Abstract
Introduction
Since February 2020, the outbreak of COVID-19 in Italy has forced the health care system to undergo profound rearrangements in its services and facilities, especially in the worst-hit areas in Northern Italy. In this setting, inpatient and outpatient services had to rethink and reorganize their activities to meet the needs of patients during the “lockdown”. The Italian Association of Myology developed a survey to estimate the impact of these changes on patients affected by neuromuscular disorders and on specialized neuromuscular centers during the acute phase of COVID-19 pandemic.
Methods
We developed an electronic survey that was sent to neuromuscular centers affiliated with the Italian Association of Myology, assessing changes in pharmacological therapies provision, outpatient clinical and instrumental services, support services (physiotherapy, nursing care, psychological support) and clinical trials.
Results
40% of surveyed neuromuscular centers reported a reduction in outpatient visit and examinations (44.5% of centers in Northern regions; 25% of centers in Central regions; 50% of centers in Southern regions). Twenty-two% of centers postponed in-hospital administration of therapies for neuromuscular diseases (23.4% in Northern regions; 13.0% in Central regions; 20% in Southern regions). Diagnostic and support services (physiotherapy, nursing care, psychological support) were suspended in 57% of centers (66/43/44% in Northern, Central and Southern centers respectively) Overall, the most affected services were rehabilitative services and on-site outpatient visits, which were suspended in 93% of centers. Strategies adopted by neuromuscular centers to overcome these changes included maintaining urgent on-site visits, addressing patients to available services and promoting remote contact and telemedicine.
Conclusions
Overall, COVID-19 pandemic resulted in a significant disruption of clinical and support services for patients with neuromuscular diseases. Despite the efforts to provide telemedicine consults to patients, this option could be promoted and improved further. A close collaboration between the different neuromuscular centers and service providers as well as further implementation of telehealth platforms are necessary to ensure quality care to NMD patients in the near future and in case of recurrent pandemic waves.
Key words: SARS-CoV-2, COVID-19, neuromuscular diseases, myopathies, neuropathies, myastenia gravis, neuromuscular services
Introduction
Italy has been one of the first countries, after China, facing cases of local interhuman transmissions of severe acute respiratory syndrome-coronavirus-2 (SARS-CoV-2 infection) worldwide 1,2. The first confirmed case of coronavirus disease-2019 (COVID-19) was reported in Italy on the 21st of February 2020. Since then, more than 233.000 individuals across Italy became infected 1. To assist COVID-19 patients, territorial health care services were reorganized and some hospitals were converted into “COVID hubs” (appointed by authorities), particularly in the most affected areas. Moreover, general population was imposed strict preventative measures to limit unnecessary gatherings and movements. Despite national laws and guidelines, regional differences in the management of the crisis exist 3-7. In this emergency setting, providing services to patients with chronic diseases and disability represented a major issue for the health care system 8. Due to preventive home isolation, fragile patients and their caregivers had to face many problems in terms of diagnosis, therapy, rehabilitation and support.
Neuromuscular diseases (NMD) may represent a risk factor causing a more severe course and outcome of SARS-CoV-2 infection. Indeed, several factors may contribute, namely respiratory and cardiac involvement, which are common NMD complications, muscle weakness, disability and, in some cases, dependency from caregivers 9-11. The discontinuation of care and treatments can worsen the underlying condition, exacerbate symptoms, and increase anxiety, leading to a vicious circle and increased management concerns 12-16. Health services tried to address these needs by promoting remote patient contacts, referring patients to available nearby services and offering on-site visits only for urgent cases. Across the country, specialized NMD centers devoted their efforts and shared their knowledge in order to ensure quality care for NMD patients during these dramatic and unusual months, under the guidance of the Italian Association of Myology (AIM).
AIM associates developed a survey to quantify the extent of changes experienced by NMD centers and patients during these months, and to outline the most effective solutions undertaken, with the ultimate goal of improving NMD patients’ care.
