiographic outliers and reduced risks of iatrogenic soft tissues injuries (reduced blood loss and postoperative drainage). Further high-quality long-term studies of modern robotic systems are required in order to evaluate how the increased accuracy and reduced outliers affect the long-term survivorship of the implants and the clinical outcomes.
Key words: Robotic surgery, Total knee arthroplasty, Robotic knee surgery, Clinical outcomes, Survivorship
Introduction
Total Knee Arthroplasty (TKA) has been widely recognized as the gold standard treatment for end-stage knee osteoarthritis.1,2 This procedure is performed in more than 600.000 patients per year in the United States (US) and the number is projected to grow by 673% in 2030.3 Despite the great improvements in implant design, materials and patient-specific rehabilitation programs, up to 20% of patients are dissatisfied following TKA.2,4 Limb alignment and accuracy of implant positioning are widely considered among the most important prognostic factors for long-term implant survivorship, patient satisfaction and clinical outcomes.1,4-10
Robotic technology in TKA has been developed in order to increase accuracy in implant positioning and to reduce outliers in limb alignment compared to conventional manual technique.11-13 However, trust on robotic-TKA is limited by increased costs and longer operative time, associated with a lack of long-term evidence comparing clinical and functional outcomes to conventional manual TKA.13 The restoration of mechanical axis (0° within ± 3° of standard deviation [SD]) through tibial and femoral perpendicular cuts with respect to their mechanical axis is strongly associated with higher implant survivorship and clinical outcomes.11,12,14,15
The first robotic systems introduced in TKA were active robots based on CT images: ROBODOC® (Think Surgical, Fremont, CA, USA, originally by Integrated Surgical Systems) in 1992, and CASPAR System® (U.R.S.-ortho GmbH & Co. KG, Rastatt, DE). The surgeon was responsible of performing the surgical approach and exposition of the distal femur and proximal tibia, secure the limb into a fixed device and let the robot perform the planned bone resections. However, the CASPAR system was somewhat restrictive: femoral and tibial bone screws had to be placed preoperatively (during an initial first surgery) as fiducial markers for registration of the CT-scan in order to allow for intraoperative robotic functions. Autonomous robots had fallen out of favor due to concern over nerve and soft tissue injury and have been progressively replaced by semiautonomous systems.16,17
Classification of robotic systems
There are three types of robotic system: autonomous (active), hands-on (semi-active) and passive, based on the degree of surgeon control over the robot. The passive systems do not perform independently the operation, they are known as computer-assisted or navigation systems based on patient- and instrument- centered reference points to provide the surgeon with perioperative recommendations and guide positioning of the surgical tool.18 Active robots hold the cutting tool and autonomously make the tibial and femoral resections. Semi-active robots combine both principles, the surgeon maintains the overall control over the bone resections under the surveillance of the robot that provides a live intraoperative feedback to limit deviation from the preoperative surgical plan.12,13A three-dimensional model of the knee is obtained either intraoperatively or from dedicated preoperative images through an integrated surgical planning system that allows to make a plan of bone resections and implant positioning (Table 1).12,13
Currently, the semi-active robotic systems are widely used in robotic-assisted TKA. The Mako Robotic Arm Interactive Orthopaedic system (RIO; former MAKO Surgical Corp.®, FL, USA; now Stryker Ltd, Kalamazoo, MI, USA), approved by the Food and Drug Administration (FDA) for TKA in 2015, is an image-guided semiactive robot system that requires a CT scan to generate a 3D model of the patient’s bone structure. The plan can be modified intraoperatively with data collected during the operation and applied to the CT model. The Navio Surgical System (former Blue Belt Technologies; now Smith & Nephew, Andover, TX, USA), approved by the FDA for TKA in 2017, is an imageless CT-free semi-active robot system that intraoperatively capture the osseous anatomy during the planning phase and guides bone resection without haptic boundaries. In early 2019 was introduced the Rosa Knee System (Zimmer-Biomet, Warsaw, IN, USA), a stereotaxic instrumentation system. Threedimensional (3D) model of the knee is obtained from preoperative two-dimensional x-rays or based on MRI planning tools, landmarks are recorded intraoperatively based on the surgical plan. This system enables the surgeon to personalize in real time the surgical plan based on each patient’s individual characteristics. The cutting jigs are positioned and hold by the robot (collaborative robotic system, a.k.a. cobot), while the surgeon performs the bone cuts.19 Conversely, the Navio Surgical System and the Mako Robotic Arm Interactive Orthopaedic system do not require cutting blocks but creates stereotactic boundaries that assist the surgeon in the tibial and femoral resections.
Limitations of robotic-assisted systems
Multiple limitations have been addressed to robotic-assisted TKA: installation and maintenance costs for the robotic devices, additional costs as a consequence of the longer surgical time, the long learning curve of the surgeon and surgical team, eventual additional imaging required for the preoperative plan with increased radiation exposure (when considering image-based systems) and femoral and tibial incisions for insertion of the registration pins.20,21 In addition, it has been reported an increased blood loss and a longer anesthesia due to the longer surgical time with the first generation of robotic systems.20,21 Implant choice in robotic-assisted procedures is often limited by whether or not a robotic system utilizes an “open” or “closed” platform: closed platforms (MAKO system, Rosa Knee System, Navio system) limit the surgeons to specific, proprietary implant types; open platforms (ROBODOC system), however, permit the surgeon to use multiple implants from different companies depending on the surgeon’s preference. Lastly, fully active robotic systems have been associated with and increased soft tissue disruption and technical difficulties when converting to a conventional manual-jig procedure.20
In order to obtain a wider vision on the benefits of robotic-assisted TKA over conventional manual TKA, a systematic review of comparative studies was run to establish survivorship of the implant, complication rates, clinical outcomes, and radiographic outcomes.
