The development of Ebola virus countermeasures is challenged by our limited understanding of cell entry, especially at the step of membrane fusion. The surface-exposed viral protein, GP, mediates membrane fusion and undergoes major structural rearrangements during this process. The stability of GP at elevated temperatures (thermostability) can provide insights into its capacity to undergo these rearrangements. Here, we describe a new assay that uses GP-specific antibodies to measure GP thermostability under a variety of conditions relevant to viral entry. We show that proteolytic cleavage and acid pH have significant effects on GP thermostability that shed light on their respective roles in viral entry. We also show that the assay can be used to study how small-molecule entry inhibitors affect GP stability. This work provides a simple and readily accessible assay to engineer stabilized GP variants for antiviral vaccines and to discover and improve drugs that act by modulating GP stability.
KEYWORDS: Ebola virus, filovirus, glycoproteins, Marburg virus, membrane fusion, thermostability, virus entry
ABSTRACT
Ebola virus (EBOV) entry into cells is mediated by its spike glycoprotein (GP). Following attachment and internalization, virions traffic to late endosomes where GP is cleaved by host cysteine proteases. Cleaved GP then binds its cellular receptor, Niemann-Pick C1. In response to an unknown cellular trigger, GP undergoes conformational rearrangements that drive fusion of viral and endosomal membranes. The temperature-dependent stability (thermostability) of the prefusion conformers of class I viral fusion glycoproteins, including those of filovirus GPs, has provided insights into their propensity to undergo fusion-related rearrangements. However, previously described assays have relied on soluble glycoprotein ectodomains. Here, we developed a simple enzyme-linked immunosorbent assay (ELISA)-based assay that uses the temperature-dependent loss of conformational epitopes to measure thermostability of GP embedded in viral membranes. The base and glycan cap subdomains of all filovirus GPs tested suffered a concerted loss of prefusion conformation at elevated temperatures but did so at different temperature ranges, indicating virus-specific differences in thermostability. Despite these differences, all of these GPs displayed reduced thermostability upon cleavage to GP conformers (GPCL). Surprisingly, acid pH enhanced, rather than decreased, GP thermostability, suggesting it could enhance viral survival in hostile endo/lysosomal compartments. Finally, we confirmed and extended previous findings that some small-molecule inhibitors of filovirus entry destabilize EBOV GP and uncovered evidence that the most potent inhibitors act through multiple mechanisms. We establish the epitope-loss ELISA as a useful tool for studies of filovirus entry, engineering of GP variants with enhanced stability for use in vaccine development, and discovery of new stability-modulating antivirals.
IMPORTANCE The development of Ebola virus countermeasures is challenged by our limited understanding of cell entry, especially at the step of membrane fusion. The surface-exposed viral protein, GP, mediates membrane fusion and undergoes major structural rearrangements during this process. The stability of GP at elevated temperatures (thermostability) can provide insights into its capacity to undergo these rearrangements. Here, we describe a new assay that uses GP-specific antibodies to measure GP thermostability under a variety of conditions relevant to viral entry. We show that proteolytic cleavage and acid pH have significant effects on GP thermostability that shed light on their respective roles in viral entry. We also show that the assay can be used to study how small-molecule entry inhibitors affect GP stability. This work provides a simple and readily accessible assay to engineer stabilized GP variants for antiviral vaccines and to discover and improve drugs that act by modulating GP stability.
INTRODUCTION
Ebola virus (EBOV) is an enveloped negative-strand RNA virus in the family Filoviridae. The virus is responsible for causing Ebola virus disease (EVD), a devastating clinical syndrome that is characterized by early nonspecific findings followed by severe gastrointestinal symptoms and hemorrhage complications (1–3). Multiple ebolaviruses, including Sudan virus (SUDV), are capable of causing human disease with significant mortality. However, EBOV has been responsible for the majority of recorded human outbreaks, including two recent large-scale outbreaks—the unprecedented 2013 to 2016 West African epidemic (4) and an ongoing outbreak in the Democratic Republic of the Congo (https://www.who.int/csr/don/12-september-2019-ebola-drc/en/). Although an EBOV vaccine was recently approved by the FDA (5), no FDA-approved therapeutics are currently available for any of the filoviruses (6).
EBOV entry into cells requires a complex sequence of events that are mediated by the sole surface-exposed viral glycoprotein (GP). The GP is composed of two subunits that are tethered by noncovalent interactions and an intersubunit disulfide bond. GP1, the membrane-distal subunit, contains the receptor-binding site (RBS), which is shielded by the glycan cap, and a variable and highly glycosylated mucin-like domain (Muc) (7–11). GP2, the transmembrane subunit, mediates membrane fusion and contains sequences characteristic of class I viral membrane fusion proteins, including an internal fusion loop, N- and C-terminal heptad repeats that form ɑ-helical coiled coils, and a flexible membrane-proximal extracellular region (7, 12, 13). Virions initially attach to host cells through both GP and viral membrane-mediated interactions with multiple cellular attachment factors (14, 15). After internalization via a macropinocytosis-like mechanism (16–18), virions traffic along the endocytic pathway to late endo/lysosomal compartments (19, 20). Here, they are cleaved by host proteases cathepsins B and L (CatB and CatL, respectively) in the β13-14 loop of GP1. This removes the GP1 glycan cap and Muc, exposing the RBS and producing a metastable, primed intermediate of GP, GPCL (21–23). GPCL is then able to bind to the host receptor, Niemann-Pick C1 (NPC1), a cholesterol transporter located in the endo/lysosomal membrane. Binding to NPC1 is necessary but not sufficient for viral entry (24, 25).
Despite the considerable body of research on EBOV entry, its precise mechanism, especially at the membrane fusion step, remains poorly understood. Following receptor binding, an unknown trigger causes a series of conformational rearrangements that bring the host endosomal and viral membranes together to form a fusion pore, enabling the release of the viral nucleocapsid into the cytoplasm. Although the intermediate conformations of GP during membrane fusion have not been experimentally visualized, GP2 rearrangements likely culminate in a postfusion 6-α-helix bundle similar to that observed for other class I viral membrane fusion proteins, indicating an analogous fusion mechanism (12, 13).
The thermostability of class I viral membrane fusion proteins has provided a valuable surrogate for their capacity to undergo entry-related conformational changes. For example, mutations in the influenza A virus and human immunodeficiency virus glycoproteins that alter their thermostability and viral infectivity also affect their propensity to undergo acid pH- or receptor-mediated conformational changes during membrane fusion (26–28). Similarly, the stability of the EBOV GP can impact viral infectivity. Specifically, a GP1 mutation, A82V, that emerged during the West African outbreak decreased GP thermostability and increased viral infectivity in cell culture (29, 30). In contrast, small-molecule inhibitors bind into a pocket at the base of GP and destabilize it (31–33), indicating that reductions in GP thermostability can have opposing effects on EBOV entry and infection. Further, we recently showed that a thermostabilizing GP mutation, R64A, abolishes infection and that compensatory second-site mutations reduce GP thermostability (34). Work to date thus indicates that both decreased and increased GP thermostability can influence EBOV entry.
Although informative, previous studies of EBOV GP thermostability have largely relied on either hydrophobic dye- (31–33) or membrane-binding assays (35) with recombinant glycoprotein ectodomains. In the former type of assay, region-specific conformational changes in GP cannot be readily assessed, whereas in the latter, the potential stabilizing effects of the GP transmembrane domain and the membrane environment are neglected. Here, we sought to bridge the gap between these approaches by developing a quantitative assay for heat-induced conformational changes in full-length GP displayed on the membranes of intact vesicular stomatitis virus (VSV) particles. Specifically, we used a panel of GP-specific conformation-sensitive monoclonal antibodies (MAbs) to detect heat-induced loss of the prefusion conformation of EBOV GP under different conditions and extended these observations to other filovirus glycoproteins. We show that the structural core of filovirus GP undergoes a concerted conformational rearrangement at a characteristic temperature range that is lowered by GP proteolytic cleavage and by some, but not all, mutations that modulate its proteolytic susceptibility. Counterintuitively, we find that GP thermostability is increased by acid pH. Finally, we confirm that some selective estrogen receptor modulators (SERMs) can destabilize EBOV GP, as shown previously with recombinant GP ectodomains, but find that their destabilizing effect on filovirus glycoproteins can be at least partially decoupled from their antiviral activity.
RESULTS
Development of an epitope-loss ELISA to study the stability of the EBOV GP.
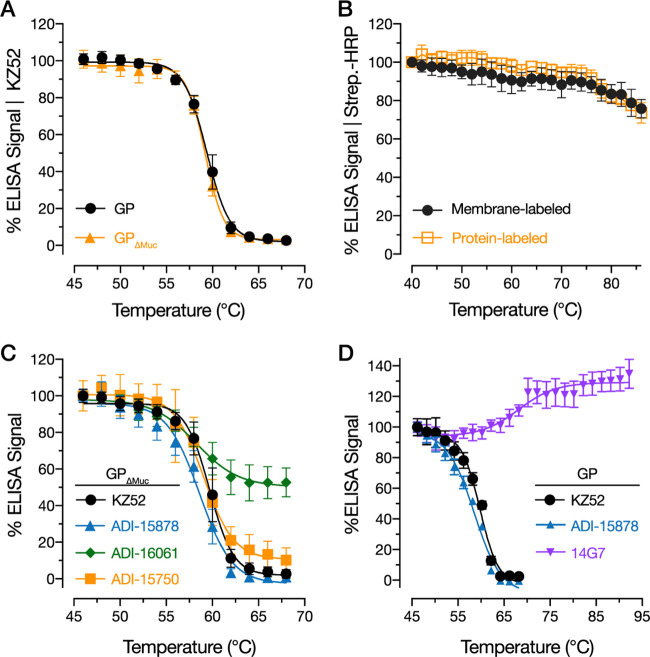
To interrogate the thermostability of native, full-length EBOV GP in biological membranes, we developed an assay that utilizes conformation-specific MAbs to detect the heat-induced loss of structure of a given epitope. Recombinant VSVs expressing EBOV GP (rVSV-GP) were heated at a range of temperatures, cooled to 4°C, and directly coated onto enzyme-linked immunosorbent assay (ELISA) plates. The binding capacities of selected conformation-specific MAbs were then determined by ELISA. We also tested the thermostability of a fully infectious mutant lacking the mucin-like domain (Muc), GPΔMuc (21, 36). We first used the well-characterized EBOV GP-specific MAb KZ52, which detects a conformational GP1 to GP2 intersubunit epitope in the prefusion GP trimer (that is maintained in GPΔMuc) (7, 37). The thermal denaturation curves obtained for GP and GPΔMuc showed a similar sigmoid shape; strong KZ52 binding was observed at low temperatures but decreased to background levels between 56 and 64°C (Fig. 1A). This profile is consistent with a two-state model in which the KZ52 epitope is either present or absent in GP, with an increasing probability of denaturing the epitope with increasing temperature. Similar half-maximal MAb binding temperatures (Tm ~ 59°C) were obtained for GP and GPΔMuc, suggesting that Muc does not contribute to the stability of the GP prefusion conformation. Therefore, we largely used viral particles bearing GPΔMuc in the following experiments.
