Abstract
The incidence of pancreatic cancer (PCa) is increasing worldwide and has become one of the leading causes of cancer-related death. Screening for high risk populations is fundamental to overcome this intractable malignancy. Diabetes mellitus (DM) is classically known as a risk factor for PCa. Recently the reverse causality is in the spotlight, that is to say, DM is considered to be a manifestation of PCa. Numbers of epidemiological studies clarified that new-onset DM (≤2-year duration) was predominant in PCa patients and the relative risk for PCa inversely correlated with duration of DM. Among patients with new-onset DM, elder onset, weight loss, and rapid exacerbation of glycemic control were reported to be promising risk factors and signs, and the model was developed by combining these factors. Several pilot studies disclosed the possible utility of biomarkers to discriminate PCa-associated DM from type 2 DM. However, there is no reliable biomarkers to be used in the practice. We previously reported the application of a multivariate index for PCa based on the profile of plasma free amino acids (PFAAs) among diabetic patients. We are further investigating on the PFAA profile of PCa-associated DM, and it can be useful for developing the novel biomarker in the near future.
Keywords: pancreatic cancer, diabetes mellitus, risk factor, biomarker, screening
1. Introduction
The incidence of pancreatic cancer (PCa) is increasing worldwide, and PCa has become the 3rd leading cause of cancer-related death in the US [1] and the 4th in Japan [2]. Due to difficulty in diagnosing PCa in its early stage, only a limited proportion of patients can undergo curative resection. It is essential to select the high risk populations and conduct screening in asymptomatic individuals for improving the prognosis of PCa.
Diabetes mellitus (DM) is known as a risk factor for various malignancies: such as hepatocellular, breast, ovarian, endometrial, and gastrointestinal cancers; and total cancer incidence is reported to increase by 10% in diabetic patients [3]. DM is also recognized as a risk factor for PCa as in other cancers [4,5,6,7]. In addition, recent studies revealed that DM can develop as one of the symptoms of PCa [8,9]. Thus, DM, especially new-onset DM, is expected to be a clue to detect PCa in the early stage and improve the prognosis of this intractable malignancy.
However, the prevalence and the incidence of DM is too high, thus screening in all diabetic patients is ineffective in view of the cost-benefit balance. Further risk stratification for PCa among diabetic patients is warranted. In this review, we discuss the risk factors and biomarkers for PCa in diabetic patients.
2. New-Onset Diabetes Mellitus as a Clue for Early Diagnosis of Pancreatic Cancer
DM is a risk factor for PCa, and this classical causality was well-documented in previous studies. Everhart et al. reported a pooled relative risk (RR) of 2.1 (95% confidence interval (CI), 1.6–2.8) for PCa among diabetic patients in their meta-analysis of 9 cohort studies and 11 case-control studies [4]. Liao WC et al. recently carried out a systematic review of 9 studies (6 cohort studies and 3 case-control studies) and reported a pooled RR of 1.83 (95% CI, 1.50–2.24) [7]. Several studies also revealed a dose-response relationship between PCa incidence and fasting blood glucose [5,7,10]. Though the majority of these studies focused on type 2 DM, a few studies also documented that type 1 DM was a risk factor for PCa [11,12].
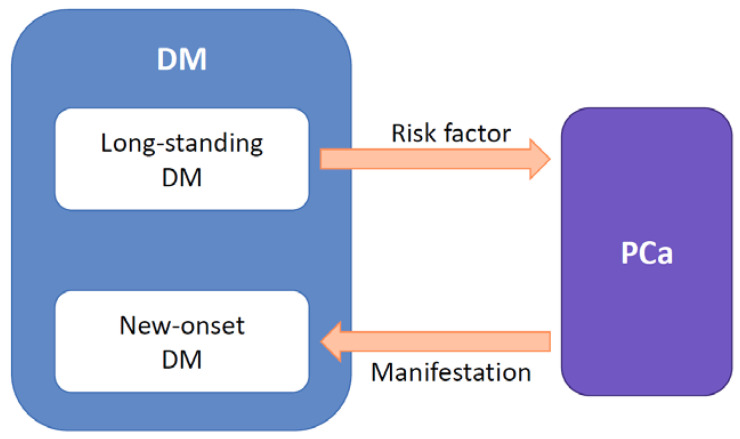
However, Chari ST et al. cast light on the reverse causality between PCa and DM. They revealed that new-onset DM (≤ 2-year duration) was predominant in patients with PCa and frequently resolved after surgical resection [13,14]. They also disclosed the increasing trend in fasting blood glucose before the diagnosis of PCa [8,13]. They speculated that new-onset DM was induced by the tumor, thus this “PCa-associated DM” can be classified as type 3c DM according to the classification proposed by the American Diabetes Association [15]. This strong association between PCa and new-onset DM was confirmed by many studies [16,17,18,19,20,21], and new-onset DM is now considered to be a manifestation of PCa (Figure 1). Among these studies, new-onset DM was defined as DM diagnosed within 2-3 years before PCa diagnosis.
Figure 1.
Bidirectional causality between diabetes mellitus (DM) and pancreatic cancer (PCa). Long-standing DM (> 2-year duration) is a risk factor for PCa, meanwhile new-onset DM (≤ 2-year duration) is a manifestation of PCa.
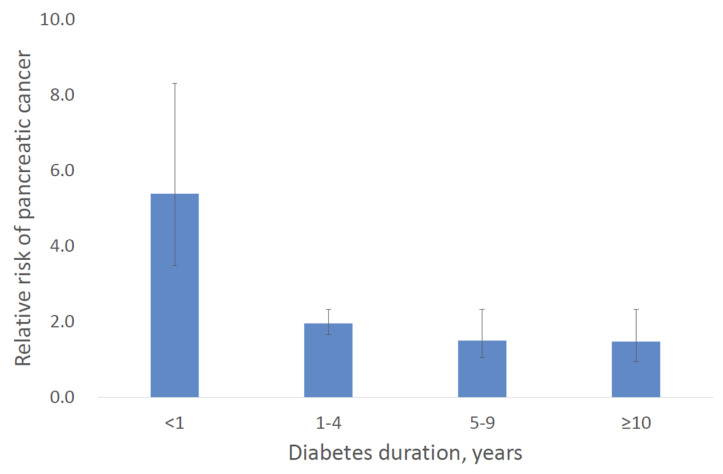
Ben Q et al. provided the important evidence on the association between PCa risk and duration of DM [9]. In their meta-analysis, the highest RR of 5.38 (95% CI, 3.49–8.30) was reported in DM patients with short duration of 1 year or less. The RR for PCa gradually decreased according to diabetes duration: 1.95 (95% CI, 1.65–2.31) in 1–4 years, 1.49 (95% CI, 1.05–2.12) in 5–9 years, and 1.47 (95% CI, 0.94–2.31) in 10 years and more. Their results are summarized in Figure 2. Thus, new-onset DM can be a diagnostic clue to select high risk populations among diabetic patients.
