A 69‐year‐old woman presented to the emergency department with central dull chest pain. Electrocardiography revealed Q waves and ST elevation in the inferior leads and cardiac troponin I was elevated at 1506 ng/L (normal range <10). She was taken for emergent coronary angiography, which demonstrated chronic occlusion of her right coronary artery, left ventricular ejection fraction of 34% and basal hyperkinesis with mid‐ventricular and apical dyskinesis consistent with takotsubo syndrome (Fig. 1).
FIGURE 1.
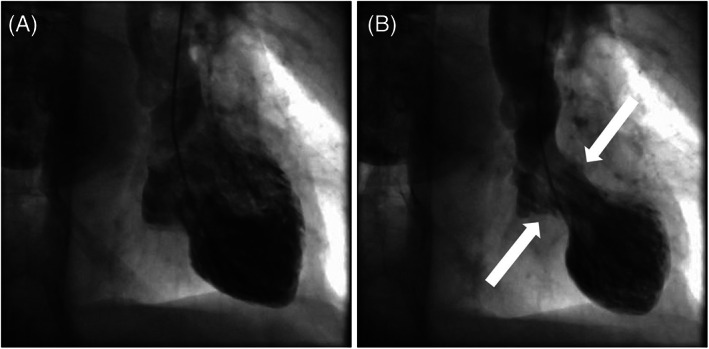
Left ventriculogram images in (A) diastole and (B) systole demonstrating basal hyperkinesis (white arrows) and apical ballooning pathognomonic for takotsubo syndrome.
Relevant background medical history included stage 1 non‐small‐cell lung cancer treated with surgical wedge resection. Fifteen months post‐resection, surveillance computed tomography (CT) of the chest demonstrated a new spiculated nodule. After discussion with the patient, a CT‐guided biopsy was arranged. Due to the implementation of the COVID‐19 pandemic lockdown, the post‐biopsy clinic appointment was changed to a phone consultation. During the phone consultation the patient was informed that the biopsy demonstrated recurrence of lung adenocarcinoma. The patient later stated that since the phone conversation, she had been excessively worrying about the diagnosis and prognosis. To the best of our knowledge, this is the first reported case of an adverse outcome possibly exacerbated by replacing an in‐patient consultation with a phone consult.
The COVID‐19 pandemic has caused major disruption to almost every facet of life. Early studies indicate that social distancing restrictions are having a major impact on the psychological well‐being of patients. 1 Simultaneously, the same restrictions are also imposing limitations on the delivery of ‘standard’ healthcare services. Many hospitals have chosen to cancel in‐person outpatient visits and instead replaced them with telemedicine. However, the change in circumstances has been so rapid that many institutions, including ours, are still in the infancy stages of implementing an important aspect of telemedicine (video communication). Not surprisingly, many outpatient consultations are being conducted entirely through phone conversation. 2 While video communication has benefits in comparison to telephone consultation, its inadequacies in ‘breaking bad news’ are stark. Wolf et al. highlighted some of the concerning issues during the COVID‐19 pandemic. 3 With no control over the setting in which news is delivered, patients can answer a telemedicine call while in public organising essentials, or in self‐isolation without support from family or friends. Many patients require assistance in setting up digital platforms to enable telemedicine to occur, and the potential for technological interruptions during key parts of discussion can add to patient distress.
Telemedicine has numerous benefits such as reduced costs to health services and most importantly high patient satisfaction, 4 and although there are campaigns advocating for telemedicine to be a new standard of care, lack of face‐to‐face communication could potentially exacerbate a patient's anxiety, particularly in an at‐risk individual. Our patient was an ‘at‐risk’ patient, as a recent review by Desail et al. highlighted the emotional turmoil and inflammatory state of malignancy as potential triggers for takotsubo syndrome in cancer patients. 5 Phone consultations come at the expense of the lack of non‐verbal cues, which can be of paramount importance to physicians when ‘breaking bad news’ to a patient.
Our patient was commenced on bisoprolol, ramipril, aspirin, received inpatient psychology review, which is routine at our institution, and was discharged with outpatient cardiac rehabilitation follow up arranged. This report highlights that while telemedicine/phone consultation can be extremely useful, it can be challenging for patients. There is an urgent need for the development of best practice guidelines and resources to mitigate patients' anxiety associated with phone and telemedicine consultation.
Acknowledgements
We are grateful to the patient of the Gold Coast University Hospital Health Service, Gold Coast, Australia, for her consent for this manuscript.
References
- 1. Hao X, Zhou D, Li Z, Zeng G, Hao N, Li E et al. Severe psychological distress among epilepsy patients during the COVID‐19 outbreak in southwest China. Epilepsia 2020; 61: 1166–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Rajasekaran K. Access to telemedicine: are we doing all that we can during the COVID‐19 pandemic? OtolaryngolHead Neck Surg 2020; 163:104–6. [DOI] [PubMed] [Google Scholar]
- 3. Wolf I, Waissengrin B, Pelles S. Breaking bad news via telemedicine: a new challenge at times of an epidemic. Oncologist 2020; 25: e879–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Cain SM, Moore R, Sturm L, Mason T, Fuhrman C, Smith R et al. Clinical assessment and management of general surgery patients via synchronous telehealth. J Telemed Telecare 2017; 23: 371–5. [DOI] [PubMed] [Google Scholar]
- 5. Desail A, Noor A, Joshi S, Kim AS. Takotsubo cardiomyopathy in cancer patients. Cardio‐Oncology 2019; 5: 7. [DOI] [PMC free article] [PubMed] [Google Scholar]