FIG 1.
Thermal denaturation curves for prefusion epitopes in uncleaved EBOV GP. (A) rVSV-GP and rVSV-GPΔMuc were incubated at the indicated temperatures for 10 min, after which the samples were cooled to 4°C and KZ52 binding was assessed by ELISA. Averages ± standard deviations (SD) are shown; n = 9 from 3 independent experiments. Average absorbance range at 450 nm (A450) at lowest temperature tested (46 °C), 2.0 to 2.3. (B) Membrane- and protein-labeled rVSV-GPΔMuc preparations were incubated at the indicated temperatures, and biotin-labeled particles were detected with streptavidin-HRP by ELISA. Averages ± SD are shown; n = 6 from 2 independent experiments. (C) Effect of virus preincubation at the indicated temperatures on binding by MAbs ADI-15878, ADI-16061, ADI-15750, and KZ52. Averages ± SD are shown; n = 15 from 4 independent experiments (except ADI-15878, where n = 12 from 4 independent experiments). Average A450 at lowest temperature tested (46 °C),1.6 to 2.2. (D) Effect of virus preincubation at the indicated temperatures on binding by Muc-specific MAb 14G7. Binding curves for KZ52 and ADI-15878 binding are shown for comparison. Averages ± SD are shown; n = 9 from three independent experiments. Average A450 at lowest temperature tested (46 °C), 0.75 to 1.2.
To rule out the trivial possibility that the loss of KZ52 binding was due to decreased virion capture onto ELISA plates or shedding of GP from viral particles at elevated temperatures, protein- or membrane-biotinylated preparations of VSV-GPΔMuc were also subjected to the same protocol, and the virion-associated biotin signal was measured by ELISA. Both GP and viral particles were detected at all temperatures tested, including temperatures far exceeding those used in the epitope-loss ELISA (Fig. 1B). Importantly, only minimal reductions in biotin signal were observed at temperatures over which KZ52 binding titrated (56 to 64°C), with significant decreases only occurring at temperatures >72°C (Fig. 1B). These experiments indicate that the irreversible loss of KZ52 binding to GP at elevated temperatures is a consequence of the thermal denaturation of the KZ52 epitope and not the loss of viral particles or GP.
The GP base and glycan cap subdomains undergo a concerted loss of prefusion conformation at elevated temperatures.
To investigate if the loss of the KZ52 epitope at elevated temperatures was specific to this epitope or instead reflected larger-scale changes in the prefusion conformation of GP, we tested additional conformation-sensitive MAbs whose epitopes are distinct from that of KZ52: ADI-15750, ADI-15878, and ADI-16061 (38). ADI-15750 recognizes the glycan cap subdomain in GP, ADI-15878 binds a distinct interprotomer epitope in the GP base spanning GP1 and the GP2 fusion loop, and ADI-16061 recognizes a GP2 epitope in the stalk of the GP trimer (38). The thermal denaturation curves for the ADI-15750 and ADI-15878 epitopes were superimposable with that of KZ52, with Tm values of ∼59°C (Fig. 1C). In contrast, the ADI-16061 epitope was largely resistant to elevated temperatures, possibly because this epitope in the GP2 HR2 domain is stabilized by its proximity to the GP membrane anchor. Alternatively, it is possible that the ADI-16061 epitope partially renatures during the cooling step or subsequent steps in the ELISA (Fig. 1C). The increased thermostability of the ADI-16061 stalk epitope was not explained by its increased binding to GP; ADI-16061 (and the other MAbs tested) were found to have similar relative binding to unheated GP (data not shown). In contrast to the GP base and glycan cap subdomains probed above, Muc was shown to be largely disordered, with several Muc-specific MAbs recognizing linear epitopes (10, 11, 39–41). To investigate the thermostability of Muc, we used MAb 14G7, which recognizes a linear Muc epitope (39). Over the temperature range at which the base and glycan cap epitopes were lost, we observed no appreciable reduction in the 14G7 epitope (Fig. 1D). Instead, 14G7 recognition was enhanced at very high temperatures (Fig. 1D), possibly due to the increased exposure of its linear epitope (39). Taken together, these experiments demonstrate that the highly structured regions of the GP trimer, including the base and glycan cap subdomains, suffer a concerted, irreversible loss of their prefusion conformation at elevated temperatures.
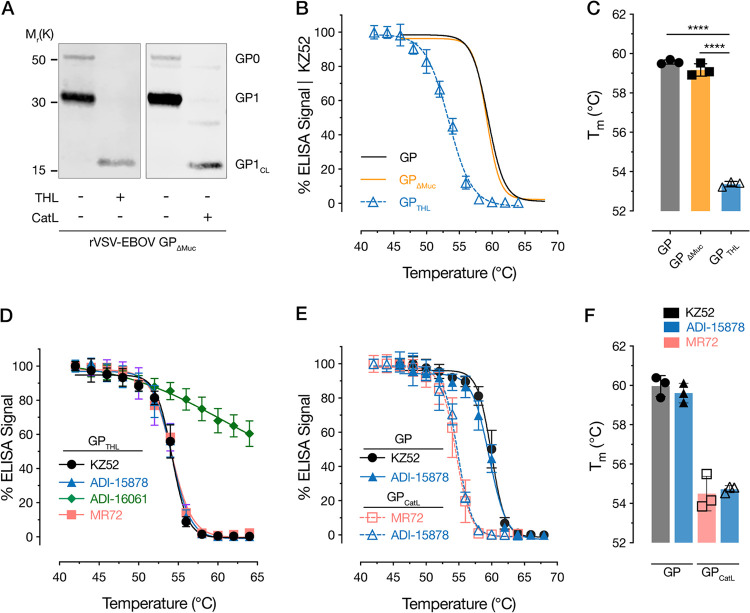
EBOV GP is destabilized by proteolytic cleavage.
Proteolytic cleavage of GP by endosomal cysteine cathepsins CatB and CatL exposes the binding site for its critical endo/lysosomal receptor, NPC1, and primes it to undergo subsequent entry-related conformational changes (35, 42, 43). Previous work also suggests that cleaved GP conformers (GPCL) generated in vitro are more conformationally labile than their uncleaved counterparts (35, 43). To investigate the consequences of proteolytic processing on GP thermostability, rVSV-GP was incubated with thermolysin (THL) as described previously and tested in the epitope-loss ELISA (22, 43). THL is proposed to mimic the cleavage of GP by CatB during viral entry (22). GP cleavage was verified by Western blot analysis (Fig. 2A). Although the thermal denaturation curve for THL-cleaved GPCL (GPTHL) resembled those of GP and GPΔMuc in sigmoidal shape, it was left shifted by ∼6°C relative to the latter, indicating decreased stability (Fig. 2B and C). We obtained similar findings with the GP base epitope of MAb ADI-15878 and the RBS epitope of MR72 (8, 44). ADI-16061’s GP stalk epitope was even more resistant to denaturation in GPTHL than in its uncleaved counterpart (Fig. 2D). As with GP, differences in MAb binding to unheated GPTHL did not correlate with the thermostability of a given epitope and could not explain the stability of the ADI-16061 stalk epitope (data not shown).
FIG 2.
Proteolytic cleavage with thermolysin (THL) and cathepsin L (CatL) destabilizes EBOV GP. (A) THL and CatL cleavage of rVSV-GPΔMuc was verified by Western blotting with anti-GP1 N-terminal peptide polyclonal rabbit sera. (B and C) Thermal denaturation curves (B) and calculated melting temperature values (Tm) (C) obtained with KZ52 for rVSVs bearing GPTHL compared to uncleaved GP and GPΔMuc. Averages ± SD are shown; n = 9 from 3 independent experiments. Average A450 at lowest temperature tested (42°C), 1.9. Data for GP and GPΔMuc are from Fig. 1 and are shown for comparison. (D) Thermal denaturation curves for rVSV-GPTHL obtained with MAbs KZ52, ADI-15878, ADI-16061, and MR72. Averages ± SD are shown; n = 15 from 5 independent experiments except for MR72 and ADI-15878 (n = 12 from 4 independent experiments). Average A450 range at lowest temperature tested (42°C), 1.9 to 2.3. (E and F) Thermal denaturation curves (E) and Tm values (F) for GP and GPCatL as assessed with KZ52 and ADI-15878 (GP) and MR72 and ADI-15878 (GPCatL). Averages ± SD are shown; n = 9 from three independent experiments. Average A450 range at lowest temperature tested (42°C), 2.0 to 2.2.
We next asked if cleavage with the more entry-relevant endosomal cysteine protease CatL also destabilizes GP. Accordingly, we treated rVSV-GP with recombinant human CatL and verified the generation of CatL-cleaved GPCL (GPCatL) by Western blot analysis (Fig. 2A). Because KZ52 does not bind GPCatL (44), we used ADI-15878 and MR72 to assess its thermostability (44). As expected, CatL cleavage also destabilized GP and did so to a similar extent as THL, with a Tm of ∼55°C for both ADI-15878 and MR72 (Fig. 2E and F). Together, these experiments indicate that the proteolytic removal of the glycan cap and cleavage in the β13-14 loop of GP1 associated with GP→GPCL cleavage destabilize the prefusion conformation of GP, affording one mechanism by which GP is primed for membrane fusion-related conformational changes during entry.
The GP proteins of other ebolaviruses are also destabilized by proteolytic cleavage.
Because GP→GPCL cleavage is a prerequisite for cell entry by all filoviruses that have been evaluated to date (21, 23, 45), we postulated that this cleavage also destabilizes GPs from divergent ebolaviruses. Accordingly, we used the pan-ebolavirus base-binding MAb ADI-15878 to probe the thermal stability of GPs from the divergent ebolaviruses Sudan virus (SUDV) and the recently discovered Bombali virus (BOMV) in the epitope-loss ELISA (46–49). THL cleavage of SUDV GP and BOMV GP was verified by Western blot analysis (Fig. 3A). As described for other ebolaviruses, BOMV GP1 was cleaved by THL to an ∼17,000 Da (17 kDa) product, which is consistent with its capacity to recognize NPC1 through exposure of its RBS (49). Like EBOV GPTHL, SUDV and BOMV GPTHL displayed reduced thermostability relative to their uncleaved counterparts, indicating that GP cleavage plays a similar role for several (and likely all) ebolaviruses in destabilizing the prefusion conformation of GP (Fig. 3B and C). Although SUDV GP resembled EBOV GP in thermostability in both its uncleaved and cleaved forms, BOMV GP was much less stable. Indeed, uncleaved BOMV GP had a similar Tm to that of EBOV GPCL (Fig. 3B and C). These findings reveal differences in the intrinsic stability of the GP prefusion conformation among ebolaviruses, with potential implications for their cell entry and infection mechanisms.
