1.
The COVID‐19 pandemic is one of the greatest public heath challenges of the last century. This is a virulent and contagious virus which has spread rapidly across the globe, causing severe illness and widespread social and economic disruptions. Given the massive toll of the current pandemic, there is an urgent need for research on all aspects of the virus and its spread, including the impact of demographic characteristics, biological factors, and pre‐existing medical conditions on the risk of infection and subsequent development of complications. The spread and severity of the current pandemic are rooted in the underlying political, morbidity, and mortality patterns that exist in different regions and countries of the world.
The epidemiological transition is a model for long‐term shifts in population mortality rates that are tied to economic and demographic changes and is described in terms of four stages: (a) pestilence and famine, (b) receding pandemics, (c) degenerative and man‐made diseases, and (d) delayed degenerative diseases (Olshansky & Ault, 1986; Omran, 1971). The stage of pestilence and famine is characterized by large swings in mortality rates that follow infectious disease epidemics and famine conditions, while the stage of receding pandemics is characterized by increases in life expectancy, largely due to lower mortality rates at young ages brought about curbing the spread of infectious disease and by stabilizing the food supply. The age of degenerative and lifestyle diseases is characterized by further increases in life expectancy brought about by shifting the mortality burden to older ages with a shift to noncommunicable diseases (NCDs) as major causes of death. Finally, the age of delayed degenerative diseases is characterized by improved prevention and the treatment of NCDs, leading to lower mortality rates, especially during older age.
Figure 1 presents age‐adjusted death rates for heart disease, stroke, cancer, and influenza and pneumonia from 1900 to 2017 in the United States (Bastian, Tejada Vera, Arias, et al., 2019). With the exception of the spike of influenza and pneumonia deaths in 1918 associated with the Spanish Flu pandemic, a clear transition is seen between 1900 and the 1970's where chronic disease mortality (heart disease, stroke, and cancer) is increasing while deaths from influenza and pneumonia continue to decrease over time. Finally, the period of delayed degenerative diseases is also apparent from 1980 to present day, with decreasing death rates from NCDs, especially for heart disease and stroke.
FIGURE 1.
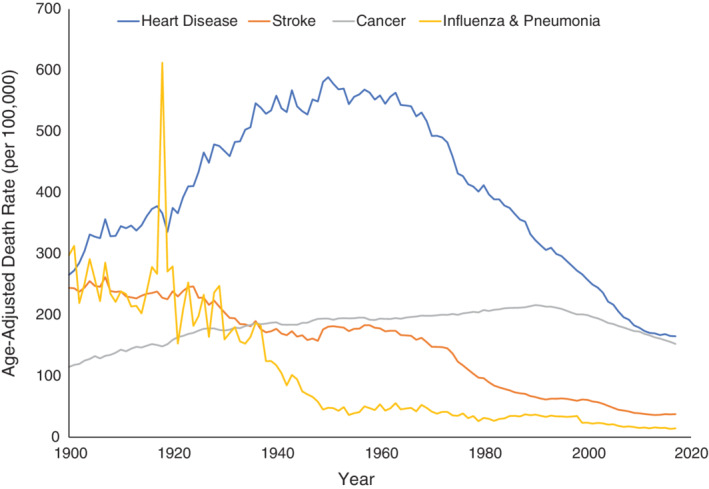
Major causes of death, United States, 1900 to 2017
Within the context of epidemiological transition, theories of nutritional and physical activity transitions have sought to explain how changes related to lifestyle have occurred in parallel with the increasing prevalence of obesity and NCDs (Katzmarzyk & Mason, 2009; Popkin, 2004; Popkin, Adair, & Ng, 2012). While overall life expectancy has continued to increase in the United States, the disease burden associated with obesity and related conditions such as type 2 diabetes continues to increase. Recent estimates indicate that 37.7% of the US adults have obesity (Hales, Fryar, Carroll, Freedman, & Ogden, 2018), while 13% have type 2 diabetes (Centers for Disease Control and Prevention, 2020). It has been suggested that obesity is a major contributor to the slowing of the increase in life expectancy in the United States (Olshansky et al., 2005).
