Abstract
Objective
The coronavirus disease 2019 (COVID‐19) has altered how the current generation of thoracic surgery residents are being trained. The aim of this survey was to determine how thoracic surgery program directors (PDs) are adapting to educating residents during the COVID‐19 pandemic.
Methods
Thoracic surgery PDs of integrated, traditional (2 or 3 year), and combined 4 + 3 general/thoracic surgery training programs in the United States were surveyed between 17th April and 1st May 2020 during the peak of the COVID‐19 pandemic in much of the United States. The 15‐question electronic survey queried program status, changes to the baseline surgical practice, changes to didactic education, deployment/scheduling of residents, and effect of the pandemic on case logs and preparedness for resident graduation.
Results
All 23 institutions responding had ceased elective procedures, and most had switched to telemedicine clinic visits. Online virtual didactic sessions were implemented by 91% of programs, with most (69.6%) observing same or increased attendance. PDs reported that 82.7% of residents were on a non‐standard schedule, with most being deployed in a 1 to 2 week on, 1 to 2 week off block schedule. Case volumes were affected for both junior and graduating trainees, but a majority of PDs report that graduating residents will graduate on time without perceived negative effect on first career/fellowship position.
Conclusions
The COVID‐19 pandemic has radically changed the educational approach of thoracic surgery programs. PDs are adapting educational delivery to optimize training and safety during the pandemic. Long‐term effects remain uncertain and require additional study.
Keywords: cardiothoracic surgery, program directors, surgical education, thoracic surgery residency
Abbreviations
- ACGME
Accreditation Council for Graduate Medical Education
- COVID‐19
coronavirus disease 2019
- PD
program director
1. INTRODUCTION
The sudden emergence of the severe acute respiratory syndrome coronavirus‐2 as the pathogen responsible for the novel coronavirus disease 2019 (COVID‐19) has changed the provision of healthcare in the United States and globally in early 2020. This has particularly impacted the field of cardiothoracic surgery with elective (and in some institutional cases more urgent) operative interventions being delayed indefinitely, stay at home orders for certain clinical staff, re‐distribution of clinical workforces to care for patients with COVID‐19, and disruption in normal public services affecting the healthcare workforce. This has led to a direct effect on cardiothoracic surgery residents training to be the next generation of surgeons, either by limiting technical development or changing the way resident education outside of the operating room occurs. Indeed, resident physicians from mansy fields have stepped up to fill in the gaps in our healthcare teams during this trying period.
Program directors (PD) in thoracic surgery residencies are now tasked with a novel educational dilemma: training cardiothoracic surgeons in the art and practice of the field without consistent operative experience, traditional didactic exposure, and under constant threat of infection from a disease currently causing a worldwide pandemic. Though residents are concerned for personal/family safety and exposure to COVID‐19, they have continued to vocalize a need and desire to adapt training to the situation at hand to maximize educational opportunities whenever possible. 1 , 2 Given this desire, many PDs in thoracic surgery have implemented changes to didactic curriculum, simulation, resident schedules, resident deployments, and case/training requirements to account for the COVID‐19 pandemic. We surveyed thoracic surgery PDs during the peak of the current pandemic with the aim of understanding the changes various institutions have made to optimize thoracic surgery resident education while dealing with the varying clinical demands of the COVID‐19 pandemic.
2. METHODS
2.1. Ethics
This study was approved by the Institutional Review Board of the University of Pittsburgh. Thoracic PDs took the survey voluntarily and survey results were reported in aggregate without any identifying information.
2.2. Study population
Thoracic surgery PDs of Accreditation Council for Graduate Medical Education (ACGME) accredited thoracic surgery residencies (74 accredited traditional thoracic surgery programs, 27 integrated thoracic surgery training programs, and 13 4 + 3 combined general/thoracic surgery programs) were sent an e‐mail invitation to complete the survey between 17th April and 1st May 2020. Two reminder e‐mails were sent to the PDs over the course of the 2‐week period to prompt completion. Associate PDs listed were also encouraged to complete the survey if the PD was unable to do so for any reason. This was a voluntary survey with no incentive offered for completion, and participants in the study could stop at any time. Only completed surveys were included for analysis in this study.