Materials and Methods
The systematic search was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta- Analyses guidelines. The US National Library of Medicine (PubMed/MEDLINE), EMBASE, and the Cochrane Database of Systematic Reviews were queried for publications from January 1990 to December 2019 using various combinations of the search terms “total knee arthroplasty,” “robot-assisted total knee arthroplasty,” “robotic total knee”, “robot total knee replacement” in combination with the Boolean operators (AND, OR, *).
Only abstracts that compared the clinical outcomes of patients who underwent robotic TKA with conventional manual TKA were reviewed. Inclusion criteria were any original study in which patients 18 years and older received a primary TKA, postoperative complications were reported, clinical outcomes were reported using validated patient-reported scales, radiographic outcomes were reported and implant survivorship free of implant revision was reported. Eexclusion criteria were case reports, surgical technique reports, review articles, expert opinions, letters to editors, biomechanical reports, instructional course lectures, studies on animal, cadaver or in vitro investigations, book chapters, abstract from scientific meetings, unpublished reports, studies with less than 20 knees per group, studies with a mean follow-up less than 3 months and studies written in nonenglish language.
Two independent reviewers (F.M. and G.C.) separately conducted the described search by title and abstract. Both authors compiled a list of studies not excluded after application of the inclusion and exclusion criteria. If the title and abstract of each study contained insufficient information to determine its appropriateness for inclusion, the full manuscript was reviewed. If the articles met inclusion criteria following a title and abstract screen, the full text was obtained and reviewed. A cross-reference research of the selected articles was also performed to obtain other relevant articles for the study. If there was disagreement between the 2 reviewers, the senior author (I.D.M.) was consulted and consensus was reached. During initial review of the data, the following information were collected for each study: title, first author, year of publication, study design, number of patients, patients dead and lost at follow-up, age of patients, length of follow-up, type of robotic system, type of knee implant, complications, survivorship of the implants, radiographic and patientsreported outcomes.
Table 1.
Robotic Systems and Functional Characteristics.
| System | Corporation | Arthroplasty | Preoperative Planning | Control | Platform | Bone Resection |
|---|---|---|---|---|---|---|
| ROBODOC | THINK Surgical, Freemont, CA, USA | TKA, THA (femur) | CT scan | Autonomous | Open | Mill |
| iBlock | OMNIlife Science, East Taunton, MA, USA | TKA | None | Autonomous | Closed | Saw |
| CASPAR | U.R.S.-ortho GmbH & Co. KG, Rastatt, DE | TKA, THA | CT scan | Autonomous | Open | Mill |
| MAKO | Stryker Ltd, Kalamazoo, MI, USA | UKA, PFA, TKA, THA | CT scan | Semiautonomous, haptic | Closed | Burr, saw |
| Navio PFS | Smith & Nephew, Andover, TX, USA | UKA, PFA, TKA | None | Semiautonomous | Closed | Burr, saw |
| Rosa knee | Zimmer-Biomet, Warsaw, IN, USA | TKA | None | Semiautonomous | Closed | Saw |
TKA, Total Knee Arthroplasty; THA, Total Hip Arthroplasty; UKA, Unicondylar Knee Arthroplasty; PFA, Patellofemoral Arthroplasty.
The level of evidence in the included studies was determined using the Oxford Centre for Evidence-Based Medicine Levels of Evidence. The methodological quality of each study and the different types of detected bias were assessed independently by each reviewer with the use of modified Coleman methodology score.22
Results
Study Selection
The search resulted in 107 abstracts that were examined (Figure 1). Following elimination of duplicate articles, predetermined inclusion and exclusion criteria were applied. In total, 9 articles16,18,23-29 met the inclusion criteria and were included in the analysis (Table 2).
Quality of studies and possible risk of bias
Among the 9 studies, 3 were randomized control trials (RCTs) (out of 9, 33%)23,24,26, 3 (33%)18,25,29 prospective comparative studies and 3 (33%)16,27,28 retrospective comparative studies. Two studies (22%)23,26 were classified as level of evidence (LOE) I, 1 study (11%)24 as LOE II, 1 study (11%)16 as LOE III and 5 studies (55%)18,25,27-29 as LOE IV.
The “quality assessment” of the studies for methodological deficiencies was examined using the modified Coleman methodology score. 22
The total mean modified Coleman score was 58/100 (range, 40/100 to 72/100) assessing for fair overall quality of the studies. Selection, detection and performance biases were found in 6 studies out of 9. 16,18,25,27-29 A meta-analysis was not undertaken due to the general fair quality of the studies (Table 2).
Table 2.