Figure 2.
Relative risks of pancreatic cancer in patients with diabetes mellitus according to diabetes duration. The data are quoted from Ben Q et al. [9]. Bars indicate 95% confidence intervals.
As for high risk populations for PCa, intraductal papillary mucinous neoplasm (IPMN) of the pancreas is a well-established risk factor [22,23,24,25]. To date, a number of studies investigated the association between IPMN and DM. DM is prevalent in patients with IPMN [26,27], and Capurso G et al. reported an odds ratio (OR) of 1.79 (95% CI, 1.08–2.98) for IPMN in diabetic patients [26]. In addition, DM is reported to be associated with degree of dysplasia of IPMN [28,29,30]. Morales-Oyarvide V et al. reported that the OR for high grade dysplasia (HGD) and invasive carcinoma among diabetic patients was 2.02 (95% CI, 1.02–4.01) and 2.05 (95% CI, 1.08–3.87), respectively [28]. Thus, DM is a risk factor not only for a precursor lesion of PCa, but also for malignant transformation of the precursor. Meanwhile, new-onset DM is also reported to be associated with malignant IPMN [31,32,33,34,35]. Pergolini I et al. reported a high OR of 4.615 (95% CI, 1.423–14.698) for HGD/invasive cancer in patients with new-onset or worsening diabetes [31]. New-onset DM can be considered to be a manifestation of malignant transformation of IPMN, as in development of ductal adenocarcinoma.
We previously reported that PCa patients without symptoms, such as jaundice, pain, and appetite loss, in whom new-onset DM was a only clue to diagnosis of PCa had better prognosis than symptomatic patients (median survival time, 20.2 months vs. 10.2 months, p < 0.01) [19]. Pelaez-Luna M et al. reviewed computed tomography (CT) scans performed at PCa diagnosis and before diagnosis, and they reported that only 4 patients out of 13 had unresectable disease at the onset of DM [36]. Thus, screening for PCa among patients with new-onset DM can improve the prognosis.
However, PCa incidence within 3 years of meeting criteria for diabetes was reported to be only 0.85% by Chari ST et al. [37] and 0.25% by Munigala S et al. [38]. To date, there are a few studies attempting prospective screening for PCa in new-onset DM patients. Ogawa Y et al. reported that endoscopic retrograde pancreatography demonstrated PCa in 5 out of 36 diabetic patients (13.9%) with new-onset and onset after age 55 years [39]. Damiano J et al. reported that routine imaging, preferably by magnetic resonance imaging, in 115 patients with new-onset DM aged over 50 years detected 6 cases with PCa (5.2%) [40]. Illes D et al. performed abdominal ultrasonography in 115 patients with new-onset DM, then found 3 cases (2.6%) [41]. To establish effective screening in patients with new-onset DM, further selection using risk factors and biomarkers is warranted.
3. Risk Factors for Pancreatic Cancer in Patients with New-Onset Diabetes Mellitus
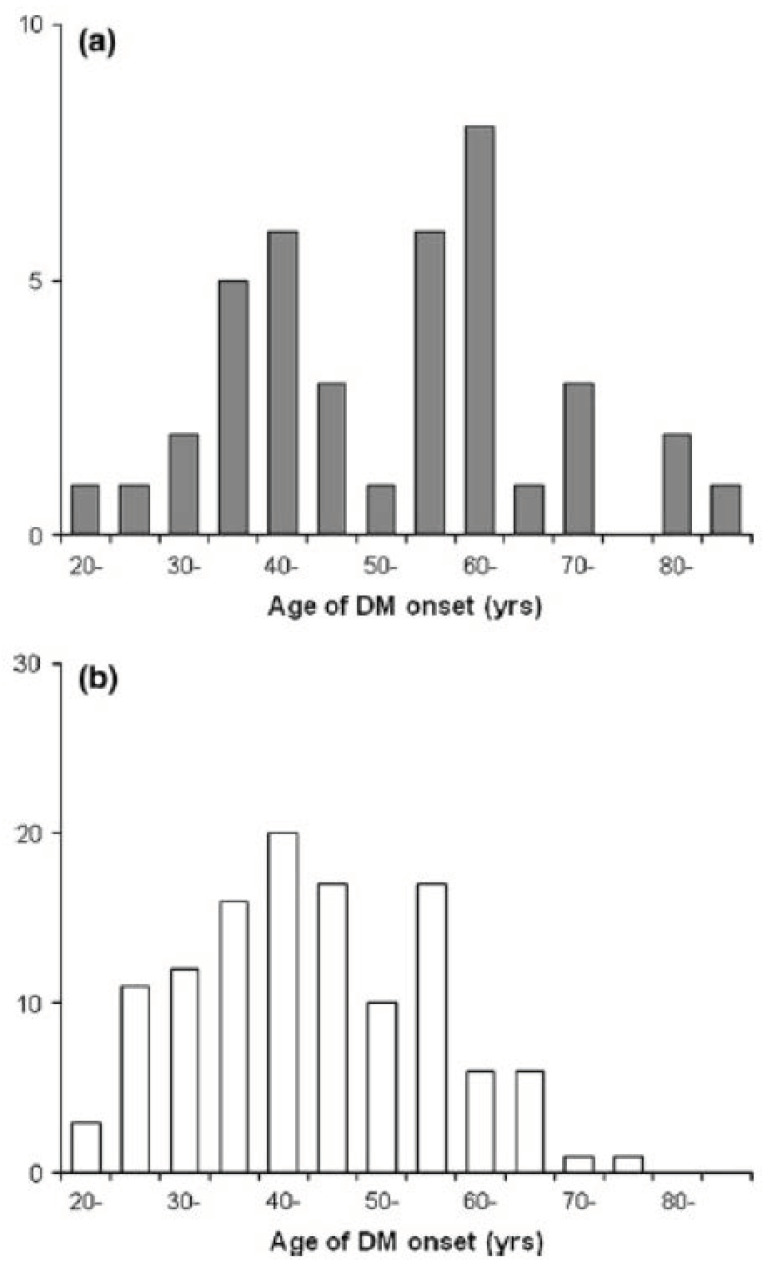
In previous reports, several risk factors for and signs of PCa were investigated in patients with new-onset DM (Table 1). Elder onset of DM is a widely accepted risk factor [37,38,42,43], and the reported RR for PCa of individuals with DM onset age of 65 or elder was 2.01 (95% CI, 1.51–2.68) [38] and that of 70 or elder was 4.52 (95% CI, 1.61–12.74) [37]. We previously reported age distribution of DM onset comparing diabetic patients with PCa and those without. Among diabetic patients with PCa, there was a prominent peak between 55–65 years, and more than half were over 55 years old (Figure 3) [43]. Smoking and alcohol consumption are known as risk factors for PCa, and the synergic interaction of DM and these habits are reported [44,45]. Smoking is also well recognized as a risk factor for type 2 DM. Nicotine, the major component in cigarette smoke, is revealed to induce premature senescence of pancreatic β cells [46]. Meanwhile, nicotine is considered to reach the pancreas via the bloodstream or directly through the papilla Vater from the duodenum [47], then cause alteration in the signal transduction pathways and in the expression of protooncogene in pancreatic cells [48]. Thus, smoking is a risk factor of both PCa and DM.
