Abstract
Aim and objective
To explore nurses’ experiences regarding shift patterns while providing front‐line care for COVID‐19 patients in isolation wards of hospitals in Shanghai and Wuhan during the novel coronavirus pandemic. Our findings will help to optimise shift work scheduling, use the existing nursing workforce more efficiently and improve nursing quality.
Background
Nurses are one of the main professionals fighting against COVID‐19. Providing care for COVID‐19 patients is challenging. In isolation wards, the workload has increased, and the workflow and shift patterns are completely different from the usual. More importantly, there is a shortage of nurses. Therefore, it is essential and urgent to arrange nurses’ shifts correctly and use the existing workforce resources efficiently.
Design
A qualitative descriptive study of 14 nurses in Chinese hospitals was conducted.
Methods
Semi‐structured interviews were used based on the phenomenological research method; data were analysed using Colaizzi's method of data analysis. This study aligns with the COREQ checklist.
Results
Four themes were extracted: assess the competency of nurses to assign nursing work scientifically and reasonably, reorganise nursing workflow to optimise shift patterns, communicate between managers and front‐line nurses to humanise shift patterns, and nurses’ various feelings and views on shift patterns.
Conclusion
It is necessary to arrange shift patterns scientifically and allocate workforce rationally to optimise nursing workforce allocation, reduce nurses’ workload, improve nursing quality and promote physical and mental health among nurses during the COVID‐19 pandemic.
Relevance to clinical practice
This study emphasised nurses’ experiences on shift patterns in isolation wards, providing useful information to manage shift patterns. Nursing managers should arrange shifts scientifically, allocate nursing workforce rationally, formulate emergency plans and establish emergency response rosters during the COVID‐19 pandemic.
Keywords: COVID‐19, nurses, nursing workforce, qualitative study, shift work schedule
What does this paper contribute to the wider global community?
Nursing managers should evaluate nurses’ competencies and work abilities in advance to arrange the shifts reasonably.
Nursing managers should fully consider the experiences of nurses caring for COVID‐19 patients to arrange shift patterns and scheduling in a reasonable and scientific manner.
Scientifically and reasonably arranged shift patterns optimise nursing workforce allocation, improve nursing quality and promote nurses’ physical and mental health during the COVID‐19 pandemic.
It is crucial to establish an emergency response roster during the COVID‐19 pandemic.
1. INTRODUCTION
Nurses have always played an important role in infection prevention, control, isolation and containment, as well as in public health in general, as initially advocated by Florence Nightingale (Smith, Ng, & Ho, 2020). Today, they have become one of the primary providers of care for patients infected with the coronavirus disease 2019 (COVID‐19) in the fight against the pandemic, which has presented new challenges for nurses.
Traditionally, in nursing, shift work is divided into three 8‐hr shifts per day. However, due to the shortage of nurses in isolation wards during the COVID‐19 pandemic, a pattern of 8‐ to 12‐hr shifts per day has been adopted. A study showed that nurses working shifts of ≥12 hr and those working overtime report lower nursing quality and patient safety (Griffiths et al., 2014).
Moreover, in China, in view of the extreme scarcity of medical protective materials during the early stage of the epidemic, medical workers on the front line overcame difficulties by using such items for the longest possible time. For instance, in order to avoid wasting protective gear, nurses did not drink water for eight hours or more to delay having to go to the restroom.
Nurses are working around the clock and have an increased workload in isolation wards. Thus, crucial problems concerning nursing workforce allocation are the lack of nurses and shift arrangements in nursing posts (Han, Chen, & Li, 2018). Nursing workforce allocation directly affects patient safety and care quality (Dembe, Delbos, & Erickson, 2009). Hence, science‐based and reasonable nursing shift patterns that consider nurses’ perspectives are essential for optimising and utilising nursing workforce effectively, reducing workload and promoting nursing quality and patient care.
2. BACKGROUND
The World Health Organization (WHO) declared the COVID‐19 outbreak a public health emergency of international concern on 30 January 2020 (World Health Organization, 2020a, 2020b). Despite rigorous global containment and quarantine efforts, the incidence of COVID‐19 continues to rise, with 90,870 laboratory‐confirmed cases and over 3,000 deaths as of 3 February 2020 (Sohrabi et al., 2020) and 6, 663, 304 confirmed cases and 392, 802 deaths as of 6 June 2020 worldwide (World Health Organization, 2020a, 2020b). Thus, COVID‐19 presents a vast public health challenge worldwide.
Patients infected with COVID‐19 must be intensively treated in isolation wards. When disaster strikes in one location, help comes from all quarters; thus, nurses from other hospitals all over China volunteered to take care of COVID‐19 patients in Hubei and Wuhan, China. However, during COVID‐19, nursing workflow in isolation wards changed greatly due the widespread outbreak, strong infection and rapid deterioration; that is, it was a challenging situation for nurses.
Nurses caring for COVID‐19 patients in China do not only provide therapeutic nursing (e.g. intravenous infusion and intramuscular injection), but also primary nursing care (e.g. bathing bedridden patients), which increases their workload. Increased workloads, in turn, may lead to increased work stress, patient morbidity and mortality, and incidence of adverse events as well as prolonged patient hospitalisation (Aiken, Clarke, Sloane, Sochalski, & Silber, 2002; Lin, Huang, & Lu, 2013). Therefore, nurses’ responsibilities and workflow in isolation wards must be readjusted immediately to decrease their workload, including shift hours, overtime working hours and actual working hours (Liu, Lee, Chia, Chi, & Yin, 2012).