Type of study, level of evidence, mean follow up per study.
| Author | Type of study | Level of evidence | Mean follow up (months) | Modified Coleman score | Type of bias |
|---|---|---|---|---|---|
| Khlopas et al. 2019 | Prospective case control | IV | 3 | 66 | Selection, detection and performance |
| Cho et al. 2019 | Retrospective case control | IV | 130 | 48 | Selection, detection and performance |
| Yang et al. 2017 | Retrospective case control | IV | 126 (100-138) | 45 | Selection, detection and performance |
| Merchand et al. 2017 | Prospective case control | IV | 6 | 60 | Selection, detection and performance |
| Liow et al. 2016 | Randomized control trial | II | 24 | 67 | Detection and performance |
| Song et al. 2013 | Randomized control trial | I | 65 (41-81) | 72 | Detection and performance |
| Song et al. 2011 | Randomized control trial | I | 16 (13-19) | 57 | Detection and performance |
| Park et al. 2007 | Prospective case control | IV | 45 | 63 | Selection, detection and performance |
| Siebert et al. 2002 | Retrospective case control | III | 6 | 40 | Selection, detection and performance |
Figure 1.
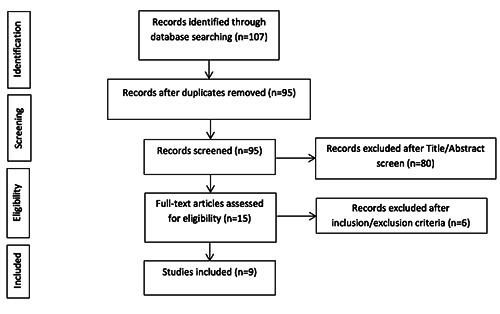
PRISMA flow diagram outlining the systematic review process. PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
General characteristics
Overall, 1199 TKAs in 1159 patients were included in the systematic review; robotic-assisted (RA) TKA was performed in 614 knees (51%, 608 patients) whereas conventional manual (CM) TKA was performed in 585 knees (49%, 551 patients). Women represented 72% of the patients in the RA-TKA group and 70% in the CMTKA group. The mean age of the patients in the RA-TKA group was 66 years (range, 63 to 69 years), while in the CM-TKA group was 68 years (range, 65 to 68 years). The mean follow-up was 46 months (range, 3 months to 11 years) (Table 3).
The ROBODOC® System (Think Surgical, Fremont, CA, USA) was used in 6 studies (67%)18,23,24,26-28, the MAKO Robotic- Arm (MAKO Surgical Corp, Ft. Lauderdale, FL, USA) in 2 studies (22%)25,29 and the CASPAR® System (U.R.S.-ortho GmbH & Co. KG, Rastatt, DE) in 1 study (11%)16.
In the RA-TKA group the NexGen knee system (NexGen®, Zimmer Inc., Warsaw, IS, USA) was implanted in 374 knees (out of 614, 61% in the RA group), the Triathlon Cruciate Retaining system (Stryker, Mahwah, NJ) in 170 cases (28%) and the LC Search Evolution® knee-system (Aesculap, Tuttlingen, Germany) in 70 cases (11%). In the CM-TKA group the NexGen knee system (NexGen®, Zimmer Inc., Warsaw, IS, USA) was implanted in 463 cases (out of 585, 79%) and the Triathlon Cruciate Retaining system (Stryker, Mahwah, NJ) in 122 cases (out of 585, 21%) (Table 3).
The operating time was reported in 4 studies out of 9 (44%)16,23,24,26. Three studies (11%)23,24,26 reported mean surgical time of 88 minutes in the RA group (range, 79-95 minutes) and of 79 minutes in the CM group (range, 70-93 minutes). Among the 4 studies, 3 did not achieved statistical significance (p=not significant). However, Song et al,23 reported that the mean operative time in the RA group was 25 minutes longer when compared with the CM group (p<0.001), while the postoperative blood drainage was higher in the CM group (933 ± 467 mL) when compared with the RA group (613 ± 318 mL, p<0.001). Song et al,26 reported a lower mean blood loss in the RA group (568.6 mL, SD ± 385) when compared with the CM group (816 mL, SD ± 425, p=0.005).
Survivorship and complication rates
Four studies (44%)24,26-28 reported revision rates. The overall revision rate was 1.7% in the RA group and 2.7% in the CM group. Yang et al,27 reported an overall survivorship of 98.5% at 5 years in the RA group and 97.6% in the CM group; 97.1%, and 92.3% respectively at 10 years (p=0.31). Cho et al,28 reported an overall survivorship of 98.8% in the RA group and 98.5% in the CM (p=0.563), with no cases of aseptic loosening in the RA group compared to the two cases in the CM group (1%, p=0.48). Song et al,26 reported a survivorship among both groups of 100% at short-term follow up (1.3 years) from infection and aseptic loosening. Liow et al,24 reported an overall survivorship of 93.5% in the RA group and 100% in the CM group at a mean follow-up of 2 years. One of the 2 revision in the RA group was due to persistent lateral-sided pain secondary to lateral overhang of the tibial component at 20 months, likely related to manual implantation after abortion of robotic procedure (Table 4).
Six studies (66.7%)16,18,23,24,27,28 reported complications that required reoperation with an overall reoperation rate of 2.4% in the RA group (15 out of 614) and 1.4% in the CM group (8 out of 331) at a mean follow-up of 5.5 years (range, 0.5-10.8 years). However, none of the studies reported statistical significance when comparing the two groups (p=0.27, p=0.48). Periprosthetic joint infection was the most frequent complication among both groups (RA 1.7%; CA 1%). Complications directly associated to the robotic systems surgical technique were reported in 2.3% of the cases (14 out of 614). Further complications that did not required reoperation are addressed in Table 4.