Table 1.
Risk factors, early signs, and biomarkers for pancreatic cancer in patients with diabetes mellitus.
| Risk Factor | New-Onset (≤2-Year Duration) Elder-Onset (≥65 Years) |
|---|---|
| Early sign | Body weight loss Rapid exacerbation of glycemic control |
| Biomarker | Islet amyloid polypeptide (IAP) Soluble receptor 2 of tumor necrosis factor-α (sTNF-αR2) Osteoprotegerin (OPG) Vanin-1 (VNN1) Matrix metalloproteinase 9 (MMP9) Insulin-like growth factor (IGF) Circulating RNA Plasma free amino acid profile |
Figure 3.
Age distribution of diabetes mellitus (DM) onset (a) in diabetic patients with pancreatic cancer and (b) in diabetic patients without pancreatic cancer. This figure is adopted from Mizuno S et al. [43].
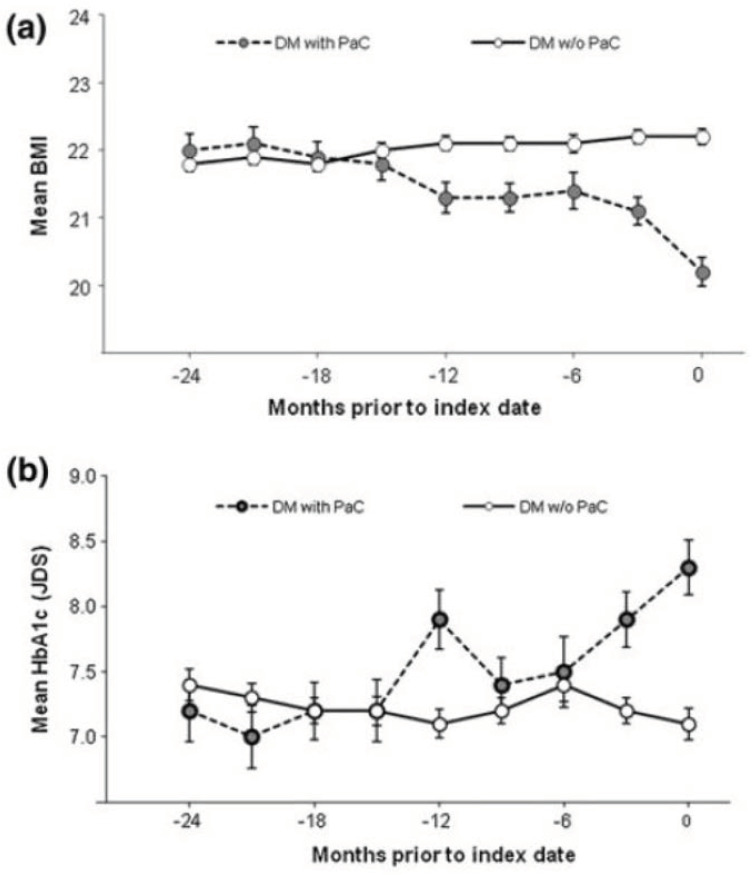
Body weight loss is a well-documented sign of PCa patients with DM [39,40,46,47,48]. Although body weight loss is a symptom also seen in type 2 DM subjects, Hart PA et al. reported significantly higher proportion of PCa-associated DM patients lost weight at onset of DM than type 2 DM patients (59% vs. 30%, p = 0.02) [49]. Mueller AM et al. calculated adjusted odds ratios (aORs) according to the degree of weight loss, and reported that aOR for weight loss by 10.0–14.9% was 3.58 (95%CI, 2.31–5.54) and that for loss by ≥ 15.0% was 4.56 (95% CI, 2.82–7.36), compared with stable weight [50]. Rapid exacerbation of glycemic control was also reported to be associated with increased risk of PCa. Huang BZ et al. reported more rapid increases in levels of glucose (37.47 mg/dL vs. 27.68 mg/dL, p < 0.01) and hemoglobin A1c (HbA1c) (1.39% vs. 0.86%, p < 0.001) in the month preceding the diagnosis of DM [51]. We previously demonstrated that simultaneous weight loss and HbA1c elevation were seen one year before the diagnosis of PCa among diabetic patients (Figure 4) [43]. The combination of signs can be helpful for early diagnosis of PCa.
Figure 4.
Temporal changes in (a) body mass index (BMI) and (b) hemoglobin A1c (HbA1c) in diabetic patients with pancreatic cancer (black circle with dashed line) and those without (white circle with solid line). This figure is adopted from Mizuno S et al. [43]. Bars indicate standard error of the mean. DM, diabetes mellitus; PCa, pancreatic cancer.
4. Discrimination Models for Pancreatic Cancer in Patients with New-Onset Diabetes Mellitus
By using the combination of these risk factors and signs described above, enriching patients with new-onset DM for PCa screening is expected to be established. There are a few models reported to identify high risk individuals among patients with new-onset DM (Table 2).
Table 2.
Discrimination models for pancreatic cancer in patients with new-onset diabetes mellitus.
| Author | Sample Size | Study Design | Factors | AUC |
|---|---|---|---|---|
| Dong X [52] | 413 | Matched case-control study | BMI, age of DM onset, HBV infection, T.Bil, ALT, Cre, APO-A1, WBC | 0.82 |
| Boursi B [53] | 109,385 | Retrospective cohort study | Age, BMI, change in BMI, smoking, use of PPI, anti-diabetic medications, HbA1c, cholesterol, Hb, Cre, ALP | 0.82 |
| Sharma A [54] | 1561 | Retrospective cohort study | Change in weight, change in blood glucose, age at DM onset | 0.87 |
AUC, area under the curve; BMI, body mass index; DM, diabetes mellitus; HBV, hepatitis B virus; T.Bil, total bilirubin; ALT, alanine aminotransferase; Cre, creatinine; APO-A1, apolipoprotein-A1; WBC, white blood cell; PPI, proton pump inhibitors; HbA1c, hemoglobin A1c; Hb, hemoglobin; ALP, alkaline phosphatase.
Dong X et al. conducted a matched case-control study of 171 cases and 242 controls with new-onset DM and reported a prediction model which included 8 markers [52]. The area under the curve (AUC) of their model was up to 0.815, though the results were not validated.
Boursi B et al. conducted a retrospective cohort study of 109,385 patients with new-onset DM and reported a discrimination model which comprised 11 factors [53]. Their model provided an AUC of 0.82 and could reduce individuals who would undergo definitive screening to only 6.19% when the predicted risk threshold for PCa screening was set at 1% over 3 years. They performed internal validation using a bootstrapping procedure and reported negligible optimism.
