Abstract
Corynebacterium jeikeium is a commensal bacterium that colonizes human skin, and it is part of the normal bacterial flora. In non-risk subjects, it can be the cause of bad body smell due to the generation of volatile odorous metabolites, especially in the wet parts of the body that this bacterium often colonizes (i.e., groin and axillary regions). Importantly, in the last few decades, there have been increasing cases of serious infections provoked by this bacterium, especially in immunocompromised or hospitalized patients who have undergone installation of prostheses or catheters. The ease in developing resistance to commonly-used antibiotics (i.e., glycopeptides) has made the search for new antimicrobial compounds of clinical importance. Here, for the first time, we characterize the antimicrobial activity of some selected frog skin-derived antimicrobial peptides (AMPs) against C. jeikeium by determining their minimum inhibitory and bactericidal concentrations (MIC and MBC) by a microdilution method. The results highlight esculentin-1b(1-18) [Esc(1-18)] and esculentin-1a(1-21) [Esc(1-21)] as the most active AMPs with MIC and MBC of 4–8 and 0.125–0.25 µM, respectively, along with a non-toxic profile after a short- and long-term (40 min and 24 h) treatment of mammalian cells. Overall, these findings indicate the high potentiality of Esc(1-18) and Esc(1-21) as (i) alternative antimicrobials against C. jeikeium infections and/or as (ii) additives in cosmetic products (creams, deodorants) to reduce the production of bad body odor.
Keywords: Corynebacterium jeikeium, antibiotic resistance, antimicrobial peptides, minimum inhibitory concentration, minimum bactericidal concentration, hemolysis, cytotoxicity, cosmetics
1. Introduction
Corynebacteria are Gram-positive, aerobic, catalase-positive, generally non-motile rods, and this genus comprises Corynebacterium diphtheriae and other different species defined as nondiphtheriae corynebacteria (diphtheroids) [1,2]. Corynebacterium jeikeium (commonly known as group JK corynebacterium by the Centers for Disease Control and Prevention) is part of the human skin flora as Staphylococcus epidermidis and is among the most common bacteria isolated from hospitalized patients [3,4,5]. In particular, its colonization affects groin and axilla where the moist environment favors the formation of malodor substrates leading, in some cases, to an unpleasant body smell [6,7]. C. jeikeium is ubiquitous and largely innocuous, and importantly, it offers substantial epidermal protection thanks to the production of bacteriocin-like compounds that are used to counteract possible pathogenic competitors [8]. However, in the last few decades, C. jeikeium has become the etiological agent of infections associated with skin wounds and implanted medical devices, as well as of nosocomial infections especially in hospitalized patients [1]. Indeed, in these latter, due to the impaired immune system, “helpful” microorganisms belonging to the commensal flora and regularly living within the host can turn into opportunistic pathogens leading to the appearance of infections with an illness state [9,10,11,12,13]. Considering the rising enhancement of people recovering from chemotherapy treatments or with a compromised defense mechanism, the number of these nosocomial infections (encompassing endocarditis, pneumoniae, peritonitis, and enteritis) is actually extremely alarming [14,15]. The first line therapies to combat C. jeikeium-associated infections include glycopeptides vancomycin or teicoplanin. Unfortunately, the inappropriate usage of these antibiotics and the high selective pressure have made this bacterium resistant to vancomycin, teicoplanin, linezolid, quinupristin-dalfopristin, daptomycin, and tigecycline [16]. Hence, new agents with antimicrobial activity are urgently needed. Naturally-occurring antimicrobial peptides (AMPs) represent a valid alternative to traditional antibiotics, as they are active against a broad spectrum of microbes, from Gram-positive and Gram-negative bacteria to fungi and viruses [17,18,19,20,21,22,23]. Furthermore, compared to conventional drugs, they have further biological functions, such as a wound-healing, antidiabetic, anti-inflammatory, and immune-modulatory activities [24,25,26,27,28,29,30,31]. Amphibian skin secretion is considered a rich source of broad-spectrum AMPs, and over the years, numerous peptides have been isolated and classified into the corresponding families, such as esculentins, temporins, and bombinins H [32,33]. Recently, we characterized the potent effectiveness of two derivatives of the N-terminal part of two frog skin AMPs, i.e., esculentin-1a and -1b, namely esculentin-1a(1-21) (Esc(1-21)) and esculentin-1b(1-18) (Esc(1-18)), respectively, especially against alarming human pathogens, such as Pseudomonas aeruginosa and Candida albicans, either in vitro or in vivo [34,35,36]. Here, for the first time, we explore the efficacy of these two alpha-helical peptides against C. jeikeium by determining their minimum inhibitory concentrations (MIC) and compare this activity with that of other peptide isoforms belonging to different AMP families (i.e., the alpha-helical temporin A, temporin B, temporin G, and bombinin H2). The minimum bactericidal concentration (MBC) of both esculentin derivatives is also determined, along with mechanistic studies to gain insight into their mode of action. Moreover, to evaluate the safety profile of these peptides for the development of new antimicrobials, their hemolytic activity on mammalian erythrocytes and their effect on the viability of three different mammalian cell lines are also investigated.