Radiographic outcomes
All studies aimed to mechanical alignment. Radiographic outliers were defined with an error greater of ± 3° for mechanical axis (θ), coronal (a) and sagittal (g) femoral inclinations and coronal (b) and sagittal (d) tibial inclinations. Five studies (55%)16,23,26-28 analyzed radiographic outcomes and reported an overall rate of outliers of 16% (64 out of 381) in the RA group and 76% (306 out of 404) in the CM group. Among them, Song et al,23 reported a significant reduction of outliers for mechanical axis in the RA group when compared with the CM group (0% vs 24%; p<0.001). Siebert et al,16 reported a highly significant difference in tibiofemoral alignment between the two groups (RA: 1/70, 1.4% [4° deviation from planned angle] vs CM: 18/52, 35% [deviation >3°- 7°]; p<0.0001). Song et al,26 reported a significant improvement in outliers for tibial sagittal inclination (d) (RA 2/30, 7% vs CM 15/30, 50%; p=0.001), for femoral coronal inclination (a) (RA 0% vs CM 8/30, 27%; p=0.008) and for mechanical axis (θ) (RA 0% vs CM 7/30, 23%; p=0.001). Yang et al,27 reported a significant improvement regarding radiographic outliers for mechanical axis (θ) (RA 6/69, 9% vs CM 13/39, 33%; p<0.001), coronal femoral inclination (a) (RA 4/69, 6% vs CM 12/39, 31%; p<0.001), sagittal femoral inclination (g) (RA 10/69, 14% vs CM 23/39, 60%; p<0.001) and sagittal tibial inclination (d) (RA 6/69, 9% vs CM 17/39, 44%; p<0.001). Finally, Cho et al,28 reported a higher rate of outliers among the CM group (91%, 128 cases) when compared to the RA group (19%, 22 cases; p<0.05).
Table 3.
Number of patients, sex, mean age, type of robot and type of knee implant per study.
| Author | Patients/knees | Sex | Mean age (years) | Type of robot | Type of knee implant |
|---|---|---|---|---|---|
| Khlopas et al. 2019 | RA: 150/150 | RA: 95f/55m | RA: 65 | MAKO | Triathlon CR |
| CM: 102/102 | CM: 59f/43m | CM: 68 | |||
| Cho et al. 2019 | RA: 155/160 | RA: 141f/14m | RA: 68 | ROBODOC | RA: NexGen CR: 157, PS 3 CM: NexGen CR: 167, PS 63 |
| CM: 196/230 | CM: 163f/33m | CM: 68 | |||
| Yang et al. 2017 | RA: 71/71 | RA: 66f/6m | - | ROBODOC | NexGen CR |
| CM: 42/42 | CM: 39f/3m | ||||
| Merchand et al. 2017 | RA: 20/20 | RA: 14f/6m | RA: 69 | MAKO | Triathlon CR |
| CM: 20/20 | CM: 10f/10m | CM: 67 | |||
| Liow et al. 2016 | RA: 31/31 | - | - | ROBODOC | NexGen LPS Flex |
| CM: 29/29 | |||||
| Song et al. 2013 | RA: 50/50 | RA: 46f/4m | RA: 66 | ROBODOC | NexGen |
| CM: 50/50 | CM: 45f/5m | CM: 65 | |||
| Song et al. 2011 | RA: 30/30 | RA: 30f | - | ROBODOC | NexGen |
| CM: 30/30 | CM: 30f | ||||
| Park et al. 2007 | RA: 32/32 | - | RA: 63 | ROBODOC | NexGen LPS |
| CM: 30/30 | CM: 68 | ||||
| Siebert et al. 2002 | RA: 69/70 | RA: 48f/21m | RA: 66 | CASPAR | RA: LC Search Evolution CM: NexGen |
| CM: 52/52 | CM: 40f/12m | CM:68 |
RA, Robot-assisted technique; CM, Conventional-manual technique; -, Not reported.
Radiolucent lines (RRLs) were analyzed in only one study (11%); Yang et al,27 reported no cases of radiolucent lines (RLLs) in the RA group and 6 cases (35%) in the CM group (4 on the femoral side and 2 on the tibial side) at a mean of 10.5 years (range, 8.4-11.5 years); none of the RLLs were progressive and 5 of them (83%) were <2mm (p<0.001).
Clinical outcomes
Clinical outcomes were reported in all 9 studies (100%)16,18,23-29 with significant postoperative improvements compared to the respective mean preoperative values. Six studies (66%)18,23,24,26-28 reported a mean postoperative range of movement (ROM) in the RA group of 126° (range 118°-133°) and of 128° (range 122°-131°) in the CM group. The Hospital for Special Surgery (HSS) score was used in 4 studies (44%)23,26-28 reporting a mean postoperative value of 92 points in the RA group (range, 88.5-96.7 points) and 91 points in the CM group (range, 86.7-94.7 points). The Western Ontario and McMaster Universities (WOMAC) score was used in 5 studies,23,26-29 reporting a mean value of 13 points in the RA group (range, 7-29 points) and 16 points in the CM group (range, 11-30 points) (p<0.05). Liow et al,24 reported a better SF- 36 general health (p=0.04) at 6 months and a better SF-36 vitality (p=0.03) and role emotional (p=0.02) at 2 years postoperatively in the RA group when compared with the CA group. The postoperative Knee Society Score (KSS) was used in 3 studies,18,24,25 reporting a mean value of 80 points in the RA group (range, 66-92 points) and 82 points (range, 67-91 points) in the CA group (p<0.001) (Table 5).