Methods
Study design
We designed a cross-sectional study based on a multicentric survey (Appendix 1).
The period considered in the survey runs from February 23rd to April 30th 2020, i.e. the most acute phase of the pandemic in Italy. Thirty-seven referral Centers for Neuromuscular Diseases were enrolled. The questionnaire was sent via e-mail to members of the AIM responsible for the enrolled centers. Geographical areas were divided into three macro-areas: Northern Italy, comprising the regions Valle d’Aosta, Piedmont, Liguria, Lombardy, Veneto, Trentino, Friuli Venezia Giulia, Emilia Romagna; Central Italy, including Tuscany, Lazio, Marche, Umbria; Southern Italy accounting for Abruzzi, Molise, Campania, Apulia, Calabria, Basilicata, Sicily and Sardinia.
Setting and participants
The survey included questions addressing how the activity of the center and clinical practice had changed and which services reported the worst difficulties from February 23rd, 2020 to April 30th, 2020. The questionnaire was divided into five sections:
Center and neurologist identification information;
Access of patients to standard home pharmacological therapy;
Access of patients to hospital-administered pharmacological treatments, including Nusinersen, intravenous immunoglobulins (IVIG), intravenous corticosteroids, rituximab, enzyme replacement therapy (ERT) for Pompe disease, plasma exchange (PLEX), edaravone and others;
Management of clinical trials;
Management of care-related services such as physiotherapy, home nurse service, psychological support for the patient and the caregiver, prenatal diagnosis.
Results
Thirty Italian Neuromuscular Centers completed the survey: 18/20 centers from Northern Italy, (response rate – r.r. 90%); 8/10 centers from Central Italy (r.r. 80%); 4/7 centers from South Italy, (r.r. 57%). Four centers were exclusively dedicated to the pediatric population (2 in Northern Italy and 2 in Central Italy), while 26 assisted both pediatric and adult patients. Regional differences in the impact of COVID-19 epidemic emerged, partly as a consequence of the different geographical viral spread. The impact on activities and services provided by Neuromuscular Center on the national territory is summarized in Table I.
Table I.
Impact on activities and services provided by Neuromuscular Center on the national territory (yes: performed; no: not performed; DH: Day Hospital drug administration; FKT: physiokinesitherapy).
| Outpatient visit and exams | Therapy | Services | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | DH | Chronic home therapy | Clinical trials | Total | FKT | Psychological support | Home nursing service | Prenatal diagnosis | |||
| Italy | Yes | 16.7% | 64% | 39% | 93.3% | 63% | 43% | 7% | 66.7% | 33% | 87.5% |
| No | 40.% | 22% | 7% | 3.4% | 37% | 57% | 93% | 33.3% | 67% | 12.5% | |
| Partial | 43.3% (urgencies only) |
14% | 54% (some) |
3.3% (some) |
|||||||
| North | Yes | 11% | 63.6% | 41% | 89% | 63% | 34% | 0% | 84% | 20% | 77.5% |
| No | 44.5% | 23.4% | 12% | 5.5% | 37% | 66% | 100% | 16% | 80% | 22.5% | |
| Partial | 44.5% (urgencies only) |
13% | 47% (some) |
5.5% (some) |
|||||||
| Center | Yes | 0% | 73% | 43% | 100% | 76% | 57% | 12.5% | 50% | 87.5% | 100% |
| No | 25% | 13% | 0% | 0% | 24% | 43% | 87.5% | 50% | 12.5% | 0% | |
| Partial | 75% (urgencies only) |
13% | 57% (some) |
||||||||
| South | Yes | 0% | 60% | 25% | 100% | 62% | 56% | 20% | 50% | 75% | 100% |
| No | 50% | 20% | 0% | 0% | 38% | 44% | 80% | 50% | 25% | 0% | |
| Partial | 50% (urgencies only) |
20% | 75% (some) |
||||||||
Outpatient visit and exams
From February 20th, 2020, a marked reduction in both outpatient visits and exams was observed in all Italian Neuromuscular Centers. Only 16.7% of centers all over the country continued to provide in-hospital visits and 43.3% of them limited the visits to medical emergencies and urgencies (Fig. 1). However, neuromuscular specialists were generally available on-call for neurological emergencies and a substantial part of the planned visits were replaced by remote telephone contact. In Northern Italy, the worst-hit area, 44.5% of centers were not able to provide outpatient visits and instrumental procedures, while in Central and Southern Italy outpatient visits were not performed in 25 and 50% of centers respectively. Cancelled visits were delayed or replaced with remote contact in the same proportion. The 75% of pediatric-dedicated centers guaranteed outpatients visits and exams.