Life expectancy at birth increased in the United States from 47.3 years in 1900 to 78.6 years in 2017 (Arias & Xu, 2019); however, there remain significant racial disparities (National Center for Health Statistics, 2018). In 2014, non‐Hispanic African Americans could expect to live 3.6 years less than White Americans and 6.6 years less than Hispanic Americans under current mortality patterns (Arias, 2016). A total of 51% and 64% of this racial gap in life expectancy between White and African Americans in men and women, respectively, can be explained by differences in mortality rates from diabetes, cardiovascular disease, and cancer (Harper, Lynch, Burris, & Davey Smith, 2007). Furthermore, the national prevalence estimates for obesity among Non‐Hispanic African Americans (39.9%) and Hispanics (34.1%) are significantly higher than in Whites (29.9%) in the United States (Centers for Disease Control and Prevention et al., 2020). Thus, it is clear that efforts to reduce racial disparities in health should focus on understanding and reducing disparities in NCD incidence and mortality, in addition to underlying health conditions such as obesity.
Thus, the United States and other high‐income countries are at a stage of epidemiological transition where the major causes of mortality stem from NCDs such as cardiovascular disease and cancer, and significant health disparities exist in these conditions. Globally, countries are at different stages and are proceeding through the epidemiological transition at different rates; however, 80% of deaths from NCDs now occur in low‐ and middle‐income countries (World Health Organization, 2005).
Given the current state of epidemiological transition in the United States and in other high‐income countries, our health systems have evolved to treat and manage the high prevalence of NCDs, while less focus has been placed on infectious disease epidemiology. It is within this public health environment that a very contagious infectious virus (SARS‐CoV‐2) and associated disease (COVID‐19) emerged in the spring of 2020. The COVID‐19 pandemic presents a monumental challenge for public health. Given the rapid spread of COVID‐19 in the population, there is an urgent need to better understand all aspects of the SARS‐CoV‐2 virus and its transmission, including the impact of demographic factors (age, sex, race, etc.), biological factors, and pre‐existing medical conditions on the risk of infection and development of complications. As described above, the health framework in the United States and many other countries are layered with health inequities.
There is also evidence that older adults and African Americans are at increased risk of developing complications that require hospitalization compared to younger adults and White Americans, respectively (Braithwaite & Warren, 2020; Price‐Haywood, Burton, Fort, & Seoane, 2020; Richardson et al., 2020). Early clinical evidence suggest that pre‐existing conditions such as type 2 diabetes, hypertension, and obesity increase the risk and severity of complications associated with COVID‐19 (Garg et al., 2020; Kalligeros et al., 2020; Lighter et al., 2020; Richardson et al., 2020; Simonnet et al., 2020). Taken together, a perfect storm was in place to fuel a public health disaster.
Within the context of epidemiological and nutritional transitions, the current obesity epidemic is the result of long‐term excess of caloric intake over expenditure at the population level. Obesity appears to be a key underlying disease related to the progression of COVID‐19 severity. Reports from France indicate that higher body mass index (BMI) was associated with an increased risk of requiring invasive mechanical ventilation among COVID‐19 patients (Simonnet et al., 2020) and that the prevalence of obesity was significantly higher in critical COVID‐19 patients in the ICU compared to the general population of Lyon (Caussy et al., 2020). Two reports from China also showed that patients with obesity (defined according to Asian/Chinese specific BMI cut‐offs) had a significantly higher odds (OR = 3.40; 95% CI: 1.40‐2.86 and OR = 2.91; 95% CI: 1.31‐6.47) of developing severe COVID‐19 compared to normal weight patients (Cai et al., 2020; Gao et al., 2020). Data from a large academic health center in New York City showed that among patients under the age of 60 years, those with a BMI ≥35 kg/m2 had a significantly higher odds (OR = 3.6; 95% CI: 2.5‐5.3) of being hospitalized compared those with a lower BMI (Lighter et al., 2020). Additional data from New York City showed that BMI ≥40 kg/m2 was associated with an increased risk of mortality in both younger (OR 5.1; 95% CI: 2.3‐11.1) and older (OR 1.6; 95% CI: 1.2‐2.3) COVID‐19 patients, although the odds was higher among the younger patients (Klang et al., 2020). Finally, data from a cohort of 3481 COVID‐19 patients in Louisiana presented a significantly increased risk of hospitalization among African American COVID‐19 patients compared to white patients (OR = 1.96; 95% CI: 1.62‐2.37) and also among those with obesity (OR = 1.43; 95% CI: 1.20‐1.71) compared to those without obesity (Price‐Haywood et al., 2020). Thus, the weighted evidence suggests that obesity is a significant factor in the development of severe COVID‐19 complications and mortality. However, the degree to which the presence of obesity and chronic conditions explain these sex and race differences in rates of SARS‐COV‐2 infection is currently unknown.