Discussion
Robotic-assisted technique has been associated with increased accuracy and precision in coronal and sagittal alignment, better early functional outcomes and reduced limb malalignment compared with conventional manual-jig technique.11-13,15
Based on the current evidence there is no difference in short-to-mid term survivorship, aseptic loosening, periprosthetic joint infection and complication rates between RA-TKA and CM-TKA. In addition, there is no significant difference regarding the operating time between the two techniques suggesting that longer time is not associated with increased complication. The incidence of pin-related fracture as technique-related complication is very low and overall not reported in the literature, however, technique-related complications were reported in 2.3% of the cases in the RA group.
Table 4.
Complications in Robotic-Assisted and Conventional Manual-jig Technique.
| Author | RA Complications | CM Complications |
|---|---|---|
| Khlopas et al. 2019 | - | - |
| Cho et al. 2019 | 2 Deep infections (two-stage revision) | 1 Deep infection (two stage revision) 2 Aseptic Loosening (implant revision) 2 Polyethylene wear (implant revision) 1 Knee instability (implant revision) (p=0.48) |
| Yang et al. 2017 | 2 Deep infection (two-stage revision) No cases of radiolucent lines | 2 Deep infection (two-stage revision) 1 Knee instability (implant revision) (p=0.27) 6 Radiolucent lines, non-progressive (p<0.001) |
| Merchand et al. 2017 | - | - |
| Liow et al. 2016 | 1 Superficial wound infection 1 Early infection (washout and liner exchange) 1 Lateral pain in tibial component due to malposition after aborted procedure (revision tibial component) 1 Deep vein thrombosis 3 Abortion of robot procedure (2 technical error and 1 robot error) | 1 Deep vein thrombosis |
| Song et al. 2013 | 2 Superficial wound infections 1 Seroma at pin site 2 patellar tendon abrasion 1 Skin rash (conservative treatment) | 2 Superficial wound infections 1 Incisional skin sloughing |
| Song et al. 2011 | - | - |
| Park et al. 2007 | 1 Superficial wound infection 1 Patellar tendon rupture 1 Patellar dislocation 1 Peroneal injury | - |
| Siebert et al. 2002 | 3 Skin irritation at pin site (conservative treatment) 1 Complication due to defective registration marker, full correction achieved by converting to a manual technique | - |
RA, Robotic-assisted technique; CM, Conventional manual-jig technique.
Regarding clinical outcomes, patients’ satisfaction was increased in RA-TKA group with better early clinical outcomes compared to CM-TKA and no significant differences of ROM were reported between the two groups, in line with what is reported in the current literature.12,13 Previous studies suggested that postoperative ROM and implant stability are influenced from the posterior inclination of the tibial component.12,30 In addition, insufficient knee ROM is usually caused by inappropriate component sizing, a tight extension or flexion gap, component malalignment or malrotation, a lack of rehabilitation and swelling of the periarticular soft tissue.31 Siebert et al,16 reported reduced soft tissue swelling and earlier regain of full ROM in the RA group when compared to the CM group. However, there was no significant difference regarding ROM between the two groups and soft tissue swelling was not properly quantified. Nevertheless, WOMAC and KSS scoring systems showed significantly higher scores in the RA-TKA group (p<0.05). Improved preservation of the periarticular soft tissue in robotic TKA may reduce local postoperative inflammatory response, pain and postoperative soft tissue swelling. According to our results, in the RA group was reported a reduced mean intraoperative blood loss (RA 568 mL, SD ± 385 vs CM 816mL, SD ± 425; p=0.005) and reduced postoperative drainage (RA 613 ± 318 mL vs CM 933 ± 467 mL; p<0.001).23,26 These findings, in line with the current literature,13 support that increased soft tissue protection is associated with reduced postoperative pain and periarticular swelling, leading to better early clinical outcomes. However, only two studies included in this systematic review compared blood loss and postoperative drainage between the two groups, more evidences are needed to evaluate the association between intraoperative soft tissue protection and early clinical outcomes.
Regarding the radiological findings, lower incidence of outliers was assessed for mechanical axis (θ), coronal (a) and sagittal (g) femoral inclinations and coronal (b) and sagittal (d) tibial inclinations confirming the higher accuracy and precision of the technique. The high degree of accuracy was demonstrated in the cadaveric study by Parratte et al,19 using the Rosa Knee System (Zimmer-Biomet, Warsaw, Indiana, USA). The author reported no significant difference compared to the preoperative plan in resection angles (except for the femoral flexion angle, mean difference of -0.95°); no differences regarding the thickness of the resection (except for the distal medial femoral and medial proximal tibial cuts) and the hip-knee-ankle angle mean difference was -0.03°±0.87°. However, further in vivo studies are necessary to evaluate if the accuracy obtained in a cadaveric study is reproducible in larger cohorts. Given the similar mid-term survivorship between RATKA and CM-TKA, the significative higher accuracy and precision in alignment correction and the lower incidence of outliers in both coronal and sagittal planes might represent a strong determinant for implants long-term survivorship, where there are still no studies available.