Figure 1.
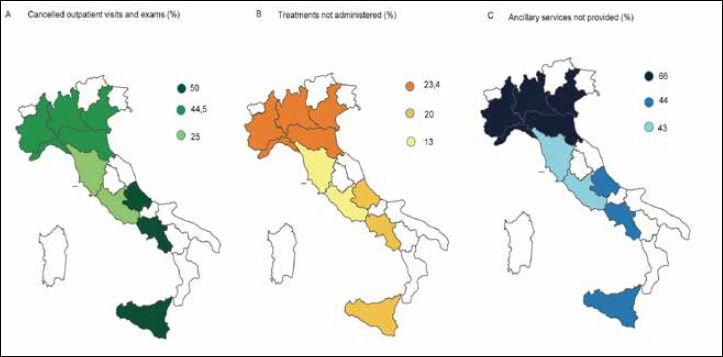
Geographical distribution of the impact of COVID-19 on the activity of NMD centers in Italy. The figure displays the percentage of outpatient visits and exams, treatments and ancillary services that have not been performed in three different part of Italy. Panel A shows that percentages of visits and exams that have been cancelled within the considered time interval in Northern, Central and Southern Italy. Panel B and C highlight the bigger impact of COVID-19 pandemic on treatment administration and ancillary services in Northern Italy than in the other parts of the country.
Therapy administration and availability
Overall therapeutic pharmacological provisions (chronic pharmacological treatments, in-hospital administered therapies, experimental therapies) were guaranteed in 64% of interviewed centers (Fig. 1).
Chronic outpatient treatments remained available for the majority of patients (93.3% of Italian centers and the totality of the exclusively-pediatric centers).
Neuromuscular patients in regular clinical practice often refer to specialized centers for day-hospital (DH) treatments, particularly for intravenous drug administration. In this regard, 38% of centers provided in-hospital therapeutic administration without changes and 50% of centers with minor changes in Northern Italy. In Central and Southern Italy this service was mostly provided without major interruptions, but some difficulties were reported by 57 and 75% of centers in Central and Southern regions respectively.
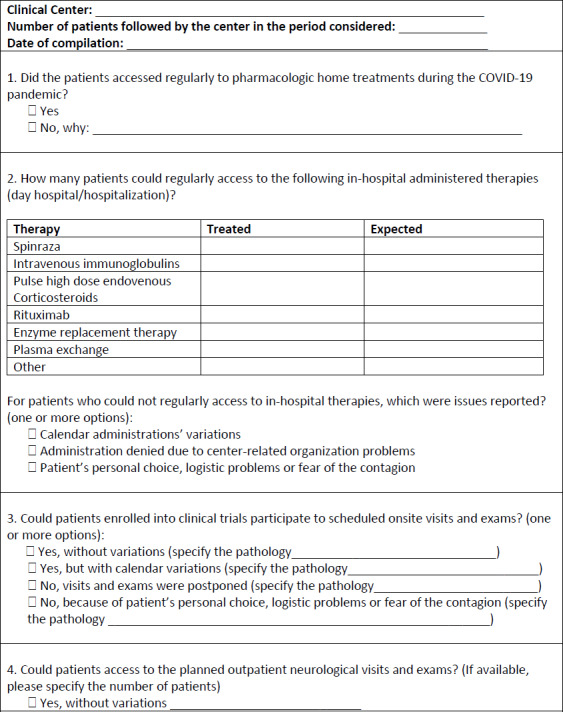
We analyzed effectively performed DH treatments. Pulse high dose intravenous corticosteroids were administered in 94% of scheduled patients, while Intravenous Immunoglobulins (IVIG) administrations were provided in 74% of planned patients. Conversely, the monoclonal antibody Rituximab was administered only in 53% of expected cases. Referral centers for Nusinersen succeeded in 77% of scheduled administrations. In centers providing these treatments, Edaravone was administered in 98% of programmed patients, while ERT was maintained in 87% of patients with Pompe disease. Conversely, plasma exchange was performed in a higher number of patients than expected (Fig. 2).