Nurses not only work long hours in isolation wards due to the shortage of nurses, but also wear protective gear for 8‐ to 12‐hr shifts, which causes dehydration and discomfort. For instance, wearing N95 masks for a long time causes bloody marks on nurses’ faces. Longer work hours are associated with errors and adverse patient outcomes (Ungard, Kroger‐Jarvis, & Davis, 2019). Furthermore, working longer shifts exposed nurses to a higher risk of mental or physical fatigue, increased levels of stress and decreased job performance and care quality (Griffiths et al., 2014; Jarrar, Minai, Al‐Bsheish, Meri, & Jaber, 2019; Matheson, O'Brien, & Reid, 2014; Rogers, Hwang, Scott, Aiken, & Dinges, 2004). Therefore, the shift length must be discussed and organised considering nurses’ perspectives in order to promote high‐quality nursing.
3. AIM
We aim to explore the experiences of nurses who have taken care of COVID‐19 patients in isolation wards in China, specifically regarding shift patterns, with the goal of providing a basis for nursing managers to arrange shifts scientifically and rationally, to reduce work hours and workload, optimise nursing workforce allocation and improve nursing quality and patient care.
4. METHODS
4.1. Study design
A qualitative exploratory descriptive design was followed. Semi‐structured interviews were conducted based on the phenomenological research approach and Colaizzi's seven‐step method; the interviews explored nurses’ experiences regarding shift patterns in isolation wards during the COVID‐19 pandemic. This study aligns with the consolidated criteria for reporting qualitative research (COREQ; Tong, Sainsbury, & Craig, 2007; Appendix S1). Approval was obtained from the hospital ethics committee (Ethical approval number: SH9H‐2020‐TK192‐1). In addition, all participants signed informed consent forms.
4.2. Sampling and participants
The participants were nurses who had volunteered to take care of COVID‐19 patients in isolation wards in the hospitals of Wuhan and Shanghai. A total of fourteen nurses were approached and invited to participate in the study. They were informed of the purpose and importance of the study and they provided their written informed consent before participation. No one dropped out of the study.
Nurses in different hospitals and isolation wards were selected to ensure the representativeness of the sample and data saturation. They were selected through purposive sampling, whereby the researcher consciously selected participants for maximum variation. The age of nurses ranged from 24–43 (33.5 ± 6.0) years, and years of service ranged from 2–23 (11.8 ± 6.9) years, as shown in Table 1.
TABLE 1.
Sociodemographic information of participants (n = 14)
| Characteristics of participants | Descriptions | Numbers |
|---|---|---|
| Age range | 24–43 years | 14 |
| Sex | Male | 1 |
| Female | 13 | |
| Highest educational level | Bachelor's degree | 9 |
| Associate degree | 5 | |
| Professional title | Nurse in charge | 4 |
| Nurse Practitioner | 8 | |
| Registered nurse | 2 | |
| Position | Head nurse | 4 |
| Nurse | 10 | |
| Years of service | 2–5 | 3 |
| 6–10 | 4 | |
| 11–15 | 3 | |
| 16–20 | 2 | |
| More than 20 | 2 | |
| Specialty | Intensive care | 7 |
| Surgical care | 3 | |
| Chronic care | 4 |
4.3. Interviews
The authors consulted relevant literature, two clinicians, two PhDs of Nursing Practice, two clinical nursing experts and two volunteer nurses to revise the interview outline. The final interview guide consisted of six open‐ended questions to explore various aspects of the nurses’ experiences on shift patterns in isolation wards: (a) Please briefly introduce your work experience. (b) Please briefly describe the condition of the hospital and isolation wards where you cared for the COVID‐19 patients. (c) Please briefly introduce the current situation of the nursing workforce and shifts in the isolation wards. (d) What impact do the current shifts have on your work efficiency or work quality? (e) What is the impact of the current shifts on your body and mind? (f) What do you think are the advantages and disadvantages of shifts or what improvements do you hope for shift patterns?
4.4. Data collection
The authors individually contacted fourteen nurses in the isolation wards and provided them with verbal information about the study. The authors and participants were colleagues, which facilitated the process of sharing work experience and ideas with the authors. Semi‐structured, in‐depth interviews based on phenomenological methods were conducted. The results were anonymous, and the participants were represented using numbers to maintain confidentiality.
Due to the high infectivity of COVID‐19, fourteen nurses were interviewed via WeChat video during the 14‐day medical observation period. The interviews took place in quiet rooms with good network conditions, depending on the preference of the participant. They lasted for 60–90 min and were audio taped and later transcribed. During data collection, authors observed and recorded the tone, facial expression, body movement and emotional responses as participants were talking; field notes were written down.
4.5. Data analysis
The data were analysed using Colaizzi's method (Colaizzi, 1978), which comprises the following seven steps: (a) transcribing tape‐recorded interviews verbatim into text and reading the participants’ descriptions multiple times; (b) extracting significant statements from each description; (c) formulating meanings from those significant statements; (d) organising those formulated meanings into themes; (e) integrating the results of the data analysis into a description of the phenomenon under study; (f) returning the results to the participants for validation; and (g) incorporating any new, relevant data into the fundamental structure of the phenomenon (Chesser‐Smyth, 2005).
Data were analysed and clustered into themes and sub‐themes. Significant statements and meanings were extracted and two authors analysed and coded the data to formulate categories, which further enhanced credibility of the interview results.
4.6. Preunderstanding
All the authors are female and have knowledge and experience on qualitative research. The first author (G) is a nurse with a master's degree. J and H are head nurses with master's degrees. L and H both have a PhD in Nursing. Therefore, they could provide the nursing perspective on the research question in focus.
5. RESULTS
Four themes were developed. Sub‐themes were formulated describing the different aspects of nurses’ experiences regarding shift patterns in isolation wards during the COVID‐19 outbreak (Figure 1).
FIGURE 1.
