Abstract
Aims
Admission rates for acute decompensated heart failure (HF) declined during the COVID‐19 pandemic. However, the impact of this reduction on hospital mortality is unknown. We describe temporal trends in the presentation of patients with acute HF and their in‐hospital outcomes at two referral centres in London during the COVID‐19 pandemic.
Methods and results
A total of 1372 patients hospitalized for HF in two referral centres in South London between 7 January and 14 June 2020 were included in the study and their outcomes compared with those of equivalent patients of the same time period in 2019. The primary outcome was all‐cause in‐hospital mortality. The number of HF hospitalizations was significantly reduced during the COVID‐19 pandemic, compared with 2019 (P < 0.001). Specifically, we observed a temporary reduction in hospitalizations during the COVID‐19 peak, followed by a return to 2019 levels. Patients admitted during the COVID‐19 pandemic had demographic characteristics similar to those admitted during the equivalent period in 2019. However, in‐hospital mortality was significantly higher in 2020 than in 2019 (P = 0.015). Hospitalization in 2020 was independently associated with worse in‐hospital mortality (hazard ratio 2.23, 95% confidence interval 1.34–3.72; P = 0.002).
Conclusions
During the COVID‐19 pandemic there was a reduction in HF hospitalization and a higher rate of in‐hospital mortality. Hospitalization for HF in 2020 is independently associated with more adverse outcomes. Further studies are required to investigate the predictors of these adverse outcomes to help inform potential changes to the management of HF patients while some constraints to usual care remain.
Keywords: Heart failure, COVID‐19, In‐hospital mortality, Hospitalization, Trends
Temporal trends in heart failure admission and adjusted Kaplan–Meier curves for in‐hospital mortality during the COVID‐19 pandemic.
Introduction
The COVID‐19 pandemic has been the most difficult public health emergency of our time and has dramatically affected all health care systems, requiring the reconfiguration of usual care pathways. The UK, and especially London, experienced the highest burden of COVID‐19 in Europe. 1 Multiple measures were adopted to limit the spread of the virus. In line with these measures, health care was reconfigured. This resulted in a reduction in specialty bed availability and the redeployment of specialist cardiology staff. Those staff remaining in cardiology departments looked after patients with a broader range of cardiac conditions than prior to the pandemic.
Over the last months, a persistent decline in admission for many cardiovascular conditions has been observed. 2 , 3 , 4 , 5 , 6 As with acute coronary syndromes, hospitalization for heart failure (HF) declined progressively during the COVID‐19 pandemic and patients presenting to hospital had a more advanced phenotype compared with those admitted in similar periods in previous years. 4 So far, data on HF hospitalization rates after the peak of the pandemic, which have potentially surged to normal or above normal levels, are scant.
As reported by the National Heart Failure Audit in the UK, between 5% and 10% of patients hospitalized with HF die in‐hospital and more than 30% of those discharged after an acute decompensation experience an adverse outcome within 12 months of the index hospitalization. 7 Whether the reduction in hospital admissions for HF during COVID‐19 is associated with more adverse outcomes is still unknown.
The aim of the present study is to describe temporal trends in hospitalization with HF throughout the pandemic and, importantly, the associated in‐hospital outcomes.
Methods
Study design and population
This was a prospective cohort study of unselected patients hospitalized for HF. Consecutive patients with HF, older than 18 years, presenting to two referral centres in London, King's College Hospital and Princess Royal University Hospital, from 7 January to 14 June 2020 were included in the study and their data compared with data for patients presenting during the equivalent period in 2019. To exclude possible extrinsic factors influencing HF admissions, the first week of January was excluded from the analysis, and observation was started from 7 January. The ‘COVID‐19 time’ has been defined as the period between 2 March 2020, when the first COVID‐19 death in the UK occurred, and 14 June 2020, which represents the last day of full lockdown before commerce reopened in England. Patients were included in the analysis if they had a discharge diagnosis of HF in the first or second diagnostic position according to appropriate ICD codes [I11.0 Hypertensive heart disease with (congestive) heart failure; I25.5 Ischaemic cardiomyopathy; I42.0 Dilated cardiomyopathy; I42.9 Cardiomyopathy, unspecified; I50.0 Congestive heart failure; I50.1 Left ventricular failure; I50.9 Heart failure, unspecified]. This information was extracted from our local hospital episode statistics (HES) data.