Surgical time continues to be an issue in robotic-assisted technique; it can lead to a higher risk of infection, blood loss and other postoperative complications,32 127 min has been indicated as a critical point leading to an increased risk of infection.33According to Hampp et al,34 following a single cadaver training for a surgeon with no previous robotic experience, it was sufficient a number of 12 RA-TKAs to obtain greater accuracy and precision compared with the conventional manual technique. Siebert et al,16 reported a longer surgical time for the first 70 robotic cases (mean 135 minutes, range 80-220 minutes) followed by an almost normal surgical time (approximately 90 minutes). Song et al,26 reported a mean operative time 25 minutes longer in the robotic-assisted TKA but no increased complication rates in short-term follow-up. Sodhi et al35 analyzed the learning curve of two high-volume surgeons with no previous experience in robotic-assisted TKA in 40 cases and reported a significant decrease in operative time from the first 20 cases to the last 20 cases. In addition, there was no significant difference between the last 20 robotic-assisted cases compared to the conventional manual technique (99 vs 84 vs 81 minutes; p<0.05). Kayani et al,36 reported that robotic-assisted TKA was associated with a learning curve of 7 cases for operative time and surgical team comfort levels but there was no learning curve for accuracy of implant positioning, limb alignment, posterior condylar offset ratio, posterior tibial slope and joint line preservation.
Increased costs are a consistent problem in robotic surgery. According to the current literature, these costs may be partially offset since RA patients had statistically significantly lower 90-day Episode-of-Care costs (p<0.0001), lower facility costs, shorter length-of-stay, and higher chance of being dismissed at home.37 One potential costrelated concern is the preoperative imaging such as CT-scans; however, this enhanced imaging modality did not contribute to net higher overall healthcare costs.37 Kayani et al,36 reported that reduced bone and periarticular soft tissue injury is a factor in lowering the overall cost by reducing the post-acute care. The soft tissue protection in RA technique has been previously described in a cadaveric study by Khlopas et al,38 assessing that in robotic-assisted technique tibial subluxation and patellar eversion are not required in order to achieve an optimal visualization, reducing ligament and capsular stretching, length of stay, and complication rate. Kayani et al,39 in order standardize the soft tissue involvement, proposed a Macroscopic Soft Tissue Injury classification (MASTI) based on intraoperative assessment of the soft tissue envelope. The knee was divided in four zones (medial tibial, lateral tibial, anterior and posterior), evaluated for soft tissue iatrogenic injury and graded from stage 1 to 6: uninvolved soft tissue, planned soft tissue release, soft tissue contusion, soft tissue fibrillation or incomplete damage, soft tissue cleavage and complete unintentional soft tissue detachment. The sawblade, active only within the confines of the stereotactic boundaries, may have helped to better protect the periarticular soft tissue envelope compared to the manually controlled sawblade.
Table 5.
Operating Time, ROM, HSS, WOMAC, KSS and KS Function Score.
| Author | Clinical Outcome Scale | Significant Difference between RA-TKA and CM-TKA |
|---|---|---|
| Khlopas et al. 2019 | KSS1 | NO |
| 1RA 65.5-CM 67.2 | ||
| Cho et al. 2019 | ROM1, HSS2, WOMAC3, KSf4 | NO |
| 1RA 130.7°-CA 130°; 2RA 88.5-CM 86.7; 3RA 10.1-CM 13; 4RA 87.8-CM 87.4 | ||
| Yang et al. 2017 | ROM1, HSS2, WOMAC3 | NO |
| 1RA 132.6°-CM 131; 2RA 89-CM 88; 3RA 7.6-CM 11.5 | ||
| Merchand et al. 2017 | WOMAC | YES |
| RA 7-CM 14 (p<0.05) | ||
| Liow et al. 2016 | ROM1, KSS2, KSSf3 | NO |
| 1RA 118°-CM 125°; 2RA 82-CM 88; 3RA 77-CM 74 | ||
| Song et al. 2013 | ROM1, HSS2, WOMAC3 | NO |
| 1RA 128°-CM 129°; 2RA 96.7-CM 94.7; 3RA 28.9-CM 30 | ||
| Song et al. 2011 | ROM1, HSS2, KSS3 | NO |
| 1RA 129°-CM 129°; 2RA 95.2-CM 94.7; 3RA 11-CM 13 | ||
| Park et al. 2007 | ROM1, KSS2, KSSf3 | NO |
| 1RA 118°-CM 122°; 2RA 92-CM 91; 3RA 88 CM 88 |
ROM, Range of Movement; HSS, Hospital for Special Surgery Score; WOMAC, Western Ontario and McMaster Universities; KSS, Knee Society Score; RA, robotic-assisted technique; CM, conventional-manual technique.
Promising results of the robotic-assisted technique have been reported in the unicompartmental total knee arthroplasty using the Robotic Arm Interactive Orthopedic (RIO) System (MAKO Surgical Corp., Ft. Lauderdale, FL, USA) with 2-to- 3 years survivorship of 98.8%.40 Significant improved outcomes have been described by Zhang et al.41 In addition, Batailler et al,42 compared the BlueBelt Navio surgical system (Smith and Nephew®) with the conventional manual technique reporting a better overall alignment and no cases of complications directly related to the robotic technique.
Multiple limitations have been encountered. The majority of the studies involved (7 out of 9, 78%) robotic systems no longer in use since the fully active ROBODOC System® and the CASPAR System® are now outdated and replaced by the newer systems. Functional outcomes were evaluated using various systems, which made it difficult to organize it and give an overall interpretation. The majority of the studies included (5 out of 9) were level of evidence IV with reported selection, detection and performance bias.