Human genetic predisposition may also play a role in COVID‐19, conceivably affecting either function or regulation of expression of relevant genes, and consequently influencing disease incidence or severity, or both. The SARS‐CoV‐2 virus uses Angiotensin Converting Enzyme 2 (ACE2) as a receptor and docking station to attach to cells (Zhou et al., 2020). Viral entry into the cell requires proteolytic processing of the viral S protein, which can be performed at the cell surface by the protease TMPRSS2, or alternatively in the lysosome by the proteases Cathepsin B or Cathepsin L (Hoffmann et al., 2020). Further viral replication relies on specific proteins encoded by viral genomic RNA. Viral release triggers the adaptive immune system, and it has been observed that the severe and life‐threatening form of COVID‐19 is often accompanied by a “cytokine storm”—a situation where humoral communication between different components of the adaptive as well as the innate immune system gets out of control, to the point where the body cannot mount an efficient defense against the virus any longer (Tisoncik et al., 2012; Zheng et al., 2020). Key players in this cytokine storm are the pro‐inflammatory cytokines TNF, IL1B, IL6, the anti‐inflammatory cytokine IL10 which might lead to immune system paralysis when produced in excess, and the pro‐inflammatory chemokines CXCL10 and CCL2. Finally, parallel to the cytokine storm, genes mediating antibody‐dependent disease enhancement, specifically FCGR2A and FCGR2B (Li et al., 2019; Verbeek, Hirose, & Nishimura, 2019), are also potential candidates where genetic variation may affect disease progression. The degree to which genetic variation in these potential mechanisms of disease progression may vary according to obesity and/or race and ethnicity are not currently known.
In conclusion, we are facing a multi‐faceted syndemic of COVID‐19, obesity and NCDs which has fueled the global pandemic. African Americans and patients with obesity and other chronic underlying conditions are at particularly high risk of developing severe COVID‐19 complications and should be considered high‐risk patients. A better understanding of the mechanisms associated with this increased risk is required to be better prepared to respond to future infectious disease epidemics. Recent events have highlighted that although we face public health threats from obesity and NCDs on a daily basis, we must remain prepared to face serious infectious disease threats—either from novel agents, or from old foes that will exploit weaknesses in our health systems associated with diminished health capacity and health disparities. The COVID‐19 pandemic has brought renewed focus on deeply entrenched health disparities which must be addressed to improve the health of the entire population.
AUTHOR CONTRIBUTIONS
Peter Katzmarzyk: Conceptualization; writing‐original draft; writing‐review and editing. Michael Salbaum: Writing‐original draft; writing‐review and editing. Steven Heymsfield: Writing‐review and editing.