Figure 2.

In-hospital administered therapy versus expected. Percentage of patients who received in-hospital administered therapies in the worse-hit period compared to the scheduled administrations for Nusinersen, IVIG, pulse high dose intravenous corticosteroids, Rituximab, ERT for Pompe disease, Edaravone and PLEX.
The most relevant changes in treatment administration in this period were those for myasthenia gravis, followed by those affected with neuropathies, spinal muscular atrophy (SMA), amyotrophic lateral sclerosis (ALS), inflammatory and metabolic myopathies. Two centers referred their patients (with a diagnosis of myasthenia gravis, ALS, SMA and Pompe disease) to other institutions for the prosecution of treatment.
The reasons why patients did not receive in-hospital therapy administration were mainly related to personal decisions, e.g. fear of the contagion. In most cases, pharmacological in-hospital treatments were postponed or rearranged, while, in few cases, drug administration was temporarily interrupted due to the high risk for the patient to develop serious COVID-19 complications in case of infection.
Clinical trials
Clinical trials continued with scheduled visits and exams in 63% of centers, with a minor percentage of interruptions in the regions of Central Italy. Reasons for interruption were logistic problems, safety issues and patients’ fear of contagion.
Experimental trials involving ALS and Pompe disease faced greater difficulties. As regards ALS patients, 60% of trial-related visits were delayed or cancelled for precautionary reasons. Patients with Pompe disease did not undergo visits and exams in 50% of cases.
Conversely, more than 75% of the centers participating in clinical trials for other neuromuscular diseases, including myasthenia gravis, inflammatory myopathies and neuropathies, DMD and SMA, performed the scheduled visits and exams with only minor lags. Particularly, visits and exams scheduled for clinical trials were conducted in the 87.5% of pediatric-dedicated centers.
Services
Services provided by neuromuscular centers, such as rehabilitation, home care nursing, psychological support and prenatal diagnosis, faced a reduction in 57% of centers, showing higher reduction rates in geographical areas with higher numbers of SARS-CoV-2 cases (aggregate services reduction in 66% of Northern NMD centers, 43% of Central centers and 44% of Southern centers) (Fig. 1). The most affected service was rehabilitation, since physical therapy sessions were suspended in 93% of centers, and postponed or delayed in a minor number of centers due to patient-related travel problems. Indeed, only 7% of surveyed centers reported that physical therapy sessions continued without variations (all Northern centers faced the interruption of sessions, while 12.5% of Central centers and 20% of Southern centers maintained the service).
Despite some difficulties, psychological support to families was provided in 66.7% of centers upon request.
Home nursing care service was not provided in 67% of centers, with a higher reduction rate in Northern Italy regions, where only 20% of expected patients obtained regular assistance. Also, session duration was reduced. The suspension was mainly determined by a choice of the families to protect their relatives from external contacts.
Services associated to prenatal diagnosis remained accessible in 87.5% of centers providing this service, in some cases with minor delays.
Fifty% of pediatric-dedicated centers reduced physiotherapy and home care nursing, while no center reported any defection in psychological support and prenatal diagnosis services.