2.3. Survey instrument
The survey instrument was developed to answer questions regarding changes in resident didactic education, document changes to resident schedules and deployment to care for patients with COVID‐19, characterize concerns regarding case numbers and resident graduation, and estimate to some level the COVID‐19 imposed burden on a given program. The survey questions were internally tested for face validity of content and clarity by 3 experts in thoracic surgery and 2 persons not associated with the field, and a pilot study of the final survey instrument was tested for functionality and clarity among the authors before release of the final survey instrument. Survey instrument questions can be reviewed in Supplemental Table. The survey was also designed to be purposefully brief (<5 minutes to complete) as to maximize participation and minimize incomplete responses during the pandemic peak. The survey questions were developed by a select group of the authors (GC, IS) and deployed as a secure electronic survey instrument via a validated commercial platform (Qualtrics, Raleigh, NC).
2.4. Statistical analysis
Data from the completed surveys were reported as number (%) for categorical variables and median (range) for continuous variables. Because of the small number of responses in many categories no sub‐analysis was planned, and only raw data has been reported for clarity.
3. RESULTS
3.1. Institutional characteristics during coronavirus disease 2019
There were 23 institutions submitting responses from either the PD or associate PD during the 2‐week study period representing all major geographic regions of the United States and accounting for 29.2% (33/113 programs surveyed) of all ACGME thoracic surgery residencies. There was a 28.8% response rate (21/73) for traditional 2 to 3 year thoracic surgery training programs surveyed, 33.3% (9/27) for integrated 6 year programs, and 23.1% (3/13) for combined 4 + 3 general/thoracic surgery training programs. PDs reported a median of 6 residents (range, 1‐24) active within their programs during the pandemic survey period. Figure 1A demonstrates institutional changes that had been enacted at the time of the survey (during the peak of the pandemic in many areas) across the institutions surveyed. Figure S1 shows the dates that elective procedures were halted at the surveyed programs' institutions. The highest level of ACGME stage reached by each program was reported as stage 1 (business as usual) for 3 (13.0%) programs, stage 2 (increased clinical demand guidance) for 10 (43.5%) programs, and stage 3 (pandemic emergency status guidance) for 9 (39.1%) programs.
Figure 1.
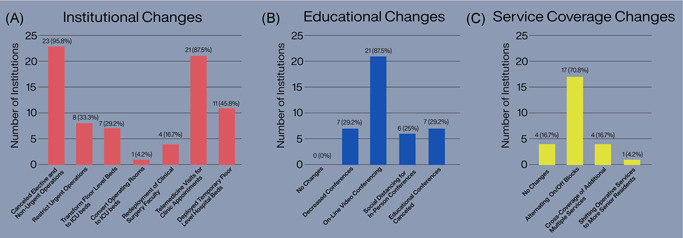
A, Institutional changes occurring to adjust to the current coronavirus disease 2019 (COVID‐19) pandemic response among thoracic surgery programs surveyed. B, Changes made to educational curriculum/didactic conferences during the COVID‐19 pandemic in thoracic surgery programs. C, Changes to resident service coverage/schedules implemented by thoracic surgery programs during the COVID‐19 pandemic
3.2. Changes to didactic/educational curriculum
Figure 1B demonstrates the changes PDs of thoracic surgery residencies implemented regarding didactic curriculum and education activities during the COVID‐19 pandemic. On‐line video conferencing was the most frequent implementation with 21 (91%) of programs electing to utilize this technology in some manner. It was additionally noted that live simulation sessions normally scheduled in person were canceled in lieu of online virtual activities. Interestingly, five (21.7%) PDs reported increased resident attendance at conference while seven (30.4%) noticed a decrease in conference attendance during the pandemic.