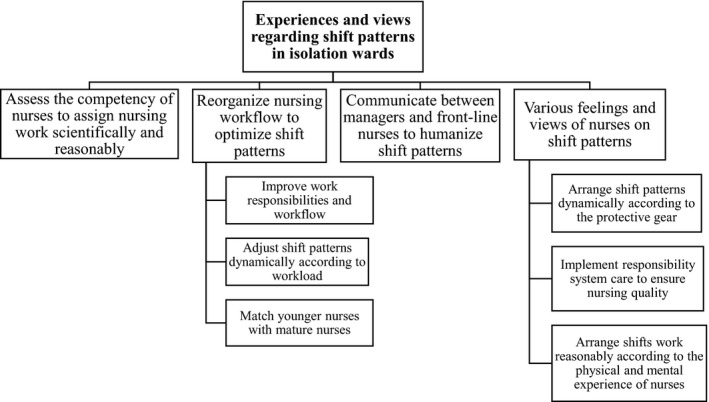
Overview of themes and sub‐themes
5.1. Theme 1: assess the competency of nurses to assign nursing work scientifically and reasonably
The COVID‐19 outbreak is a highly infectious public health event that calls for a large number of healthcare workers to treat and care for the infected patients in isolation wards. Many nurses from all over China have volunteered to work in designated hospitals, purpose‐built hospitals and isolation wards. Moreover, temporary medical teams have been formed to combat the spread of COVID‐19. However, Chinese nurses’ work experience, skills and competency vary. Therefore, nursing managers should evaluate nurses’ professional expertise, position, professional title, age, years of service and competency as soon as possible to assign nursing work scientifically and reasonably, and utilise the existing nursing workforce efficiently.
“Before the assignment, we were basically not asked about our work experience or anything like that.”. (Participant 4)
The nurses who had no experience in intensive care said that they were worried about detecting changes in the patients’ condition in time and using medical equipment (e.g. ventilator and high‐flow oxygen therapy apparatus) correctly in the intensive care isolation unit. However, nurses who had been working in intensive care units were assigned to mild isolation wards, a challenging environment for them. Nursing managers should assign nurses taking in consideration their areas of expertise to ensure effective nursing work.
“I was assigned to A1 isolation ward. I was confused at that time. Because my specialty is intensive care, and I thought I may be assigned to A3 intensive care isolation unit. But I was assigned to A1 isolation ward. The patients in A1 isolation ward are in stable condition and small rely on nurses [for] self‐care ability. Basically patients are able to take care of themselves. If [it were] me, I'd like to make an assessment of nurses’ age, work experience and expertise before I make an arrangement. I will arrange the shifts according to nurses’ work experience, competency, and physical condition, then decide [which] nurses [should] care for the [less serious] or the more serious patients. Later, the head nurse found out my specialty is intensive care and then I was assigned to A3 ICU isolation ward.”. (Participant 1)
5.2. Theme 2: reorganise nursing workflow to optimise shift patterns
The following sub‐themes were discussed: improve work responsibilities and workflow, adjust shift patterns dynamically according to workload and match younger nurses with more experienced nurses.
5.2.1. Improve work responsibilities and workflow
Facing a large number of patients infected with COVID‐19, China immediately set up designated hospitals and isolation wards. The demand for healthcare professionals significantly increased, and changes have taken place in the nursing work to adapt to the situation. Nursing work responsibilities and workflow had to be readjusted and improved in a short period of time for nurses to be able to carry out nursing work orderly.
“This ward is actually a temporary isolation ward. And the head nurse and nurses are transferred from each ward, and we volunteer nurses also come from different hospitals. That is, we don't know this isolation ward and workflow, and we don't have a clue about how to care for those patients. Later we had a meeting every night to discuss and improve the work responsibilities and workflow, and then the head nurse arranged shifts more reasonably.”. (Participant 4)
With the continuous improvement in the work responsibilities and workflow, nurses knew their responsibilities and performed their respective duties by cooperating with each other; thus, nursing work was completed smoothly.
“We were a little passive at first, but after a few days of work, we gradually figured out the rules and were able to take the initiative to complete the nursing work. We grasped the workflow. We find it very difficult when the workflow in not clear. We discuss and finalize the workflow, so the work responsibilities [are] arranged more reasonably and we work more smoothly.”. (Participant 8)
“At first, it was not very clear about the work responsibilities when I came to the isolation ward. That is to say, I did not know what to do at that point. Then the workflow was established, I gradually got familiar with it.”. (Participant 12)
5.2.2. Adjust shift patterns dynamically according to workload
Uncertainties and emergencies have emerged during the COVID‐19 outbreak, which are different from routine clinical nursing work. In the early stage of the epidemic, nurses worked a 8‐ or 12‐hr shifts. In addition, many patients were sent to isolation wards with only one nurse on duty, resulting in an increased workload. Therefore, the head nurses should have dynamically adjusted nurses’ working hours and increased the number of nurses on duty according to the workload to ensure patient safety and care quality.
“I think [I can tolerate] the eight hour working hours. It [was] mainly at the beginning, we [were] not familiar with anything including workflow and environment when we work[ed] in [the] middle and night shifts. So the work efficiency and work quality [were] certainly affected, and we were stressed and tired. In fact, at that time, there were fewer nurses on the middle and night shift, I think the night shift [should have more] nurses. In the middle shift, patients infected with COVID‐19 were constantly sent to the isolation wards for treatment. Four or five patients were sent together. So I have to arrange beds for them, prepare daily necessities, and solve their various problems, and then I need to take venous blood and arterial blood gas analysis [for] test[ing]. Always busy, [it] never stops. In the night shift, I started working at 3:30 and that day I remember there were about 20 venous blood, more than 20 arterial blood gas, and about 40 throat swabs, and I had to give oral medicine to the patients. There was a lot of work to do. The workload is heavy and more nurses are needed.”. (Participant 5)
“At the beginning, [it was a] mess. We adjust[ed] our schedules dynamically. At first, we worked an eight‐hour shift, then we worked a six‐hour shift, finally we settled on a four‐hour shift.”. (Participant 6)
5.2.3. Match younger nurses with more experienced nurses
Volunteer nurses caring for COVID‐19 patients have different working abilities, years of service and professional competences. The study suggested that younger and/or less experienced nurses could work together with mature and experienced nurses to ensure nursing safety and quality. An excellent team and fixed collocation can cultivate tacit understanding and facilitate efficient completion of work.