Discussion
During the first wave of COVID-19 pandemic, Italian health care system had to rapidly and heavily reorganize inpatient and outpatient services, particularly in the worst-hit areas 3,6,17,18. In this setting, specialized NMD centers were no exception. Under the guidance of AIM, they tried to address the needs of fragile NMD patients and to maintain essential services. However, despite these common intents, many NMD patients suffered from home isolation and temporary interruption of a part of outpatient visits and exams, thus struggling to receive standard therapies and rehabilitative sessions and facing the risk of worsening of their disease or exacerbation of symptoms 7,19.
With this survey, AIM aimed to assess the impact of SARS-CoV-2 pandemic on NMD centers and NMD patients’ care in Italy. We found that changes related to the pandemic partly followed the regional burden of infections across Italy. Centers in Northern Italy experienced a heavier reduction of inpatient therapy administration and ancillary services if compared to NMD centers in Central and Southern Italy. On the other hand, outpatient neurological visits and exams suffered from a marked reduction in Southern regions. Concerning these results, however, we acknowledge the possibility of a sampling bias, since centers from Southern regions were less represented.
From the survey, it emerged that most centers ensured in-hospital visits for urgent cases and tried to limit the worsening of NMD diseases through remote contact advice. Provision of chronic pharmacological therapy was unaffected, whereas many centers faced difficulties in the administration of in-hospital therapies. Particularly, rituximab and IVIG were the most challenging to deliver appropriately, and patients who suffered the greatest change in in-hospital treatment delivery were myasthenia gravis patients. Indeed, patients with auto-immune and inflammatory NMD receiving immunosuppressive treatment generally present a higher risk of complications from infectious diseases 14,20. Thus, treatments might have been cancelled in order to let these patients avoid unnecessary travels.
Furthermore, the pandemic partially affected the regular course of clinical trials as well. Scheduled visits and exams were performed without major problems and with the necessary precautions only in 63% of centers.
Ancillary services such as rehabilitation, home care nursing and psychological support were markedly affected nation-wide. Due to the additional risk of infection from close patient-therapist contact 21, rehabilitation services were generally suspended. Remote physiotherapy was not provided, possibly because of the difficulties experienced by disabled patients and their caregivers in conducting physical sessions without support. Home nursing care was provided in a higher number of cases as compared to physical therapy, despite the risks deriving from close contact with operators being similar. Psychological support for patients and caregiver was generally available, since it could be provided through remote contact. Finally, services related to prenatal diagnosis were accessible in most centers. Exclusively-pediatric centers deserve a further comment, since their activity resulted less affected and services were generally maintained throughout the pandemic; however, rehabilitative activities requiring personal contact were reduced and extra-regional travels were avoided. This is partly due to an effort of the Health Care System to guarantee assistance to little fragile patients. Moreover, we hypothesize that buildings and spaces dedicated to pediatric population was less involved in the conversion to assist COVID-19 patients.
This cross-sectional, multicentric study was the first to specifically address the issues experienced by NMD patients in our country and to provide a picture of the pandemic burden for NMD specialists in different regions. Limitations of the study include the fact that we depicted the pandemic burden during a reduced time span, in a rapidly developing context in terms of preventative measures, organizational settings and law framework. A further limitation consists in the different restrictive measures applied regionally that may have led to a heterogeneous impact on the access to care for NMD patients.
In addition to the abovementioned sampling bias, methodological limitations associated to the survey itself could be the adhesion bias, as centers volunteering for the study might not represent a uniform sample, and the referral bias, as centers which encountered problems might have been more prone to answer promptly. On the other hand, centers heavily involved in the emergency might have experienced difficulties in answering the survey due to lack of time. Nonetheless, surveys are an effective tool to rapidly gather information without direct in-person contacts. In addition, our survey reached a consistent part of NMD centers across Italy.