Conclusions
This systematic review of comparative studies supports that robotic-assisted TKA offers benefits in accuracy, precision and alignment correction with lower outliers and reduced errors in coronal and sagittal planes. Patients’ satisfaction in RA-TKA is increased in the early postoperative time with better clinical outcomes compared to CM-TKA. Short-to-mid-term survivorship and complication rates did not show significant difference among the two groups. However, further high-quality long-term studies and RCTs comparing modern robotic systems and conventional manual technique are needed to validate the relationship between improved accuracy and implant survivorship, complication rates, functional outcomes and cost-effectiveness.
Funding Statement
Funding: none.
References
- 1.Bourne RB, Chesworth BM, Davis AM, et al. Patient satisfaction after total knee arthroplasty: Who is satisfied and who is not? Clin Orthop Relat Res 2010;468: 57-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kim TK, Chang CB, Kang YG, et al. Causes and Predictors of Patient’s Dissatisfaction After Uncomplicated Total Knee Arthroplasty. J Arthroplasty 2009;24:263-71. [DOI] [PubMed] [Google Scholar]
- 3.Kurtz S, Ong K, Lau E, et al. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Jt Surg - Ser A 2007;89:780-5. [DOI] [PubMed] [Google Scholar]
- 4.Gunaratne R, Pratt DN, Banda J, et al. Patient Dissatisfaction Following Total Knee Arthroplasty: A Systematic Review of the Literature. J Arthroplasty 2017;32:3854-60. [DOI] [PubMed] [Google Scholar]
- 5.Noble PC, Conditt MA, Cook KF, Mathis KB. The John Insall Award: Patient expectations affect satisfaction with total knee arthroplasty. Clin Orthop Relat Res 2006;35-43. [DOI] [PubMed] [Google Scholar]
- 6.Abdel MP, Ledford CK, Kobic A, et al. Contemporary failure aetiologies of the primary, posterior-stabilised total knee arthroplasty. Bone Jt J 2017;99B:647-52. [DOI] [PubMed] [Google Scholar]
- 7.Chawla H, Nwachukwu BU, Van Der List JP, et al. Cost effectiveness of patellofemoral versus total knee arthroplasty in younger patients. Bone Jt J 2017;99B:1028-36. [DOI] [PubMed] [Google Scholar]
- 8.Devers BN, Conditt MA, Jamieson ML, et al. Does Greater Knee Flexion Increase Patient Function and Satisfaction After Total Knee Arthroplasty? J Arthroplasty 2011;26:178-86. [DOI] [PubMed] [Google Scholar]
- 9.Cerciello S, Robin J, Lustig S, et al. The role of patelloplasty in total knee arthroplasty. Arch Orthop Trauma Surg 2016;136:1607-13. [DOI] [PubMed] [Google Scholar]
- 10.Saccomanno MF, Sircana G, Masci G, et al. Allergy in total knee replacement surgery: Is it a real problem? World J Orthop 2019;10:63-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Khlopas A, Sodhi N, Sultan AA, et al. Robotic Arm-Assisted Total Knee Arthroplasty. J Arthroplasty 2018;33: 2002-6. [DOI] [PubMed] [Google Scholar]
- 12.Ren Y, Cao S, Wu J, et al. Efficacy and reliability of active robotic-assisted total knee arthroplasty compared with conventional total knee arthroplasty: A systematic review and meta-analysis. Postgrad Med J 2019;125-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kayani B, Konan S, Ayuob A, et al. Robotic technology in total knee arthroplasty: a systematic review. EFORT Open Rev 2019;4:611-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Abdel MP, Oussedik S, Parratte S, et al. Coronal alignment in total knee replacement: historical review, contemporary analysis, and future direction. Bone Jt J. 2014;96 B:857-62. [DOI] [PubMed] [Google Scholar]
- 15.Mannan A, Vun J, Lodge C, et al. Increased precision of coronal plane outcomes in robotic-assisted total knee arthroplasty: A systematic review and meta-analysis. Surgeon 2018;16:237-44. [DOI] [PubMed] [Google Scholar]
- 16.Siebert W, Mai S, Kober R, Heeckt PF. Technique and first clinical results of robot-assisted total knee replacement. Knee 2002;9:173-80. [DOI] [PubMed] [Google Scholar]
- 17.Bautista M, Manrique J, Hozack WJ. Robotics in Total Knee Arthroplasty. J Knee Surg 2019;32:600-6. [DOI] [PubMed] [Google Scholar]
- 18.Park SE, Lee CT. Comparison of Robotic-Assisted and Conventional Manual Implantation of a Primary Total Knee Arthroplasty. J Arthroplasty 2007; 22:1054-9. [DOI] [PubMed] [Google Scholar]
- 19.Parratte S, Price AJ, Jeys LM, et al. Accuracy of a New Robotically Assisted Technique for Total Knee Arthroplasty: A Cadaveric Study. J Arthroplasty 2019;34:2799-803. [DOI] [PubMed] [Google Scholar]
- 20.Bargar WL. Robots in orthopaedic surgery: Past, present, and future. Clin Orthop Relat Res 2007;31-6. [PubMed] [Google Scholar]
- 21.Kayani B, Konan S, Pietrzak JRT, et al. The learning curve associated with robotic-arm assisted unicompartmental knee arthroplasty. Bone Jt J 2018;100B: 1033-42. [DOI] [PubMed] [Google Scholar]
