Graphical Abstract
The battle of COVID-19 is currently at different levels of intensity in each country and even each city. The authors have prepared succinct recommendations regarding the care of patients with breast cancer, divided into phases that can easily be adapted to each units' needs and resources, and stepped up or stepped down according to escalating and de-escalating circumstances. The structure can also be transposed easily to different cancer types, enabling continued provision of best standards of care despite unprecedented stressors.
Graphical Abstract.
Surgery must go on
Introduction
Globally, the COVID-19 pandemic has proven to be an unpredictable enemy imposing unprecedented challenges. The multidisciplinary breast cancer team at the National University Hospital, Singapore, a tertiary academic medical centre, manages about 600 patients with breast cancer annually. Resource and manpower diversions for COVID-19 services have resulted in loss of clinic assistants, inpatient beds, operating theatres and specialty-trained staff. Daily operations were adapted to allow continuation of provision of standard of care without an impending backlog.
Implementation of COVID-19 strategies started on 20 February 2020. During March 2020, the team was able to decrease the outpatient load by more than 50 per cent without compromising cancer detection rates. By better screening of referrals, a doubling of the proportion of oncological patients was seen compared with the average month before COVID-19. The use of telecommunication resulted in deferral and discharge of around 200 patients, while all patients continued to be treated with a high standard of care.
Here, this experience is shared, with guidance on functional operations that may be adopted in other healthcare systems worldwide experiencing similar stressors. The recommendations are divided into four phases according to the COVID-19 situation, allowing easy adaptation to the local context.
Recommendations
The operational recommendations of the unit were developed after reviewing available guidelines1–4 with the following priorities: patient safety and oncological outcomes; staff safety; and rationing of resources, prioritizing timely detection of cancers whose delayed diagnosis could significantly affect patient prognosis and survival.
Caveats
These recommendations should not supersede clinician judgement and individualized care, and should align with institutional guidelines. Multidisciplinary tumour board (MTB) discussions for fair allocation are essential when resources are limited.
Phases
Recommendations are divided into four phases depending on a country's COVID-19 status.
Phase 1: semiurgent setting
Disease is severe and spreads easily between people, but there is no community spread. Hospital resources are ample, institutions have sufficient ICU beds and ventilator capacity, and the COVID-19 trajectory is not escalating rapidly. Operational changes are at the institutional level, and focus on streamlining and preparedness.
Phase 2: urgent setting
Disease is severe, with contained community spread. Large but controlled numbers of patients who are positive for COVID-19 do not overwhelm the system in terms of ICU beds, ventilator capacity and medical supplies, with evidence of control reflected as dwindling case numbers.
Phase 3: lockdown
Disease is severe, with uncontained community spread seen as a spike of cases even with measures in place. Systems are strained though adequate, with significant rerouting of resources to COVID-19 care.
Phase 4: uncontrolled pandemic
Disease is severe with uncontrolled spread. Resources are exhausted despite being fully routed to COVID-19 care.
Outpatient breast services
All services are specialist run (clinics, operations, radiation and chemotherapy administration), allowing redeployment of undifferentiated staff for COVID-19 care. A centralized appointment line was set up to screen referrals from within and outside the hospital. Patients are triaged into three groups based on the likelihood of having cancer: urgent (review within the week), early (1–2 weeks) and non-essential (3–6 months). Non-oncological operations are reviewed by telecommunication and deferred accordingly. Medical tourism is disallowed at an institutional level and second-opinion consultations from other sites discouraged. Prioritization of outpatient breast services is summarized in Fig. 1.
Fig. 1.
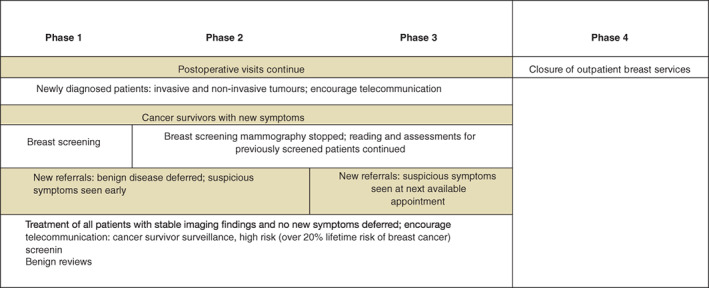
Patient prioritization for breast clinics during COVID-19 pandemic
Screening
Mammographic screening was discontinued when entering phase 2, with the rationale that the majority of screen-detected disease is oestrogen receptor-positive, with less aggressive tumours and slower progression, so missing early disease is less likely to have a broad impact on subsequent survival. The compromise will, however, always exist, that a small portion of patients will eventually require more treatment, which may have been avoidable with screening.
