Abstract
Introduction
Australia has fortunately had a low prevalence coronavirus disease 2019 (COVID‐19), and our healthcare system has not been overwhelmed. We aimed to determine whether, despite this, a decline in acute stroke presentations, imaging and intervention occurred during the pandemic at a busy stroke centre.
Methods
The number of ‘code stroke’ activations, multimodal CTs and endovascular clot retrievals (ECRs) performed during the pandemic period (3/1/2020–5/10/2020) at a large comprehensive stroke centre was compared against the pre‐pandemic period (3/1/2019–1/31/2019) using Z‐statistics. Year‐on‐year comparison of the number of patients with large vessel occlusions (LVOs) and ECRs performed per month was also made.
Results
The number of ‘code stroke’ activations and patients undergoing multimodal CT per month decreased significantly (P < 0.0025) following lockdown on 29th March. The number of ECRs also decreased (P = 0.165). The nadir in the weekly number of CTs coincided with lockdown and the peak of new COVID‐19 cases. The number of patients with LVOs and ECRs increased by 15% and 14%, respectively, in March but decreased by 55% and 48%, respectively, in April.
Conclusions
The significant decrease in volume of ‘code stroke’ activations and acute stroke imaging following lockdown was accompanied by a concomitant decrease in patients with LVOs and ECRs. The decrease in imaging was therefore not driven purely by patients with mild strokes and stroke mimics, but also included those with severe strokes. Since Australia had a low prevalence of COVID‐19, this observed decrease cannot be attributed to hospital congestion and is instead likely driven by patient fear.
Keywords: ‘Code Stroke’, COVID‐19, endovascular clot retrieval, imaging, stroke
Introduction
Coronavirus disease 2019 (COVID‐19) has had a disruptive effect on healthcare systems around the world. Since March, when the disease entered a pandemic phase, contingency plans have been implemented in healthcare systems and hospitals around the world, including the deferral of elective medical procedures. 1 , 2 , 3 These changes to clinical operations were aimed at creating capacity and preserving resources so that hospitals could deal with a projected surge in COVID‐19 patients while continuing to care for patients with other acute medical conditions necessitating treatment. However, there is emerging evidence from media 4 and the scientific literature 5 , 6 , 7 , 8 that the volume of patients receiving care for emergent and time‐sensitive conditions has also decreased.
Acute ischaemic stroke (AIS), a leading cause of morbidity and mortality, is a time‐critical emergency. Endovascular clot retrieval (ECR) is now the standard of care treatment for AIS patients with intracranial large vessel occlusions (LVOs) up to 24 hours of onset. 9 It has been shown to decrease disability and improve outcomes. 10 , 11 , 12 Imaging, including non‐invasive angiography, is recommended by guidelines in the work‐up of AIS patients who present within the ECR window to identify those with LVOs who may benefit from treatment. 9 During the COVID‐19 pandemic, emergency guidance from the American Stroke Association and Australian Stroke Coalition has been to continue providing evidence based stroke treatment, including ECR. 13 , 14 Yet a recent analysis reported an approximately 40% decrease in the volume of patients who underwent acute stroke imaging across 856 hospitals in the United States. 6 At a comprehensive stroke centre in Barcelona, which is at the heart of a region severely affected by the pandemic and where 60% of bed capacity was occupied by COVID‐19 patients, the number of stroke admissions and ECRs performed reduced by a quarter. 7 France, another nation that has been hit hard by the pandemic, also experienced a significant decrease in the number of ECRs performed. 8 The decline in patients receiving care for AIS in these European settings was postulated to be due to saturation of emergency medical services, including emergency transport system capacity, during the crisis. 7 , 8
In comparison with the United States, France and Catalonia, which were the focus of previous analyses of the collateral effects of the pandemic on stroke imaging and care, Australia has had a low prevalence of COVID‐19. 7 , 8 , 15 Our emergency transport services and hospitals have not been overwhelmed. The purpose of this investigation is therefore to share insights into the impact of the pandemic on stroke imaging and intervention from the lens of a high volume comprehensive stroke centre in Australia (>200 ECRs per year), where service was not disrupted by a surge in COVID‐19 patients. The volume of ‘code stroke’ presentations and acute stroke imaging was assessed. We also looked at the number of patients with a radiologically confirmed LVO and the number of ECRs performed during and prior to the pandemic. The aim was to test the hypothesis that any decrease in volume of stroke presentations during the pandemic was driven by a reduction in the number of patients coming to hospital with mild strokes and stroke mimics.