FIG 3.
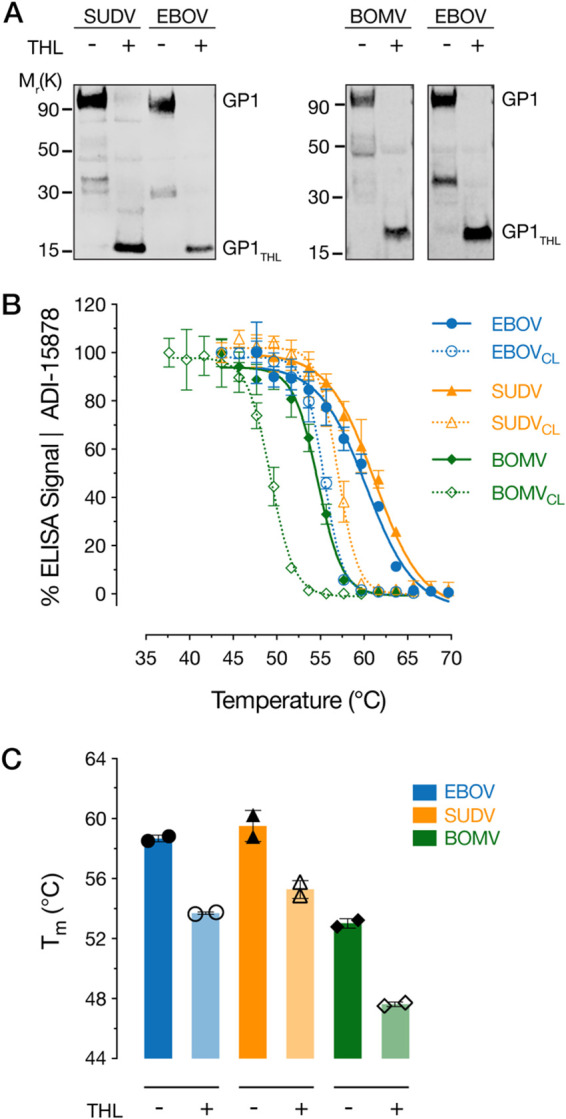
Thermostability of GPs from other ebolaviruses. (A) THL cleavage conditions for rVSV-SUDV GP and rVSV-BOMV GP were verified by Western blotting with anti-GP1 N-terminal peptide polyclonal rabbit sera. (B) Thermal denaturation curves for rVSVs bearing GP and GPTHL from EBOV, SUDV, and BOMV were determined with ADI-15878. Averages ± SD are shown; n = 6 from 2 independent experiments. Average A450 range at lowest temperature tested, 0.8 to 1.1 for GP and 1.3 to 2.0 for GPCL. (C) Calculated Tm values from the thermal denaturation curves in panel B. Averages ± SD are shown; n = 2 from 2 independent experiments.
A subset of CatB-independent EBOV GP mutants exhibits decreased thermostability.
In a previous study, we selected and characterized EBOV GP mutants bearing single-point mutations that afforded CatB-independent virus entry (43). Because two of these mutations (I584F and K588R) were located at the GP1-GP2 intersubunit interface, we proposed that they destabilize the GP prefusion conformation in a manner that enables virions to bypass the CatB cleavage requirement. To more rigorously evaluate this hypothesis, we assessed the thermostability of the GPΔMuc and GPTHL forms of the CatB-independent N40K, D47V, I584F, and K588R mutants in the epitope-loss ELISA (Fig. 4). We observed little or no left shift in the thermal denaturation curves for GPN40K and GPD47V, indicating that these mutations do not confer CatB independence by destabilizing GP (Fig. 4A and D). In contrast, the thermal denaturation curves of both GPI584F and GPK588R and their GPTHL intermediates were left shifted relative to those of GP wild type (GPWT). Unexpectedly, K588R rendered GP considerably more unstable than did I584F, despite the fact that the latter was much more sensitive than the former to proteolytic degradation (Fig. 4B to D) (43). These results lend further support to the hypothesis that the key function of GP cleavage by CatB is to destabilize GP’s prefusion conformation (34, 35, 43). They also indicate, however, that some GP mutants bypass the CatB cleavage requirement by mechanisms other than GP destabilization that remain to be identified (34).
FIG 4.
Thermostability of EBOV GP mutants with altered proteolytic requirements for viral entry. Thermal denaturation curves for GP and GPTHL for CatB-independent GP mutants N40K and D47V (A), I584F (B), and K588R (C) relative to WT. Averages ± SD are shown; n = 6 from 2 independent experiments. WT EBOV curves (blue) from panel A are shown for comparison in panels B and C. (D) Average Tm values from two independent experiments. (E) Summary of the thermostability (panels A to D) and protease sensitivity phenotypes (from [43]) for the indicated GP mutants.
Endosomal acid pH stabilizes GP’s prefusion conformation.
Endosomal acid pH is critical for filovirus entry and appears to play multiple roles in this process; previous work implicates it in the activity of the cysteine cathepsins that proteolytically cleave GP (21, 22, 50, 51) for optimal GP-NPC1 binding (52), to induce rearrangement of the GP2 fusion loop to a membrane-active form (53), and to stabilize the GP2 postfusion 6-α-helix bundle structure (50, 54). In addition, acid pH has been proposed to act as a trigger for viral membrane fusion (35, 53). We reasoned that if acid pH was indeed directly involved in GP fusion triggering, it may be expected to reduce the thermostability of GP’s prefusion conformation. Unexpectedly, we observed significant enhancements in the thermostability of both GP and GPCL at pH values below 6.5, with Tm value increases of ∼4°C at pH values of 5.5 to 6.0 relative to those at pH 8.0 (Fig. 5). These findings suggest that acid pH alone is unlikely to play a direct role in triggering GPCL for viral membrane fusion prior to receptor binding. Instead, they raise the possibility that the acid-dependent stabilization of GP and GPCL is an adaptive response to endo/lysosomal conditions during entry.
FIG 5.
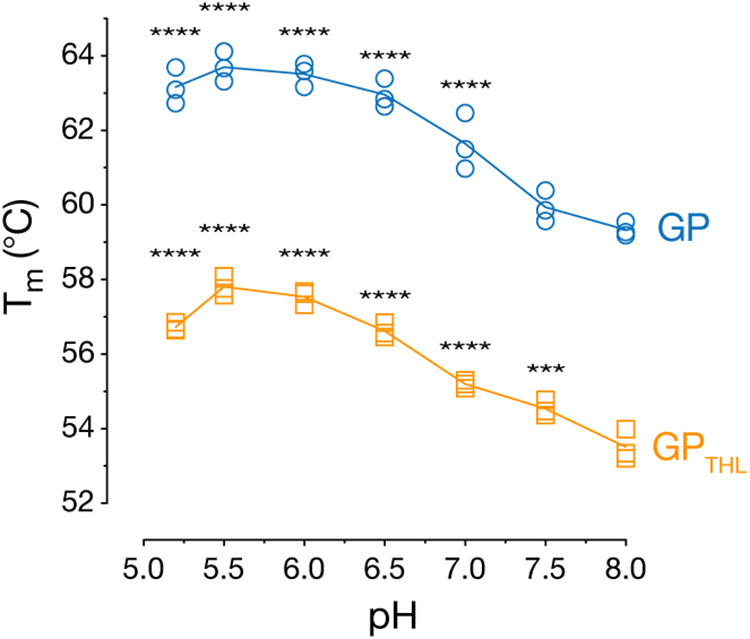
Effect of pH on the thermostability of EBOV GP. rVSVs bearing GP and GPTHL were incubated in at the indicated pH values for 1 h at room temperature and then shifted to the indicated temperatures. Virions were then captured onto ELISA plates, and GP was detected at neutral pH using MAb KZ52. The Tm values computed from three independent thermal denaturation curves at each pH (n = 9) are shown. One-way analysis of variance (ANOVA) with Dunnett’s post hoc correction for multiple comparisons was used to analyze the Tm relative to pH 8 (***, P < 0.001; ****, P > 0.0001).
Small-molecule inhibitor toremifene decreases GP thermostability at acid pH.
The SERM toremifene has been proposed to inhibit EBOV infection by destabilizing GP (31). To evaluate the potential destabilizing effect of toremifene in the epitope-loss ELISA, we preincubated rVSV-EBOV GP with toremifene and heated viral particles in the presence of the inhibitor at different pH values. As above (Fig. 5), the Tm was observed to increase with decreasing pH for both GP and GPCL, with a maximal increase of 4°C at pH 5.7 (Fig. 6A). Although toremifene had no effect on GP thermostability at mildly alkaline pH (7.5 to 8.0), it decreased GP thermostability relative to the vehicle control at acidic pH values, with a maximal decrease of about 4°C at pH 5.2 (Fig. 6A). In contrast, toremifene had a smaller effect on the thermostability of GPTHL (Fig. 6A). We next tested the dose dependence of toremifene’s capacity to destabilize GP at pH values of 7.5 and 5.2. Drug concentrations greater than 3.3 μM were necessary for toremifene-mediated GP destabilization, with significantly greater effects seen at acid pH, as described above (maximal ΔTm of ∼9°C at pH 5.2 versus ∼2°C at pH 7.5) (Fig. 6B). These findings are in line with those reported by Zhao and coworkers using a recombinant GP ectodomain in a completely different (fluorescence-based) thermostability assay (31). Together, these results confirm that toremifene destabilizes EBOV GP in an acid pH- and dose-dependent manner.
FIG 6.