2. Results
2.1. Antimicrobial Activity of Frog Skin-Derived AMPs
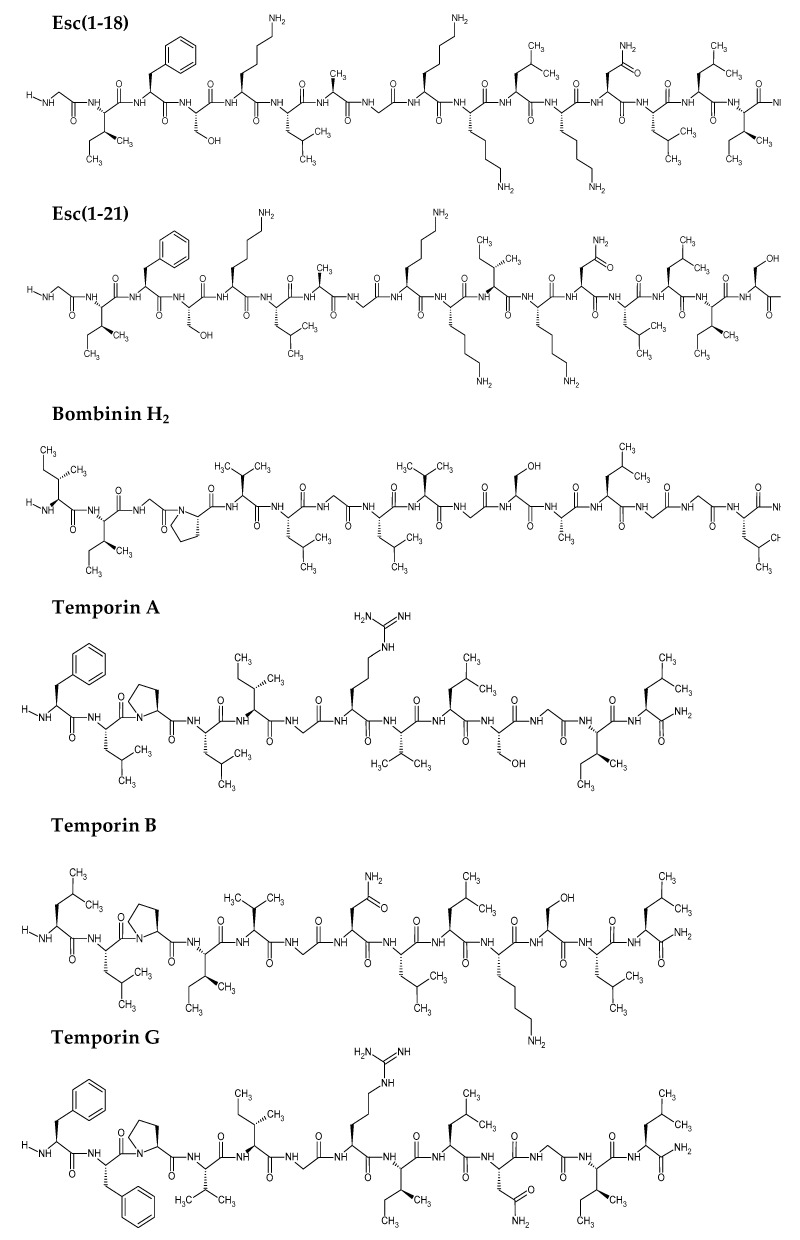
Esc(1-18) and Esc(1-21), collectively named esculentin peptides, as well as the frog skin-derived AMPs temporin A, temporin B, temporin G, and bombinin H2 (Figure 1) were tested against the reference strain C. jeikeium ATCC BAA-949 to assess the MIC, i.e., the lowest peptide concentration able to visually inhibit microbial growth after 20 h of incubation at 37 °C.
Figure 1.
Names and primary structures of the selected peptides. Chemical structures were drawn with ChemSketch, Advanced Chemistry Development, Inc. (ACD/Labs).
As reported in Table 1, esculentin peptides showed the strongest efficacy in inhibiting C. jeikeium growth with MICs of 4 µM and 0.125 µM for Esc(1-18) and Esc(1-21), respectively. This result was quite surprising, considering that esculentin peptides have a well-documented preferential activity towards Gram-negative bacteria [36,37]. In comparison, MICs ranging from 8 to 16 µM were obtained for the other selected AMPs. Unlike temporins and bombinin H2, esculentin peptides are lysine-rich AMPs with a higher cationicity and lower hydrophobicity, as indicated by the corresponding grand average of hydropathicity index (GRAVY; Table 1), which is used to represent the hydrophobicity value of a peptide [38].
Table 1.
Antimicrobial activity (MIC) of different frog skin AMPs against C. jeikeium. The net charge at neutral pH and grand average of hydropathicity (GRAVY) of each peptide are also indicated. GRAVY values were provided by https://web.expasy.org [39].
| Peptide | Sequence | MIC (µM) | Net Charge | GRAVY |
|---|---|---|---|---|
| Esc(1-18) | GIFSKLAGKKLKNLLISG-NH2 | 4 | +5 | 0.383 |
| Esc(1-21) | GIFSKLAGKKIKNLLISGLKG-NH2 | 0.125 | +6 | 0.338 |
| Temporin A | FLPLIGRVLSGIL-NH2 | 8 | +2 | 1.808 |
| Temporin B | LLPIVGNLLKSLL-NH2 | 8 | +2 | 1.638 |
| Temporin G | FFPVIGRILNGIL-NH2 | 16 | +2 | 1.577 |
| Bombinin H2 | IIGPVLGLVGSALGGLLKKI-NH2 | 8 | +3 | 1.525 |
Interestingly, when the most active esculentin peptides were tested for their bactericidal activity, they were found to cause almost the complete killing of the bacterial population with an MBC (i.e., the lowest peptide concentration able to cause a ≥3 log reduction in the number of bacterial cells) 2-fold higher than the corresponding MIC, i.e., 8 µM and 0.25 µM for Esc(1-18) and Esc(1-21), respectively.
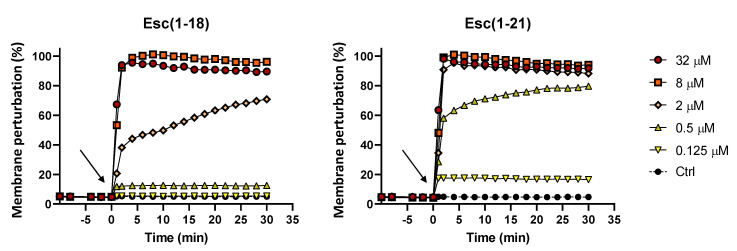
2.2. Membrane Permeabilization
Esculentin peptides are known to display an antibacterial activity mainly through a membrane-perturbing mechanism of action. To verify their ability to perturb the cytoplasmic membrane of Gram-positive bacteria, such as C. jeikeium, a Sytox Green assay was performed. Sytox Green is a fluorescent probe unable to cross intact membranes, and its fluorescence intensity significantly increases upon binding to nucleic acids. As shown in Figure 2, the rapid increase of the fluorescent signal immediately after peptide addition to the bacterial cells (arrow) indicated that the perturbation of the membrane was the result of the peptide-induced membrane damage, allowing the internalization of the probe with a consequent binding to the bacterial DNA. Both esculentin AMPs manifested a dose-dependent fast kinetic membrane destabilization with a total perturbation of the phospholipid bilayer already within the first minutes of treatment at the highest concentration of 32 µM. According to the MIC and MBC values, the most active Esc(1-21) exhibited a stronger effect compared to Esc(1-18), even at a concentration as low as 0.5 µM with about 60% membrane damage within the first 2 min.
Figure 2.
Membrane perturbation assay performed with the Sytox Green dye. The percentage of membrane damage was calculated with respect to the maximum membrane permeabilization obtained with the highest peptide concentration (32 µM) and the addition of 1 mM EDTA + 0.5% Triton X-100. Arrows indicate the addition of the peptide. Data points are the mean of triplicate measurements from a single experiment representative of three independent experiments. Controls (Ctrl) are cells not treated with the peptides.