3.3. Changes in resident rotations/deployments
Although 4 (17.3%) programs reported no change in resident rotation scheduling, the remaining programs reported a variety of changes to normal resident working schedules (Figure 1C). The most frequent reported change by PDs was implementing a staggered “platoon” deployment strategy with a 1 to 2 weeks on/off alternating deployment schedules for residents in 17 (73.9%) programs to limit exposure. Prolonged additional cross‐coverage above normal and shifting of operative responsibilities to more senior residents were less commonly reported strategies. Importantly, three (13.0%) of PDs have had to re‐deploy thoracic surgery residents to nonsurgical services to assist with the primary care of COVID‐19 patients during this time, with another 12 (52.2%) of programs reports that they have plans to re‐deploy if clinical volume of COVID‐19 spikes and requires attention. PDs reported in a free‐text response that the re‐deployed residents are working in COVID‐19 intensive care environments, helping to staff bedside procedure teams, or staffing extra‐corporal life support teams.
3.4. Effect of COVID‐19 pandemic on resident technical development and promotion
Figure 2 (top) shows how PDs believe COVID‐19 will affect both junior and graduating thoracic surgery resident case volumes. Most PDs agree that their residents will suffer a negative effect on surgical case volumes because of the pandemic. Given these effects on case volumes, only one (4.3%) PD stated the COVID‐19 pandemic will affect the ability of this year's graduating residents to finish, while 19 (82.6%) stated there would be no anticipated delay. Despite being able to graduate on time, Figure 2 (bottom) demonstrates there was more uncertainty on graduating resident preparedness. There were four PDs (17.4%) expressing concerns that the COVID‐19 pandemic will negatively affect initial career or advanced fellowship performance of graduating thoracic surgery residents this year and another five (21.7%) unsure of the effect.
Figure 2.
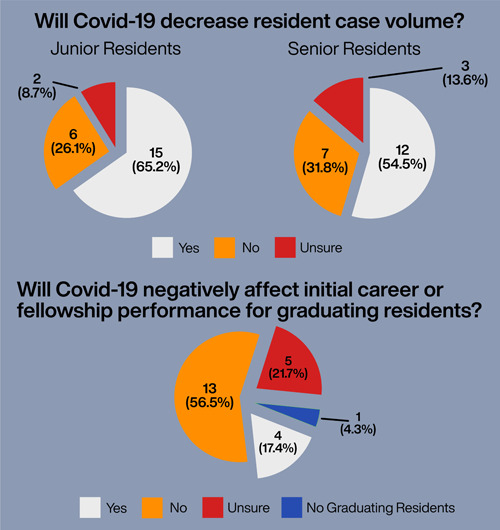
Top: Perceived effect on resident case volumes by the COVID‐19 pandemic. Bottom: Program director opinions regarding any negative affect on initial career/fellowship performance of graduating thoracic surgery fellows due to the COVID‐19 pandemic. COVID‐19, coronavirus disease 2019
4. DISCUSSION
4.1. Study implications
The evolving COVID‐19 pandemic has altered the traditional training paradigm for thoracic surgery residents training in 2020 and likely beyond. With elective surgeries that would be considered teaching cases being canceled, mandatory social distancing and staff reductions on clinical wards, and repurposing parts of or entire hospitals in some areas specifically to treat patients with COVID‐19, thoracic surgical residents and other medical trainees have had major training disruptions due to current educational methods. 3 , 4 This study administered to PDs in thoracic surgery is a first attempt to gauge the current “intra‐pandemic” status of thoracic surgery training programs during what is likely the peak of the first wave of COVID‐19. The intent was to catalog what was happening during this initial wave of COVID‐19 to provide guidance to programs that may be affected by a second wave, and to provide guidance for improvement in educational methodology in crisis situations in the future beyond the current pandemic.