Sharma A et al. reported a more simple discrimination model which was called Enriching New-Onset Diabetes for Pancreatic Cancer (END-PAC) [54]. They conducted a retrospective cohort study of 1561 patients with new-onset DM and developed the END-PAC model which comprised only 3 factors: change in weight, change in blood glucose, and age at onset. The AUC of this model was 0.87. In the validation cohort, an END-PAC score of ≥ 3 identified PCa with a sensitivity of 78%, specificity of 82%, and enriched the PCa prevalence of 0.82% in the population-based cohort to 3.6% (4.4-fold) in END-PAC model-defined cohort. The authors recently reported a larger-scale validation among 13,947 patients with new-onset DM [55]. The AUC was 0.75, and the sensitivity, specificity, positive predictive value, and negative predictive value were 62.6%, 78.5%, 2.0%, and 99.7%, respectively.
5. Biomarkers for Pancreatic Cancer in Patients with Diabetes Mellitus
In addition to the risk stratification by using the combination of risk factors, development of biomarkers to discriminate PCa-associated DM, which is classified as type 3c DM, from type 2 DM is expected to be useful for the effective PCa screening. Less invasive measurement of biomarkers can be a second sieve to select individuals who should undergo invasive examinations, such as endoscopic ultrasonography (EUS) and contrast-enhanced CT. Several biomarkers are reported to be potent for diagnosing PCa-associated DM (Table 1).
5.1. Islet Amyloid Polypeptide
Permert J et al. reported that plasma concentration of islet amyloid polypeptide (IAPP), a hormonal factor secreted from the pancreatic beta cells, elevated in patients with PCa-associated DM, though that in patients with type 2 DM was normal or low [56]. IAPP has diabetogenic effects in vitro and in vivo, thus was considered to cause insulin resistance in PCa-associated DM. Chari ST et al. confirmed the elevation of IAPP among patients with PCa-associated DM in their study of larger sample size [57]. However, the diagnostic yield was not satisfactory, and the sensitivity was only 50%.
5.2. Soluble Receptor 2 of Tumor Necrosis Factor-α
C-reactive protein (CRP) is increased in PCa patients due to the systemic inflammatory response to the tumor, and tumor necrosis factor-α (TNF-α) is an upregulating factor of CRP. Grote VA et al. measured the prediagnostic concentrations of soluble TNF receptors (sTNF-Rs) [58]. They disclosed that PCa risk tended to increase with higher levels of sTNF-R2 and this association was stronger in diabetic individuals. The OR of PCa for a doubling in sTNF-R2 concentration was 4.76 (95% CI, 1.11–20.37) among diabetic individuals, whereas that among non-diabetic individuals was 1.12 (95% CI, 0.73–1.72).
5.3. Osteoprotegerin
Osteoprotegerin (OPG) is a soluble decoy receptor for TNF-related apoptosis inducing ligand (TRAIL), and belongs to the TNF receptor superfamily (TNFRSF). Shi W et al. conducted a meta-analysis on gene expression microarray datasets, and found that OPG was up-regulated in PCa tissues [59]. The serum level of OPG was elevated in patients with PCa-associated DM, and the receiver operating characteristic (ROC) curve revealed that serum OPG provided an AUC of 0.737 with a sensitivity of 68.0% and a specificity of 73.9% to distinguish PCa-associated DM from new-onset type 2DM.
5.4. Vanin-1
Huang H et al. explored specific genes using microarray analysis of peripheral blood samples, which were unique in patients with PCa-associated DM compared with type 2 DM, and reported that vanin-1 (VNN1), a pantetheinase which acts a key regulator in oxidative stress, was a candidate for a biomarker [60]. Their group later investigated the functional mechanisms of VNN1 in the pathogenesis of PCa-associated DM, and disclosed that overexpression of VNN1 in the tumor tissues decreased glutathione concentration, increased reactive oxygen species (ROS), then aggravated paraneoplastic islet dysfunction [61].
5.5. Matrix Metalloproteinase 9
Matrix metalloproteinase 9 (MMP9) is one of the zinc-dependent endopeptidase family, and is synthesized by both tumor and peritumoral stromal cells. The expression of MMP by pancreatic tumor cells is considered to be an early phenomenon, since it occurs not only advanced, but also in borderline tumors and non-invasive IPMN [62]. Microarray analysis by Huang H et al. disclosed that the combination of VNN1 and MMP9 was useful to discriminate PCa-associated DM from type 2 DM [60]. Moz S et al. reported an AUC of 0.886 by combining MMP9 and CA19-9 for discriminating PCa-associated DM from type 2 DM, though there was no significant difference compared with CA19-9 only (AUC, 0.866) [63].
5.6. Insulin-Like Growth Factor
Insulin-like growth factor (IGF) is a growth hormone-regulated polypeptide involved in both human development and the maintenance of normal function and homeostasis in most human cells, and accumulating evidence suggests that serum concentration of IGF may influence cancer risk. Suzuki H et al. reported that the polymorphic variants of IGF genes might serve as a susceptibility factor for PCa, and disclosed a high OR of 5.69 (95%CI, 2.63–12.3) by joint effect of the susceptible allele and diabetes [64].
5.7. Circulating RNA
Recently, circulating RNAs are emerging as non-invasive markers for detecting PCa [65]. Tumor cells release substantial amounts of RNA into the bloodstream that strongly resist RNases in the blood, and these circulating RNAs are upregulated in the serum and plasma of cancer patients. Dai X et al. reported a six-serum mircoRNA panel with an AUC of 0.887 to discriminate PCa-associated DM form type 2 DM [66].
5.8. Plasma Free Amino Acid Profile
Recently, metabolomic analysis using liquid chromatography-mass spectrometry is applied to various cancers and disclosed disease-specific profile of plasma free amino acids (PFAAs) [67,68]. Fukutake N et al. developed a multivariate index for PCa based on the PFAA profile of PCa patients compared with that of healthy controls [69], and we previously reported a comparable diagnostic yield of this PFAA index in individuals with DM and those without [70]. Among diabetic patients, the sensitivity was 66.7% and the specificity was 92.7%. The concentration of PFAAs is reported to be affected by DM [71,72], thus further investigation on the difference of the PFAA profile between PCa-associated DM and type 2 DM can be useful for effective PCa screening among patients with new-onset DM.
A number of studies reported the possible utility of the biomarkers of PCa-associated DM However, these studies were case-control study setting with a limited sample size, thus there is no reliable biomarker to discriminate PCa-associated DM and type 2 DM at present.
6. Conclusions
To overcome the dismal prognosis of PCa, effective screening for asymptomatic individuals is required to be established. DM is an early manifestation of PCa, thus DM can be a diagnostic clue for early detection of PCa. New-onset DM is the first sieve to enrich diabetic patients for PCa screening, and the combination of risk factors and biomarkers will be the second one. In the US, a prospective study to establish a new-onset diabetes cohort of 10,000 subjects 50 years or older (NOD study) is ongoing [73]. Further advance in the research on the risk factors and biomarkers for PCa in new-onset DM is expected.