2.3. Cytotoxicity
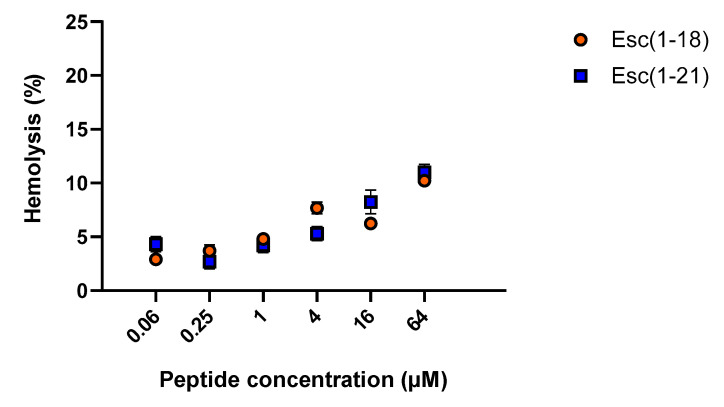
2.3.1. Hemolytic Activity
To evaluate the potential cytotoxicity of esculentin peptides in the short term, they were tested for the ability to lyse mammalian red blood cells after 40 min of treatment at 37 °C. Both AMPs caused a weak and similar hemolysis with an ~10% release of hemoglobin at a concentration of 64 µM, which is significantly higher than the antimicrobial dosages, thus suggesting their safety profile for short-term treatment (Figure 3).
Figure 3.
Effect of Esc(1-18) and Esc(1-21) on mammalian red blood cells after 40 min of incubation at 37 °C. The percentage of hemolysis was calculated with respect to the control (cells treated with vehicle). Data are the means ± standard error of the mean (SEM) of three independent experiments.
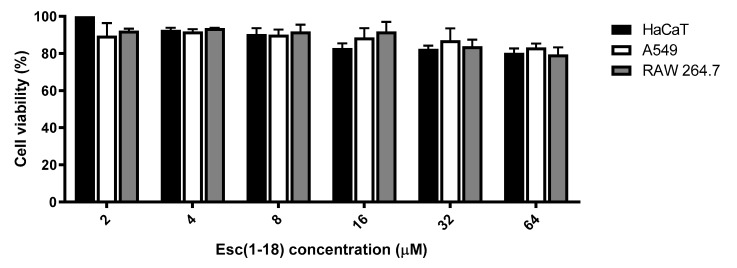
2.3.2. Peptides’ Effect on the Metabolic Activity of Mammalian Cells
Since the long-term cytotoxicity of Esc(1-21) was extensively described in earlier studies [40,41], we similarly investigated the potential cytotoxic effect of Esc(1-18) after a long time interval (24 h) against three different mammalian cell lines, i.e., the human immortalized keratinocytes (HaCaT cells), the human alveolar epithelial A549 cells, and the murine RAW 264.7 macrophages, by the 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT) assay (see Materials and Methods). Figure 4 shows the percentage of cell viability after 24 h of exposure to Esc(1-18) in the concentration range of 2–64 µM. Even at the highest peptide concentration tested, only a weak reduction in the percentage of metabolically-active cells was observed (about 20%) compared to the untreated control samples. Similar data were previously collected for viability assays performed with Esc(1-21) at the same concentrations, except for the greater cytotoxicity against macrophages at 64 µM (i.e., about 50% cell viability) [41]. Lacking the harmful effect of esculentin peptides, particularly for Esc(1-18) at the antimicrobial concentrations (MIC and MBC values), suggested they are safe compounds, also for long-term treatment.
Figure 4.
Dose-dependent effect of Esc(1-18) at different concentrations on the viability of HaCaT, A549, and RAW 264.7 cell lines after 24 h of treatment. The percentage of metabolically-active cells compared to untreated control samples is reported on the Y-axis. All data are the mean of three independent experiments ± SEM.
3. Discussion
Having been considered harmless and protective to humans, C. jeikeium has turned into a relevant etiological agent of dangerous infections, especially in hospitalized people or patients under chemotherapy. These include skin and wound infections, meningitis, enteritis, osteomyelitis, pyelonephritis, prosthetic joint infections, peritonitis, pneumonia, and liver abscess in patients with AIDS [42,43,44,45,46,47,48,49,50]. Unfortunately, current antibiotic therapies are often ineffective due to the onset of antibiotic resistance [51,52]. Interestingly, AMPs are promising hits to open the door for the generation of a new class of antimicrobials. In recent years, we thoroughly investigated the activity of Esc(1-18) and Esc(1-21) against a large number of microorganisms. However, no studies have been conducted so far for these peptides, as well as for other AMPs, against C. jeikeium. Here, for the first time, we analyzed the effect of some frog skin AMPs against this bacterium and selected the esculentin peptides as the most active molecules with an MIC of 0.125 and 4 µM for Esc(1-21) and Esc(1-18), respectively. This outcome is in sharp contrast with the weaker activity of Esc(1-21) previously recorded against other Gram-positive bacteria (e.g., Staphylococcus aureus, S. epidermidis), where MICs ranging from 1 to 64 µM were found [37]. Note that both the higher cationicity and lower hydrophobicity of esculentin peptides compared to the other AMPs used for comparison (Table 1) would promote the peptide interaction with the anionic phospholipid headgroups of the bacterial membrane, thus explaining the higher antimicrobial activity of esculentin peptides. However, we cannot exclude the contribution of other chemical/physical features of the peptides (i.e., amphipathicity, length, oligomeric state) for the final outcome. Analogously, among esculentin peptides, the significantly higher antibacterial activity of Esc(1-21) compared to the shorter analog Esc(1-18) is likely due to the higher net positive charge and longer size of the former. Indeed, a minimum length for a peptide in alpha-helical conformation to span and perturb a phospholipid bilayer (∼30 Å thick) is 20 amino acids. Both esculentin peptides displayed the capability to kill C. jeikeium at a concentration two-fold higher than the MIC. Remarkably, despite the obtained MICs being comparable to those of traditional antibiotics [53,54], we have to take into account the additional advantageous features owned by these AMPs. As an example, we already demonstrated the ability of Esc(1-21) to promote re-epithelialization of a pseudo-wound by stimulating the migration of human keratinocytes, a relevant property for the therapeutic development of these peptides. Indeed, besides contributing to the elimination of C. jeikeium skin/wound-associated infections, the peptide would help to repair the damaged epithelial tissue. In addition, the membrane-perturbing activity makes these AMPs even more interesting compounds, as bacteria are less prone to develop resistance to them. This is because the acquisition of resistance to AMPs would imply a complete reorganization of the bacterial membrane; an energetically unfavorable process not compatible with bacterial survival [55,56,57,58,59,60]. Moreover, in contrast with mammalian AMPs, esculentin peptides can preserve antimicrobial activity in the presence of biological fluids [37]. Esc(1-21) was found to induce a complete permeabilization of the bacterial membrane at a concentration range from 2 to 32 µM. Differently, only 50% of the membrane perturbation had been previously achieved by this peptide against other Gram-positive bacteria (i.e., Streptococcus agalactiae ATCC 13813) at the higher concentration of 50 µM [36]. Finally, both esculentin peptides displayed a non-toxic profile on different types of mammalian cells, e.g., erythrocytes, keratinocytes, alveolar epithelial cells, and macrophages, either after a short- or long-term treatment. Importantly, HaCaT cells are a reliable and helpful in vitro model to determine the toxicity of various agents on the skin layer because