Methods
Data source
This study was performed at Monash Health, a network of hospitals with 3 emergency departments (EDs), which serves as one of two major comprehensive stroke centres in the second most populous state (population 6.4 million) of Australia. The state is divided into two catchments, one for each major comprehensive stroke centre. Emergency services adhere strictly to these when transferring stroke patients, including from other hospitals. The other major comprehensive stroke centre is more than 40 km away for the vast majority of patients in our catchment, who are therefore unlikely to self‐present there. No changes were made to the availability and emergent access to acute stroke imaging and endovascular treatment for eligible patients during the pandemic.
Data from our institution were reviewed for this retrospective study. Specifically, via our Radiological Information System (RIS) and Picture Archiving and Communication System (PACS), we determined the number of multimodal CTs (consisting of non‐enhanced CT, CT angiography [CTA], and CT perfusion [CTP]) performed for a ‘code stroke’ work‐up per week for the period from 1 March 2019 to 10 May 2020. For the same period, we assessed via our hospital’s records the number of ‘code stroke’ activations per month on patients who had presented to our hospital directly through our emergency departments (including via emergency transport). The total number of ED presentations was also assessed. The number of ECRs performed in eligible patients per month was also determined by querying the database of our neuro‐interventional service. For each patient who underwent ECR, whether they were transferred from another hospital or presented directly to our emergency department was recorded, as well as the time between presentation and multimodal CT (Door‐to‐CT time), a key performance metric of stroke imaging. The multimodal stroke CTs of patients were assess by two readers (J.M. and S.A.) for the presence of an LVO. The number of patients with an LVO, as well as the percentage of patients undergoing multimodal stroke CT who had an LVO, was also determined.
This study was approved by our institutions’ IRB which waived the requirement for informed consent due to the retrospective study design and anonymization of all data.
Data analysis and statistics
For Australia, the period from 1 March 2019 to 31 January 2020 was deemed the pre‐pandemic period since it preceded the announcement of a 14‐day ban for non‐citizens arriving from China. Triggered by the first Australian COVID‐19 fatality on March 1, the period from 1 March 2020 to 10 May 2020 was considered the pandemic period while February was considered a transition month. Other notable timepoints in Australia were as follows: (i) all international travel banned for Australians (17 March 2020); (ii) strict social distancing of 4 sqm/person mandated (20 March 2020); (iii) Australian border closure (25 March 2020); and (iv) public gathering of more than two people banned with a stay at home rule imposed (29 March 2020 – ongoing).
The pre‐pandemic period was deemed the baseline relative to which we compared the pandemic period. Z‐statistics were used to determine whether the number of ‘code stroke’ activations, multimodal CTs and ECRs were significantly different from the pre‐pandemic mean. Statistical analyses were performed using a dedicated software written in Python. A P‐value < 0.0025, corresponding to a z‐score > 2.8, was considered significant, indicating there is only a 0.25% chance that the value falls within the fluctuation distribution of the pre‐pandemic baseline. To test for the correlation between pre‐pandemic baseline patient numbers and corresponding normal scores, the Shapiro–Wilk test was used.
To address seasonal or holiday‐related changes, we also reviewed 2019/20 year‐on‐year changes in patient numbers for the two pandemic months of March and April and four pre‐pandemic months of November to January.
Results
During the pre‐pandemic period, from 1 March 2019 to 31 January 2020, a ‘code stroke’ was called on a total of 2125 patients who presented (including via emergency transport) to our institution’s emergency departments and were suspected to have an acute ischaemic stroke. Of these, 1818 underwent multimodal CT for diagnostic work‐up. ECR was performed in 216 patients.
During the pandemic months of March and April, there were 277 ‘code stroke’ activations, 202 patients underwent multimodal CT, and 21 ECRs were performed. The monthly breakdown for the pre‐pandemic and pandemic periods is given in Table S1 of the Supplement. The Shapiro–Wilk test confirmed normality of all patient numbers for the pre‐pandemic period.
Demographic data for patients undergoing multimodal CT are also given in the data Supplement (Table S2a for the pre‐pandemic period and Table S2b for the pandemic period; Figure S1).