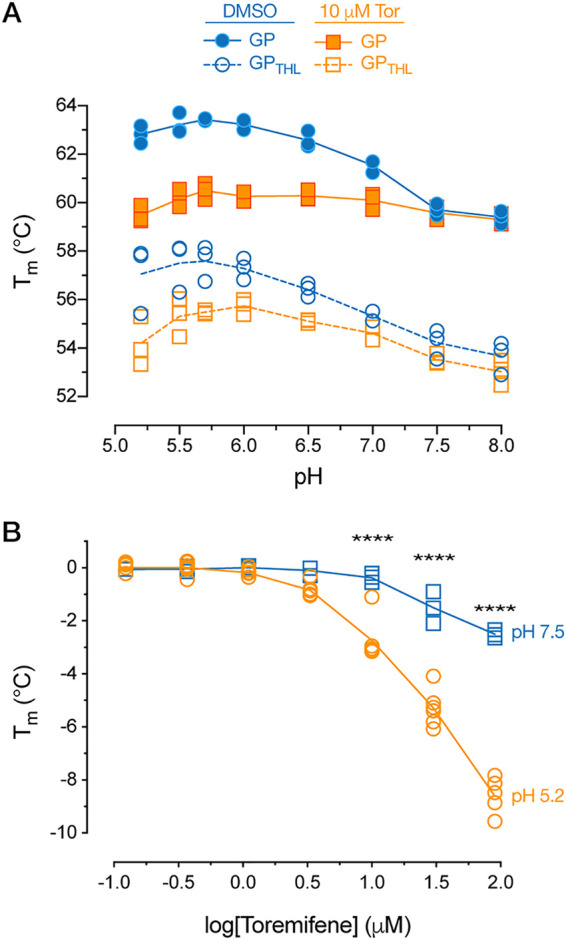
Effect of toremifene on EBOV GP thermostability. (A) rVSV-EBOV GP particles were diluted in PBS adjusted to the indicated pH values containing toremifene (10 μM) or 0.1% DMSO, incubated for 1 h at room temperature, and then incubated at the indicated temperatures. Virions were then captured onto ELISA plates, and GP was detected at neutral pH using MAb KZ52. The Tm values computed from three independent thermal denaturation curves at each pH (n = 9) are shown. (B) Effect of toremifene concentration on GP thermostability at pH 5.2 versus pH 7.5 determined as described in panel A. The Tm values computed from five independent thermal denaturation curves for pH 5.2 (n = 15) and three independent curves for pH 7.5 (n = 9) are shown. pH 7.5 versus pH 5.2: ****, P < 0.0001 by two-way ANOVA with Sidak's post hoc correction for multiple comparisons.
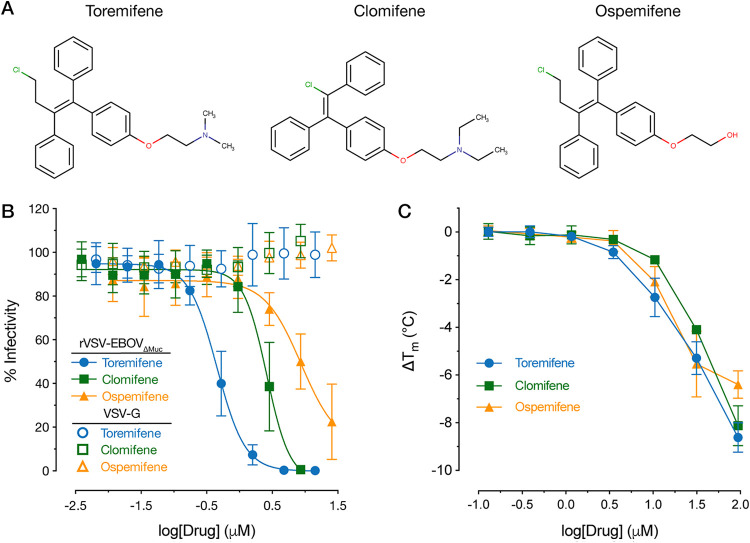
SERM-mediated GP destabilization and inhibition of EBOV infection are not fully correlated.
Among the SERMs known to inhibit EBOV entry, only toremifene has been tested for its effect on GP stability (31–33, 55). Here, we tested two additional SERMs and structural analogs of toremifene, clomifene, and ospemifene. Entry by VSV-GPΔMuc was strongly inhibited by toremifene with a 50% inhibitory concentration (IC50) of ∼450 nM (Fig. 7B), as previously reported (56). Clomifene and ospemifene were much less potent, with IC50s of 2.6 μM and 8.7 μM, respectively (Fig. 7B). Indeed, complete entry inhibition was not observed with ospemifene, even at the highest noncytotoxic doses tested. VSV G-dependent infection, as a control, was not affected by any of the drugs, indicating specific inhibition of EBOV GP-mediated entry. Despite their reduced potency as entry inhibitors, clomifene and ospemifene closely resembled toremifene in their capacity to destabilize GP in the epitope-loss ELISA (Fig. 7C). To further investigate the discrepancy between entry inhibition and GP destabilization with these molecules, we assessed whether the decreased destabilization of GPTHL by toremifene correlated with decreased inhibition of rVSV-GPTHL. There was no significant difference in toremifene inhibition of precleaved or cleaved rVSV-GP-mediated entry (data not shown). The disconnect between the inhibition of GP-dependent viral entry and the destabilization of GP strongly suggests that mechanisms other than GP destabilization account for the potent antiviral activity of toremifene.
FIG 7.
Effect of toremifene structural analogs on EBOV GP-dependent entry and thermostability. (A) Chemical structures for toremifene and two SERMs that are structural analogs, clomifene and ospemifene. (B) SERM-mediated inhibition of rVSV-EBOV GP entry in Vero cells. Averages ± SD are shown; n = 9 from 3 independent experiments. (C) Effect of clomifene and ospemifene on the thermostability of EBOV GP was determined with KZ52 as described above. Data for the effect of toremifene on thermostability of EBOV GP are from Fig. 6 and are shown for comparison. Tm values computed from three independent thermal denaturation curves at each pH (n = 9) are shown.
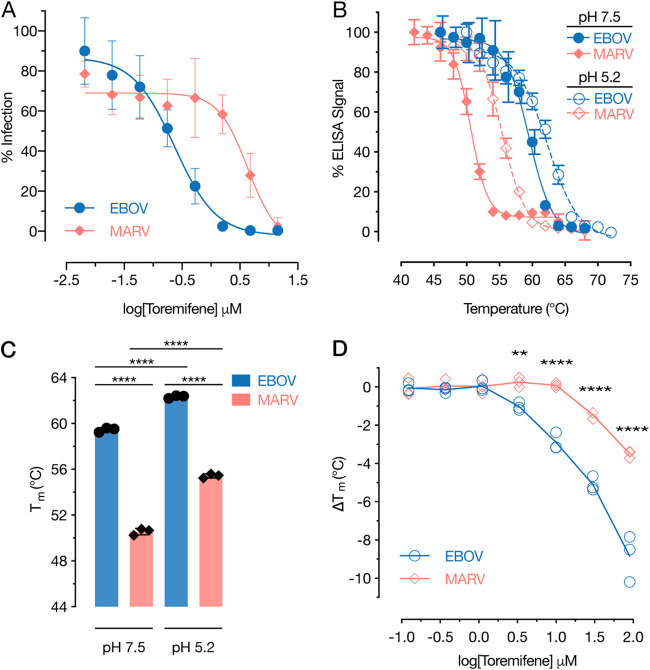
MARV GP is less susceptible to toremifene-mediated destabilization and viral entry inhibition.
Previous work indicates that Marburg virus (MARV) entry is inhibited by toremifene, but to a lesser degree than is EBOV (56, 57). We were able to confirm these findings (Fig. 8A). Whether toremifene also affects MARV GP stability has not been reported, however. Accordingly, we used MR191, a human MAb specific for the NPC1-binding site in MARV GP (58), to adapt the epitope-loss ELISA to rVSV-MARV GP. MARV GP was significantly less thermostable than EBOV GP (Fig. 8B and C). Further, acid pH increased the Tm of MARV GP to an extent similar to that of EBOV GP, suggesting that these divergent glycoproteins share at least some molecular determinants of acid-dependent stability (Fig. 8A and B). We next examined the thermostability of MARV GP in the presence of toremifene. Concordant with rVSV-MARV GP’s reduced susceptibility to toremifene (Fig. 8A), MARV GP was also less sensitive than EBOV GP to toremifene’s destabilizing effects (Fig. 8D). Our findings strongly suggest that toremifene can bind to and destabilize MARV GP despite substantial differences between MARV and EBOV GPs in the configuration of the toremifene-binding pocket (Fig. 9).
FIG 8.
Thermostability of MARV GP and its susceptibility to toremifene. (A) The effect of toremifene on rVSV-MARV GP in Vero cells was determined as described in Fig. 7B. Averages ± SD are shown; n = 9 from 3 independent experiments. (B) Thermal denaturation curves for rVSVs MARV and EBOV GP were determined at pH 7.5 and pH 5.2 with MR191 (MARV) and KZ52 (EBOV), respectively. Averages ± SD are shown; n = 9 from 3 independent experiments. Average A450 range at lowest temperature tested, 0.7 to 1.3. (C) Calculated Tm values from the thermal denaturation curves in panel B. Averages ± SD are shown; n = 3 from 3 independent experiments. ****, P < 0.0001 by one-way ANOVA with Tukey’s post hoc correction for multiple comparisons. (D) Effect of toremifene on the thermostability of MARV and EBOV GP at pH 5.2 was determined as described above. The Tm values computed from three independent thermal denaturation curves at each pH (n = 9) are shown. EBOV versus MARV: **, P < 0.01; ****, P < 0.0001 by two-way ANOVA with Sidak’s post hoc correction for multiple comparisons.
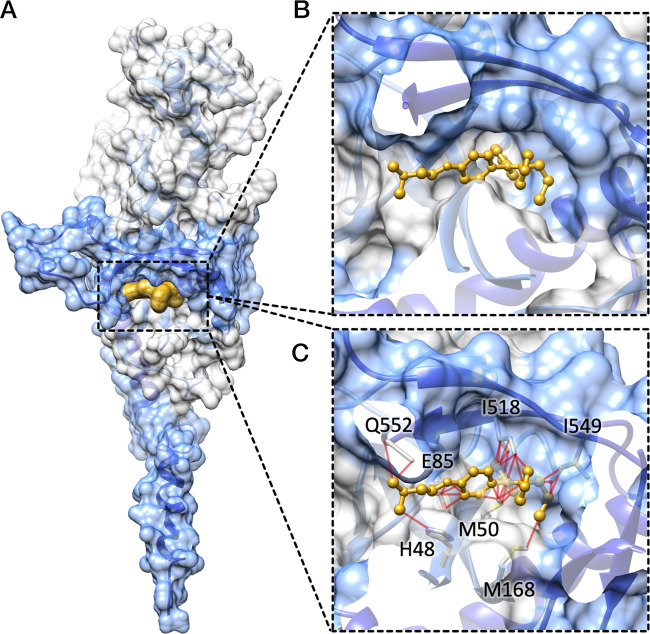
FIG 9.