keratinocytes represent 95% of the epidermal cells [61,62]. In comparison, the evaluation of the peptides’ effect against lung epithelial cells, i.e., the A549 alveolar cell line, and immune cells, like macrophages, is of great interest for their crucial role in orchestrating both immune defense and inflammatory responses [63,64,65]. It is noteworthy that esculentin peptides may be developed not only as alternative antimicrobials against C. jeikeium infections, but also as additives in cosmetic products (e.g., creams, deodorants) aimed at countering the colonization of C. jeikeium and, as a result, axillary malodor formation. In fact, this bacterium is involved in the generation of volatile odorous metabolites, attributed to the bacterial degradation of skin lipids and specific odor precursors that are responsible for the unpleasant human body smell, in sweat secretions [6,7,66]. Frequent showers and different soaps cannot solve the problem of the so-called “wild axilla”, thus provoking serious psychological concerns. Patients suffering from bad smell can adopt various atypical behaviors minimizing social interactions. This can lead to anxiety, decreased self-esteem, and low quality of life due to social difficulties, e.g., avoiding intimacy [67,68]. Overall, the potent antimicrobial action of esculentin peptides, especially of Esc(1-21) [MIC, 0.125 µM], and their safety profile make them attractive molecules for therapeutic and/or cosmetic application. Based on the amino acid sequence analysis conducted through bioinformatic platforms (https://webs.iiitd.edu.in/raghava/algpred/submission.html and https://web.expasy.org/protparam, [39,69]), it has been predicted that esculentin peptides are devoid of allergenic properties and have an estimated half-life time in mammalian reticulocytes (in vitro) of about 30 h, which is a compatible time for possible daily usage. This is also consistent with our recent in vivo efficacy studies showing: (i) an antimicrobial efficacy of Esc(1-21), 36 h after intra-tracheal administration in murine models of acute bacterial lung infection; and (ii) the absence of immunogenicity in mice [70,71]. In the work of Rahnamaeian and Vilcinskas, the authors already emphasized the feasibility of short-sized AMPs as cosmetic ingredients of topical formulations such as creams, lotions, shampoos, and wound dressings to deter dermatological pathogens [72]. As proof of this, Haisma and coworkers designed cream/gel formulations (e.g., a water-in-oil cream with lanolin, an oil-in-water cream with polyethylene glycol hexadecyl ether, and a hypromellose gel) containing the LL-37-derived AMP P60.4Ac to successfully eradicate methicillin-resistant S. aureus from colonized human epidermal models [73]. Taken all together, the data presented in this work demonstrated for the first time the high potentiality of esculentin peptides as a new choice to fight the undesirable infections caused by C. jeikeium in both healthy and susceptible individuals.
4. Materials and Methods
4.1. Microorganism and Cell Lines
The microorganism used in the study was the reference strain C. jeikeium ATCC BAA-949. The culture media used for bacterial growth and the various assays were tryptone soy broth and agar (TSB and TSA, respectively) supplemented with 0.1% Tween 80 (TSB+ and TSA+). Furthermore, the following cell cultures were employed: the human immortalized keratinocyte cell line, HaCaT (from AddexBio, San Diego, CA, USA), the human type II alveolar epithelial cell line A549, and the murine RAW 264.7 macrophage cell line (from the American Type Culture Collection, Manassas, Va). The three cell lines were cultured in Dulbecco’s Modified Eagle’s Medium supplemented with 4 mM glutamine (for HaCaT cells) or 2 mM glutamine (for the A549 and RAW 264.7 cell lines), 10% heat-inactivated fetal bovine serum (FBS), and 0.1 mg/mL of penicillin and streptomycin at 37 °C and 5% CO2, in 25 cm2 or 75 cm2 flasks. In the case of macrophages, sodium pyruvate and non-essential amino acids were also added to the culture medium.
4.2. Peptides
Esc(1-18), Esc(1-21), temporin A, temporin B, temporin G, and bombinin H2 were purchased from Biomatik (USA/Canada). Each peptide was assembled by stepwise solid-phase synthesis and purified via reverse-phase high-performance liquid chromatography to a purity of 98% using a gradient of acetonitrile in 0.1% aqueous trifluoroacetic acid (from 28% to 100% in 30 min) at a flow rate of 1.0 mL/min. Molecular masses were verified by electron spray ionization mass spectrometry.
4.3. Antimicrobial Assays
The MIC of the different AMPs against C. jeikeium ATCC BAA-949 were determined following the previously described procedure with some modifications [57]. The bacterium was grown in TSB+ up to an optical density (O.D.) of 0.8 (λ = 590 nm) and diluted to reach a concentration of 2× 106 colony forming units (CFU) per mL. Aliquots (50 µL) of this dilution were added to 50 µL of TSB+ supplemented with 2-fold serial dilution of peptides previously dispensed in the wells of a 96 well plate. Controls were bacteria not treated with the peptides. The plate was then incubated for 20 h at 37 °C, and the MIC was defined as the lowest peptide concentration that visually inhibits microbial growth (absence of turbidity) after 20 h incubation. For determining the MBC of the most potent peptides, i.e., Esc(1-18) and Esc(1-21), aliquots from MIC, 2× MIC and 4× MIC wells were spread onto TSA+ plates for CFU counting after an overnight incubation. MBC was defined as the lowest peptide concentration able to cause a ≥3 log reduction in the number of cells of the initial inoculum after 20 h of incubation.
4.4. Membrane Permeabilization: Sytox Green Assay
To assess the ability of Esc(1-21) and Esc(1-18) to perturb the cytoplasmic membrane permeability of C. jeikeium ATCC BAA-949, the Sytox Green assay was performed as previously reported, with some modifications [35]. Approximately 1× 107 CFU/mL were incubated with 1 μM Sytox Green in PBS for 5 min in the dark. After peptide addition, changes in fluorescence intensity (λ exc = 485 nm, λ ems = 535 nm) caused by the binding of the dye to intracellular DNA were monitored for 30 min in the microplate reader (Infinite M200, Tecan, Salzburg, Austria) at 37 °C and plotted as the percentage of membrane perturbation relative to that obtained after treating bacteria with the highest peptide concentration (32 μM) and the addition of 1 mM EDTA + 0.5% Triton X-100 (final concentration). The peptide concentrations ranged from 0.125 to 32 μM. Controls were cells not treated with the peptides.