The total number of ‘code stroke’ activations in patients presenting to our institution dropped during February (transition month), with more pronounced decline during the pandemic period, reaching significance (p < 0.0025) in April following the lockdown (Fig. 1). The total number of ED presentations and ED patients who underwent CT also decreased significantly (p < 0.0025) during the pandemic period (Fig. S2).
Fig. 1.

Number of ‘code stroke’ activations (solid yellow line), patients undergoing multimodal ‘code stroke’ CTs (solid red line) and ECRs performed each month (solid blue line) between 03/01/2019–04/30/2020. The corresponding dashed lines of the same colour indicate the lower 95% confidence interval boundary for each during the pre‐pandemic period. Note that there is a lag of the nadir and all data points relative to Fig. 2. This is due to the accounting of patient numbers for a particular month at the close of the month.
The number of patients undergoing multimodal CT per month also decreased during February and the pandemic period, reaching significance (P < 0.0025) in April. Figure 2 shows the number of patients presenting to our institution who underwent multimodal ‘code stroke’ CT per week relative to the weekly number of new and cumulative COVID‐19 cases in Australia. At the start of the pandemic period on 1 March 2020, there was a considerable decline in patients undergoing multimodal CT, crossing the 95% confidence interval by March 20 and reaching significance (P < 0.0025) in the weeks of March 27 and April 10. This aligned well with the peak of the number of new COVID‐19 cases in Australia. The nadir was in the week of March 27, when the population was placed in lockdown. At this nadir, the number of CTs decreased 68% relative to the weekly average over the pre‐pandemic period. Although still depressed, weekly patient numbers have started to increase.
Fig. 2.
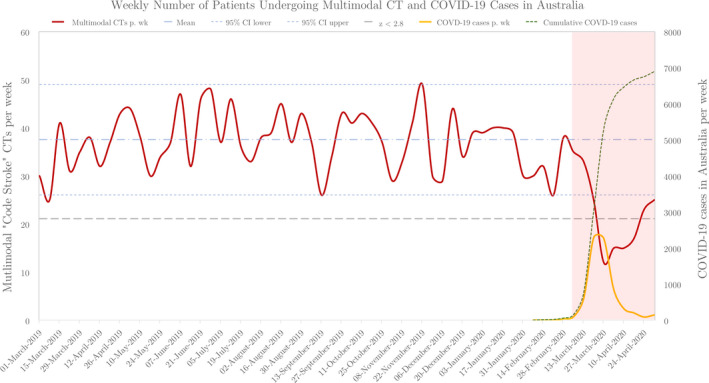
Number of patients who underwent multimodal ‘code stroke’ CT each week (03/01/2019–05/10/2020) for suspected acute ischaemic stroke (solid red line). Mean (dot‐dash blue line) and 95% confidence intervals (dashed blue lines) of weekly patient numbers for the pre‐pandemic period. Datapoints below the dashed grey line ( z = 2.8) line are significantly lower than the mean weekly case number (p < 0.0025). The pandemic period is highlighted by the red overlay box. Number of weekly new COVID‐19 cases in Australia (dashed orange) and corresponding cumulative numbers (dashed green) are shown. Starting with the beginning of the pandemic period, a clear decline in the weekly number of scans can be seen that corresponds well with the onset and duration of the peak of the COVID‐19 pandemic.
The number of ECRs also decreased during the pandemic months (16 in March and 11 in April) compared to the compared to the pre‐pandemic mean of 18.4, but this decline did not reach significance (P = 0.165).
Year‐on‐year (Fig. 3), there was a mild relative decrease in the number of ‘code stroke’ activations and patients undergoing multimodal CTP but a 14% increase in the number of ECRs performed in March. There was a substantial relative year‐on‐year decline across all categories in April, with a 37% decrease in ‘code stroke’ activations, 54% decrease in multimodal CTs and 48% decrease in ECRs performed. Both the absolute number and percentage of patients with LVOs increased in March compared to the pre‐pandemic months (Fig. 4a, Table S3). In April, the absolute number of patients with LVOs decreased but the percentage was similar to the pre‐pandemic months. Year‐on‐year, there was a mild increase in the number of LVOs in March (+15%), but marked decrease in April (−55%) (Fig. 4b).
Fig. 3.