- 22.Sambandam SN, Gul A, Priyanka P. Analysis of methodological deficiencies of studies reporting surgical outcome following cemented total-joint arthroplasty of trapezio-metacarpal joint of the thumb. Int Orthop 2007;31:639-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Song EK, Seon JK, Yim JH, et al. Robotic-assisted TKA reduces postoperative alignment outliers and improves gap balance compared to conventional TKA knee. Clin Orthop Relat Res 2013;471:118-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Liow MHL, Goh GSH, Wong MK, et al. Robotic-assisted total knee arthroplasty may lead to improvement in quality-oflife measures: a 2-year follow-up of a prospective randomized trial. Knee Surgery, Sport Traumatol Arthrosc 2016;25:2942-51. [DOI] [PubMed] [Google Scholar]
- 25.Khlopas A, Sodhi N, Hozack W, et al. Patient-Reported Functional and Satisfaction Outcomes after Robotic- Arm-Assisted Total Knee Arthroplasty: Early Results of a Prospective Multicenter Investigation. J Knee Surg 2019;10075. [DOI] [PubMed] [Google Scholar]
- 26.Song EK, Seon JK, Park SJ, et al. Simultaneous bilateral total knee arthroplasty with robotic and conventional techniques: A prospective, randomized study. Knee Surgery, Sport Traumatol Arthrosc 2011;19:1069-76. [DOI] [PubMed] [Google Scholar]
- 27.Yang HY, Seon JK, Shin YJ, et al. Robotic total knee arthroplasty with a cruciate-retaining implant: A 10-year follow-up study. CiOS Clin Orthop Surg 2017;9:169-76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cho KJ, Seon JK, Jang WY, et al. Robotic versus conventional primary total knee arthroplasty: clinical and radiological long-term results with a minimum follow-up of ten years. Int Orthop 2019;43:1345-54. [DOI] [PubMed] [Google Scholar]
- 29.Marchand RC, Sodhi N, Khlopas A, et al. Patient Satisfaction Outcomes after Robotic Arm-Assisted Total Knee Arthroplasty: A Short-Term Evaluation. J Knee Surg 2017;30:849-53. [DOI] [PubMed] [Google Scholar]
- 30.Choong PF, Dowsey MM, Stoney JD. Does Accurate Anatomical Alignment Result in Better Function and Quality of Life? Comparing Conventional and Computer-Assisted Total Knee Arthroplasty. J Arthroplasty 2009;24: 560-9. [DOI] [PubMed] [Google Scholar]
- 31.Nelson CL, Kim J, Lotke PA. Stiffness After Total Knee Arthroplasty Surgical Technique. Jbjs 2004;86:1479-84. [PubMed] [Google Scholar]
- 32.Naranje S, Lendway L, Mehle S, Gioe TJ. Does Operative Time Affect Infection Rate in Primary Total Knee Arthroplasty? Clin Orthop Relat Res 2015;473:64-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Peersman G, Laskin R, Davis J, et al. Prolonged operative time correlates with increased infection rate after total knee arthroplasty. HSS J 2006;2:70-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hampp E, Scholl L, Prieto M, et al. Robotic-Arm Assisted Total Knee Arthroplasty Demonstrated Greater Accuracy to Plan Compared to Manual Technique 2018;1:299-293. [DOI] [PubMed] [Google Scholar]
- 35.Sodhi N, Khlopas A, Piuzzi N, et al. The Learning Curve Associated with Robotic Total Knee Arthroplasty. J Knee Surg 2018:17-21. [DOI] [PubMed] [Google Scholar]
- 36.Kayani B, Konan S, Huq SS, et al. Robotic-arm assisted total knee arthroplasty has a learning curve of seven cases for integration into the surgical workflow but no learning curve effect for accuracy of implant positioning. Knee Surg Sport Traumatol Arthrosc 2019;27:1132-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cool CL, Jacofsky DJ, Seeger KA, et al. A 90-day episode-of-care cost analysis of robotic-arm assisted total knee arthroplasty. J Comp Eff Res 2019;8: 327-36. [DOI] [PubMed] [Google Scholar]
- 38.Khlopas A, Chughtai M, Hampp EL, et al. Robotic-Arm Assisted Total Knee Arthroplasty Demonstrated Soft Tissue Protection. Surg Technol Int 2017;30: 441-6. [PubMed] [Google Scholar]
- 39.Kayani B, Konan S, Pietrzak JRT, Haddad FS. Iatrogenic Bone and Soft Tissue Trauma in Robotic-Arm Assisted Total Knee Arthroplasty Compared With Conventional Jig-Based Total Knee Arthroplasty: A Prospective Cohort Study and Validation of a New Classification System. J Arthroplasty 2018;33:2496-501. [DOI] [PubMed] [Google Scholar]
- 40.Pearle AD, Van Der List JP, Lee L, et al. Survivorship and patient satisfaction of robotic-assisted medial unicompartmental knee arthroplasty at a minimum two-year follow-up. Knee 2017;24:419-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zhang F, Li H, Ba Z, et al. Robotic armassisted vs conventional unicompartmental knee arthroplasty. Medicine (Baltimore) 2019;98:e16968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Batailler C, White N, Ranaldi FM, et al. Improved implant position and lower revision rate with robotic-assisted unicompartmental knee arthroplasty. Knee Surg Sport Traumatol Arthrosc 2019;27:1232-40. [DOI] [PubMed] [Google Scholar]