Telecommunication
All meetings including MTBs are held virtually using teleconferencing tools with an institutional account on a virtual private network. Patient telecommunication methods comprise traditional telephone calls, e-mails or teleconferencing tools. Staff were provided with telecommunication training (verification of patient identity, dissemination of information regarding safety measures for COVID-19, reassurance regarding quality of care) in order to contact patients for counselling, symptom review and, if appropriate, deferral of appointments together with return advice and contact information. Clear documentation is essential to ensure continuity of care.
Surgical oncology
If possible, surgery is deferred to optimize manpower and resource reallocation, with the judicious use of neoadjuvant chemotherapy (NACT) and neoadjuvant endocrine therapy (NAET). Operations are scheduled in the morning to facilitate same-day discharges. Reconstruction should be limited to those requiring a hospital stay not exceeding 48 h or delayed as appropriate. Patients with higher perioperative risks that potentially necessitate high-dependency or intensive care should be deferred to NACT/NAET if possible, as these are the most valuable resources for treatment during the COVID-19 pandemic. Prioritization of breast surgery is summarized in Fig. 2.
Fig. 2.
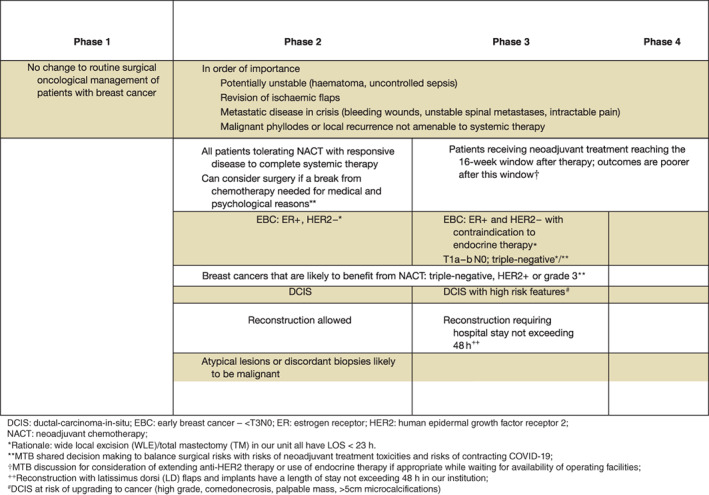
Patient prioritization for breast surgery during COVID-19
Postoperative care
Established pathways and trained breast-care nurses allowed postoperative visits to be limited (Appendix S1, supporting information). Same-day adjuvant therapy appointments were organized to minimize hospital visits.
Adjuvant treatment
The time-sensitive nature of adjuvant therapy and fractionated nature of radiotherapy (RT) pose unique challenges5. The goal is to minimize patients' exposure to COVID-19, without compromising oncological outcomes while limiting the burden on strapped resources. Heightened measures of infection control and screening for COVID-19 are undertaken on oncological floors, where teams are given direct access to pandemic teams to test and treat suspect cases. Telecommunication with appropriate triaging is supported by mobile pharmacies. Continued shared decision-making, in terms of survival benefits from treatment balanced against risks of treatment toxicities and susceptibility to COVID-19, is prioritized. Treatment of patients for whom adjuvant therapy did not confer proven survival benefit was deferred.
Medical oncology
Inpatient chemotherapy is limited to exceptional cases for bed conservation. Adapted regimens that are less myelosuppressive or require shorter infusion times are preferred, with use of oral and subcutaneous (instead of intravenous) formulations wherever possible. Granulocyte colony stimulating factor as primary prophylaxis is considered for high-risk regimens to decrease risks of complications.
Radiation oncology
Hypofractionated schedules for adjuvant breast RT are preferred6. In phase 3, adjuvant RT can be delayed up to 3 months after surgery7–9, and boost RT omitted in selected patients10. Omission of adjuvant RT in low-risk patients with negligible survival benefits should be discussed11. Palliative RT is reserved for crises such as spinal cord compression, uncontrolled bleeding from fungating tumours and intractable pain.
Impact of interventions owing to COVID-19 on breast cancer services
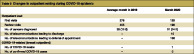
Table 1 shows the improvement in proportion of patients with breast cancer and efficiency of telemedicine and triaging. Strategies were implemented on 20 February 2020. In March 2020, the outpatient load decreased by more than 50 per cent without compromising cancer detection rates. A doubling of the proportion of oncological cases with a mean waiting time from referral to specialist visit of 5 days was seen. Telecommunication resulted in deferral and discharge of around 200 patients. All patients continued to be treated according to standard of care.
Table 1.
