1.
Since the start of the SARS‐CoV‐2 outbreak in China in December 2019 COVID‐19 has affected nearly 4,5 million people around the world, with almost 286 000 fatalities reported as of the current date. 1 The World Health Organization declared COVID‐19 as a Public Health Emergency of International Concern on January 30th, 2020 and on March 11th COVID‐19 was declared a pandemic disease. 2 In Spain, first cases were diagnosed in early February, with the incidence peak occurring between the last week of March and the first week of April. At the time of writing this article, 227 000 patients were infected and 26 000 patients had died of COVID‐19. 1 The rapid spread of the virus and the severity of the disease has been a real challenge to the health systems of most affected countries, compelling to the transformation of hospitals in COVID‐19 monographic centres. In order to cover COVID‐19 overwhelming necessities, non‐COVID activity was reduced to the minimum, cancelling non‐urgent surgery, outpatient clinics and treatments, and diagnostic tests.
Once the acute phase of the pandemic is being overcome a new, unprecedented scenario is challenging health systems. This post‐COVID‐19 era is characterized, by one side, by the menace of a new COVID‐19 outbreak, especially nosocomial outbreaks affecting high‐risk population, such as fragile and immunosuppressed patients. In the other side, safety of healthcare professionals is a major issue since the start of the pandemic, with high rates of infected workers causing fear and stress among health staff.
In order to create safe environments for both patients and workers, Hospitals will need to adequate spaces, avoiding shared rooms and other service facilities, this is: Hospitals need to become ‘liquid’. This objective can be difficult to achieve in antique, obsolete buildings, with rigid structures and spaces.
In this context, Hospital at Home (HaH) Units appear as an ideal solution to palliate these deficiencies. Hospital at Home is defined as a model capable to provide twenty‐four hours a day, seven days a week, hospital‐level care at home without the need of conventional admission. 3 The benefits of the model, such as the better outcomes in terms of health recovery and costs have been published in literature. 4 This model has been worldwide implemented during the last 20 years, although with different idiosyncrasies due to different health system's policies. Spanish public health system has fostered the creation and implementation of strong and multidisciplinary HaH Units in both tertiary and secondary hospitals.
Previously to the SARS‐CoV‐2 outbreak, HaH were focused in avoiding conventional admission in patients consulting in the Emergency Room (ER) or in Primary Care, 5 and providing early discharge service for surgical and nonsurgical hospital services 6 (Figure 1). HaH Units usually include nurse and medical staff with the support of administrative staff, physiotherapists, social workers and other professionals. Visits at home are performed by a nurse and a doctor, and along with clinical and physical assessment a variety of procedures are available such as blood test, microbiology cultures, bedside ultrasound, midline placement, EKG, peak‐flow, etc. Personal protection equipment such as gloves, hat, glasses, facemask and gown are used when entering in the home of patients with indication for air or contact isolation (ie. drug resistant bacteria, influenza virus infection), assuring a safe contact for both patient and healthcare professional. HaH has recently proven to be not only a safe but also a less expensive alternative to conventional hospitalization, with costs up to 38% lower than a complete hospital admission. 7 Moreover, HaH are easily scalable devices, as nurse and medical staff volume can be adapted to the work load at each time, rapidly scalable in times of need, such as the influenza season in winter, 8 or in this case the COVID‐19 pandemic. Although more specific cost‐effectiveness studies in COVID‐19 patients are needed, a positive cost‐effective imbalance to HaH units is presumable and should be taken into consideration in constraint times such as the present.
FIGURE 1.