As a result of these events, traditional education paradigms in thoracic surgery (and surgical specialties more widely) are in need of innovation. 5 , 6 , 7 On‐line video conferencing for delivery of live and interactive didactic activities has been widely adopted in surgical residencies, and our study indicates this is true for thoracic surgery as well. 8 Even live simulation sessions have been transitioned to virtual supervised practice with some success. 9 This was noted by one of the free‐text responses in our survey as well. Simulation guided remotely/virtually certainly is an area in need of further development given the need for continued technical training in thoracic surgery and will require further dedicated study. Interestingly in our study, many programs experienced increase in resident attendance at these conferences when held virtually; this may be especially helpful for larger programs covering multiple institutions outside of pandemic times. It is important to note that even with the near universal transition to virtual education, several programs felt the need to cancel some educational activities or hold in‐person meetings with social distancing guidelines, indicating that a complete move to virtual may be difficult for certain interactions. While not the focus of our study, various platforms have been utilized that provide for real‐time discussion and participation in conferences, display of clinical data/imaging in a HIPPA compliant manner, participation by residents and faculty from various sites who normally may not be able to attend an in‐person meeting, and the ability to record sessions for cataloging and review by students asynchronously if desired. The continuation of didactic educational activities and focus on educational principles seems to be preserved among thoracic PDs, and is greatly appreciated by resident learners as confirmed by previous reports. 2
The reassignment of residents to COVID‐19 services seems to have been limited to a few centers experiencing large volume of patients with COVID‐19 at the time of our survey. PDs in thoracic surgery report being in the ACGME stage 3 (pandemic emergency status guidance) level in 39% of centers, but only 13% have had to redeploy thoracic surgery residents to care for medical patients with COVID‐19 in nonsurgical settings. PDs of programs that may have a surge of patients with COVID‐19 in the future should consider the need to redeploy thoracic surgery residents to COVID‐19 intensive care unit settings and staffing procedure teams as their local resources dictate; this was not necessary even at a majority of the programs reporting the ACGME pandemic stage 3 guidance. PDs should look to the ACGME designated guidance and assess the resource utilization of their own programs to determine if redeployment can be done in the setting of current thoracic surgery workforce needs, and further considering the patient care needs of the institution on an individual basis. If there is a surge of COVID‐19 patients and residents are not required to care for patients with COVID‐19, there should be consideration to keeping a number of the residents at home for protection of the work force as was done by a majority of the programs reporting an ACGME stage 1 or 2 status. The safety and wellness of residents during these times is something both current and future residents find important in thoracic surgery careers, and should be considered when making these staffing decisions. 1 , 4 , 10
The importance of the ACGME guidance on providing leeway for graduating resident case logs is imperative given the decrease in case numbers expected by PDs. 11 Indeed, many graduating residents will likely experience further fall‐out from the pandemic including delayed/altered board examination schedules, depressed final case numbers, and in very rare circumstances (according to our study) delay in graduation. 12 By the point in the year the pandemic peaked, most residents typically would have fulfilled the basic programmatic requirements; however, they would be counting on cases in the last several months to obtain additional repetitions with cases to achieve proficiency beyond the minimum requirements. The effect of these lost cases, if any, remains to be seen and will require further study. With that being said, most PDs remain confident their graduating thoracic surgery residents will be prepared to take on initial career placements and advanced fellowships as they had planned. The effect on more junior residents is less clear given that the length of the pandemic, timing of any future waves of COVID‐19 cases, and implementation of further social distancing guidelines may continue to affect case numbers and clinical experience for some time. Close follow‐up of operative experiences will be needed to ensure continued excellence in clinical training for all thoracic surgery residents.
4.2. Limitations
There are a relatively small number of thoracic surgery training programs in the United States compared with other specialties, and as a result the number of programs surveyed here is small and does not allow for stratification and comparison beyond what is reported. Though our overall response rate was 29.2% which is very strong for a voluntary survey and encompassed programs from all geographic regions, certain programs that may have been harder hit or having a different overall experience may not have responded limiting our capture of some more severe pandemic experiences. The survey was limited in scope to capture intra‐pandemic practices; the longitudinal changes in thoracic surgery education will need to be followed closely to determine if the changes made during the COVID‐19 pandemic transition into a new standard. Additionally, long‐term results of decreased/interrupted operative experience is not easy to predict given our techniques and deserves further study.