Author Contributions
S.M. provided literature review and manuscript drafting; Y.N., K.I., K.S., H.O., T.H., Y.S., A.I., S.K., K.N., T.S. (Tatsuya Sato), R.H., T.S. (Tomotaka Saito), N.T., H.K., H.I., and K.K. provided topic outlining, expertise, and manuscript editing. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no externa funding.
Conflicts of Interest
The University of Tokyo (Tokyo, Japan) and Ajinomoto Co., Inc. (Tokyo, Japan) are conducting a collaborative research project on the profile of plasma free amino acids among patients with pancreatic cancer, and this project is approved by the ethical commitees. This project is funded by Ajinomoto Co., Inc. and employees of the company are joining the project as co-investigators. The funder provided support in the form of salaries for the employees but does not play any additional role in the study design, data collection or analysis, decision to publish, or preparation of the manuscript.
References
- 1.Rawla P., Sunkara T., Gaduputi V. Epidemiology of Pancreatic Cancer: Global Trends, Etiology and Risk Factors. World J. Oncol. 2019;10:10–27. doi: 10.14740/wjon1166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Matsubayashi H., Ishiwatari H., Sasaki K., Uesaka K., Ono H. Detecting Early Pancreatic Cancer: Current Problems and Future Prospects. Gut Liver. 2020;14:30–36. doi: 10.5009/gnl18491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Suh S., Kim K.W. Diabetes and Cancer: Cancer Should Be Screened in Routine Diabetes Assessment. Diabetes Metab. J. 2019;43:733–743. doi: 10.4093/dmj.2019.0177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Everhart J., Wright D. Diabetes mellitus as a risk factor for pancreatic cancer. A meta-analysis. JAMA. 1995;273:1605–1609. doi: 10.1001/jama.1995.03520440059037. [DOI] [PubMed] [Google Scholar]
- 5.Jee S.H., Ohrr H., Sull J.W., Yun J.E., Ji M., Samet J.M. Fasting serum glucose level and cancer risk in Korean men and women. JAMA. 2005;293:194–202. doi: 10.1001/jama.293.2.194. [DOI] [PubMed] [Google Scholar]
- 6.Hassan M.M., Bondy M.L., Wolff R.A., Abbruzzese J.L., Vauthey J.N., Pisters P.W., Evans D.B., Khan R., Chou T.H., Lenzi R., et al. Risk factors for pancreatic cancer: Case-control study. Am. J. Gastroenterol. 2007;102:2696–2707. doi: 10.1111/j.1572-0241.2007.01510.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Liao W.C., Tu Y.K., Wu M.S., Lin J.T., Wang H.P., Chien K.L. Blood glucose concentration and risk of pancreatic cancer: Systematic review and dose-response meta-analysis. BMJ. 2015;350:g7371. doi: 10.1136/bmj.g7371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pannala R., Leibson C.L., Rabe K.G., Timmons L.J., Ransom J., de Andrade M., Petersen G.M., Chari S.T. Temporal association of changes in fasting blood glucose and body mass index with diagnosis of pancreatic cancer. Am. J. Gastroenterol. 2009;104:2318–2325. doi: 10.1038/ajg.2009.253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ben Q., Xu M., Ning X., Liu J., Hong S., Huang W., Zhang H., Li Z. Diabetes mellitus and risk of pancreatic cancer: A meta-analysis of cohort studies. Eur. J. Cancer. 2011;47:1928–1937. doi: 10.1016/j.ejca.2011.03.003. [DOI] [PubMed] [Google Scholar]
- 10.Nagai M., Murakami Y., Tamakoshi A., Kiyohara Y., Yamada M., Ukawa S., Hirata T., Tanaka S., Miura K., Ueshima H., et al. Fasting but not casual blood glucose is associated with pancreatic cancer mortality in Japanese: EPOCH-JAPAN. Cancer Causes Control. 2017;28:625–633. doi: 10.1007/s10552-017-0884-0. [DOI] [PubMed] [Google Scholar]
- 11.Harding J.L., Shaw J.E., Peeters A., Cartensen B., Magliano D.J. Cancer risk among peaple with type 1 and type 2 diabetes: Disentangling true associations, detection bias, and reverse causation. Diabetes Care. 2015;38:264–270. doi: 10.2337/dc14-1996. [DOI] [PubMed] [Google Scholar]
- 12.Stevens R.J., Roddam A.W., Veral V. Pancreatic cancer in type 1 and young-onset diabetes: Systematic review and meta-analysis. Br. J. Cancer. 2007;96:507–509. doi: 10.1038/sj.bjc.6603571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chari S.T., Leibson C.L., Rabe K.G., Timmons L.J., Ransom J., de Andrade M., Petersen G.M. Pancreatic cancer-associated diabetes mellitus: Prevalence and temporal association with diagnosis of cancer. Gastroenterology. 2008;134:95–101. doi: 10.1053/j.gastro.2007.10.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pannala R., Leirness J.B., Bamlet W.R., Basu A., Petersen G.M., Chari S.T. Prevalence and clinical profile of pancreatic cancer-associated diabetes mellitus. Gastroenterology. 2008;134:981–987. doi: 10.1053/j.gastro.2008.01.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.American Diabetes Association Diagnosis and classification of diabetes. Diabetes Care. 2011;34:S62–S69. doi: 10.2337/dc11-S062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ben Q., Cai Q., Li Z., Yuan Y., Ning X., Deng S., Wang K. The relationship between new-onset diabetes mellitus and pancreatic cancer risk: A case-control study. Eur. J. Cancer. 2011;47:248–254. doi: 10.1016/j.ejca.2010.07.010. [DOI] [PubMed] [Google Scholar]
- 17.Liao K.F., Lai S.W., Li C.I., Chen W.C. Diabetes mellitus correlates with increased risk of pancreatic cancer: A population-based cohort study in Taiwan. J. Gastroenterol. Hepatol. 2012;27:709–713. doi: 10.1111/j.1440-1746.2011.06938.x. [DOI] [PubMed] [Google Scholar]
- 18.Aggarwal G., Rabe K.G., Petersen G.M., Chari S.T. New-onset diabetes in pancreatic cancer: A study in the primary care setting. Pancreatology. 2012;12:156–161. doi: 10.1016/j.pan.2012.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mizuno S., Nakai Y., Isayama H., Takahara N., Miyabayashi K., Yamamoto K., Kawakubo K., Mohri D., Kogure H., Sasaki T., et al. Diabetes is a useful diagnostic clue to improve the prognosis of pancreatic cancer. Pancreatology. 2013;13:285–289. doi: 10.1016/j.pan.2013.03.013. [DOI] [PubMed] [Google Scholar]