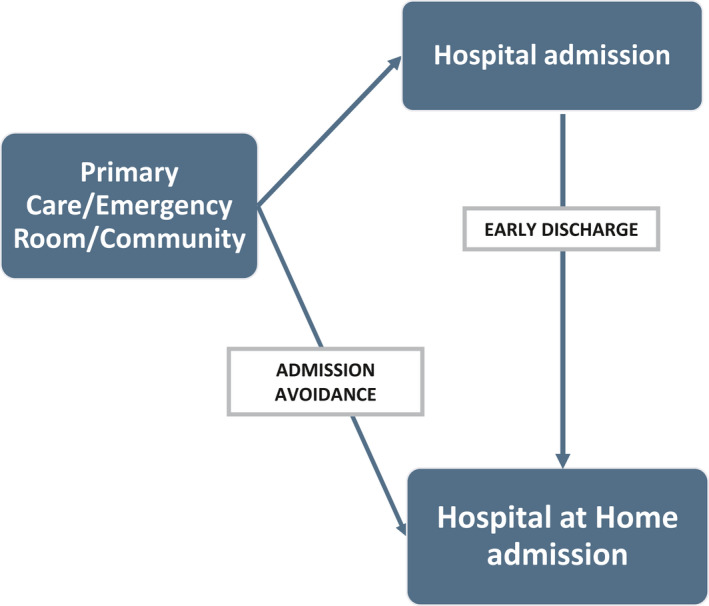
Flow chart of patients admitted in Hospital and Hospital at Home Units
HaH Units should adapt to the new post‐COVID19 scenario providing solutions to the main issues previously raised. From our point of view there are four objectives to HaH to achieve:
First of all HaH units should provide home admission and hospital‐level care for those patients with non‐COVID acute illness, detected in the outpatient clinics, or in the GP clinic. This is especially relevant for patients with chronic conditions presenting recurrent flares such as COPD or chronic heart failure and for patients with high risk of presenting a severe form of COVID‐19 such as haematological and oncological patients with immunosuppressive therapies, solid organ transplant recipients or elderly patients. Home assessment of these patients by HaH on demand of the specialist doctor, may avoid unnecessary and risky visits to the ER or Day Hospital (DH) and avoid hospital admission.
At another level of the healthcare continuum, HaH units are an optimum option for delivering early discharge logistics for patients admitted in the hospital. In order to reduce the hospital stay, and therefore the risk of nosocomial infections, HaH feasibility should be assessed for each patient admitted to conventional ward and reevaluated every 48 hours of admission. This strategy is remarkably useful in surgical services, in order to optimize discharge for noncomplicated post‐surgical patients, which has proved to be safe and improve patient recovery in different fields such as thoracic surgery or orthopaedics 9 but also for complicated post‐surgeries such as wound infections, orthopaedic prosthetic infections, comorbidities decompensation, etc. In medical wards, early discharge should also be evaluated for every patient, especially in infected patients needing long antibiotic treatments such as infective endocarditis or osteomyelitis. 10
Day Hospitals work as outpatient centres for evaluation, diagnosis and treatment of patients with chronical or subacute conditions. Examples of these are DH of Oncology or Hematology where patients receive chemotherapy and can be assessed without previous appointment in case of clinical worsening. Although DH are useful resources to replace hospital admission and also to avoid ER visits, can be a risky environment both for at risk patients and professionals, due to a high turnover and occupation rate and unknown COVID19 status. HaH Units may compliment DH services, providing home visits for programmed intravenous treatments (antibiotics, chemotherapy…) or clinical assessment and evaluation in acutely ill patients. Complex wound care is a great burden for DH, especially those of Dermatology or Vascular surgery. For these patients shared care between specialist and HaH is a safe alternative, providing wound care with specialized nurses at home, and telematic follow‐up of the wound by medical staff.
Finally, HaH Units have played different roles during the COVID‐19 pandemic, but mostly provided first line care of COVID‐19 patients at their homes or in medicalized civil buildings such as hotels. 11 During this period, HaH units have accumulated a large amount of experience in dealing with COVID‐19 patients, the evolution of the disease and the criteria for HaH admission (Table 1) or conventional hospitalization transfer due to clinical worsening. This experience should be posed at the disposal of General Practitioners in Primary Care Centers, nursing homes and other outpatient facilities, acting as a COVID‐19 expert consultation service, with home assessment of suspected COVID‐19 patients, diagnostic testing (including nasopharynx swab for PCR, bedside thoracic echography, blood test…) and managing of patients including home care or hospital derivation for severe ones.