“There are six critical care groups, and the leaders decide how to match the group members to build an excellent team. There are eight nurses in my group, and low seniority and high seniority nurses match to care for patients together. For example, I have been working for more than 15 years and I was matched with a male nurse [who] worked for three years to care for patients together. Therefore, the leaders allocated nurses according to the combination of high and low seniority nurses, which is conducive to the work.”. (Participant 2)
The fixed combination of senior and junior nurses improves understanding among the team members and work efficiency and reduces low seniority nurses’ performance‐related stress.
“Basically, nurses are fixed and I work together with three other nurses. There are nearly 45 patients in the isolation ward, we know what to do every day, and we have a good match. We can finish the work smoothly.”. (Participant 4)
“[I am] a low seniority nurse. I was afraid that I couldn't take good care of those patients. If there [were] an emergency, there [would] have been a lot of pressure for me. Later, I work[ed] with a high seniority nurse, two nurses cooperat[ing] to improve work efficiency, ensure the quality of nursing, and relieve my pressure.”. (Participant 11)
5.3. Theme 3: Communication between managers and front‐line nurses to humanise shift patterns
Occasionally, nursing managers may neglect first‐line nurses’ opinions due to the rapid development and the urgency of the epidemic, which results in communication difficulties. Therefore, communication should be strengthened to adjust shift patterns appropriately taking front line nurses’ perspectives into consideration.
“A volunteer male nurse think[s] the shifts arrangement is not reasonable. Actually, I know it's really difficult for any head nurse to solve the problem. It is necessary to explore how to arrange the shift arrangement reasonably. And communication is very important.”. (Participant 1)
Head nurses should communicate with front‐line nurses, consider their physical and mental health, and listen to their opinions in order to humanise shift patterns and increase nurses’ work enthusiasm.
“I think to obey the order. For me personally, although I can develop a good habit—a work habit of strict execution and it's also possible to exercise my willpower, actually the head nurse should consider my physical and mental health and listen to my opinions, and then make appropriate scheduling, which is more conducive to my nursing work.”. (Participant 2)
5.4. Theme 4: nurses’ various feelings and views on shift patterns
During the COVID‐19 outbreak, shift patterns are mainly as follows: 4‐ or 8‐hr shifts in contaminated areas (e.g. intensive care isolation wards or mild isolation wards) and 8‐ or 12‐hr shifts in semi‐contaminated areas (e.g. nurse station). There are day shifts, evening shifts and night shifts. All nurses work 40 hr per week. Nurses have varying feelings and views on shift patterns in isolation wards during the COVID‐19 outbreak.
Some nurses support 4‐hr shifts because, although they are drained, time passes very quickly; they do not have to worry about drinking water to delay using the restroom mid‐shift or taking breaks, unlike in 8‐hr shifts; and many aspects of their lives are not limited. Nurses supporting 8‐hr shifts argue that 4‐hr shifts do not guarantee good rest and the longer the shift, the longer they can conserve the protective gear.
Three sub‐themes were discussed: arrange shift patterns dynamically according to protective gear use, reduce shift‐to‐shift handovers to ensure high‐quality nursing and pay attention to nurses’ physical and psychological well‐being.
5.4.1. Arrange shift patterns dynamically according to protective gear use
Protective equipment influences shift patterns’ arrangements and preferences. Nurses expressed that 8‐hr shifts could reduce the use of protective suits, goggles, masks and other protective materials, while 4‐hr shifts could reduce the spread of infection.
“I think the eight hours shift is reasonable because it fits the pattern of all our paramedics in Shanghai. The eight hours shift can reduce the consumption of protective supplies. And there is no problem for nurses who have the experience and competence to care for the patients in severe and critical condition to work eight hours during the epidemic.”. (Participant 1)
“I think the effective time of the mask may only be 4.5 hr. And the goggles are recycled and it fogs easily after using about two hours. So we all voted for the four‐hour shifts.”. (Participant 3)
5.4.2. Reduce shift‐to‐shift handovers to ensure high‐quality nursing
Compared with 4‐hr shifts, 8‐hr shifts can reduce shift‐to‐shift handovers. A reduced number of handovers might have beneficial effects as handovers are associated with errors (Griffiths et al., 2014). Thus, 8‐hr shifts are more conducive to less errors and high‐quality nursing.
“I think the eight‐hour shifts [are] more effective in responsible system nursing and there is also a period of intensive treatment and care for those patients. It will also reduce handover errors compared to the four‐hour shifts. Meanwhile, nurses and doctors can effectively communicate with each other, which play a[n] important role in promoting the treatment and care of patients.”. (Participant 7)
5.4.3. Pay attention to nurses’ physical and psychological well‐being
During the epidemic, nurses felt uncomfortable wearing the protective suits and goggles and were disturbed due to fear of infection and physical discomfort. They also felt anxious because they could not leave the room. Therefore, nursing managers should pay attention to nurses’ physical and psychological well‐being during the shifts.
“I measured my heart rate and oxygen saturation when I [was] wearing the protective gear in the isolation room. Sitting in the chair without moving, my heart rate had reach 120 beats per minute and the oxygen saturation was only 94% to 95%. In addition, protective suits, masks are recommended to change [after] four hours. After more than four hours, there is a concern about whether the protective gear are still effective for me.”. (Participant 6)
“I feel uncomfortable. I wear the protective gear all the time. And I have to wear diapers. I try to adapt to it both physically and mentally.”. (Participant 13)
“I'm capable of working four hours in isolation [both] mentally and physically. But there's a bit of physical and psychological pressure [on] me to care for those patients for eight hours.”. (Participant 8)
6. DISCUSSION
6.1. Allocate shift patterns scientifically and reasonably according to nurses’ competency
Competency refers to individuals’ knowledge, skills, abilities and qualities (Foss, Janken, Langford, & Patton, 2004); nursing competency includes core abilities required for fulfilling one's role as a nurse (Fukada, 2018). Nurses are essential in the healthcare system and they assist as first responders, direct care providers, information providers/educators and mental health counsellors when disasters occur (Chan et al., 2010). Not surprisingly, nurses are playing an important role in nursing care and health education during the COVID‐19 pandemic.