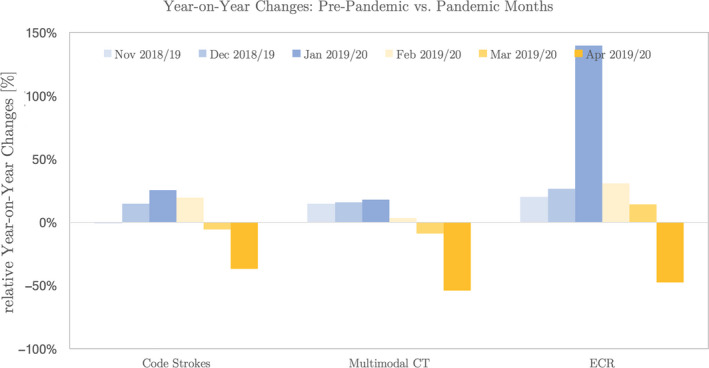
Relative year‐on‐year change in the numbers of ‘code stroke’ activations, multimodal CTs and ECRs performed in the pandemic months and four immediate pre‐pandemic months.
Fig. 4.
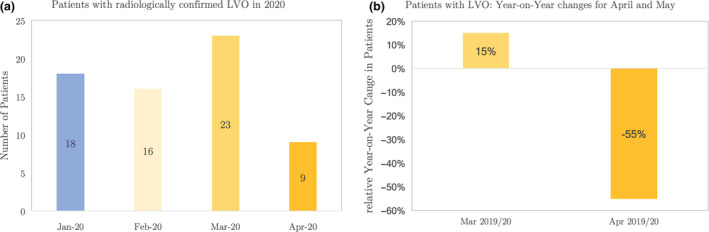
(a) The number of patients with an LVO who presented to our institution in the two immediate pre‐pandemic months (January and February) and the pandemic months (March and April). (b) Year‐on‐year (2019to2020) change in the number of LVO patients in the two pandemic months of March and April.
The percentage of ECR patients who were direct presentations to our hospital is shown in Figure 5. There was a significant decline (P < 0.025) in April compared to the 9‐month pre‐pandemic period.
Fig. 5.
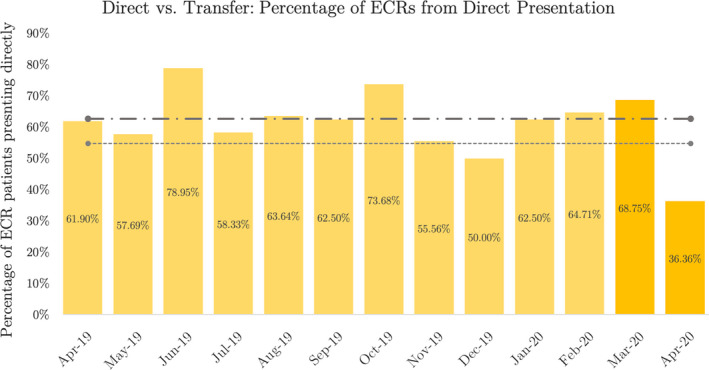
Proportion of patients undergoing ECR who presented directly to our institution (as a percentage of the total number of ECRs, which also includes patients transferred from an outside hospital).
The median Door‐to‐CT time decreased to 9 minutes (inter‐quartile range 7–16 minutes) during the pandemic months of March and April compared to the pre‐pandemic months where the median was 22 minutes (inter‐quartile range 15–32 minutes). The number of patients who underwent ECR during the pandemic months was too small to determine whether these time reductions were statistically significant.
The number of COVID‐19 positive or suspected patients who underwent multimodal CT and ECR was also too small to determine whether there were significant delays caused by additional precautions taken by the CT and interventional neuroradiology teams when caring for these patients, such as use of personal protective equipment (PPE). Only one COVID‐19 suspected or positive patient underwent ECR during this time. Both the Door‐to‐CT time and Door‐to‐Puncture time in this patient were above the 90th centile of the pre‐pandemic values.
Discussion
Our retrospective analysis shows that both the number of patients presenting to our institution with a suspected acute ischaemic stroke and volume of multimodal CT scans performed to rule out stroke declined significantly during the pandemic period. The number of LVOs remained stable in the first pandemic month but decreased proportionally in the second month along with the number of ECRs performed. The results of this study casts in numbers the perception of decline in stroke patients presenting to hospital during the pandemic in a community where the prevalence of infection has been low, and the healthcare system has not been challenged by a surge in COVID‐19‐related presentations.