Katzmarzyk PT, Salbaum JM, Heymsfield SB. Obesity, noncommunicable diseases, and COVID‐19: A perfect storm. Am J Hum Biol. 2020;32:e23484. 10.1002/ajhb.23484
REFERENCES
- Arias, E. (2016). Changes in life expectancy by race and Hispanic origin in the United States, 2013–2014. Hyattsville, MD: National Center for Health Statistics; (NCHS data brief, no 244). [PubMed] [Google Scholar]
- Arias, E. , & Xu, J. (2019). United States life tables, 2017. Hyattsville, MD: National Center for Health Statistics. [PubMed] [Google Scholar]
- Bastian, B. , Tejada Vera, B. , Arias, E. , et al. (2019). Mortality trends in the United States, 1900–2017. Hyattsville, MD: National Center for Health Statistics. https://www.cdc.gov/nchs/data-visualization/mortality-trends/index.htm. [Google Scholar]
- Braithwaite, R. , & Warren, R. (2020). The African American petri dish. J Health Care Poor Underserv, 32, 2 (Epub ahead of print). [DOI] [PubMed] [Google Scholar]
- Cai, Q. , Chen, F. , Wang, T. , Luo, F. , Liu, X. , Wu, Q. , … Xu, L. (2020). Obesity and COVID‐19 severity in a designated hospital in Shenzhen, China. Diabetes Care, 43, 1392–1398. [DOI] [PubMed] [Google Scholar]
- Caussy, C. , Pattou, F. , Wallet, F. , Simon, C. , Chalopin, S. , Telliam, C. , et al. (2020). Prevalence of obesity among adult inpatients with COVID‐19 in France. Lancet Diabetes Endocrinol, 8(9), 562–564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention . (2020). National diabetes statistics report 2020. Atlanta, GA: Centers for Disease Control and Prevention, Department of Health and Human Services. [Google Scholar]
- Centers for Disease Control and Prevention , National Center for Chronic Disease Prevention and Health Promotion , & Division of Population Health . (2020). BRFSS prevalence & trends data. Retrieved from https://www.cdc.gov/brfss/brfssprevalence/.
- Gao, F. , Zheng, K. I. , Wang, X. B. , Sun, Q. F. , Pan, K. H. , Wang, T. Y. , … Zheng, M. H. (2020). Obesity is a risk factor for greater COVID‐19 severity. Diabetes Care, 43, E72–E74. [DOI] [PubMed] [Google Scholar]
- Garg, S. , Kim, L. , Whitaker, M. , O'Halloran, A. , Cummings, C. , Holstein, R. , … Fry, A. (2020). Hospitalization rates and characteristics of patients hospitalized with laboratory‐confirmed coronavirus disease 2019—COVID‐NET, 14 states, March 1–30, 2020. MMWR. Morbidity and Mortality Weekly Report, 69, 458–464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hales, C. M. , Fryar, C. D. , Carroll, M. D. , Freedman, D. S. , & Ogden, C. L. (2018). Trends in obesity and severe obesity prevalence in US youth and adults by sex and age, 2007‐2008 to 2015‐2016. JAMA, 319, 1723–1725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harper, S. , Lynch, J. , Burris, S. , & Davey Smith, G. (2007). Trends in the black‐white life expectancy gap in the United States, 1983‐2003. JAMA, 297, 1224–1232. [DOI] [PubMed] [Google Scholar]
- Hoffmann, M. , Kleine‐Weber, H. , Schroeder, S. , Kruger, N. , Herrler, T. , Erichsen, S. , et al. (2020). SARS‐CoV‐2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell, 181, 271–280e278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalligeros, M. , Shehadeh, F. , Mylona, E. K. , Benitez, G. , Beckwith, C. G. , Chan, P. A. , & Mylonakis, E. (2020). Association of obesity with disease severity among patients with COVID‐19. Obesity, 28(7), 1200–1204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katzmarzyk, P. T. , & Mason, C. (2009). The physical activity transition. Journal of Physical Activity & Health, 6, 269–280. [DOI] [PubMed] [Google Scholar]