Outcome measures
The primary outcomes of the study were trends in hospitalization for HF throughout the observation period and in‐hospital mortality. Ethnicity, specialty ward allocation at admission and discharge, length of stay and readmission rates were also available for analysis. A pre‐defined subgroup analysis, to evaluate the impact of COVID‐19, considered only the timeframe from 2 March to 14 June 2020.
Statistical analysis
Variables are expressed as the mean and standard deviation, median and interquartile range (IQR), or count and percentage, as appropriate. The results are reported in line with ‘Strengthening the Reporting of Observational Studies in Epidemiology’ (STROBE) guidelines. 8 Baseline characteristics were compared using Pearson's chi‐squared test for categorical variables or the Student's t‐test for continuous variables, using the Brown–Forsythe statistic when the assumption of equal variances did not hold, or the non‐parametric Mann–Whitney U‐test when necessary. Normality of distribution was assessed using the Shapiro–Wilk test. To fit hospitalization trends in both cohorts, a cubic term and a quadratic term were used and compared by means of the extra‐sum‐of‐square F‐test. Survival curves for in‐hospital mortality were estimated and compared between years by means of the log‐rank test. To adjust for possible confounders in estimating the association between year of admission and prognosis of HF admission, multivariable Cox regression models were estimated from an unselected list of candidate prognostic variables obtained from the univariable analyses (i.e. those with a P‐value of ≤0.1). IBM SPSS Statistics Version 25.0 (IBM Corp., Armonk, NY, USA) and R (R Foundation for Statistical Computing, Vienna, Austria) were used for statistical analyses.
Sensitivity analysis
A sensitivity analysis, including only patients with HF in either the first or second diagnostic position, was conducted to ascertain potential differences in mortality according to diagnostic position. Furthermore, a sensitivity analysis excluding patients with concurrent COVID‐19 infection and HF was performed.
Results
Total study population
During the study period, a total of 1372 hospitalizations for HF were recorded. Of those, 794 occurred from 7 January to 14 June 2019 and 578 occurred during the equivalent period in 2020. Trends of HF admission differed between 2019 and 2020 (P < 0.001). Although hospitalizations for HF were consistent over the study period in 2019, hospitalizations showed a progressive decline during the COVID‐19 pandemic, followed by a gradual return to baseline until the end of the study period in June 2020 (Figure 1 ). Similar trends were observed when HF was considered in either the first or second diagnostic position (online supplementary Figure S1 ).
Figure 1.
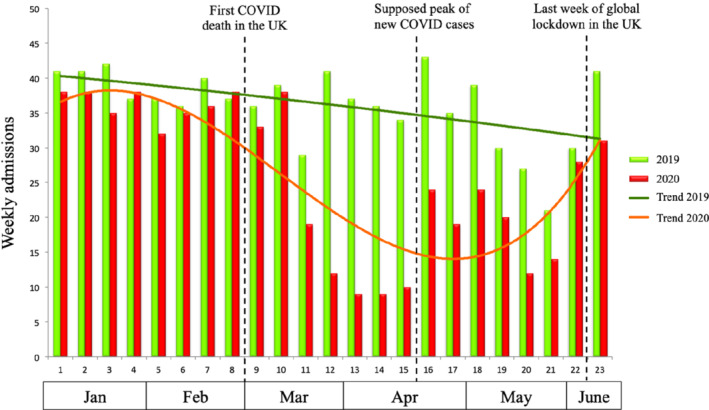
Temporal trends in decompensated heart failure hospital admissions during the COVID‐19 pandemic and in the corresponding period in 2019.
Admitted patients had similar demographic characteristics over the whole study period (Table 1 ). However, in 2020 more patients were admitted to general medicine wards compared with 2019 (83% and 77%, respectively; P = 0.008). Median length of stay was comparable between 2019 and 2020 (6 days, IQR 3–12 days and 7 days, IQR 3–14 days, respectively; P = 0.29), although patients admitted in 2020 showed a lower readmission rate (5% in 2020 vs. 8% in 2019; P = 0.03). Similarly, in the pre‐specified subgroup analysis, although the demographic characteristics of patients admitted with HF during COVID‐19 were comparable, the median length of in‐hospital stay was 1 day shorter during COVID‐19 compared with the same period in 2019 (6 days, IQR 3–11 days in 2020 vs. 7 days, IQR 2–13 days in 2019; P = 0.03) (Table 2 ).
Table 1.