4.5. Hemolytic Assay
The short-term cytotoxicity of Esc(1-18) and Esc(1-21) was evaluated against sheep red blood cells (OXOID, SR0051D) by adapting the already described procedure [74]. Erythrocytes (O.D. of 0.5 at λ= 500 nm) in 0.9 % (w/v) NaCl were incubated for 40 min at 37 °C with 4-fold serial dilutions of Esc(1-18) and Esc(1-21) (0.06–64 μM). Complete lysis was obtained by resuspending erythrocytes in distilled water. All samples were centrifuged for 5 min at 900× g, and the amount of hemoglobin released in the supernatant by lysed red blood cells was measured at 415 nm using a microplate reader (Infinite M200; Tecan, Salzburg, Austria).
4.6. Cytotoxicity Test on Mammalian Cell Lines
The long-term cytotoxicity of Esc(1-18) was investigated by the MTT assay according to [41], as previously carried out for Esc(1-21). MTT (Sigma-Aldrich, St. Luis, MO, USA) is a yellow dye that, upon intracellular entry, is converted into insoluble and dark purple formazan crystals by mitochondrial dehydrogenases. This reduction occurs only in metabolically-active cells; therefore, the colorimetric absorbance is directly proportional to the cell viability. About 4 × 104 cells, suspended in DMEM supplemented with glutamine (at the concentration indicated for each cell line) and 2% FBS without antibiotic, were plated in triplicate wells of a microtiter plate. After overnight incubation at 37 °C and 5% CO2, the medium was replaced by fresh serum-free medium containing the peptide at different concentrations. Cells not treated with the peptide were used as controls. After 24 h of incubation at 37 °C in a 5% CO2 atmosphere, the medium was removed, and MTT solution in Hank’s buffer (final concentration 0.5 mg/mL) was added to each well. The plate was incubated for 4 h at 37 °C and 5% CO2. Afterwards, the formazan crystals were dissolved by adding acidified isopropanol, and the absorbance of each well was measured at 570 nm using the microplate reader (Infinite M200; Tecan, Salzburg, Austria) (cell viability was calculated by assuming a percentage of 100% for control cells without any peptide treatment).
4.7. Statistical Analysis
Unless otherwise specified, all experiments were performed three times, and the obtained values were reported as the mean ± SEM.
5. Conclusions
AMPs are an effective alternative to conventional antibiotics in the battle to defeat microbial pathogens, due to their membrane-active microbicidal activity and to further biological properties. In the last few decades, C. jeikeium raised concerns in the clinical field because of the increased occurrence of its infections, especially in immunocompromised or hospitalized subjects. In non-risk patients, this bacterium normally colonizes skin (e.g., axilla), causing a bad smell. Here, for the first time, we characterized the efficacy of two derivatives of esculentin-1 peptides, i.e., Esc(1-18) and Esc(1-21), against C. jeikeium and highlighted their high potentiality as new antimicrobials with negligible cytotoxicity. Beyond the clinical relevance that these peptides can have in the scenario of antibiotic resistance, they represent excellent candidates to be used at low concentrations in the production of cosmetics designed to reduce bad body odors.
Author Contributions
B.C., M.R.L., and F.C. performed the experiments and contributed to writing the manuscript; W.V. contributed to analyzing the data; M.L.M. and V.D.C. conceived of the experimental work, analyzed the data, and critically revised the manuscript. All authors have read and agreed to the published version of the manuscript。
Funding
This work was supported by grants of Sapienza University (Projects RM11816436113D8A and RM11916B6A28725C) and by a grant from Pasteur-Italia Fondazione Cenci Bolognetti (Anna Tramontano 2018).
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Bernard K. The genus corynebacterium and other medically relevant coryneform-like bacteria. J. Clin. Microbiol. 2012;50:3152–3158. doi: 10.1128/JCM.00796-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cogen A.L., Nizet V., Gallo R.L. Skin microbiota: a source of disease or defence? Br. J. Dermatol. 2008;158:442–455. doi: 10.1111/j.1365-2133.2008.08437.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Coyle M.B., Lipsky B.A. Coryneform bacteria in infectious diseases: clinical and laboratory aspects. Clin. Microbiol. Rev. 1990;3:227–246. doi: 10.1128/CMR.3.3.227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Larson E.L., McGinley K.J., Leyden J.J., Cooley M.E., Talbot G.H. Skin colonization with antibiotic-resistant (JK group) and antibiotic-sensitive lipophilic diphtheroids in hospitalized and normal adults. J. Infect. Dis. 1986;153:701–706. doi: 10.1093/infdis/153.4.701. [DOI] [PubMed] [Google Scholar]
- 5.Altonsy M.O., Kurwa H.A., Lauzon G.J., Amrein M., Gerber A.N., Almishri W., Mydlarski P.R. Corynebacterium tuberculostearicum, a human skin colonizer, induces the canonical nuclear factor-kappaB inflammatory signaling pathway in human skin cells. Immun. Inflamm. Dis. 2020;8:62–79. doi: 10.1002/iid3.284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Barzantny H., Brune I., Tauch A. Molecular basis of human body odour formation: insights deduced from corynebacterial genome sequences. Int. J. Cosmet. Sci. 2012;34:2–11. doi: 10.1111/j.1468-2494.2011.00669.x. [DOI] [PubMed] [Google Scholar]
- 7.James A.G., Austin C.J., Cox D.S., Taylor D., Calvert R. Microbiological and biochemical origins of human axillary odour. FEMS Microbiol. Ecol. 2013;83:527–540. doi: 10.1111/1574-6941.12054. [DOI] [PubMed] [Google Scholar]
- 8.Noble W.C. Short Communications: Activity of Corynebacterium jeikeium Bacteriocin in Vivo. Microb. Ecol. Health Disease. 1988;1:201–203. doi: 10.3109/08910608809141536. [DOI] [Google Scholar]
- 9.Proenca J.T., Barral D.C., Gordo I. Commensal-to-pathogen transition: One-single transposon insertion results in two pathoadaptive traits in Escherichia coli -macrophage interaction. Sci. Rep. 2017;7:4504. doi: 10.1038/s41598-017-04081-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Littman D.R., Pamer E.G. Role of the commensal microbiota in normal and pathogenic host immune responses. Cell Host Microbe. 2011;10:311–323. doi: 10.1016/j.chom.2011.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lai Y., Gallo R.L. Commensal skin bacteria as the probiotic of the cutaneous immune response. Expert Rev. Dermatol. 2010;5:251–253. doi: 10.1586/edm.10.24. [DOI] [Google Scholar]
- 12.Rath S., Rud T., Karch A., Pieper D.H., Vital M. Pathogenic functions of host microbiota. Microbiome. 2018;6:174. doi: 10.1186/s40168-018-0542-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cabrera-Cancio M.R. Infections and the compromised immune status in the chronically critically ill patient: prevention strategies. Respir. Care. 2012;57:979–990. doi: 10.4187/respcare.01621. [DOI] [PubMed] [Google Scholar]