Docking by structural superposition reveals steric clashes between toremifene and MARV GP in the binding pocket. (A) Overview of the EBOV GP monomer bound to toremifene (GP1, light gray surface;GP2, blue surface; toremifene, yellow surface; PDB ID 5JQ3) (31). (B) Closeup view of toremifene (yellow ball and sticks) bound to EBOV GP (GP1, light-gray surface; GP2, blue surface); no steric clashes were observed between the protein and the ligand. (C) MARV GP monomer (GP1, light-gray surface; GP2, blue surface; PDB ID 5UQY) (70) was structurally superimposed to the EBOV GP-toremifene complex (only toremifene is shown as yellow ball and sticks) using Chimera (71). Structural clashes (red edges) between atoms in MARV GP (depicted as sticks) and toremifene were identified using Chimera and default parameters.
DISCUSSION
The thermostability of viral glycoproteins can reflect their fusogenicity (26–28). To extend previous studies of filovirus GP thermostability, which rely on purified, recombinant GP ectodomains, we developed and characterized a simple, readily accessible antibody-based assay that measures the stability of full-length GP trimers embedded in viral membranes (Fig. 1 and 2). Our findings were both qualitatively and quantitatively concordant with the results of previously published GP thermostability assays (31, 35). One advantage of the approach we have developed is that it allows us to probe the thermostability of specific sequences in GP; in contrast, the fluorescence-based thermal shift assays typically employed for this purpose do not provide such region-specific information. Herein, we found that the highly structured subdomains of the GP trimer—the base and glycan cap—both undergo a concerted loss of conformation at a characteristic temperature range (Fig. 1C), whereas the GP stalk, comprising sequences in the GP2 HR1 and HR2 heptad repeat-forming sequences, is relatively refractory to thermal denaturation (Fig. 1C). The availability of epitopes in the Muc domain actually increased at elevated temperatures, consistent with previous work suggesting it is intrinsically disordered (Fig. 1D).
Another advantage of our approach is its capacity to interrogate the thermostability of divergent GPs through the use of engineered rVSVs and conformation-sensitive MAbs with pan-ebolavirus and pan-filovirus reactivity. Here, we showed that the GPs of the newly discovered ebolavirus BOMV and MARV are much less stable than those of EBOV and SUDV (Fig. 3B and C and Fig. 8B and C), suggesting differences in their entry mechanisms that remain to be defined. We speculate that variations in GP thermostability among filoviruses (with attendant consequences for route/efficiency of cell entry and environmental stability) may impact their capacity to infect different types of hosts and spread between them in nature.
Using this thermostability assay, we investigated the effect of GP proteolytic priming—an essential step in filovirus entry—on EBOV GP stability. Our results, together with previous findings (35, 43), indicate that removal of the glycan cap and cleavage within the partially disordered β13-14 loop connecting the base and glycan cap sharply reduce thermostability (Fig. 2), whereas the removal of Muc has little effect (Fig. 1A). Interestingly, differences in the C terminus of the cleaved GP1 subunit generated by THL and CatL did not significantly impact GPCL thermostability (Fig. 2B to E). Because the additional processing of GP1CatL at its C terminus by CatB (mimicked by THL) is required for entry (22, 43), we infer that the role of the latter cleavage step is likely not to destabilize GP per se but to prime GP for the action of another, unidentified entry host factor (34).
To further investigate the importance of GP destabilization by proteolytic cleavage during entry, we analyzed the thermostability of our previously described CatB-independent GP mutants (Fig. 4) (43). Combined with their known protease-sensitivity phenotypes (43), our analysis of thermostability suggests three distinct mechanisms of CatB independence (summarized in Fig. 4E). Only one of the mutants, GP(K588R), which is slightly more susceptible to proteolysis, exhibited a strong reduction in thermostability that may afford bypass of the requirement for cleavage-mediated destabilization (Fig. 4C). More protease-sensitive mutants, including GP(I584F) and, to a lesser extent, GP(N40K), possessed WT thermostability (Fig. 1A and B). We postulate that these mutations confer CatB independence by accelerating cleavage by other endosomal cysteine cathepsins, such as CatL. The mechanism by which D47V, which alters neither thermostability (Fig. 1A) nor protease sensitivity (43), affords CatB independence is presumably distinct from the above. Thus, although thermostability can correlate with CatB independence, increased protease sensitivity and decreased thermostability at least partly reflect distinct molecular mechanisms by which GP proteins can bypass the CatB cleavage requirement during entry.
These apparently complex relationships among the molecular bases of GP thermostability, protease sensitivity, and CatB dependence also extend to other filoviruses. As reported previously, many filovirus GPs, including those of SUDV and MARV, are CatB independent (23, 45). Although filovirus GPs are indeed polymorphic at some of the amino acid sequence positions altered in the CatB-independent EBOV GP mutants, the mutation of SUDV or Reston virus (RESTV) GP to the cognate EBOV GP residues at these positions did not render them CatB dependent (23), suggesting the existence of other unknown molecular determinants. Similarly, we observed that the CatB independence of SUDV GP could not be explained by its thermostability (Fig. 3B and C) since it resembled EBOV GP in this regard. We did find, however, that MARV GP, which is CatB independent, is much less thermostable than EBOV GP (Fig. 8B and C), raising the possibility that both of its phenotypes share a molecular basis similar to that of EBOV GP(K588R). More work is needed to test this hypothesis and to determine if BOMV GP, which is much less stable than EBOV GP (Fig. 3B and C), is also CatB independent.
Given the many roles endosomal acid pH is proposed to play in filovirus entry, we measured the pH dependence of GP thermostability and found, counterintuitively, that acid pH stabilizes both uncleaved and cleaved GP. This effect appears to be broadly shared among filoviruses, including the divergent EBOV and MARV GPs (Fig. 5 and Fig. 8B and C). Further, the common behavior of GP and GPCL indicates that the sequences that modulate the pH dependence of GP thermostability reside within its base or stalk subdomains and not the glycan cap or Muc. Our findings complicate previous hypotheses proposing that acid pH serves as part of the molecular trigger for viral membrane fusion (35, 54, 59); if this were the case, one might expect GP stability to be reduced at acidic pH values, as reported for other acid-triggered class I viral membrane fusion proteins (26). However, these experiments do not exclude acid pH playing a role in triggering fusion following receptor binding, which has been shown for other viral glycoproteins (60, 61). Indeed, acid pH was recently shown to promote increased GP-induced lipid mixing, but only with soluble NPC1 domain C-coated liposomes. Additionally, inclusion of Ca2+ further increased lipid mixing, reinforcing the notion that receptor binding and additional factors may influence the role of acid pH in triggering fusion (59). We speculate that the acid pH-mediated stabilization of GP prior to receptor binding plays a functional role in filovirus entry. It may, for instance, help to explain the increased affinity of GP for NPC1 at acid pH (52). Alternatively or in addition, it may prevent premature GP2 fusion loop deployment until viral delivery to late endo/lysosomal compartments, where NPC1 binding and/or additional GP cleavage events can drive fusogenic conformational changes (34). Finally, these observations may also explain the behavior of toremifene and some other EBOV entry inhibitors, which selectively destabilize GP at acid pH (Fig. 6 and Fig. 7D) (31, 33). We propose that toremifene exerts its antiviral effect, in part, by counteracting the acid-dependent stabilization of GPCL and promoting premature GPCL triggering in endosomal compartments.
Although toremifene can potently block EBOV entry, it only modestly inhibits MARV entry (Fig. 8A) (56, 57). Using our epitope-loss ELISA, we found that toremifene is a less potent destabilizer of MARV GP than EBOV GP at acid pH (Fig. 8D), concordant with its reduced antiviral activity. A structural alignment of the toremifene-bound EBOV GP and apo MARV GP X-ray crystal structures (Fig. 9) suggests that the geometry of the putative toremifene-binding pocket in MARV GP is not compatible with the EBOV-binding configuration of toremifene, potentially resulting in an alternative binding mode of the drug and a reduction in binding affinity (Fig. 9B). Hence, toremifene analogs specifically engineered to fit into the unique pocket in MARV GP may afford enhanced antiviral activity.
Finally, we used viral infectivity assays and the epitope-loss ELISA to more closely examine the relationship between the antiviral activity of toremifene and its analog SERMs and their capacity to destabilize GP. We found a disconnect between the two phenotypes that is most clearly evident for the close structural analog ospemifene and suggests multiple mechanisms of toremifene action. Specifically, whereas ospemifene resembled toremifene in its capacity to destabilize EBOV GP at acid pH, ospemifene was a much less potent viral entry inhibitor. Given that the two compounds differ only in the substitution of the tertiary amine in toremifene with a hydroxy group in ospemifene, we speculate that they differ not in their capacity to bind to GP but, rather, in the enhanced lysosomotropic activity of toremifene. This property, conferred by toremifene’s tertiary amine, is observed in a large class of otherwise structurally unrelated class II cationic amphiphilic drugs (CADs) (24, 62–65) and is expected to enhance the accumulation of toremifene, but not ospemifene, in acidic intracellular compartments. Concordantly, we have observed that toremifene induces profound changes in the morphology and dynamics of cellular endo/lysosomal compartments (E. Mittler, T. P. Alkutkar, R. K. Jangra, and K. Chandran, unpublished data). These unwanted effects may limit the utility of toremifene and other CADs as antifilovirus therapeutics.
In summary, we describe a simple and highly adaptable assay that can be used to measure the thermostability of viral membrane-embedded GP proteins from diverse filoviruses under a variety of conditions relevant to cell entry. Aside from its utility in mechanistic studies of filovirus entry, this assay should facilitate the engineering of GP variants with enhanced stability for use in vaccine development, the discovery of new antiviral drugs that alter GP stability, and the identification of host factors that drive or inhibit filovirus entry by modulating GP fusogenicity.
MATERIALS AND METHODS
Cell lines and viruses.
Vero African grivet kidney cells were cultured in Dulbecco’s modified Eagle medium (DMEM) (Life Technologies, Carlsbad, CA) supplemented with 2% fetal bovine serum (Atlanta Biologicals, Flowery Branch, GA), 1% penicillin-streptomycin (Life Technologies), and GlutaMax. Cells were grown at 37°C and 5% CO2 in a humidified incubator.
The recombinant vesicular stomatitis Indiana viruses (rVSV) encoding enhanced green fluorescent protein (eGFP) in the first position with GP proteins from EBOV/Mayinga (EBOV/H.sap-tc/COD/76/Yambuku-Mayinga), SUDV/Boneface (SUDV/C.por-lab/SSD/76/Boneface), and BOMV (BOMV/Mops condylurus/SLE/2016/PREDICT_SLAB000156) in place of VSV G were generated as previously described (43, 49, 66). Viruses containing EBOV/Mayinga lacking Muc (rVSV-GPΔMuc) were generated by genetic deletion of residues 309 to 489 in the rVSV vector (36). Viruses encoding CatB-independent mutant EBOV GPs were generated previously (43).