- 20.Aggarwal G., Kamada P., Chari S.T. Prevalence of diabetes mellitus in pancreatic cancer compared to common cancers. Pancreas. 2013;42:198–201. doi: 10.1097/MPA.0b013e3182592c96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Setiawan V.W., Stram D.O., Porcel J., Chari S.T., Maskarinec G., Le Marchand L., Wilkens L.R., Haiman C.A., Pandol S.J., Monroe K.R. Pancreatic Cancer Following Incident Diabetes in African Americans and Latinos: The Multiethnic Cohort. J. Natl. Cancer Inst. 2019;111:27–33. doi: 10.1093/jnci/djy090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tada M., Kawabe T., Arizumi M., Togawa O., Matsubara S., Yamamoto N., Nakai Y., Sasahira N., Hirano K., Tsujino T., et al. Pancreatic cancer in patients with pancreatic cystic lesions: A prospective study in 197 patients. Clin. Gastroenterol. Hepatol. 2006;4:1265–1270. doi: 10.1016/j.cgh.2006.07.013. [DOI] [PubMed] [Google Scholar]
- 23.Kawakubo K., Tada M., Isayama H., Sasahira N., Nakai Y., Yamamoto K., Kogure H., Sasaki T., Hirano K., Ijichi H., et al. Incidence of extrapancreatic malignancies in patients with intraductal papillary mucinous neoplasms of the pancreas. Gut. 2011;60:1249–1253. doi: 10.1136/gut.2010.227306. [DOI] [PubMed] [Google Scholar]
- 24.Oyama H., Tada M., Takagi K., Tateishi K., Hamada T., Nakai Y., Hakuta R., Ijichi H., Ishigaki K., Kanai S., et al. Long-term Risk of Malignancy in Branch-Duct Intraductal Papillary Mucinous Neoplasms. Gastroenterology. 2020;158:226–237. doi: 10.1053/j.gastro.2019.08.032. [DOI] [PubMed] [Google Scholar]
- 25.Kleeff J., Korc M., Apte M., La Vecchia C., Johnson C.D., Biankin A.V., Neale R.E., Tempero M., Tuveson D.A., Hruban R.H., et al. Pancreatic cancer. Nat. Rev. Dis. Primers. 2016;2:16022. doi: 10.1038/nrdp.2016.22. [DOI] [PubMed] [Google Scholar]
- 26.Capurso G., Boccia S., Salvia R., Del Chiaro M., Frulloni L., Arcidiacono P.G., Zerbi A., Manta R., Fabbri C., Ventrucci M., et al. Risk factors for intraductal papillary mucinous neoplasm (IPMN) of the pancreas: A multicentre case-control study. Am. J. Gastroenterol. 2013;108:1003–1009. doi: 10.1038/ajg.2013.42. [DOI] [PubMed] [Google Scholar]
- 27.Mizuno S., Isayama H., Nakai Y., Yoshikawa T., Ishigaki K., Matsubara S., Yamamoto N., Ijichi H., Tateishi K., Tada M., et al. Prevalence of Pancreatic Cystic Lesions Is Associated With Diabetes Mellitus and Obesity: An Analysis of 5296 Individuals Who Underwent a Preventive Medical Examination. Pancreas. 2017;46:801–805. doi: 10.1097/MPA.0000000000000833. [DOI] [PubMed] [Google Scholar]
- 28.Morales-Oyarvide V., Mino-Kenudson M., Ferrone C.R., Sahani D.V., Pergolini I., Negreros-Osuna A.A., Warshaw A.L., Lillemoe K.D., Fernandez-Del Castillo C. Diabetes mellitus in intraductal papillary mucinous neoplasm of the pancreas is associated with high-grade dysplasia and invasive carcinoma. Pancreatology. 2017;17:920–926. doi: 10.1016/j.pan.2017.08.073. [DOI] [PubMed] [Google Scholar]
- 29.Gausman V., Kandel P., Van Riet P.A., Moris M., Kayal M., Do C., Poneros J.M., Sethi A., Gress F.G., Schrope B.A., et al. Predictors of Progression Among Low-Risk Intraductal Papillary Mucinous Neoplasms in a Multicenter Surveillance Cohort. Pancreas. 2018;47:471–476. doi: 10.1097/MPA.0000000000001027. [DOI] [PubMed] [Google Scholar]
- 30.Yoshioka T., Shigekawa M., Ikezawa K., Tamura T., Sato K., Urabe M., Sueyoshi H., Yamai T., Suda T., Sakamori R., et al. Risk Factors for Pancreatic Cancer and the Necessity of Long-Term Surveillance in Patients With Pancreatic Cystic Lesions. Pancreas. 2020;49:552–560. doi: 10.1097/MPA.0000000000001521. [DOI] [PubMed] [Google Scholar]
- 31.Pergolini I., Jager C., Safak O., Goss R., Novotny A., Ceyhan G.O., Friess H., Demir I.E. Diabetes and Weight Loss Are Associated With Malignancies in Patients With Intraductal Papillary Mucinous Neoplasms. Clin. Gastroenterol. Hepatol. 2020 doi: 10.1016/j.cgh.2020.04.090. [DOI] [PubMed] [Google Scholar]
- 32.Wiesenauer C.A., Schmidt C.M., Cummings O.W., Yiannoutsos C.T., Howard T.J., Wiebke E.A., Goulet R.J., Jr., McHenry L., Sherman S., Lehman G.A., et al. Preoperative predictors of malignancy in pancreatic intraductal papillary mucinous neoplasms. Arch. Surg. 2003;138:610–618. doi: 10.1001/archsurg.138.6.610. [DOI] [PubMed] [Google Scholar]
- 33.Lubezky N., Ben-Haim M., Nakache R., Lahat G., Blachar A., Brazowski E., Santo E., Klausner J.M. Clinical presentation can predict disease course in patients with intraductal papillary mucinous neoplasm of the pancreas. World J. Surg. 2010;34:126–132. doi: 10.1007/s00268-009-0269-y. [DOI] [PubMed] [Google Scholar]
- 34.Duconseil P., Adham M., Sauvanet A., Autret A., Perinel J., Chiche L., Mabrut J.Y., Tuech J.J., Mariette C., Turrini O. Fukuoka-Negative Branch-Duct IPMNs: When to Worry? A Study from the French Surgical Association (AFC) Ann. Surg. Oncol. 2018;25:1017–1025. doi: 10.1245/s10434-017-6318-0. [DOI] [PubMed] [Google Scholar]
- 35.Jan I.S., Chang M.C., Yang C.Y., Tien Y.W., Jeng Y.M., Wu C.H., Chen B.B., Chang Y.T. Validation of Indications for Surgery of European Evidence-Based Guidelines for Patients with Pancreatic Intraductal Papillary Mucinous Neoplasms. J. Gastrointest. Surg. 2019 doi: 10.1007/s11605-019-04420-9. [DOI] [PubMed] [Google Scholar]
- 36.Pelaez-Luna M., Takahashi N., Fletcher J.G., Chari S.T. Resectability of presymptomatic pancreatic cancer and its relationship to onset of diabetes: A retrospective review of CT scans and fasting glucose values prior to diagnosis. Am. J. Gastroenterol. 2007;102:2157–2163. doi: 10.1111/j.1572-0241.2007.01480.x. [DOI] [PubMed] [Google Scholar]