5. CONCLUSIONS
Thoracic surgery PDs report several changes in the delivery of training to current thoracic surgery residents during the COVID‐19 pandemic. Most didactic/educational activities have migrated to on‐line interactive delivery and has been well‐received. Resident schedules have been impacted with many PDs reporting decreased operative experience among all residents, and residents put onto alternate scheduling paradigms to limit exposure and provide care to patients with COVID‐19 in some instances. Importantly, most PDs are confident that graduating thoracic surgery residents will finish on time and do not foresee negative consequences in first career/advanced fellowship placement. Additional longitudinal study is warranted to see how thoracic surgery education changes because of the ongoing COVID‐19 pandemic.
CONFLICT OF INTERESTS
The authors declare that there are no conflict of interests.
Supporting information
Supporting information
Supporting information
ACKNOWLEDGMENTS
The authors would like to thank the research coordinators at the Heart and Vascular Institute at UPMC for administrative and data management support for this project. The authors would also like to thank the thoracic surgery program directors who chose to participate in this voluntary survey during such a challenging time for all.
Coyan GN, Aranda‐Michel E, Kilic A, et al. The impact of COVID‐19 on thoracic surgery residency programs in the US: A program director survey. J Card Surg. 2020;35:3443–3448. 10.1111/jocs.14954
REFERENCES
- 1. He K, Stolarski A, Whang E, Kristo G. Addressing general surgery residents' concerns in the early phase of the COVID‐19 pandemic. J Surg Educ. 2020;77:735‐738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Dineen EH, Hsu JJ, Saeed A. Reinforcing cardiology training during a pandemic: an open letter to our leaders. Circulation. 2020;142:95‐97. [DOI] [PubMed] [Google Scholar]
- 3. Newman NA, Lattouf OM. Coalition for medical education‐a call to action: a proposition to adapt clinical medical education to meet the needs of students and other healthcare learners during COVID‐19. J Card Surg. 2020;1174‐1175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Simons G, Baldwin DS. Covid‐19: doctors must take control of their wellbeing. BMJ. 2020;369:m1725. [DOI] [PubMed] [Google Scholar]
- 5. Kania K, Abu‐Ghname A, Agrawal N, Maricevich RS. Four strategies for plastic surgery education amidst the COVID‐19 pandemic. Plast Reconstr Surg. 2020;146:252. [DOI] [PubMed] [Google Scholar]
- 6. Stambough JB, Curtin BM, Gililland JM, et al. The past, present, and future of orthopedic education: lessons learned from the COVID‐19 pandemic. J Arthroplasty. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Coe TM, Jogerst KM, Sell NM, et al. Practical techniques to adapt surgical resident education to the COVID‐19 era. Ann Surg. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Chick RC, Clifton GT, Peace KM, et al. Using technology to maintain the education of residents during the COVID‐19 pandemic. J Surg Educ. 2020;77:729‐732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Lewis EE, Taylor LJ, Hermsen JL, McCarthy DP, Fiedler AG. Cardiothoracic education in the time of COVID‐19: how I teach it. Ann Thorac Surg. 2020;110:362‐363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Coyan GN, Kilic A, Gleason TG, et al. Medical student perceptions of a career in cardiothoracic surgery: results of an institutional survey. J Thorac Cardiovasc Surg. 2019;159:1906‐1912. [DOI] [PubMed] [Google Scholar]
- 11. Potts JR. Residency and fellowship program accreditation: effects of the novel coronavirus (COVID‐19) pandemic. J Am Coll Surg. 2020;230:1094‐1097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Fong ZV, Qadan M, McKinney R, et al. Practical implications of novel coronavirus COVID‐19 on hospital operations, board certification, and medical education in surgery in the USA. J Gastrointest Surg. 2020;24:1232‐1236. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting information
Supporting information