- Klang, E. , Kassim, G. , Soffer, S. , Freeman, R. , Levin, M. A. , & Reich, D. L. (2020). Morbid obesity as an independent risk factor for COVID‐19 mortality in hospitalized patients younger than 50. Obesity Advance Online Publication May 24, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li, S. S. , Gilbert, P. B. , Carpp, L. N. , Pyo, C. W. , Janes, H. , Fong, Y. , et al. (2019). Fc gamma receptor polymorphisms modulated the vaccine effect on HIV‐1 risk in the HVTN 505 HIV vaccine trial. J Virol, 93(21), e02041–e02018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lighter, J. , Phillips, M. , Hochman, S. , Sterling, S. , Johnson, D. , Francois, F. , & Stachel, A. (2020). Obesity in patients younger than 60 years is a risk factor for Covid‐19 hospital admission. Clin Infect Dis (Advance online publication April 9, 2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Center for Health Statistics . (2018). Health, United States. Hyattsville, MD: US Department of Health and Human Services. [Google Scholar]
- Olshansky, S. J. , & Ault, A. B. (1986). The fourth stage of the epidemiologic transition: The age of delayed degenerative diseases. The Millbank Quarterly, 64, 355–391. [PubMed] [Google Scholar]
- Olshansky, S. J. , Passaro, D. J. , Hershow, R. C. , Layden, J. , Carnes, B. A. , Brody, J. , … Ludwig, D. S. (2005). A potential decline in life expectancy in the United States in the 21st century. The New England Journal of Medicine, 352, 1138–1145. [DOI] [PubMed] [Google Scholar]
- Omran, A. R. (1971). The epidemiologic transition. A theory of the epidemiology of population change. The Milbank Memorial Fund Quarterly, 49, 509–538. [PubMed] [Google Scholar]
- Popkin, B. M. (2004). The nutrition transition: An overview of world patterns of change. Nutrition Reviews, 62(7) Pt 2, S140–S143. [DOI] [PubMed] [Google Scholar]
- Popkin, B. M. , Adair, L. S. , & Ng, S. W. (2012). Global nutrition transition and the pandemic of obesity in developing countries. Nutrition Reviews, 70, 3–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Price‐Haywood, E. G. , Burton, J. , Fort, D. , & Seoane, L. (2020). Hospitalization and mortality among black patients and white patients with Covid‐19. The New England Journal of Medicine, 382, 2534–2543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richardson, S. , Hirsch, J. S. , Narasimhan, M. , Crawford, J. M. , McGinn, T. , Davidson, K. W. , et al. (2020). Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID‐19 in the New York City area. JAMA, 323, 2052–2059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simonnet, A. , Chetboun, M. , Poissy, J. , Raverdy, V. , Noulette, J. , Duhamel, A. , … Verkindt, H. (2020). High prevalence of obesity in severe acute respiratory syndrome coronavirus‐2 (SARS‐CoV‐2) requiring invasive mechanical ventilation. Obesity, 28, 1195–1199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tisoncik, J. R. , Korth, M. J. , Simmons, C. P. , Farrar, J. , Martin, T. R. , & Katze, M. G. (2012). Into the eye of the cytokine storm. Microbiology and Molecular Biology Reviews, 76, 16–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verbeek, J. S. , Hirose, S. , & Nishimura, H. (2019). The complex association of FcgammaRIIb with autoimmune susceptibility. Frontiers in Immunology, 10, 2061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . (2005). Preventing chronic disease: A vital investment. WHO Global Report. WHO, Geneva.
- Zheng, H. Y. , Zhang, M. , Yang, C. X. , Zhang, N. , Wang, X. C. , Yang, X. P. , … Zheng, Y. T. (2020). Elevated exhaustion levels and reduced functional diversity of T cells in peripheral blood may predict severe progression in COVID‐19 patients. Cellular & Molecular Immunology, 17, 541–543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou, P. , Yang, X. L. , Wang, X. G. , Hu, B. , Zhang, L. , Zhang, W. , et al. (2020). A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature, 579(7798), 270–273. [DOI] [PMC free article] [PubMed] [Google Scholar]