Since 2018, following the publication of two high‐profile trials showing the benefit of ECR in the late time‐window, it has since been routine practice at our institution to perform multimodal stroke CT on all patients with a suspected ischaemic stroke presenting within 24 hours of onset. 10 , 12 The intake of stroke patients has been relatively stable since then. Other than seasonal factors and holidays, no other extrinsic factors or changes in internal process could therefore explain the dramatic decline in patient numbers during the pandemic period. We have addressed the former by assessing the relative year‐on‐year changes in patient numbers and shown a substantial decline in the number of ‘code stroke’ activations, multimodal CTs, LVO presentations and ECRs performed in April.
Both the absolute number and percentage of patients with LVOs amongst those undergoing multimodal CT increased in March. This suggests, in keeping with our hypothesis, that patients with severe strokes continued to present to hospital during this early pandemic period, while those with mild strokes or stroke mimics may have been deterred from coming into hospital. In April, following the lockdown and peak in new COVID‐19 cases, the number of patients presenting with LVOs decreased in alignment with the decrease in patients undergoing multimodal CT. The percentage of LVOs therefore did not increase compared to the pre‐pandemic months. The decline in stroke presentations and imaging during April therefore also included patient with severe strokes, counter to our hypothesis. Due to the relatively short temporal span of the COVID‐19 event, we were only able to operate with point estimates, which is a limitation of the study.
A decline in stroke imaging across the United States and a significant decrease in ECRs performed in France during the pandemic have already been reported. 6 , 8 A single‐centre study from Catalonia found a modest decrease in stroke admissions and ECRs. 7 France, the United States and Catalonia have all been severely affected by COVID‐19, causing a strain on their healthcare systems, an important point of distinction between these prior investigations and ours. In Australia, we were fortunate that our healthcare system was not overwhelmed by a surge in COVID‐19 patients. Our geographic isolation and low population density, as well as early institution of travel bans, have likely kept the disease at bay. Hospital and emergency service (including emergency transportation) capacity was therefore not a rate limiting factor that could explain the reduction in ‘code stroke’ activations, multimodal CTs and ECRs. Since healthcare providers in referring hospitals and at our institution have not altered their practice, the question remains: what was the cause for the decrease in ‘code strokes,’ including LVOs?
One potential hypothesis is a true decrease in patients suffering AIS. As a ‘healthcare system COVID preparedness’ measure, elective surgical procedures have been curtailed. 1 This has, in turn, decreased the number of patients coming off anticoagulation, a known risk factor for ischaemic stroke. 16 However, it has been shown that fewer than 5% of strokes are related to cessation of anticoagulation as a part of perioperative management. 17 This is therefore speculated to be a minor contributing factor.
We hypothesize that the main driving force behind the decline in acute stroke presentations was patients avoiding hospital presentation and medical care due to social distancing rules, the lockdown and fear of contracting COVID‐19. The nadir in multimodal stroke CTs immediately followed the peak in new COVID‐19 cases and coincided with the week in which lockdown was instituted, suggesting that patients’ adherence to the lockdown and fear of contracting COVID‐19 may have led to a decrease in stroke presentations to hospitals. Since the decrease in ‘code stroke’ activations and patients undergoing multimodal CT had already decreased in February and March, prior to the lockdown but during extensive media coverage of the toll extracted by COVID‐19 in other parts of the world, fear is suspected to have played a large part in this phenomenon. We speculate that altruism may have motivated some patients to avoid coming to hospital and ‘burdening’ the healthcare system during the crisis. It is also possible that the lockdown rules resulted in delayed presentation of socially isolated individuals.
The increased percentage of LVOs amongst patients undergoing multimodal CT in the first pandemic month suggests that those with more severe strokes continued to come into hospital prior to lockdown, while patients with milder symptoms chose to stay away, causing a decrease in number of ‘code strokes’ and multimodal stroke CTs. In April, following lockdown, even the number of LVOs decreased. We speculate that this may be due to increasing anxiety in the community, despite declining incidence of new COVID‐19 cases in Australia. Kansagra et al also observed that differences in the incidence of COVID‐19 did not correlate with decreased utilization of stroke imaging. 6
In addition to the decrease in the total number of ECRs during April, there was also a decrease in the proportion of patients undergoing ECR who presented directly to our institution, compared to those who were transferred from a primary stroke centre. Access to transfer resources does not, therefore, appear to have been a driving factor in the decline in patients undergoing ECR. Since these referring hospitals are peripheral and rural centres, fear of presenting to hospital may have been less than in more densely populated metropolitan areas where the prevalence of COVID‐19 was higher. This is, however, speculative.