This study found that it is crucial to evaluate nurses’ work ability and professional competence (including age, years of service and expertise) for shift and team arrangement. Work ability is defined as an individual's ability to perform tasks and to meet the required skill and competency levels at work (Suleiman, 2017). Making these evaluations in a timely manner would allow low seniority nurses to benefit from the support of more experienced colleagues and feel less pressure in caring for patients, while high seniority nurses could assist in their areas of professional expertise, where they can be most useful. This would ultimately result in reasonably arranged shifts that optimise the use of the nursing workforce.
Our findings are consistent with previous research indicating that competency could improve job satisfaction and nursing quality, and reduce work pressure (Wu et al., 2018). It has also been reported that mature and experienced nurses working together with younger and/or less experienced nurses could lower fatigue levels, ensure safer practice and ultimately improve nurse well‐being (Yu, Somerville, & King, 2019). Therefore, nursing managers should evaluate volunteer nurses’ competency and work ability before assigning them to the intensive care or mild isolation wards. This will enable them to make efficient use of the nursing workforce, especially during nurse shortages in the COVID‐19 outbreak.
6.2. Make use of the existing nursing workforce more efficiently and formulate emergency plans to optimise nursing workforce allocation and improve nursing quality
The COVID‐19 epidemic is a major public health emergency. The virus has spread faster and wider than any other and is the most difficult to contain. It is both a crisis and a major test for China and worldwide. COVID‐19 is rapidly developing and highly contagious; therefore, infected patients were gathered for treatment and intensive care in isolation wards. Various medical institutions responded positively to set up temporary isolation wards, and nurses volunteered to work there. Nursing managers are faced with great challenges because work responsibilities, workflow, work efficiency, workforce allocation, shifts flexibility and nursing quality should need to be improved in a short period of time to match the current, severe situation.
6.2.1. Implement flexible shifts and fixed allocation to enhance work efficiency and reduces work pressure
Flexible shifts allow to make flexible adjustments while maintaining the basic shift structure. It is based on the hierarchical management to allocate and utilise the existing nursing workforce reasonably, improve work efficiency and ensure nursing quality. A study found that unpredictable shift patterns resulted in higher fatigue levels, compared to regular fixed shifts (Han, Trinkoff, & Geiger‐Brown, 2014). Our study confirms that flexible shifts can guarantee that nurses have time to rest and reduce nurses’ workload and stress, especially during the middle‐of‐the‐day and night shifts.
Further, we found that fixed allocation of less experienced nurses with more experienced ones supplements the less experienced nurses’ ability, improves their work ability and reduces work pressure. It can also cultivate tacit understanding and improve work efficiency.
It has been reported that flexible shifts and fixed allocation can optimise the shifts, provide an efficient work environment, ensure nurses have sufficient time to recuperate and improve quality of healthcare and patients’ outcomes (Butler et al., 2019). Therefore, nursing managers should implement flexible shifts and fixed allocation according to the number and condition of infected patients, workload and nursing workforce.
6.2.2. Optimise the nursing workflow and formulate emergency plan to carry out emergency work in an orderly manner
This study found that workflow and responsibilities in isolation wards are not clear in the early stages of the epidemic. However, nursing managers and nurses continued to explore and communicate with each other. The workflow had been optimised by the second week of work, and the solidarity and cooperation between nurses promoted the nursing work to be carried out efficiently, which improved the work efficiency and nursing quality. The standardised workflow is helpful for nurses to carry out their work quickly, efficiently, accurately and orderly, and it can optimise nursing workforce allocation and improve the quality of nursing. In addition, once the work responsibilities and workflow are stated, nursing managers should conduct timely training for nurses to ensure the adequate implementation of workflow.
Importantly, the COVID‐19 outbreak has inspired nursing managers to formulate emergency plans, establish emergency nursing teams and carry out emergency knowledge and skills training as well as simulation exercises for nurses, which are important measures to respond to emergencies effectively. Studies have shown that nurses’ emergency knowledge and skills come largely from practice and training (Al Thobaity, Plummer, Innes, & Copnell, 2015; Labrague et al., 2018). Moreover, it is not only necessary to train nurses’ specialised knowledge, skills and emergency capabilities, but also to identify training needs in first aid, field triage, advanced basic life support and infection control (Fung, Loke, & Lai, 2008; Labrague, Yboa, McEnroe‐Petitte, Lobrino, & Brennan, 2016). Moreover, palliative care training is essential during the COVID‐19 pandemic (Borasio, Gamondi, Obrist, Jox, & For, 2020). Therefore, nursing managers should optimise the workflow and clarify work responsibilities as soon as possible according to the epidemic situation and the characteristics of the isolation wards. Summarising experience, formulating emergency plans and building emergency teams should be implemented in preparation for emergencies.
6.3. Strengthen the communication between nursing managers and front‐line nurses to meet the needs of nurses and arrange shifts humanely
Due to a severe shortage of nurses during the early stage of the COVID‐19 epidemic, nursing managers could not take into account nurses’ personal needs when scheduling shifts. The situation had improved with the increase of volunteer nurses and the strengthening of communication. Nurses expressed that they took the initiative to communicate with the nursing managers if shifts were unreasonable or they felt tired; nursing managers responded by trying to accommodate their needs and making reasonable schedules.