- 37.Chari S.T., Leibson C.L., Rabe K.G., Ransom J., de Andrade M., Petersen G.M. Probability of pancreatic cancer following diabetes: A population-based study. Gastroenterology. 2005;129:504–511. doi: 10.1016/j.gastro.2005.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Munigala S., Singh A., Gelrud A., Agarwal B. Predictors for Pancreatic Cancer Diagnosis Following New-Onset Diabetes Mellitus. Clin. Transl. Gastroenterol. 2015;6:e118. doi: 10.1038/ctg.2015.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ogawa Y., Tanaka M., Inoue K., Yamaguchi K., Chijiiwa K., Mizumoto K., Tsutsu N., Nakamura Y. A prospective pancreatographic study of the prevalence of pancreatic carcinoma in patients with diabetes mellitus. Cancer. 2002;94:2344–2349. doi: 10.1002/cncr.10493. [DOI] [PubMed] [Google Scholar]
- 40.Damiano J., Bordier L., Le Berre J.P., Margery J., Dupuy O., Mayaudon H., Bauduceau B. Should pancreas imaging be recommended in patients over 50 years when diabetes is discovered because of acute symptoms? Diabetes Metab. 2004;30:203–207. doi: 10.1016/S1262-3636(07)70111-8. [DOI] [PubMed] [Google Scholar]
- 41.Illes D., Terzin V., Holzinger G., Kosar K., Roka R., Zsori G., Abraham G., Czako L. New-onset type 2 diabetes mellitus --A high-risk group suitable for the screening of pancreatic cancer? Pancreatology. 2016;16:266–271. doi: 10.1016/j.pan.2015.12.005. [DOI] [PubMed] [Google Scholar]
- 42.Lee J.H., Kim S.A., Park H.Y., Lee K.H., Lee K.T., Lee J.K., Bae J.C., Kim K.W. New-onset diabetes patients need pancreatic cancer screening? J. Clin. Gastroenterol. 2012;46:e58–e61. doi: 10.1097/MCG.0b013e318238348c. [DOI] [PubMed] [Google Scholar]
- 43.Mizuno S., Nakai Y., Isayama H., Yanai A., Takahara N., Miyabayashi K., Yamamoto K., Kawakubo K., Mohri D., Kogure H., et al. Risk factors and early signs of pancreatic cancer in diabetes: Screening strategy based on diabetes onset age. J. Gastroenterol. 2013;48:238–246. doi: 10.1007/s00535-012-0622-z. [DOI] [PubMed] [Google Scholar]
- 44.Bo X., Shi J., Liu R., Geng S., Li Q., Li Y., Jin H., Yang S., Jiang H., Wang Z. Using the Risk Factors of Pancreatic Cancer and Their Interactions in Cancer Screening: A Case-Control Study in Shanghai, China. Ann. Glob. Health. 2019;85 doi: 10.5334/aogh.2463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.La Torre G., Sferrazza A., Gualano M.R., de Waure C., Clemente G., De Rose A.M., Nicolotti N., Nuzzo G., Siliquini R., Boccia A., et al. Investigating the synergistic interaction of diabetes, tobacco smoking, alcohol consumption, and hypercholesterolemia on the risk of pancreatic cancer: A case-control study in Italy. Biomed. Res. Int. 2014;2014:481019. doi: 10.1155/2014/481019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Sun L., Wang X., Gu T., Hu B., Luo J., Qin Y., Wan C. Nicotine triggers islet β cell senescence to facilitate the progression of type 2 diabetes. Toxicology. 2020;441:152502. doi: 10.1016/j.tox.2020.152502. [DOI] [PubMed] [Google Scholar]
- 47.Lowenfels A.B., Maisonneuve P. Epidemiology and prevention of pancreatic cancer. Jpn. J. Clin. Oncol. 2004;34:238–344. doi: 10.1093/jjco/hyh045. [DOI] [PubMed] [Google Scholar]
- 48.Chowdhury P., MacLeod S., Udupa K.B., Rayford P.L. Pathophysiological effects of nicotine on the pancreas: An update. Exp. Biol. Med. 2002;227:445–454. doi: 10.1177/153537020222700708. [DOI] [PubMed] [Google Scholar]
- 49.Hart P.A., Kamada P., Rabe K.G., Srinivasan S., Basu A., Aggarwal G., Chari S.T. Weight loss precedes cancer-specific symptoms in pancreatic cancer-associated diabetes mellitus. Pancreas. 2011;40:768–772. doi: 10.1097/MPA.0b013e318220816a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Mueller A.M., Meier C.R., Jick S.S., Schneider C. Weight change and blood glucose concentration as markers for pancreatic cancer in subjects with new-onset diabetes mellitus: A matched case-control study. Pancreatology. 2019;19:578–586. doi: 10.1016/j.pan.2019.03.006. [DOI] [PubMed] [Google Scholar]
- 51.Huang B.Z., Pandol S.J., Jeon C.Y., Chari S.T., Sugar C.A., Chao C.R., Zhang Z.F., Wu B.U., Wendy Setiawan V. New-Onset Diabetes, Longitudinal Trends in Metabolic Markers, and Risk of Pancreatic Cancer in a Heterogeneous Population. Clin. Gastroenterol. Hepatol. 2019;18:1812–1821. doi: 10.1016/j.cgh.2019.11.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Dong X., Lou Y.B., Mu Y.C., Kang M.X., Wu Y.L. Predictive Factors for Differentiating Pancreatic Cancer-Associated Diabetes Mellitus from Common Type 2 Diabetes Mellitus for the Early Detection of Pancreatic Cancer. Digestion. 2018;98:209–216. doi: 10.1159/000489169. [DOI] [PubMed] [Google Scholar]
- 53.Boursi B., Finkelman B., Giantonio B.J., Haynes K., Rustgi A.K., Rhim A.D., Mamtani R., Yang Y.X. A Clinical Prediction Model to Assess Risk for Pancreatic Cancer among Patients With New-Onset Diabetes. Gastroenterology. 2017;152:840–850.e3. doi: 10.1053/j.gastro.2016.11.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Sharma A., Kandlakunta H., Nagpal S.J.S., Feng Z., Hoos W., Petersen G.M., Chari S.T. Model to Determine Risk of Pancreatic Cancer in Patients With New-Onset Diabetes. Gastroenterology. 2018;155:730–739. doi: 10.1053/j.gastro.2018.05.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Chen W., Butler R.K., Lustigova E., Chari S.T., Wu B.U. Validation of the Enriching New-Onset Diabetes for Pancreatic Cancer Model in a Diverse and Integrated Healthcare Setting. Dig. Dis. Sci. 2020 doi: 10.1007/s10620-020-06139-z. [DOI] [PubMed] [Google Scholar]