- 14.Pardo S.M.M., Patel R.H., Ramsakal A., Greene J. Disseminated Corynebacterium jeikeium Infection in Cancer Patients. Cureus. 2020;12 doi: 10.7759/cureus.8764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yang K., Kruse R.L., Lin W.J.V., Musher D.M. Corynebacteria as a cause of pulmonary infection: a case series and literature review. Pneumonia. 2018;10 doi: 10.1186/s41479-018-0054-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Letek M., Ordonez E., Fernandez-Natal I., Gil J.A., Mateos L.M. Identification of the emerging skin pathogen Corynebacterium amycolatum using PCR-amplification of the essential divIVA gene as a target. FEMS Microbiol. Lett. 2006;265:256–263. doi: 10.1111/j.1574-6968.2006.00492.x. [DOI] [PubMed] [Google Scholar]
- 17.Haney E.F., Straus S.K., Hancock R.E.W. Reassessing the Host Defense Peptide Landscape. Front. Chem. 2019;7:43. doi: 10.3389/fchem.2019.00043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Di Somma A., Moretta A., Cane C., Cirillo A., Duilio A. Antimicrobial and Antibiofilm Peptides. Biomolecules. 2020;10:652. doi: 10.3390/biom10040652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Marcocci M.E., Amatore D., Villa S., Casciaro B., Aimola P., Franci G., Grieco P., Galdiero M., Palamara A.T., Mangoni M.L., et al. The Amphibian Antimicrobial Peptide Temporin B Inhibits In Vitro Herpes Simplex Virus 1 Infection. Antimicrob. Agents Chemother. 2018;62 doi: 10.1128/AAC.02367-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lupetti A., Danesi R., van ’t Wout J.W., van Dissel J.T., Senesi S., Nibbering P.H. Antimicrobial peptides: therapeutic potential for the treatment of Candida infections. Expert Opin. Investig. Drugs. 2002;11:309–318. doi: 10.1517/13543784.11.2.309. [DOI] [PubMed] [Google Scholar]
- 21.Lazzaro B.P., Zasloff M., Rolff J. Antimicrobial peptides: Application informed by evolution. Science. 2020;368 doi: 10.1126/science.aau5480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bondaryk M., Staniszewska M., Zielinska P., Urbanczyk-Lipkowska Z. Natural Antimicrobial Peptides as Inspiration for Design of a New Generation Antifungal Compounds. J. Fungi (Basel) 2017;3:46. doi: 10.3390/jof3030046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ahmed A., Siman-Tov G., Hall G., Bhalla N., Narayanan A. Human Antimicrobial Peptides as Therapeutics for Viral Infections. Viruses. 2019;11:704. doi: 10.3390/v11080704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Musale V., Casciaro B., Mangoni M.L., Abdel-Wahab Y.H.A., Flatt P.R., Conlon J.M. Assessment of the potential of temporin peptides from the frog Rana temporaria (Ranidae) as anti-diabetic agents. J. Pept. Sci. 2018;24 doi: 10.1002/psc.3065. [DOI] [PubMed] [Google Scholar]
- 25.Thapa R.K., Diep D.B., Tonnesen H.H. Topical antimicrobial peptide formulations for wound healing: Current developments and future prospects. Acta Biomater. 2020;103:52–67. doi: 10.1016/j.actbio.2019.12.025. [DOI] [PubMed] [Google Scholar]
- 26.Brunetti J., Roscia G., Lampronti I., Gambari R., Quercini L., Falciani C., Bracci L., Pini A. Immunomodulatory and Anti-inflammatory Activity in Vitro and in Vivo of a Novel Antimicrobial Candidate. J. Biol. Chem. 2016;291:25742–25748. doi: 10.1074/jbc.M116.750257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hong Y., Lee J., Vu T.H., Lee S., Lillehoj H.S., Hong Y.H. Immunomodulatory effects of avian beta-defensin 5 in chicken macrophage cell line. Res. Vet. Sci. 2020;132:81–87. doi: 10.1016/j.rvsc.2020.06.002. [DOI] [PubMed] [Google Scholar]
- 28.Ting D.S.J., Beuerman R.W., Dua H.S., Lakshminarayanan R., Mohammed I. Strategies in Translating the Therapeutic Potentials of Host Defense Peptides. Front. Immunol. 2020;11:983. doi: 10.3389/fimmu.2020.00983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yang B., Good D., Mosaiab T., Liu W., Ni G., Kaur J., Liu X., Jessop C., Yang L., Fadhil R., et al. Significance of LL-37 on Immunomodulation and Disease Outcome. Biomed. Res. Int. 2020;2020:8349712. doi: 10.1155/2020/8349712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rauf A., Ali Shariati M., Ahmed Khalil A., Bawazeer S., Heydari M., Plygun S., Laishevtcev A., Bilal Hussain M., Alhumaydhi F.A., Aljohani A.S.M. Hepcidin, an Overview of Biochemical and Clinical Properties. Steroids. 2020:108661. doi: 10.1016/j.steroids.2020.108661. [DOI] [PubMed] [Google Scholar]
- 31.Barik A., Pandiyan R., Manthiram M., Vellaisamy B. Potential Antimicrobial Peptides Elucidation From The Marine Bacteria. Cardiovasc. Hematol. Agents Med. Chem. 2020 doi: 10.2174/1871525718666200512074400. [DOI] [PubMed] [Google Scholar]
- 32.Conlon J.M., Sonnevend A. Antimicrobial peptides in frog skin secretions. Methods Mol. Biol. 2010;618:3–14. doi: 10.1007/978-1-60761-594-1_1. [DOI] [PubMed] [Google Scholar]
- 33.Ladram A., Nicolas P. Antimicrobial peptides from frog skin: biodiversity and therapeutic promises. Front. Biosci. (Landmark Ed) 2016;21:1341–1371. doi: 10.2741/4461. [DOI] [PubMed] [Google Scholar]
- 34.Chen C., Mangoni M.L., Di Y.P. In vivo therapeutic efficacy of frog skin-derived peptides against Pseudomonas aeruginosa-induced pulmonary infection. Sci. Rep. 2017;7:8548. doi: 10.1038/s41598-017-08361-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Luca V., Olivi M., Di Grazia A., Palleschi C., Uccelletti D., Mangoni M.L. Anti-Candida activity of 1-18 fragment of the frog skin peptide esculentin-1b: in vitro and in vivo studies in a Caenorhabditis elegans infection model. Cell Mol. Life Sci. 2014;71:2535–2546. doi: 10.1007/s00018-013-1500-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Islas-Rodriguez A.E., Marcellini L., Orioni B., Barra D., Stella L., Mangoni M.L. Esculentin 1-21: a linear antimicrobial peptide from frog skin with inhibitory effect on bovine mastitis-causing bacteria. J. Pept. Sci. 2009;15:607–614. doi: 10.1002/psc.1148. [DOI] [PubMed] [Google Scholar]
- 37.Kolar S.S.N., Luca V., Baidouri H., Mannino G., McDermott A.M., Mangoni M.L. Esculentin-1a(1-21)NH2: a frog skin-derived peptide for microbial keratitis. Cell Mol. Life Sci. 2015;72:617–627. doi: 10.1007/s00018-014-1694-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chang K.Y., Yang J.R. Analysis and prediction of highly effective antiviral peptides based on random forests. PLoS ONE. 2013;8:e70166. doi: 10.1371/journal.pone.0070166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.ExPasy: Bioinformatics Resourch Portal. [(accessed on 17 July 2020)]; Available online: https://web.expasy.org/protparam.