Communication between nurses and nursing managers affects shifts’ arrangements and helps to understand nurses’ professional perspective (Gan, 2019). Moreover, nursing managers must carefully review current shift patterns and examine their impact on nurses’ physical condition to guarantee nursing quality and patients safety (Min, Min, & Hong, 2019; Stimpfel, Fatehi, & Kovner, 2020). Strengthening the communication between nursing managers and front‐line nurses would allow the accommodation of nurses’ needs while arranging shifts as humanely as possible.
6.4. Provide psychological strategies to promote nurses’ physical and mental health
Nursing work is physically and mentally laborious (Barker & Nussbaum, 2011). During the COVID‐19 outbreak, nurses providing front‐line care for infected patients in isolation wards in China are at higher risk of infection and stress. They are work around the clock, wear protective gear (e.g. suits, goggles, N95 masks, and gloves) that impedes drinking water or using the restroom for four to eight hours, which easily causes discomfort (e.g. hypoxia), wear diapers or refraining from eating to avoid taking breaks and shave their hair to reduce the spread of infection and to change into protective gear more quickly (Smith et al., 2020; Thiagarajan, 2020). At the same time, nurses are witnessing the death of patients and facing the risk of respiratory transmission. Therefore, it is understandable that their bodies and minds are under great pressure.
A study showed that medical staff show psychological stress disorder, anxiety and depression during disasters or one to two weeks after an outbreak (Kenny & Hull, 2008). COVID‐19 will undoubtedly have psychological impacts for healthcare workers; front‐line workers will be particularly at risk (Kang et al., 2020; Khan et al., 2020). This can be addressed by strengthening the psychological intervention mechanism, that is the psychological preparation of nurses, in addition to their knowledge and skills (Said & Chiang, 2020). Studies emphasise strategies and interventions need to be provided to mitigate the impacts of COVID‐19 on mental health by protecting, supporting and promoting the psychological well‐being of front‐line healthcare workers at times of widespread crisis (Albott et al., 2020; Blake, Bermingham, Johnson, & Tab ner, 2020). Thus, to preserve nurses’ mental and physical health, nursing managers should allocate nursing workforce reasonably, reduce their workload and pressure, strengthen psychological assessment and intervention, train nurses in self‐psychological adjustment and provide psychological strategies during and after the outbreak.
7. CONCLUSION
A phenomenological design was used in the study. The interviews revealed the experiences of nurses providing front‐line care for COVID‐19 patients in isolation wards, particularly regarding shift patterns during the pandemic. We found that it was necessary to assess nurses’ competency in advance to assign nursing work scientifically and reasonably, to reorganise nursing workflow and optimise shift patterns, to strengthen communication between managers and front‐line nurses to humanise shift patterns, and to consider nurses’ feelings and views on shift patterns. Nursing managers should allocate and utilise nursing workforce reasonably and efficiently according to the pandemic and patients’ conditions, arrange and optimise shifts flexibly and humanely, and promote nurses’ physical and mental health. Importantly, emergency plans, teams and trainings should be developed to respond to emergency disasters and provide assistance in an effective manner.
8. RELEVANCE TO CLINICAL PRACTICE
Nurses’ experiences and views on shift patterns during an emergency are essential to improve work efficiency and nursing quality. This study emphasises the views and experiences of nurses providing front‐line care for COVID‐19 patients in isolation wards. Our findings provide a basis for nursing managers to arrange shifts scientifically and optimise nursing workforce allocation. Nurses' competency, specialty, workflow, workload and preferences should be considered by nursing managers when arranging teams and shifts. Moreover, communication between nurses and nursing managers should be strengthened. Nursing managers should allocate nursing workforce rationally and formulate emergency plans to respond to emergencies.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest.
AUTHOR CONTRIBUTIONS
(a) The idea and design of this research were performed through collaboration among all five authors. (b) The collection, analysis and interpretation of the data came from Gao, Jiang and Hou. (c) Gao, Li and Hou contributed to the drafting, writing and revising the manuscript. (d) All five authors have approved this version for publication.
Supporting information
Appendix S1
ACKNOWLEDGEMENTS
We sincerely thank the nurses providing front‐line care for patients infected with COVID‐19 and also thank them for willingly and freely shared their experiences.
Gao X, Jiang L, Hu Y, Li L, Hou L. Nurses’ experiences regarding shift patterns in isolation wards during the COVID‐19 pandemic in China: A qualitative study. J Clin Nurs. 2020;29:4270–4280. 10.1111/jocn.15464
Lili Hou and Li Li have contributed equally to this work, and their contributions are the same.
Xiaoyue Gao is the first author and Lili Jiang is the co‐first author, they have contributed equally to this work and their contributions are the same.
Funding information
This study was funded by Shanghai Jiao Tong University (Grant Number 2020RK41) and Science and Technology Commission of Shanghai Municipality (Grant Number 20692104700).
Contributor Information
Li Li, Email: pisces_liz@163.com.
Lili Hou, Email: lil212001@sh9hospital.org.cn.