Overall, COVID-19 pandemic caused a public health crisis with a potentially severe impact on the most fragile part of our society – including many NMD patients. In this context, neuromuscular centers played a pivotal role in ensuring an adequate support and care to these patients, and to reach this aim they had to rapidly reorganize their services. Some of the strategies and innovations that were experimented, such as telemedicine, could prove useful in the nearby future, after the acute phase of the pandemic 22, and deserve diffusion and standardization for their use in clinical practice. Surveys, at-distance meetings and virtual platforms will likely be valuable tools to help addressing the future concerns and challenges of NMD centers, aiming at maintaining the best standards of care for NMD patients in these difficult times.
Ethic statement
The survey has been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Financial support
No targeted funding reported.
Figures and tables
Acknowledgment
This work is generated within the European Reference Network for Neuromuscular Diseases. We gratefully acknowledge Italian Ministry of Health Ricerca Corrente 2020.
List of abbreviations
- AIM
Italian Association of Myology
- ALS
amyotrophic lateral sclerosis
- COVID-19
Corona Virus Disease 19
- DH
Day Hospital
- DMD
Duchenne Muscular dystrophy
- ERT
enzyme replacement therapy
- IVIG
intravenous immunoglobulins
- NMDs
neuromuscular diseases
- PLEX
plasma exchange
- SARS
severe acute respiratory syndrome
- SMA
spinal muscular atrophy
Appendix 1
Italian Association of Myology
Survey on the impact of the COVID-19 pandemic on the management of neuromuscular patients from 24/2/2020-30/4/2020
References
- 1.WHO. Coronavirus disease 2019 (COVID-19) situation report, May 2020. [Google Scholar]
- 2.Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study [published correction appears in Lancet 2020;395:1054-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fagiuoli S, Lorini FL, Remuzzi G, Covid-19 Bergamo Hospital Crisis Unit Adaptations and lessons in the Province of Bergamo. N Engl J Med 2020;NEJMc2011599 https://doi.org/10.1056/NEJMc2011599 [Epub ahead of print] 10.1056/NEJMc2011599 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Anelli F, Leoni G, Monaco R, et al. Italian doctors call for protecting healthcare workers and boosting community surveillance during COVID-19 outbreak. BMJ 2020;368:m1254 https://doi.org/10.1136/bmj.m1254 10.1136/bmj.m1254 [DOI] [PubMed] [Google Scholar]
- 5.Bassetti M, Giacobbe DR, Aliberti S, et al. Balancing evidence and frontline experience in the early phases of the COVID-19 pandemic: current position of the Italian Society of Anti-Infective Therapy (SITA) and the Italian Society of Pulmonology (SIP). Clin Microbiol Infect 2020;S1198-743X(20)30257-3 https://doi.org/10.1016/j.cmi.2020.04.031 10.1016/j.cmi.2020.04.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rizzi M, Castelli F, Latronico N, et al. SARS-CoV-2 invades the West. How to face a COVID-19 epidemic in Lombardy, Northern Italy? Infez Med 2020;28:133-4. [PubMed] [Google Scholar]
- 7.Lazzerini M, Barbi E, Apicella A, et al. Delayed access or provision of care in Italy resulting from fear of COVID-19. Lancet Child Adolesc Health 2020;4:e10-1. https://doi.org/10.1016/S2352-4642(20)30108-5 10.1016/S2352-4642(20)30108-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Silvestris N, Moschetta A, Paradiso A, et al. COVID-19 Pandemic and the crisis of health systems: the experience of the Apulia Cancer Network and of the Comprehensive Cancer Center Istituto Tumori “Giovanni Paolo II” of Bari. Int J Environ Res Public Health 2020;17:E2763 https://doi.org/10.3390/ijerph17082763 