- 40.Di Grazia A., Cappiello F., Imanishi A., Mastrofrancesco A., Picardo M., Paus R., Mangoni M.L. The Frog Skin-Derived Antimicrobial Peptide Esculentin-1a(1-21)NH2 Promotes the Migration of Human HaCaT Keratinocytes in an EGF Receptor-Dependent Manner: A Novel Promoter of Human Skin Wound Healing? PLoS ONE. 2015;10:e0128663. doi: 10.1371/journal.pone.0128663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Di Grazia A., Cappiello F., Cohen H., Casciaro B., Luca V., Pini A., Di Y.P., Shai Y., Mangoni M.L. D-Amino acids incorporation in the frog skin-derived peptide esculentin-1a(1-21)NH2 is beneficial for its multiple functions. Amino Acids. 2015;47:2505–2519. doi: 10.1007/s00726-015-2041-y. [DOI] [PubMed] [Google Scholar]
- 42.Ordonez-Palau S., Boquet D., Gil-Garcia M., Pardina-Solano M. Chronic osteomyelitis of the metatarsal sesamoid due to Corynebacterium jeikeium in a patient with rheumatoid arthritis. Joint Bone Spine. 2007;74:516–517. doi: 10.1016/j.jbspin.2007.01.026. [DOI] [PubMed] [Google Scholar]
- 43.Chao C.T., Huang J.W., Yen C.J. A rare and under-recognized pathogen in peritoneal dialysis peritonitis: Corynebacterium jeikeium. Perit. Dial. Int. 2013;33:580–581. doi: 10.3747/pdi.2013.00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Waters B.L. Pathology of culture-proven JK Corynebacterium pneumonia. An autopsy case report. Am. J. Clin. Pathol. 1989;91:616–619. doi: 10.1093/ajcp/91.5.616. [DOI] [PubMed] [Google Scholar]
- 45.Turett G.S., Fazal B.A., Johnston B.E., Telzak E.E. Liver abscess due to Corynebacterium jeikeium in a patient with AIDS. Clin. Infect. Dis. 1993;17:514–515. doi: 10.1093/clinids/17.3.514. [DOI] [PubMed] [Google Scholar]
- 46.Greene K.A., Clark R.J., Zabramski J.M. Ventricular CSF shunt infections associated with Corynebacterium jeikeium: report of three cases and review. Clin. Infect. Dis. 1993;16:139–141. doi: 10.1093/clinids/16.1.139. [DOI] [PubMed] [Google Scholar]
- 47.Yoshitomi Y., Kohno S., Koga H., Maesaki S., Higashiyama Y., Matsuda H., Mitsutake K., Miyazaki Y., Yamada H., Hara K., et al. Fatal pneumonia caused by Corynebacterium group JK after treatment of Staphylococcus aureus pneumonia. Intern. Med. 1992;31:930–932. doi: 10.2169/internalmedicine.31.930. [DOI] [PubMed] [Google Scholar]
- 48.Wang C.C., Mattson D., Wald A. Corynebacterium jeikeium bacteremia in bone marrow transplant patients with Hickman catheters. Bone Marrow Transpl. 2001;27:445–449. doi: 10.1038/sj.bmt.1702808. [DOI] [PubMed] [Google Scholar]
- 49.Tleyjeh I.M., Qutub M.O., Bakleh M., Sohail M.R., Virk A. Corynebacterium jeikeium prosthetic joint infection: case report and literature review. Scand. J. Infect. Dis. 2005;37:151–153. [PubMed] [Google Scholar]
- 50.Schiffl H., Mucke C., Lang S.M. Exit-site infections by non-diphtheria corynebacteria in CAPD. Perit. Dial. Int. 2004;24:454–459. doi: 10.1177/089686080402400510. [DOI] [PubMed] [Google Scholar]
- 51.Olender A. Antibiotic resistance and detection of the most common mechanism of resistance (MLSB) of opportunistic Corynebacterium. Chemotherapy. 2013;59:294–306. doi: 10.1159/000357467. [DOI] [PubMed] [Google Scholar]
- 52.Balci I., Eksi F., Bayram A. Coryneform bacteria isolated from blood cultures and their antibiotic susceptibilities. J. Int. Med. Res. 2002;30:422–427. doi: 10.1177/147323000203000409. [DOI] [PubMed] [Google Scholar]
- 53.Philippon A., Bimet F. In vitro susceptibility of Corynebacterium group D2 and Corynebacterium jeikeium to twelve antibiotics. Eur. J. Clin. Microbiol. Infect. Dis. 1990;9:892–895. doi: 10.1007/BF01967505. [DOI] [PubMed] [Google Scholar]
- 54.Neemuchwala A., Soares D., Ravirajan V., Marchand-Austin A., Kus J.V., Patel S.N. In Vitro Antibiotic Susceptibility Pattern of Non-diphtheriae Corynebacterium Isolates in Ontario, Canada, from 2011 to 2016. Antimicrob. Agents Chemother. 2018;62 doi: 10.1128/AAC.01776-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Mondal J., Ghosh P., Zhu X. An Atomistic view of Short-chain Antimicrobial Biomimetic peptides in Action. bioRxiv. 2018:323592. doi: 10.1101/323592. [DOI] [Google Scholar]
- 56.Kumar P., Kizhakkedathu J.N., Straus S.K. Antimicrobial Peptides: Diversity, Mechanism of Action and Strategies to Improve the Activity and Biocompatibility In Vivo. Biomolecules. 2018;8:4. doi: 10.3390/biom8010004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Casciaro B., Loffredo M.R., Luca V., Verrusio W., Cacciafesta M., Mangoni M.L. Esculentin-1a Derived Antipseudomonal Peptides: Limited Induction of Resistance and Synergy with Aztreonam. Protein Pept. Lett. 2018;25:1155–1162. doi: 10.2174/0929866525666181101104649. [DOI] [PubMed] [Google Scholar]
- 58.Huang H.W. DAPTOMYCIN, its membrane-active mechanism vs. that of other antimicrobial peptides. Biochim. Biophys. Acta Biomembr. 2020;1862:183395. doi: 10.1016/j.bbamem.2020.183395. [DOI] [PubMed] [Google Scholar]