Changes in outpatient setting during COVID-19 epidemic
| Average month in 2019 | March 2020 | |
|---|---|---|
| Outpatient load | ||
| First visits | 278 | 128 |
| Review visits | 405 | 199 |
| No. of cancers diagnosed | 35 (12·6) | 31 (24·2) |
| No. of telecommunications leading to discharge | – | 10 |
| No. of telecommunications leading to deferral of appointment | – | 198 |
| COVID-19-related (breast outpatient) | ||
| No. of COVID-19 swabs | – | 1 |
| No. of confirmed COVID-19 cases | – | 0 |
Values in parentheses are percentages. Numbers exclude all metastatic disease.
Looking past COVID-19
Streamlining of the service has made the authors' unit more efficient without compromising standards of care. Looking past COVID-19, they will continue to adopt telecommunication, provide better training for primary healthcare partners, and streamline patient flows in the hospital.
Supplementary Material
Appendix S1: Supporting information
Acknowledgements
The authors acknowledge the breast care team at National University Hospital for collating the operational numbers used to complete Table 1, and for their continued efforts to provide the best care for patients.
Disclosure: The authors declare no conflict of interest.
References
- 1. American College of Surgeons; COVID-19 Pandemic Breast Cancer Consortium . COVID-19: Elective Case Triage Guidelines for Surgical Care; 2020. https://www.facs.org/covid-19/clinical-guidance/elective-case/breast-cancer [accessed 16 April 2020]. [Google Scholar]
- 2. American College of Surgeons; COVID-19 Pandemic Breast Cancer Consortium . Recommendations for Prioritization, Treatment and Triage of Breast Cancer Patients During the COVID-19 Pandemic: Executive Summary; 2020. https://www.facs.org/quality-programs/cancer/executive-summary [accessed 16 April 2020]. [Google Scholar]
- 3. Tey J, Ho S, Choo BA, Ho F, Yap SP, Tuan JKLet al. Navigating the challenges of the COVID-19 outbreak: perspectives from the radiation oncology service in Singapore. Radiother Oncol 2020; 148: 189–193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Marron JM, Joffe S, Jagsi R, Spence RA, Hlubocky FJH. Ethics and resource scarcity: ASCO recommendations for the oncology community during the COVID19 pandemic. J Clin Oncol 2020; 10.1200/JCO.20.00960 [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 5. European Society for Medical Oncology . ESMO Management and Treatment Adapted Recommendations in the COVID-19 Era: Breast Cancer; 2020. https://www.esmo.org/guidelines/cancer-patient-management-during-the-covid-19-pandemic/breast-cancer-in-the-covid-19-era [accessed 15 April 2020]. [Google Scholar]
- 6. Haviland JS, Owen JR, Dewar JA, Agrawal RK, Barrett J, Barrett-Lee PJet al. ; START Trialists' Group . The UK Standardisation of Breast Radiotherapy (START) trials of radiotherapy hypofractionation for treatment of early breast cancer: 10-year follow-up results of two randomised controlled trials. Lancet Oncol 2013; 14: 1086–1094. [DOI] [PubMed] [Google Scholar]
- 7. Coles CE, Aristei C, Bliss J, Boersma L, Brunt AM, Chatterjee Set al. International guidelines on radiation therapy for breast cancer during the COVID-19 pandemic. Clin Oncol (R Coll Radiol) 2020; 32: 279–281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Simcock R, Thomas TV, Mercy CE, Filippi AR, Katz MA, Pereira IJet al. COVID-19: Global radiation oncology's targeted response for pandemic preparedness. Clin Transl Radiat Oncol 2020; 22: 55–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Flores-Balcázar CH, Flores-Luna L, Villarreal-Garza C, Mota-García A, Bargalló-Rocha E. Impact of delayed adjuvant radiotherapy in the survival of women with breast cancer. Cureus 2018; 10: e3071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Bartelink H, Maingon P, Poortmans P, Weltens C, Fourquet A, Jager Jet al. ; European Organisation for Research and Treatment of Cancer Radiation Oncology and Breast Cancer Groups. Whole-breast irradiation with or without a boost for patients treated with breast-conserving surgery for early breast cancer: 20-year follow-up of a randomised phase 3 trial. Lancet Oncol 2015; 16: 47–56. [DOI] [PubMed] [Google Scholar]
- 11. van de Water W, Bastiaannet E, Scholten AN, Kiderlen M, de Craen AJ, Westendorp RGet al. Breast-conserving surgery with or without radiotherapy in older breast patients with early stage breast cancer: a systematic review and meta-analysis. Ann Surg Oncol 2014; 21: 786–794. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1: Supporting information