To generate rVSVs bearing MARV GP, the previously described vector, VSV(mNG-P)ΔG (66, 67) encoding the fluorescent protein mNeonGreen (mNG) fused to the VSV phosphoprotein (P), was engineered to encode MARV GP (MARV/H.sap-tc/KEN/80/Mt. Elgon-Musoke) in the VSV G position. rVSV (mNG-P)-MARV GP was recovered using a plasmid-based rescue system in 293T cells as described previously (68) and amplified in Vero cells. Viral genomic RNA isolated from viral supernatants was subjected to reverse transcriptase PCR (RT-PCR) with VSV genome-specific primers flanking the GP gene as previously described, and the sequence of the resulting cDNA was verified by Sanger sequencing.
All experiments with rVSVs were carried out using enhanced biosafety level 2 procedures approved by the Einstein Institutional Biosafety Committee.
Antibodies.
ADI-15878, ADI-15750, and ADI-16061 were described previously (38). KZ52 (37) was kindly provided by Dennis Burton (Scripps Research Institute, La Jolla, CA). MR191 (69) was kindly provided by Zachary Bornholdt (Mapp Biopharmaceuticals, San Diego, CA, USA). MR72 (69) was expressed and purified as described previously (66). 14G7 (39) was kindly provided by John Dye (USAMRIID, Fort Detrick, MD, USA).
In vitro proteolytic cleavage reactions.
Cleavage conditions, including enzyme concentrations and cleavage times, were optimized for complete cleavage of GP→GPCL by Western blotting as indicated below. rVSV-EBOV GP and GPΔMuc were cleaved with 500 ng/μL thermolysin (THL; Sigma-Aldrich, St. Louis, MO) for 60 min and 30 min, respectively. rVSV-SUDV GP and rVSV-BOMV GP were cleaved with THL (250 ng/μL for 60 min). The CatB-independent mutant EBOV GPs were cleaved with THL using previously described and optimized conditions for complete cleavage (200 ng/μl for 60 min) (43). THL cleavage reactions were terminated by adding 10 mM phosphoramidon (Peptides International, Inc., Louisville, KY). For the CatL cleavage experiments, recombinant human CatL (R&D Systems Inc., Minneapolis, MN) was activated on ice for 30 min, and then rVSV-EBOV GP was cleaved for 60 min (2 μg/ml) at pH 5.5; reactions were terminated with 0.1 mM E-64 (Sigma-Aldrich, St. Louis, MO), a broad-spectrum cysteine protease inhibitor. All THL and CatL reactions were conducted at 37°C. Following cleavage, viruses were immediately used for ELISA experiments as described below.
SDS-PAGE and Western blotting.
rVSVs bearing uncleaved, THL-cleaved, or CatL-cleaved GPs were incubated with protein N-glycosidase F (PNGaseF, 250 U; New England Biolabs, Ipswich, MA) under reducing conditions for 16 h at 37°C to remove N-linked glycans. Deglycosylated samples were then resolved in 10% Novex Tricine SDS-polyacrylamide gels (Thermo Fisher, Grand Island, NY). rVSV-BOMV GP and THL-cleaved GPs were instead resolved in Bolt 4 to12% gradient gels (Thermo Fisher) with EBOV GPs for comparison. GP was detected by Western blotting with an anti-GP1 polyclonal rabbit serum described previously (21) followed by an Alexa Fluor 680 dye conjugated anti-rabbit secondary antibody (Thermo Fisher). Blots were imaged using the Li-Cor Fc fluorescence imager (Li-Cor, Lincoln, NE).
Epitope-loss ELISA.
rVSVs were cleaved as indicated above. Cleaved and/or uncleaved virions were diluted in phosphate-buffered saline (PBS) (pH 7.5) and then incubated at a temperature range from 42 to 80°C in a thermocycler (actual range for each virus indicated in Results) for 10 min followed by a temperature ramp to 4°C. After cooling, virus was directly captured onto high-binding 96-well half-area ELISA plates (Corning, Corning, NY). Plates were then blocked using 3% bovine serum albumin (BSA) in PBS. EBOV GP was detected with KZ52, ADI-15878, ADI-15750, ADI-16061, MR72, or 14G7 as indicated. MARV GP was detected with MR191. Bound antibody was detected with an anti-human antibody conjugated to horseradish peroxidase (HRP; EMD Millipore, Burlington, MA) and Ultra-TMB substrate (Thermo Fisher). All binding steps were carried out at 37°C for 1 h. Binding curves were generated using Prism (GraphPad Software, La Jolla, CA) (nonlinear regression, variable slope [four parameters]).
The effect of acid pH on GP thermostability was assessed by ELISA as above, except that the PBS incubation buffer was adjusted to pH values ranging from 5.2 to 8.0 as indicated during the heating step. To assess the effect of toremifene on GP thermostability, virus was pretreated with the drug for 1 h at room temperature and heated in the presence of 10 μM toremifene in PBS adjusted to pH ranging from 5.2 to 8.0. Drug dose-response experiments were conducted by pretreating virus with toremifene citrate, clomifene citrate (Sigma-Aldrich), ospemifene (Santa Cruz Biotechnology, Dallas, TX), or 1% dimethyl sulfoxide (DMSO) as vehicle control for 1 h at pH 5.2 and room temperature. Here, EBOV GP was detected with KZ52 and MARV GP with MR191, respectively. In these experiments, all antibody incubations were carried out at pH 7.4 to eliminate possible pH effects on antibody binding.
Control ELISAs to verify virion and protein capture.
rVSV-EBOV GPΔMuc was membrane labeled by incubating virions with 5 mM function-spacer-lipid (FSL)-biotin (Sigma-Aldrich, St. Louis, MO) for 1 h at 37°C as described previously (45). In separate reactions, GP was directly labeled using the amine-specific biotinylation reagent EZ-Link NHS-PEG4-Biotin (Thermo Fisher) according to the manufacturer’s instructions. Virions were then incubated at a range of temperatures and bound to ELISA plates as indicated above. Biotin-labeled virions were detected using Pierce streptavidin conjugated to HRP (Strep-HRP; Thermo Fisher), followed by detection with Ultra-TMB substrate.
rVSV infections.
VSVs bearing EBOV GPΔMuc or VSV G were incubated with decreasing concentrations of toremifene, clomifene, or ospemifene in DMEM for 1 h at room temperature. The virus-drug mixture was added to confluent Vero cells in 96-well culture plates and incubated for 1 h at 37°C. To avoid additional rounds of infection, 20 mM NH4Cl was added. Percent infection was scored 14 to 16 hours postinfection (h p.i.) using a Cytation 5 cell imager (BioTek, Winooski, VT). Infection was normalized to control (0 μM drug), and percent infectivity curves were generated using GraphPad Prism (nonlinear regression, variable slope [four parameters]).
Chemical structures.
Small-molecule inhibitor structures were prepared using MarvinSketch 19.9.0, 2019 (ChemAxon; https://chemaxon.com/products/marvin).
ACKNOWLEDGMENTS
We thank I. Gutierrez, E. Valencia, L. Polanco, C. Harold, and T. Alkutkar for laboratory management and technical support. We thank J. M. Fels for his comments and input on earlier versions of the manuscript.
This work was supported by National Institutes of Health (NIH) grant R01AI134824 (to K.C.) and USAID PREDICT program grant GHN-A-OO-09-00010-00 (to S.J.A.). R.H.B. III was partially supported by NIH training grant 2T32GM007288-45 (Medical Scientist Training Program) at Albert Einstein College of Medicine.
K.C. is a member of the scientific advisory board of Integrum Scientific, LLC.