10.3390/ijerph17082763 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Guidon AC, Amato AA. COVID-19 and neuromuscular disorders. Neurology 2020; April 13 [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 10.Veerapandiyan A, Wagner KR, Apkon S, et al. The care of patients with Duchenne, Becker, and other muscular dystrophies in the COVID-19 pandemic. Muscle Nerve 2020;10.1002/mus.26902. https://doi.org/10.1002/mus.26902 [Epub ahead of print] 10.1002/mus.26902 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Veerapandiyan A, Connolly AM, Finkel RS, et al. Spinal muscular atrophy care in the COVID-19 pandemic era. Muscle Nerve 2020;10.1002/mus.26903. https://doi.org/10.1002/mus.26903 [Epub ahead of print] 10.1002/mus.26903 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Damian MS. COVID-19 and people with neuromuscular disorders: World Muscle Society position and advice. Executive Board of the WMS 4th Update www.worldmusclesociety.org
- 13.Jacob S, Muppidi S, Guidon A, et al. Guidance for the management of myasthenia gravis (MG) and Lambert-Eaton myasthenic syndrome (LEMS) during the COVID-19 pandemic. J Neurol Sci 2020. https://doi.org/10.1016/j.jns.2020.116803 10.1016/j.jns.2020.116803 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gummi RR, Kukulka NA, Deroche CB, et al. Factors associated with acute exacerbations of myasthenia gravis. Muscle Nerve 2019. https://doi.org/10.1002/mus.26689 10.1002/mus.26689 [DOI] [PubMed] [Google Scholar]
- 15.de Girolamo G, Cerveri G, Clerici M, et al. Mental Health in the coronavirus disease 2019 emergency – the Italian response. JAMA Psychiatry 2020;10.1001/jamapsychiatry.2020.1276. https://doi.org/10.1001/jamapsychiatry.2020.1276 10.1001/jamapsychiatry.2020.1276 [DOI] [PubMed] [Google Scholar]
- 16.Lippi G, Henry BM, Bovo C, et al. Health risks and potential remedies during prolonged lockdowns for coronavirus disease 2019 (COVID-19). Diagnosis (Berl) 2020;7:85-90. https://doi.org/10.1515/dx-2020-0041 10.1515/dx-2020-0041 [DOI] [PubMed] [Google Scholar]
- 17.Spina S, Marrazzo F, Migliari M, et al. The response of Milan’s emergency medical system to the COVID-19 outbreak in Italy. Lancet 2020;395:e49-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nacoti M, Ciocca A, Giupponi A, et al. At the epicenter of the Covid-19 pandemic and humanitarian crises in Italy: changing perspectives on preparation and mitigation. NEJM Catalyst Innovations in Care Delivery 2020;3:1-5. [Google Scholar]
- 19.Motta Zanin G, Gentile E, Parisi A, et al. A Preliminary Evaluation of the public risk perception related to the COVID-19 health emergency in Italy. Int J Environ Res Public Health 2020;17:e3024 https://doi.org/10.3390/ijerph17093024 10.3390/ijerph17093024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Onder G, Rezza G, Brusaferro S. Case-fatality rate and characteristics of patients dying in relation to COVID-19 in Italy. JAMA. 2020;10.1001/jama.2020.4683. https://doi.org/10.1001/jama.2020.4683 10.1001/jama.2020.4683 [DOI] [PubMed] [Google Scholar]
- 21.Boldrini P, Bernetti A, Fiore P, SIMFER Executive Committee and SIMFER Committee for international affairs Impact of COVID-19 outbreak on rehabilitation services and Physical and Rehabilitation Medicine (PRM) physicians’ activities in Italy. An official document of the Italian PRM Society (SIMFER). Eur J Phys Rehabil Med 2020;10.23736/S1973-9087.20.06256-5. https://doi.org/10.23736/S1973-9087.20.06256-5 [Epub ahead of print] 10.23736/S1973-9087.20.06256-5 [DOI] [PubMed] [Google Scholar]
- 22.Cohen BH, Busis NA, Ciccarelli L. Coding in the world of COVID-19: non-face-to-face evaluation and management care. Continuum (Minneap Minn) 2020;26:1-25. [DOI] [PubMed] [Google Scholar]