So where have all the patients gone? The question remains whether the decrease in stroke imaging and intervention reflects a true decrease in the incidence of LVO strokes, or a decrease in patients seeking medical care. There are anecdotal reports of delayed presentation of stroke patients to hospital, beyond the ECR window. In a sub‐study, we attempted to see if there was a larger proportion of patients presenting with larger and/or completed infarcts as a consequence of delayed presentation to hospital; however, the numbers were too small for meaningful analysis. Perhaps future studies can shed light into what happened to these patients and reveal why they did not come into hospital during the pandemic period.
If the observed decrease in the number of LVOs and ECRs has been due to patients avoiding or delaying hospital presentation for fear of COVID‐19, the burden of neurological disability and morbidity in the community will have increased during the pandemic. This neurological disability could have been prevented with timely treatment. Therefore, in communities where the prevalence of COVID‐19 has been low, the collateral damage caused by patients avoiding medical care during the pandemic may be greater than the morbidity caused by COVID‐19 per se. As such, public awareness campaigns encouraging patients to access timely care for treatable conditions may be warranted if there is a resurgence of COVID‐19 or if a similar pandemic scenario was to occur in the future.
One thin silver lining was that the Door‐to‐CT time decreased during the pandemic months. This was attributed to reduced congestion of our emergency departments, which we speculate may have helped expedite patient transfer to the radiology department for multimodal CT. The authors are cognizant that in other health systems, where emergency departments have been overwhelmed by COVID‐19 patients, a delay in this process may have occurred. Normal workflow was disrupted during the pandemic by additional precautions required to minimize infection risk. All staff involved in the direct care of patients with suspected or confirmed COVID‐19 infection were required to don additional PPE. Intensive decontamination of equipment and rooms used to image and treat these patients was also necessary. To mitigate potential delays, additional staff were rostered to assist with these precautions. Non‐emergent outpatient CTs and elective procedures were deferred to create capacity in preparation for a surge in COVID‐19 patients. These ‘radiology preparedness measures’ likely contributed to the shorter Door‐to‐CT times, which was an unanticipated collateral benefit. The number of COVID‐19 positive and suspected patients who presented with a stroke during the study period was too small to assess whether extra precautions caused a significant delay in imaging or ECR in this group. Further studies are warranted, with pooling of data from different centres given the low prevalence of infection in Australia, to assess the impact of COVID‐19 precautions on in‐hospital performance metrics.
In conclusion, this study confirmed a marked decrease in the number of acute ischaemic stroke patients presenting to hospital and worked up during the COVID‐19 pandemic, with an associated decline in the number of ECRs performed. There was an inverse relationship with the number of new COVID‐19 patients in the community. Since the prevalence of infection in our community was low, our emergency medical services were not stressed. We therefore conclude that avoidance of hospitals, driven by fear of contracting COVID‐19 and strict adherence to the lockdown, was the most cause for this dramatic decrease in stroke patients, including those who may have benefitted from treatment. Such indirect effects of the pandemic may have greater impact than the pandemic itself. Assessment of follow‐up data from outpatient clinics and imaging for delayed presentations is warranted. There is, however, hope for those countries who are fighting their way out of the crisis in the trend we are seeing in Australia. With relaxation of the lockdown, the number of patients coming to the hospital is gradually recovering.
Supporting information
Table S1. Detailed monthly breakdown of “code stroke”, multimodal CTP and ECR numbers.
Table S2. (a) Demographics of Patients who underwent multimodal CT during the Pre‐Pandemic Period. (b) Demographics of Patients who underwent multimodal CT during the Pandemic Period.
Table S3. Percentage of patients who underwent multi‐modal CT who had an LVOs.
Fig. S1. Age distribution of female and male patients undergoing multimodal CT during the pre‐pandemic and the COVID‐19 period.
Fig. S2. Number of patients who presented to our institution’s emergency departments (solid yellow line), and number of CTs performed on emergency department patients each month (solid blue line) between 03/01/2019 – 04/30/2020.