- 56.Permert J., Larsson J., Westermark G.T., Herrington M.K., Christmanson L., Pour P.M., Westermark P., Adrian T.E. Islet amyloid polypeptide in patients with pancreatic cancer and diabetes. N. Engl. J. Med. 1994;330:313–318. doi: 10.1056/NEJM199402033300503. [DOI] [PubMed] [Google Scholar]
- 57.Chari S.T., Klee G.G., Miller L.J., Raimondo M., DiMagno E.P. Islet amyloid polypeptide is not a satisfactory marker for detecting pancreatic cancer. Gastroenterology. 2001;121:640–645. doi: 10.1053/gast.2001.27210. [DOI] [PubMed] [Google Scholar]
- 58.Grote V.A., Kaaks R., Nieters A., Tjonneland A., Halkjaer J., Overvad K., Skjelbo Nielsen M.R., Boutron-Ruault M.C., Clavel-Chapelon F., Racine A., et al. Inflammation marker and risk of pancreatic cancer: A nested case-control study within the EPIC cohort. Br. J. Cancer. 2012;106:1866–1874. doi: 10.1038/bjc.2012.172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Shi W., Qiu W., Wang W., Zhou X., Zhong X., Tian G., Deng A. Osteoprotegerin is up-regulated in pancreatic cancers and correlates with cancer-associated new-onset diabetes. Biosci. Trends. 2014;8:322–326. doi: 10.5582/bst.2014.01092. [DOI] [PubMed] [Google Scholar]
- 60.Huang H., Dong X., Kang M.X., Xu B., Chen Y., Zhang B., Chen J., Xie Q.P., Wu Y.L. Novel blood biomarkers of pancreatic cancer-associated diabetes mellitus identified by peripheral blood-based gene expression profiles. Am. J. Gastroenterol. 2010;105:1661–1669. doi: 10.1038/ajg.2010.32. [DOI] [PubMed] [Google Scholar]
- 61.Kang M., Qin W., Buya M., Dong X., Zheng W., Lu W., Chen J., Guo Q., Wu Y. VNN1, a potential biomarker for pancreatic cancer-associated new-onset diabetes, aggravates paraneoplastic islet dysfunction by increasing oxidative stress. Cancer Lett. 2016;373:241–250. doi: 10.1016/j.canlet.2015.12.031. [DOI] [PubMed] [Google Scholar]
- 62.Tamahashi U., Kumagai J., Takizawa T., Sekine M., Eishi Y. Expression and intracellular localization of matrix metalloproteinases in intraductal papillary mucinous neoplasms of the pancreas. Virchows Arch. 2008;453:79–87. doi: 10.1007/s00428-008-0617-6. [DOI] [PubMed] [Google Scholar]
- 63.Moz S., Basso D., Padoan A., Bozzato D., Fogar P., Zambon C.F., Pelloso M., Sperti C., Vigili de Kreutzenberg S., Pasquali C., et al. Blood expression of matrix metalloproteinases 8 and 9 and of their inducers S100A8 and S100A9 supports diagnosis and prognosis of PDAC-associated diabetes mellitus. Clin. Chim. Acta. 2016;456:24–30. doi: 10.1016/j.cca.2016.02.018. [DOI] [PubMed] [Google Scholar]
- 64.Suzuki H., Li Y., Dong X., Hassan M.M., Abbruzzese J.L., Li D. Effect of insulin-like growth factor gene polymorphisms alone or in interaction with diabetes on the risk of pancreatic cancer. Cancer Epidemiol. Biomark. Prev. 2008;17:3467–3473. doi: 10.1158/1055-9965.EPI-08-0514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Kishikawa T., Otsuka M., Ohno M., Yoshikawa T., Takata A., Koike K. Circulating RNAs as new biomarkers for detecting pancreatic cancer. World J. Gastroenterol. 2015;21:8527–8540. doi: 10.3748/wjg.v21.i28.8527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Dai X., Pang W., Zhou Y., Yao W., Xia L., Wang C., Chen X., Zen K., Zhang C.Y., Yuan Y. Altered profile of serum microRNAs in pancreatic cancer-associated new-onset diabetes mellitus. J. Diabetes. 2016;8:422–433. doi: 10.1111/1753-0407.12313. [DOI] [PubMed] [Google Scholar]
- 67.Miyagi Y., Higashiyama M., Gochi A., Akaike M., Ishikawa T., Miura T., Saruki N., Bando E., Kimura H., Imamura F., et al. Plasma free amino acid profiling of five types of cancer patients and its application for early detection. PLoS ONE. 2011;6:e24143. doi: 10.1371/journal.pone.0024143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Ihata Y., Miyagi E., Numazaki R., Muramatsu T., Imaizumi A., Yamamoto H., Yamakado M., Okamoto N., Hirahara F. Amino acid profile index for early detection of endometrial cancer: Verification as a novel diagnostic marker. Int. J. Clin. Oncol. 2014;19:364–372. doi: 10.1007/s10147-013-0565-2. [DOI] [PubMed] [Google Scholar]
- 69.Fukutake N., Ueno M., Hiraoka N., Shimada K., Shiraishi K., Saruki N., Ito T., Yamakado M., Ono N., Imaizumi A., et al. A Novel Multivariate Index for Pancreatic Cancer Detection Based On the Plasma Free Amino Acid Profile. PLoS ONE. 2015;10:e0132223. doi: 10.1371/journal.pone.0132223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Mizuno S., Isayama H., Nakai Y., Ishigaki K., Saito K., Sato T., Takeda T., Hakuta R., Saito T., Takahara N., et al. Diagnostic yield of the plasma free amino acid index for pancreatic cancer in patients with diabetes mellitus. Pancreatology. 2019;19:695–698. doi: 10.1016/j.pan.2019.07.002. [DOI] [PubMed] [Google Scholar]
- 71.Menni C., Fauman E., Erte I., Perry J.R., Kastenmuller G., Shin S.Y., Petersen A.K., Hyde C., Psatha M., Ward K.J., et al. Biomarkers for type 2 diabetes and impaired fasting glucose using a nontargeted metabolomics approach. Diabetes. 2013;62:4270–4276. doi: 10.2337/db13-0570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Roberts L.D., Koulman A., Griffin J.L. Towards metabolic biomarkers of insulin resistance and type 2 diabetes: Progress from the metabolome. Lancet Diabetes Endocrinol. 2014;2:65–75. doi: 10.1016/S2213-8587(13)70143-8. [DOI] [PubMed] [Google Scholar]
- 73.Maitra A., Sharma A., Brand R.E., Van Den Eeden S.K., Fisher W.E., Hart P.A., Hughes S.J., Mather K.J., Pandol S.J., Park W.G., et al. A prospective study to establish a new-onset diabetes cohort: From the consortium for the study of chronic pancreatitis, diabetes, and pancreatic cancer. Pancreas. 2018;47:1244–1248. doi: 10.1097/MPA.0000000000001169. [DOI] [PMC free article] [PubMed] [Google Scholar]