REFERENCES
- Aiken, L. H. , Clarke, S. P. , Sloane, D. M. , Sochalski, J. , & Silber, J. H. (2002). Hospital nurse staffing and patient mortality, nurse burnout, and job dissatisfaction. The Journal of the American Medical Association, 288(16), 1987–1993. 10.1001/jama.288.16.1987 [DOI] [PubMed] [Google Scholar]
- Al Thobaity, A. , Plummer, V. , Innes, K. , & Copnell, B. (2015). Perceptions of knowledge of disaster management among military and civilian nurses in Saudi Arabia. Australasian Emergency Nursing Journal, 18(3), 156–164. 10.1016/j.aenj.2015.03.001 [DOI] [PubMed] [Google Scholar]
- Albott, C. S. , Wozniak, J. R. , McGlinch, B. P. , Wall, M. H. , Gold, B. , … Vinogradov, S. . (2020). Battle buddies: Rapid deployment of a psychological resilience intervention for health care workers during the COVID‐19 pandemic. Anesthesia & Analgesia, 131(1), 43–54. 10.1213/ANE.0000000000004912 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barker, L. M. , & Nussbaum, M. A. (2011). Fatigue, performance and the work environment: A survey of registered nurses. Journal of Advanced Nursing, 67(6), 1370–1382. 10.1111/j.1365-2648.2010.05597.x [DOI] [PubMed] [Google Scholar]
- Blake, H. , Bermingham, F. , Johnson, G. , & Tabner, A. (2020). Mitigating the psychological impact of COVID‐19 on healthcare workers: A digital learning package. International Journal of Environmental Research and Public Health, 17(9), 2997. 10.3390/ijerph17092997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borasio, G. D. , Gamondi, C. , Obrist, M. , Jox, R. , & For, T. C. F. O. (2020). COVID‐19: Decision making and palliative care. Swiss Medical Weekly, 150, w20233. 10.4414/smw.2020.20233 [DOI] [PubMed] [Google Scholar]
- Butler, M. , Schultz, T. J. , Halligan, P. , Sheridan, A. , Kinsman, L. , Rotter, T. , … Drennan, J. (2019). Hospital nurse‐staffing models and patient‐ and staff‐related outcomes. Cochrane Database Systemic Review, 4, D7019. 10.1002/14651858.CD007019.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan, S. S. S. , Chan, W.‐S. , Cheng, Y. , Fung, O. W. M. , Lai, T. K. H. , Leung, A. W. K. , … Pang, S. M. C. (2010). Development and evaluation of an undergraduate training course for developing International Council of Nurses disaster nursing competencies in China. Journal of Nursing Scholarship, 42(4), 405–413. 10.1111/j.1547-5069.2010.01363.x [DOI] [PubMed] [Google Scholar]
- Chesser‐Smyth, P. A. (2005). The lived experiences of general student nurses on their first clinical placement: A phenomenological study. Nurse Education and Practice, 5(6), 320–327. 10.1016/j.nepr.2005.04.001 [DOI] [PubMed] [Google Scholar]
- Colaizzi, P. F. (1978). Psychological research as the phenomenologist views it. In Valle R., & King M. (Eds.), Existential phenomenological alternatives for psychologists. New York: Oxford University Press. [Google Scholar]
- Dembe, A. E. , Delbos, R. , & Erickson, J. B. (2009). Estimates of injury risks for healthcare personnel working night shifts and long hours. Quality and Safety Health Care, 18(5), 336–340. 10.1136/qshc.2008.029512 [DOI] [PubMed] [Google Scholar]
- Foss, G. F. , Janken, J. K. , Langford, D. R. , & Patton, M. M. (2004). Using professional specialty competencies to guide course development. Journal of Nursing Education, 43(8), 368–375. 10.3928/01484834-20040801-03 [DOI] [PubMed] [Google Scholar]
- Fukada, M. (2018). Nursing competency: Definition, structure and development. Yonago Acta Medica, 61(1), 1–7. 10.33160/yam.2018.03.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fung, O. W. , Loke, A. Y. , & Lai, C. K. (2008). Disaster preparedness among Hong Kong nurses. Journal of Advanced Nursing, 62(6), 698–703. 10.1111/j.1365-2648.2008.04655.x [DOI] [PubMed] [Google Scholar]
- Gan, I. (2019). How do nurses' work arrangements influence nurse managers' communication? A qualitative study. Journal of Nursing Management, 27(7), 1366–1373. 10.1111/jonm.12817 [DOI] [PubMed] [Google Scholar]
- Griffiths, P. , Dall’Ora, C. , Simon, M. , Ball, J. , Lindqvist, R. , Rafferty, A.‐M. , … Aiken, L. H. (2014). Nurses' shift length and overtime working in 12 European countries: The association with perceived quality of care and patient safety. Medical Care, 52(11), 975–981. 10.1097/MLR.0000000000000233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han, B. , Chen, X. , & Li, Q. (2018). Application of case mix index in the allocation of nursing human resources. Journal of Nursing Management, 26(6), 647–652. 10.1111/jonm.12593 [DOI] [PubMed] [Google Scholar]
- Han, K. , Trinkoff, A. M. , & Geiger‐Brown, J. (2014). Factors associated with work‐related fatigue and recovery in hospital nurses working 12‐hour shifts. Workplace Health Safety, 62(10), 409–414. 10.3928/21650799-20140826-01 [DOI] [PubMed] [Google Scholar]
- Jarrar, M. , Minai, M. S. , Al‐Bsheish, M. , Meri, A. , & Jaber, M. (2019). Hospital nurse shift length, patient‐centered care, and the perceived quality and patient safety. International Journal of Health Planning Management, 34(1), e387–e396. 10.1002/hpm.2656 [DOI] [PubMed] [Google Scholar]
- Kang, L. , Ma, S. , Chen, M. , Yang, J. , Wang, Y. , Li, R. , … Liu, Z. (2020). Impact on mental health and perceptions of psychological care among medical and nursing staff in Wuhan during the 2019 novel coronavirus disease outbreak: A cross‐sectional study. Brain, Behavior, and Immunity, 87, 11–17. 10.1016/j.bbi.2020.03.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kenny, D. J. , & Hull, M. S. (2008). Critical care nurses’ experiences caring for the casualties of war evacuated from the front line: Lessons learned and needs identified. Critical Care Nursing Clinics North America, 20(1), 41–49. 10.1016/j.ccell.2007.10.013 [DOI] [PubMed] [Google Scholar]