SA Amukotuwa MBBS, MMed, FRANZCR; R Bammer MEE, MBA, PhD, FISMRM; J Maingard BBiomedSci, MBBS, FRANZCR.
Conflict of interest: The authors have no conflicts of interest to declare.
References
- 1. https://www.pm.gov.au/media/elective-surgery.
- 2. https://www.cdc.gov/coronavirus/2019ncov/hcp/guidancehcf.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fcoronavirus%2F2019-ncov%2Fhealthcare-facilities%2Fguidance-hcf.html.
- 3. Weissman GE, Crane‐Droesch A, Chivers C et al. Locally informed simulation to predict hospital capacity needs during the COVID‐19 pandemic. Ann Intern Med 2020; 173(1): 21–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Roland DLI, Toy S. Doctors fret as coronavirus keeps heart, stroke patients away from ER. The Wall Street Journal 2020. https://www.wsj.com/articles/doctors‐fret‐over‐lower‐er‐attendance‐during‐pandemic‐11589454002 [Google Scholar]
- 5. Garcia S, Albaghdadi MS, Meraj PM et al. Reduction in ST‐segment elevation cardiac catheterization laboratory activations in the United States during COVID‐19 pandemic. J Am Coll Cardiol 2020; 75: 2871–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Kansagra AP, Goyal MS, Hamilton S, Albers GW. Collateral effect of Covid‐19 on stroke evaluation in the United States. N Engl J Med 2020; 383: 400–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Rudilosso S, Laredo C, Vera V et al. Acute stroke care is at risk in the era of COVID‐19: experience at a comprehensive stroke center in Barcelona. Stroke 2020; 51(7): 1991–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Kerleroux B, Fabacher T, Bricout N et al. Mechanical thrombectomy for acute ischemic stroke amid the COVID‐19 outbreak: decreased activity, and increased care delays. Stroke 2020:STROKEAHA120030373. [DOI] [PubMed] [Google Scholar]
- 9. Powers WJ, Rabinstein AA, Ackerson T et al. 2018 Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2018; 49(3): e46–e110. [DOI] [PubMed] [Google Scholar]
- 10. Albers GW, Marks MP, Kemp S et al. Thrombectomy for Stroke at 6 to 16 Hours with selection by perfusion imaging. N Engl J Med 2018; 378(8): 708–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Goyal M, Menon BK, van Zwam WH et al. Endovascular thrombectomy after large‐vessel ischaemic stroke: a meta‐analysis of individual patient data from five randomised trials. Lancet 2016; 387(10029): 1723–31. [DOI] [PubMed] [Google Scholar]
- 12. Nogueira RG, Jadhav AP, Haussen DC et al. Thrombectomy 6 to 24 hours after stroke with a mismatch between deficit and infarct. N Engl J Med 2018; 378(1): 11–21. [DOI] [PubMed] [Google Scholar]
- 13. Australian Stroke Coalition statement on stroke care during the COVID‐19 crisis, April 24, on: https://strokefoundation.org.au/.
- 14. Lyden P. Temporary emergency guidance to US stroke centers during the COVID‐19 pandemic on behalf of the AHA/ASA stroke council leadership. Stroke 2020; 51: 1910–2. [DOI] [PubMed] [Google Scholar]
- 15. https://www.worldometers.info/coronavirus/country/australia/.
- 16. Macellari F, Paciaroni M, Agnelli G, Caso V. Perioperative stroke risk in nonvascular surgery. Cerebrovasc Dis 2012; 34(3): 175–81. [DOI] [PubMed] [Google Scholar]
- 17. Wong EAMTV. High frequency of anticoagulation management issues preceding ischemic strokes in aF (in press). MJA 2020. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Detailed monthly breakdown of “code stroke”, multimodal CTP and ECR numbers.
Table S2. (a) Demographics of Patients who underwent multimodal CT during the Pre‐Pandemic Period. (b) Demographics of Patients who underwent multimodal CT during the Pandemic Period.
Table S3. Percentage of patients who underwent multi‐modal CT who had an LVOs.
Fig. S1. Age distribution of female and male patients undergoing multimodal CT during the pre‐pandemic and the COVID‐19 period.
Fig. S2. Number of patients who presented to our institution’s emergency departments (solid yellow line), and number of CTs performed on emergency department patients each month (solid blue line) between 03/01/2019 – 04/30/2020.