- 59.Raheem N., Straus S.K. Mechanisms of Action for Antimicrobial Peptides With Antibacterial and Antibiofilm Functions. Front. Microbiol. 2019;10:2866. doi: 10.3389/fmicb.2019.02866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Bechinger B., Gorr S.U. Antimicrobial Peptides: Mechanisms of Action and Resistance. J. Dent. Res. 2017;96:254–260. doi: 10.1177/0022034516679973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Colombo I., Sangiovanni E., Maggio R., Mattozzi C., Zava S., Corbett Y., Fumagalli M., Carlino C., Corsetto P.A., Scaccabarozzi D., et al. HaCaT Cells as a Reliable In Vitro Differentiation Model to Dissect the Inflammatory/Repair Response of Human Keratinocytes. Mediat. Inflamm. 2017;2017:7435621. doi: 10.1155/2017/7435621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Petushkova N.A., Rusanov A.L., Pyatnitskiy M.A., Larina O.V., Zgoda V.G., Lisitsa A.V., Luzgina N.G. Proteomic characterization of HaCaT keratinocytes provides new insights into changes associated with SDS exposure. Biomed. Dermatol. 2020;4:4. doi: 10.1186/s41702-019-0054-y. [DOI] [Google Scholar]
- 63.Kumar V. Macrophages: The Potent Immunoregulatory Innate Immune Cells. In: Bhat K.H., editor. Macrophage Activation-Biology and Disease. IntechOpen; London, UK: 2020. [DOI] [Google Scholar]
- 64.Hawdon N.A., Aval P.S., Barnes R.J., Gravelle S.K., Rosengren J., Khan S., Ciofu O., Johansen H.K., Høiby N., Ulanova M. Cellular responses of A549 alveolar epithelial cells to serially collected Pseudomonas aeruginosa from cystic fibrosis patients at different stages of pulmonary infection. FEMS Immunol. Med. Microbiol. 2010;59:207–220. doi: 10.1111/j.1574-695X.2010.00693.x. [DOI] [PubMed] [Google Scholar]
- 65.Foster K.A., Oster C.G., Mayer M.M., Avery M.L., Audus K.L. Characterization of the A549 cell line as a type II pulmonary epithelial cell model for drug metabolism. Exp. Cell Res. 1998;243:359–366. doi: 10.1006/excr.1998.4172. [DOI] [PubMed] [Google Scholar]
- 66.Barzantny H., Schroder J., Strotmeier J., Fredrich E., Brune I., Tauch A. The transcriptional regulatory network of Corynebacterium jeikeium K411 and its interaction with metabolic routes contributing to human body odor formation. J. Biotechnol. 2012;159:235–248. doi: 10.1016/j.jbiotec.2012.01.021. [DOI] [PubMed] [Google Scholar]
- 67.Kursun S., Acar B., Atakan C., Oztas B., Paksoy C.S. Relationship between genuine and pseudohalitosis and social anxiety disorder. J. Oral Rehabil. 2014;41:822–828. doi: 10.1111/joor.12206. [DOI] [PubMed] [Google Scholar]
- 68.Mogilnicka I., Bogucki P., Ufnal M. Microbiota and Malodor-Etiology and Management. Int. J. Mol. Sci. 2020;21:2886. doi: 10.3390/ijms21082886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.AlgPred: Prediction of Allergenic Proteins and Mapping of IgE Epitopes. [(accessed on 17 July 2020)]; Available online: https://webs.iiitd.edu.in/raghava/algpred/submission.html.
- 70.Casciaro B., d’Angelo I., Zhang X., Loffredo M.R., Conte G., Cappiello F., Quaglia F., Di Y.P., Ungaro F., Mangoni M.L. Poly(lactide- co-glycolide) Nanoparticles for Prolonged Therapeutic Efficacy of Esculentin-1a-Derived Antimicrobial Peptides against Pseudomonas aeruginosa Lung Infection: in Vitro and in Vivo Studies. Biomacromolecules. 2019;20:1876–1888. doi: 10.1021/acs.biomac.8b01829. [DOI] [PubMed] [Google Scholar]
- 71.Cappiello F., Ranieri D., Carnicelli V., Casciaro B., Chen H.T., Ferrera L., Di Y.P., Mangoni M.L. Bronchial epithelium repair by Esculentin-1a-derived antimicrobial peptides: involvement of metalloproteinase-9 and interleukin-8, and evaluation of peptides’ immunogenicity. Sci. Rep. 2019;9:18988. doi: 10.1038/s41598-019-55426-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Rahnamaeian M., Vilcinskas A. Short antimicrobial peptides as cosmetic ingredients to deter dermatological pathogens. Appl. Microbiol. Biotechnol. 2015;99:8847–8855. doi: 10.1007/s00253-015-6926-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Haisma E.M., Goblyos A., Ravensbergen B., Adriaans A.E., Cordfunke R.A., Schrumpf J., Limpens R.W., Schimmel K.J., den Hartigh J., Hiemstra P.S., et al. Antimicrobial Peptide P60.4Ac-Containing Creams and Gel for Eradication of Methicillin-Resistant Staphylococcus aureus from Cultured Skin and Airway Epithelial Surfaces. Antimicrob. Agents Chemother. 2016;60:4063–4072. doi: 10.1128/AAC.03001-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Casciaro B., Calcaterra A., Cappiello F., Mori M., Loffredo M.R., Ghirga F., Mangoni M.L., Botta B., Quaglio D. Nigritanine as a New Potential Antimicrobial Alkaloid for the Treatment of Staphylococcus aureus-Induced Infections. Toxins (Basel) 2019;11:511. doi: 10.3390/toxins11090511. [DOI] [PMC free article] [PubMed] [Google Scholar]