REFERENCES
- 1.Kortepeter MG, Bausch DG, Bray M. 2011. Basic clinical and laboratory features of filoviral hemorrhagic fever. J Infect Dis 204(Suppl 3):S810–6. doi: 10.1093/infdis/jir299. [DOI] [PubMed] [Google Scholar]
- 2.Schieffelin JS, Shaffer JG, Goba A, Gbakie M, Gire SK, Colubri A, Sealfon RSG, Kanneh L, Moigboi A, Momoh M, Fullah M, Moses LM, Brown BL, Andersen KG, Winnicki S, Schaffner SF, Park DJ, Yozwiak NL, Jiang P-P, Kargbo D, Jalloh S, Fonnie M, Sinnah V, French I, Kovoma A, Kamara FK, Tucker V, Konuwa E, Sellu J, Mustapha I, Foday M, Yillah M, Kanneh F, Saffa S, Massally JLB, Boisen ML, Branco LM, Vandi MA, Grant DS, Happi C, Gevao SM, Fletcher TE, Fowler RA, Bausch DG, Sabeti PC, Khan SH, Garry RF, KGH Lassa Fever Program, Viral Hemorrhagic Fever Consortium, WHO Clinical Response Team . 2014. Clinical illness and outcomes in patients with Ebola in Sierra Leone. N Engl J Med 371:2092–2100. doi: 10.1056/NEJMoa1411680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Leligdowicz A, Fischer WA, Uyeki TM, Fletcher TE, Adhikari NKJ, Portella G, Lamontagne F, Clement C, Jacob ST, Rubinson L, Vanderschuren A, Hajek J, Murthy S, Ferri M, Crozier I, Ibrahima E, Lamah M-C, Schieffelin JS, Brett-Major D, Bausch DG, Shindo N, Chan AK, O'Dempsey T, Mishra S, Jacobs M, Dickson S, Lyon GM, Fowler RA. 2016. Ebola virus disease and critical illness. Crit Care 20:217. doi: 10.1186/s13054-016-1325-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization. 2016. Situation report: Ebola virus disease: 10 June 2016. World Health Organization, Geneva, Switzerland. [Google Scholar]
- 5.Henao-Restrepo AM, Camacho A, Longini IM, Watson CH, Edmunds WJ, Egger M, Carroll MW, Dean NE, Diatta I, Doumbia M, Draguez B, Duraffour S, Enwere G, Grais R, Gunther S, Gsell P-S, Hossmann S, Watle SV, Kondé MK, Kéïta S, Kone S, Kuisma E, Levine MM, Mandal S, Mauget T, Norheim G, Riveros X, Soumah A, Trelle S, Vicari AS, Røttingen J-A, Kieny M-P. 2017. Efficacy and effectiveness of an rVSV-vectored vaccine in preventing Ebola virus disease: final results from the Guinea ring vaccination, open-label, cluster-randomised trial (Ebola Ça Suffit!). Lancet 389:505–518. doi: 10.1016/S0140-6736(16)32621-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Edwards MR, Basler CF. 2019. Current status of small molecule drug development for Ebola virus and other filoviruses. Curr Opin Virol 35:42–56. doi: 10.1016/j.coviro.2019.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lee JE, Fusco ML, Hessell AJ, Oswald WB, Burton DR, Saphire EO. 2008. Structure of the Ebola virus glycoprotein bound to an antibody from a human survivor. Nature 454:177–182. doi: 10.1038/nature07082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bornholdt ZA, Ndungo E, Fusco ML, Bale S, Flyak AI, Crowe JE, Chandran K, Saphire EO. 2016. Host-primed Ebola virus GP exposes a hydrophobic NPC1 receptor-binding pocket, revealing a target for broadly neutralizing antibodies. mBio 7:e02154-15. doi: 10.1128/mBio.02154-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wang H, Shi Y, Song J, Qi J, Lu G, Yan J, Gao GF. 2016. Ebola viral glycoprotein bound to its endosomal receptor Niemann-Pick C1. Cell 164:258–268. doi: 10.1016/j.cell.2015.12.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tran EEH, Simmons JA, Bartesaghi A, Shoemaker CJ, Nelson E, White JM, Subramaniam S. 2014. Spatial localization of the Ebola virus glycoprotein mucin-like domain determined by cryo-electron tomography. J Virol 88:10958–10962. doi: 10.1128/JVI.00870-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Beniac DR, Booth TF. 2017. Structure of the Ebola virus glycoprotein spike within the virion envelope at 11 Å resolution. Sci Rep 7:46374. doi: 10.1038/srep46374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Weissenhorn W, Carfí A, Lee KH, Skehel JJ, Wiley DC. 1998. Crystal structure of the Ebola virus membrane fusion subunit, GP2, from the envelope glycoprotein ectodomain. Mol Cell 2:605–616. doi: 10.1016/s1097-2765(00)80159-8. [DOI] [PubMed] [Google Scholar]
- 13.Malashkevich VN, Schneider BJ, McNally ML, Milhollen MA, Pang JX, Kim PS. 1999. Core structure of the envelope glycoprotein GP2 from Ebola virus at 1.9-Å resolution. Proc Natl Acad Sci U S A 96:2662–2667. doi: 10.1073/pnas.96.6.2662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Miller EH, Chandran K. 2012. Filovirus entry into cells - new insights. Curr Opin Virol 2:206–214. doi: 10.1016/j.coviro.2012.02.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Salata C, Calistri A, Alvisi G, Celestino M, Parolin C, Palù G. 2019. Ebola virus entry: from molecular characterization to drug discovery. Viruses 11:274. doi: 10.3390/v11030274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mulherkar N, Raaben M, de la Torre JC, Whelan SP, Chandran K. 2011. The Ebola virus glycoprotein mediates entry via a non-classical dynamin-dependent macropinocytic pathway. Virology 419:72–83. doi: 10.1016/j.virol.2011.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nanbo A, Imai M, Watanabe S, Noda T, Takahashi K, Neumann G, Halfmann P, Kawaoka Y. 2010. Ebolavirus is internalized into host cells via macropinocytosis in a viral glycoprotein-dependent manner. PLoS Pathog 6:e1001121. doi: 10.1371/journal.ppat.1001121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Saeed MF, Kolokoltsov AA, Albrecht T, Davey RA. 2010. Cellular entry of Ebola virus involves uptake by a macropinocytosis-like mechanism and subsequent trafficking through early and late endosomes. PLoS Pathog 6:e1001110. doi: 10.1371/journal.ppat.1001110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Simmons JA, D'Souza RS, Ruas M, Galione A, Casanova JE, White JM. 2016. Ebolavirus glycoprotein directs fusion through NPC1+ endolysosomes. J Virol 90:605–610. doi: 10.1128/JVI.01828-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Spence JS, Krause TB, Mittler E, Jangra RK, Chandran K. 2016. Direct visualization of Ebola virus fusion triggering in the endocytic pathway. mBio 7:e01857-15. doi: 10.1128/mBio.01857-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chandran K, Sullivan NJ, Felbor U, Whelan SP, Cunningham JM. 2005. Endosomal proteolysis of the Ebola virus glycoprotein is necessary for infection. Science 308:1643–1645. doi: 10.1126/science.1110656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Schornberg K, Matsuyama S, Kabsch K, Delos S, Bouton A, White J. 2006. Role of endosomal cathepsins in entry mediated by the Ebola virus glycoprotein. J Virol 80:4174–4178. doi: 10.1128/JVI.80.8.4174-4178.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Misasi J, Chandran K, Yang J-Y, Considine B, Filone CM, Côté M, Sullivan N, Fabozzi G, Hensley L, Cunningham J. 2012. Filoviruses require endosomal cysteine proteases for entry but exhibit distinct protease preferences. J Virol 86:3284–3292. doi: 10.1128/JVI.06346-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Carette JE, Raaben M, Wong AC, Herbert AS, Obernosterer G, Mulherkar N, Kuehne AI, Kranzusch PJ, Griffin AM, Ruthel G, Dal Cin P, Dye JM, Whelan SP, Chandran K, Brummelkamp TR. 2011. Ebola virus entry requires the cholesterol transporter Niemann-Pick C1. Nature 477:340–343. doi: 10.1038/nature10348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Côté M, Misasi J, Ren T, Bruchez A, Lee K, Filone CM, Hensley L, Li Q, Ory D, Chandran K, Cunningham J. 2011. Small molecule inhibitors reveal Niemann-Pick C1 is essential for Ebola virus infection. Nature 477:344–348. doi: 10.1038/nature10380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Thoennes S, Li Z-N, Lee B-J, Langley WA, Skehel JJ, Russell RJ, Steinhauer DA. 2008. Analysis of residues near the fusion peptide in the influenza hemagglutinin structure for roles in triggering membrane fusion. Virology 370:403–414. doi: 10.1016/j.virol.2007.08.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cotter CR, Jin H, Chen Z. 2014. A single amino acid in the stalk region of the H1N1pdm influenza virus HA protein affects viral fusion, stability and infectivity. PLoS Pathog 10:e1003831. doi: 10.1371/journal.ppat.1003831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Eggink D, de Taeye SW, Bontjer I, Klasse PJ, Langedijk JPM, Berkhout B, Sanders RW. 2016. HIV-1 escape from a peptidic anchor inhibitor through stabilization of the envelope glycoprotein spike. J Virol 90:10587–10599. doi: 10.1128/JVI.01616-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wang MK, Lim S-Y, Lee SM, Cunningham JM. 2017. Biochemical basis for increased activity of Ebola glycoprotein in the 2013-16 epidemic. Cell Host Microbe 21:367–375. doi: 10.1016/j.chom.2017.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Diehl WE, Lin AE, Grubaugh ND, Carvalho LM, Kim K, Kyawe PP, McCauley SM, Donnard E, Kucukural A, McDonel P, Schaffner SF, Garber M, Rambaut A, Andersen KG, Sabeti PC, Luban J. 2016. Ebola virus glycoprotein with increased infectivity dominated the 2013–2016 epidemic. Cell 167:1088–1098.e1–e5. doi: 10.1016/j.cell.2016.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zhao Y, Ren J, Harlos K, Jones DM, Zeltina A, Bowden TA, Padilla-Parra S, Fry EE, Stuart DI. 2016. Toremifene interacts with and destabilizes the Ebola virus glycoprotein. Nature 535:169–172. doi: 10.1038/nature18615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ren J, Zhao Y, Fry EE, Stuart DI. 2018. Target identification and mode of action of four chemically divergent drugs against ebolavirus infection. J Med Chem 61:724–733. doi: 10.1021/acs.jmedchem.7b01249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zhao Y, Ren J, Fry EE, Xiao J, Townsend AR, Stuart DI. 2018. Structures of Ebola virus glycoprotein complexes with tricyclic antidepressant and antipsychotic drugs. J Med Chem 61:4938–4945. doi: 10.1021/acs.jmedchem.8b00350. [DOI] [PubMed] [Google Scholar]