TABLE 1.
Hospital at Home admission criteria for COVID‐19 patients
| Early discharge from hospital ward |
|
More than 6 d since the start of symptoms |
|
Absence of fever in the last 24 h |
|
Respiratory rate < 22 rpm and oxygen saturation > 95% with FiO2 < 0.35 |
|
C Reactive protein <5 mg/dL or descending, normal LDH or descending, lymphocytes >800 cells/mm3 or ascending. |
|
No radiological progression of pneumonia. |
| Admission from Emergency room: |
|
Bilateral pneumonia in patient without high‐risk factors (>65 y old, hypertension, chronic obstructive pulmonary disease, cardiovascular disease, diabetes, cancer, immunosupression). |
|
Respiratory infection without pneumonia, or unilobar pneumonia in patients with risk factors. |
For all patients: home conditions allowing patient isolation from cohabitants.
In conclusion, we believe that HaH units are easily scalable, and with a cost‐effective growth capacity alternatives to conventional hospitalization. These units can play a major role in the reorganization of hospitals and health systems aiming to avoid unnecessary visits of the patients to health centres and therefore diminishing the risk of COVID‐19 (and also other communicable diseases) nosocomial outbreaks and healthcare professionals infections. In order to protect patients and healthcare workers in a post‐COVID 19 scenario, HaH units should be strengthened to assure pre‐COVID quality levels in health assistance.
REFERENCES
- 1. University JH . COVID‐19 Dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU).
- 2. World Health Organization . World Health Organization Health topics March 11th 2020 [Internet]. 2020 [cited 2020 May 13]. http://www.euro.who.int/en/health‐topics/health‐emergencies/coronavirus‐covid‐19/news/news/2020/3/who‐announces‐covid‐19‐outbreak‐a‐pandemic. Accessed April 18, 2020.
- 3. Kuehn BM. Hospital at home program cuts costs, improves patient health and satisfaction. JAMA. 2012;308(2):122. [Google Scholar]
- 4. Leff B, Burton L, Mader SL, et al. Comparison of functional outcomes associated with hospital at home care and traditional acute hospital care. J Am Geriatr Soc. 2009;57(2):273‐278. [DOI] [PubMed] [Google Scholar]
- 5. Shepperd S, Iliffe S, Doll HA, et al. Admission avoidance hospital at home. Cochrane Database of Syst Rev. 2016;9(9) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Gonçalves‐Bradley DC, Iliffe S, Doll HA, et al. Early discharge hospital at home. Cochrane Database of Syst Rev. 2017;6(6) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Levine DM, Ouchi K, Blanchfield B, et al. Hospital‐level care at home for acutely ill adults a randomized controlled trial. Ann Intern Med. 2020;172(2):77. [DOI] [PubMed] [Google Scholar]
- 8. Cardozo C, Nicolás D, Bodro M, et al. Influenza at Hospital at Home: A safe option during epidemic season. In: World Hospital at Home Congress. Madrid; 2019.
- 9. Bori G, Aibar J, Lafuente S, et al. Hospital at home in elective total hip arthroplasty. Hip Int. 2010;20:58‐62. [DOI] [PubMed] [Google Scholar]
- 10. Pericàs JM, Llopis J, González‐Ramallo V, et al. Outpatient parenteral antibiotic treatment for infective endocarditis: a prospective cohort study from the GAMES cohort. Clin Infect Dis. 2019;69(10):1690–1700. [DOI] [PubMed] [Google Scholar]
- 11. Pericas JM, Cucchiari D, Torrallardona‐Murphy O, Calvo J, Serralabos J, Nicolás D.Hospital at Home for the Management of COVID‐19: A Case Series of 63 Patients. Submitted; 2020.
ACKNOWLEDGEMENTS
The authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers' bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent‐licensing arrangements), or nonfinancial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript. Both authors contributed to the conception, writing and critical review of the manuscript and had access to the final version.