- Khan, S. , Siddique, R. , Li, H. , Ali, A. , Shereen, M. A. , Bashir, N. , & Xue, M. (2020). Impact of coronavirus outbreak on psychological health. Journal of Global Health, 10(1), 10331. 10.7189/jogh.10.010331 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Labrague, L. J. , Hammad, K. , Gloe, D. S. , McEnroe‐Petitte, D. M. , Fronda, D. C. , Obeidat, A. A. , … Mirafuentes, E. C. (2018). Disaster preparedness among nurses: A systematic review of literature. International Nursing Review, 65(1), 41–53. 10.1111/inr.12369 [DOI] [PubMed] [Google Scholar]
- Labrague, L. J. , Yboa, B. C. , McEnroe‐Petitte, D. M. , Lobrino, L. R. , & Brennan, M. G. (2016). Disaster preparedness in Philippine nurses. Journal of Nursing Scholarship, 48(1), 98–105. 10.1111/jnu.12186 [DOI] [PubMed] [Google Scholar]
- Lin, C. , Huang, H. , & Lu, M. (2013). The Development of nursing workforce allocation standards for acute care general wards in Taiwan. Journal of Nursing Research, 21(4), 298–306. 10.1097/jnr.0000000000000002 [DOI] [PubMed] [Google Scholar]
- Liu, L. , Lee, S. , Chia, P. , Chi, S. , & Yin, Y. (2012). Exploring the association between nurse workload and nurse‐sensitive patient safety outcome indicators. Journal of Nursing Research, 20(4), 300–309. 10.1097/jnr.0b013e3182736363 [DOI] [PubMed] [Google Scholar]
- Matheson, A. , O'Brien, L. , & Reid, J. A. (2014). The impact of shiftwork on health: A literature review. Journal of Clinical Nursing, 23(23–24), 3309–3320. 10.1111/jocn.12524 [DOI] [PubMed] [Google Scholar]
- Min, A. , Min, H. , & Hong, H. C. (2019). Work schedule characteristics and fatigue among rotating shift nurses in hospital setting: An integrative review. Journal of Nursing Management, 27(5), 884–895. 10.1111/jonm.12756 [DOI] [PubMed] [Google Scholar]
- Rogers, A. E. , Hwang, W. T. , Scott, L. D. , Aiken, L. H. , & Dinges, D. F. (2004). The working hours of hospital staff nurses and patient safety. Health Affairs (Millwood), 23(4), 202–212. 10.1377/hlthaff.23.4.202 [DOI] [PubMed] [Google Scholar]
- Said, N. B. , & Chiang, V. (2020). The knowledge, skill competencies, and psychological preparedness of nurses for disasters: A systematic review. International Emergency Nursing, 48, 100806. 10.1016/j.ienj.2019.100806 [DOI] [PubMed] [Google Scholar]
- Smith, G. D. , Ng, F. , & Ho, C. L. W. (2020). COVID‐19: Emerging compassion, courage and resilience in the face of misinformation and adversity. Journal of Clinical Nursing, 29(9–10), 1425–1428. 10.1111/jocn.15231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sohrabi, C. , Alsafi, Z. , O'Neill, N. , Khan, M. , Kerwan, A. , Al‐Jabir, A. , … Agha, R. (2020). World Health Organization declares global emergency: A review of the 2019 novel coronavirus (COVID‐19). International Journal of Surgery, 76, 71–76. 10.1016/j.ijsu.2020.02.034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stimpfel, A. W. , Fatehi, F. , & Kovner, C. (2020). Nurses' sleep, work hours, and patient care quality, and safety. Sleep Health, 6(3), 314–320. 10.1016/j.sleh.2019.11.001 [DOI] [PubMed] [Google Scholar]
- Suleiman, A. M. (2017). Occupational safety and health professionals' work ability concept perception and comprehension of regulations. Work, 56(3), 483–490. 10.3233/WOR-172514 [DOI] [PubMed] [Google Scholar]
- Thiagarajan, S. (2020). Coronavirus: Nurses shave their hair and wear adult diapers for maximum work efficiency. Mothership. Retrieved from: https://mothership.sg/2020/02/Chinese‐female‐nurses‐shave‐their‐hair/ [Google Scholar]
- Tong, A. , Sainsbury, P. , & Craig, J. (2007). Consolidated criteria for reporting qualitative research (COREQ): A 32‐item checklist for interviews and focus groups. International Journal for Quality in Health Care, 19(6), 349–357. 10.1093/intqhc/mzm042 [DOI] [PubMed] [Google Scholar]
- Ungard, W. , Kroger‐Jarvis, M. , & Davis, L. S. (2019). The Impact of shift length on mood and fatigue in pediatric registered nurses. Journal of Pediatric Nursing, 47, 167–170. 10.1016/j.pedn.2019.05.014 [DOI] [PubMed] [Google Scholar]
- World Health Organization (2020). Statement on the second meeting of the International Health Regulations (2005) Emergency Committee concerning the outbreak of novel coronavirus (2019‐ncov). Retrieved from https://www.who.int/news‐room/detail/30‐01‐2020‐statement‐on‐the‐second‐meeting‐of‐the‐international‐health‐regulations‐(2005)‐emergency‐committee‐regarding‐the‐outbreak‐of‐novel‐coronavirus‐(2019‐ncov) [Google Scholar]
- World Health Organization (2020). Coronavirus disease (COVID‐2019) situation reports: Situation Report – 138. Retrieved from https://www.who.int/docs/default‐source/coronaviruse/situation‐reports/20200606‐covid‐19‐sitrep‐138.pdf?sfvrsn=c8abfb17_4 [Google Scholar]
- Wu, X. , Li, J. , Liu, G. , Liu, Y. , Cao, J. , & Jia, Z. (2018). The effects of emotional labor and competency on job satisfaction in nurses of China: A nationwide cross‐sectional survey. International Journal of Nursing Sciences, 5(4), 383–389. 10.1016/j.ijnss.2018.08.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu, F. , Somerville, D. , & King, A. (2019). Exploring the impact of 12‐hour shifts on nurse fatigue in intensive care units. Applied Nursing Research, 50, 151191. 10.1016/j.apnr.2019.151191 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1