- 34.Fels JM, Spence JS, Bortz RH, Bornholdt ZA, Chandran K. 2019. A hyperstabilizing mutation in the base of the Ebola virus glycoprotein acts at multiple steps to abrogate viral entry. mBio 10:e01408-19. doi: 10.1128/mBio.01408-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Brecher M, Schornberg KL, Delos SE, Fusco ML, Saphire EO, White JM. 2012. Cathepsin cleavage potentiates the Ebola virus glycoprotein to undergo a subsequent fusion-relevant conformational change. J Virol 86:364–372. doi: 10.1128/JVI.05708-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Jeffers SA, Sanders DA, Sanchez A. 2002. Covalent modifications of the Ebola virus glycoprotein. J Virol 76:12463–12472. doi: 10.1128/jvi.76.24.12463-12472.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Maruyama T, Rodriguez LL, Jahrling PB, Sanchez A, Khan AS, Nichol ST, Peters CJ, Parren PW, Burton DR. 1999. Ebola virus can be effectively neutralized by antibody produced in natural human infection. J Virol 73:6024–6030. doi: 10.1128/JVI.73.7.6024-6030.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wec AZ, Herbert AS, Murin CD, Nyakatura EK, Abelson DM, Fels JM, He S, James RM, de La Vega M-A, Zhu W, Bakken RR, Goodwin E, Turner HL, Jangra RK, Zeitlin L, Qiu X, Lai JR, Walker LM, Ward AB, Dye JM, Chandran K, Bornholdt ZA. 2017. Antibodies from a human survivor define sites of vulnerability for broad protection against ebolaviruses. Cell 169:878–890.e1–e6. doi: 10.1016/j.cell.2017.04.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Olal D, Kuehne AI, Bale S, Halfmann P, Hashiguchi T, Fusco ML, Lee JE, King LB, Kawaoka Y, Dye JM, Saphire EO. 2012. Structure of an antibody in complex with its mucin domain linear epitope that is protective against Ebola virus. J Virol 86:2809–2816. doi: 10.1128/JVI.05549-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lee JE, Kuehne A, Abelson DM, Fusco ML, Hart MK, Saphire EO. 2008. Complex of a protective antibody with its Ebola virus GP peptide epitope: unusual features of a V lambda x light chain. J Mol Biol 375:202–216. doi: 10.1016/j.jmb.2007.10.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wilson JA, Hevey M, Bakken R, Guest S, Bray M, Schmaljohn AL, Hart MK. 2000. Epitopes involved in antibody-mediated protection from Ebola virus. Science 287:1664–1666. doi: 10.1126/science.287.5458.1664. [DOI] [PubMed] [Google Scholar]
- 42.Miller EH, Obernosterer G, Raaben M, Herbert AS, Deffieu MS, Krishnan A, Ndungo E, Sandesara RG, Carette JE, Kuehne AI, Ruthel G, Pfeffer SR, Dye JM, Whelan SP, Brummelkamp TR, Chandran K. 2012. Ebola virus entry requires the host-programmed recognition of an intracellular receptor. EMBO J 31:1947–1960. doi: 10.1038/emboj.2012.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wong AC, Sandesara RG, Mulherkar N, Whelan SP, Chandran K. 2010. A forward genetic strategy reveals destabilizing mutations in the ebolavirus glycoprotein that alter its protease dependence during cell entry. J Virol 84:163–175. doi: 10.1128/JVI.01832-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Shedlock DJ, Bailey MA, Popernack PM, Cunningham JM, Burton DR, Sullivan NJ. 2010. Antibody-mediated neutralization of Ebola virus can occur by two distinct mechanisms. Virology 401:228–235. doi: 10.1016/j.virol.2010.02.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ng M, Ndungo E, Jangra RK, Cai Y, Postnikova E, Radoshitzky SR, Dye JM, Ramírez de Arellano E, Negredo A, Palacios G, Kuhn JH, Chandran K. 2014. Cell entry by a novel European filovirus requires host endosomal cysteine proteases and Niemann-Pick C1. Virology 468–470:637–646. doi: 10.1016/j.virol.2014.08.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Murin CD, Bruhn JF, Bornholdt ZA, Copps J, Stanfield R, Ward AB. 2018. Structural basis of pan-ebolavirus neutralization by an antibody targeting the glycoprotein fusion loop. Cell Rep 24:2723–2732.e1–e4. doi: 10.1016/j.celrep.2018.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.West BR, Moyer CL, King LB, Fusco ML, Milligan JC, Hui S, Saphire EO. 2018. Structural basis of pan-ebolavirus neutralization by a human antibody against a conserved, yet cryptic epitope. mBio 9:e01674-18. doi: 10.1128/mBio.01674-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wec AZ, Bornholdt ZA, He S, Herbert AS, Goodwin E, Wirchnianski AS, Gunn BM, Zhang Z, Zhu W, Liu G, Abelson DM, Moyer CL, Jangra RK, James RM, Bakken RR, Bohorova N, Bohorov O, Kim DH, Pauly MH, Velasco J, Bortz RH, Whaley KJ, Goldstein T, Anthony SJ, Alter G, Walker LM, Dye JM, Zeitlin L, Qiu X, Chandran K. 2019. Development of a human antibody cocktail that deploys multiple functions to confer pan-ebolavirus protection. Cell Host Microbe 25:39–48.e1–e5. doi: 10.1016/j.chom.2018.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Goldstein T, Anthony SJ, Gbakima A, Bird BH, Bangura J, Tremeau-Bravard A, Belaganahalli MN, Wells HL, Dhanota JK, Liang E, Grodus M, Jangra RK, DeJesus VA, Lasso G, Smith BR, Jambai A, Kamara BO, Kamara S, Bangura W, Monagin C, Shapira S, Johnson CK, Saylors K, Rubin EM, Chandran K, Lipkin WI, Mazet JAK. 2018. The discovery of Bombali virus adds further support for bats as hosts of ebolaviruses. Nat Microbiol 3:1084–1089. doi: 10.1038/s41564-018-0227-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Markosyan RM, Miao C, Zheng Y-M, Melikyan GB, Liu S-L, Cohen FS. 2016. Induction of cell-cell fusion by Ebola virus glycoprotein: low pH is not a trigger. PLoS Pathog 12:e1005373. doi: 10.1371/journal.ppat.1005373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Fénéant L, Szymańska-de Wijs KM, Nelson EA, White JM. 2019. An exploration of conditions proposed to trigger the Ebola virus glycoprotein for fusion. PLoS One 14:e0219312. doi: 10.1371/journal.pone.0219312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Gong X, Qian H, Zhou X, Wu J, Wan T, Cao P, Huang W, Zhao X, Wang X, Wang P, Shi Y, Gao GF, Zhou Q, Yan N. 2016. Structural insights into the Niemann-Pick C1 (NPC1)-mediated cholesterol transfer and Ebola infection. Cell 165:1467–1478. doi: 10.1016/j.cell.2016.05.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Gregory SM, Harada E, Liang B, Delos SE, White JM, Tamm LK. 2011. Structure and function of the complete internal fusion loop from ebolavirus glycoprotein 2. Proc Natl Acad Sci U S A 108:11211–11216. doi: 10.1073/pnas.1104760108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Harrison JS, Higgins CD, Chandran K, Lai JR. 2011. Designed protein mimics of the Ebola virus glycoprotein GP2 α-helical bundle: stability and pH effects. Protein Sci 20:1587–1596. doi: 10.1002/pro.688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Shaikh F, Zhao Y, Alvarez L, Iliopoulou M, Lohans C, Schofield CJ, Padilla-Parra S, Siu SWI, Fry EE, Ren J, Stuart DI. 2019. Structure-based in silico screening identifies a potent ebolavirus inhibitor from a traditional Chinese medicine library. J Med Chem 62:2928–2937. doi: 10.1021/acs.jmedchem.8b01328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Johansen LM, Brannan JM, Delos SE, Shoemaker CJ, Stossel A, Lear C, Hoffstrom BG, Dewald LE, Schornberg KL, Scully C, Lehár J, Hensley LE, White JM, Olinger GG. 2013. FDA-approved selective estrogen receptor modulators inhibit Ebola virus infection. Sci Transl Med 5:190ra79. doi: 10.1126/scitranslmed.3005471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Chen Q, Tang K, Zhang X, Chen P, Guo Y. 2018. Establishment of pseudovirus infection mouse models for in vivo pharmacodynamics evaluation of filovirus entry inhibitors. Acta Pharm Sin B 8:200–208. doi: 10.1016/j.apsb.2017.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.King LB, Fusco ML, Flyak AI, Ilinykh PA, Huang K, Gunn B, Kirchdoerfer RN, Hastie KM, Sangha AK, Meiler J, Alter G, Bukreyev A, Crowe JE, Saphire EO. 2018. The marburgvirus-neutralizing human monoclonal antibody MR191 targets a conserved site to block virus receptor binding. Cell Host Microbe 23:101–109.e1–e4. doi: 10.1016/j.chom.2017.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Das DK, Bulow U, Diehl WE, Durham ND, Senjobe F, Chandran K, Luban J, Munro JB. 2020. Conformational changes in the Ebola virus membrane fusion machine induced by pH, Ca2+, and receptor binding. PLoS Biol 18:e3000626. doi: 10.1371/journal.pbio.3000626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Melikyan GB, Barnard RJO, Markosyan RM, Young JAT, Cohen FS. 2004. Low pH is required for avian sarcoma and leukosis virus Env-induced hemifusion and fusion pore formation but not for pore growth. J Virol 78:3753–3762. doi: 10.1128/jvi.78.7.3753-3762.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Côté M, Zheng Y-M, Liu S-L. 2009. Receptor binding and low pH coactivate oncogenic retrovirus envelope-mediated fusion. J Virol 83:11447–11455. doi: 10.1128/JVI.00748-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Shoemaker CJ, Schornberg KL, Delos SE, Scully C, Pajouhesh H, Olinger GG, Johansen LM, White JM. 2013. Multiple cationic amphiphiles induce a Niemann-Pick C phenotype and inhibit Ebola virus entry and infection. PLoS One 8:e56265. doi: 10.1371/journal.pone.0056265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Fan H, Du X, Zhang J, Zheng H, Lu X, Wu Q, Li H, Wang H, Shi Y, Gao G, Zhou Z, Tan D-X, Li X. 2017. Selective inhibition of Ebola entry with selective estrogen receptor modulators by disrupting the endolysosomal calcium. Sci Rep 7:41226. doi: 10.1038/srep41226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Halliwell WH. 1997. Cationic amphiphilic drug-induced phospholipidosis. Toxicol Pathol 25:53–60. doi: 10.1177/019262339702500111. [DOI] [PubMed] [Google Scholar]
- 65.Gehring G, Rohrmann K, Atenchong N, Mittler E, Becker S, Dahlmann F, Pöhlmann S, Vondran FWR, David S, Manns MP, Ciesek S, von Hahn T. 2014. The clinically approved drugs amiodarone, dronedarone and verapamil inhibit filovirus cell entry. J Antimicrob Chemother 69:2123–2131. doi: 10.1093/jac/dku091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Wec AZ, Nyakatura EK, Herbert AS, Howell KA, Holtsberg FW, Bakken RR, Mittler E, Christin JR, Shulenin S, Jangra RK, Bharrhan S, Kuehne AI, Bornholdt ZA, Flyak AI, Saphire EO, Crowe JE, Aman MJ, Dye JM, Lai JR, Chandran K. 2016. A “Trojan horse” bispecific-antibody strategy for broad protection against ebolaviruses. Science 354:350–354. doi: 10.1126/science.aag3267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Kleinfelter LM, Jangra RK, Jae LT, Herbert AS, Mittler E, Stiles KM, Wirchnianski AS, Kielian M, Brummelkamp TR, Dye JM, Chandran K. 2015. Haploid genetic screen reveals a profound and direct dependence on cholesterol for hantavirus membrane fusion. mBio 6:e00801-15. doi: 10.1128/mBio.00801-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Whelan SP, Ball LA, Barr JN, Wertz GT. 1995. Efficient recovery of infectious vesicular stomatitis virus entirely from cDNA clones. Proc Natl Acad Sci U S A 92:8388–8392. doi: 10.1073/pnas.92.18.8388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Flyak AI, Ilinykh PA, Murin CD, Garron T, Shen X, Fusco ML, Hashiguchi T, Bornholdt ZA, Slaughter JC, Sapparapu G, Klages C, Ksiazek TG, Ward AB, Saphire EO, Bukreyev A, Crowe JE. 2015. Mechanism of human antibody-mediated neutralization of Marburg virus. Cell 160:893–903. doi: 10.1016/j.cell.2015.01.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Hashiguchi T, Fusco ML, Bornholdt ZA, Lee JE, Flyak AI, Matsuoka R, Kohda D, Yanagi Y, Hammel M, Crowe JE, Saphire EO. 2015. Structural basis for Marburg virus neutralization by a cross-reactive human antibody. Cell 160:904–912. doi: 10.1016/j.cell.2015.01.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Pettersen EF, Goddard TD, Huang CC, Couch GS, Greenblatt DM, Meng EC, Ferrin TE. 2004. UCSF Chimera—a visualization system for exploratory research and analysis. J Comput Chem 25:1605–1612. doi: 10.1002/jcc.20084. [DOI] [PubMed] [Google Scholar]