Demographic characteristics of the total population from January to 14 June
| Total population: January to 14 June | ||||
|---|---|---|---|---|
| 2019 | 2020 | P‐value | ||
| Number of admissions (total n = 1372) | 794 | 578 | ||
| Age, years, mean ± SD | 77 ± 13 | 78 ± 12 | 0.14 | |
| Male sex, n (%) | 429 (54%) | 259 (45%) | 0.15 | |
| HF in first diagnostic position, n (%) | 501 (63%) | 382 (66%) | 0.28 | |
| Ethnicity, n (%) | White | 542 (68%) | 392 (68%) | 0.25 |
| Black | 157 (20%) | 102 (18%) | ||
| Other | 42 (5%) | 45 (8%) | ||
| Specialty at admission, n (%) | Cardiology | 90 (11%) | 55 (10%) | 0.008 |
| General medicine | 212 (77%) | 482 (83%) a | ||
| Other | 92 (12%) | 41 (7%) a | ||
| Specialty at discharge, n (%) | Cardiology | 219 (28%) | 126 (22%) a | 0.04 |
| General medicine | 283 (36%) | 214 (37%) | ||
| Other | 292 (37%) | 238 (41%) | ||
| Length of stay, days, median (IQR) | 7 (3–14) | 6 (3–12) | 0.29 | |
| Readmissions, n (%) | 59 (7%) | 25 (4%) | 0.03 | |
| Days to readmission, median (IQR) | 48 (18–203) | 26 (8–53) | 0.05 | |
| COVID‐19 cases, n | – | 9 | ||
HF, heart failure; IQR, interquartile range; SD, standard deviation.
P < 0.005 for multiple comparison.
Table 2.
Demographic characteristics of the population during the COVID‐19 pandemic
| Total population: March to 14 June | ||||
|---|---|---|---|---|
| 2019 | 2020 | P‐value | ||
| Number of admissions (total n = 775) | 484 | 291 | ||
| Age, years, mean ± SD | 77 ± 13 | 78 ± 13 | 0.16 | |
| Male sex, n (%) | 266 (55%) | 154 (53%) | 0.60 | |
| HF in first diagnostic position, n (%) | 307 (63%) | 199 (68%) | 0.18 | |
| Ethnicity, n (%) | White | 330 (73%) | 206 (77%) | 0.13 |
| Black | 98 (22%) | 42 (16%) | ||
| Other | 27 (6%) | 20 (8%) | ||
| Specialty at admission, n (%) | Cardiology | 55 (11%) | 24 (8%) | 0.005 |
| General medicine | 371 (77%) | 250 (86%) a | ||
| Other | 58 (12%) | 17 (6%) a | ||
| Specialty at discharge, n (%) | Cardiology | 147 (30%) | 57 (20%) a | 0.003 |
| General medicine | 164 (34%) | 107 (37%) | ||
| Other | 173 (36%) | 127 (44%) | ||
| Length of stay, days, median (IQR) | 7 (2–13) | 6 (3–11) | 0.03 | |
| Readmissions, n (%) | 36 (7%) | 11 (4%) | 0.06 | |
| Days to readmission, median (IQR) | 39 (20–119) | 13 (3–32) | 0.07 | |
| COVID‐19 cases, n | – | 9 | ||
HF, heart failure; IQR, interquartile range; SD, standard deviation.
P < 0.005 for multiple comparison.
In‐hospital mortality
Patients admitted with HF in 2020 experienced worse outcomes compared with those admitted in 2019. Indeed, in‐hospital mortality was significantly higher in 2020 compared with 2019 (P = 0.015) (Figure 2A ).
Figure 2.
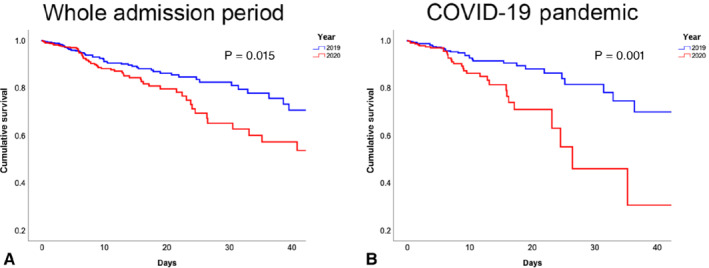
Kaplan–Meier curves for in‐hospital mortality in 2020 vs. 2019. (A) In‐hospital mortality in the total population from January to 14 June. (B) In‐hospital mortality in patients admitted during the COVID‐19 pandemic.
On multivariable analysis, after correction for demographic variables, together with older age, being admitted with HF during the COVID‐19 pandemic in 2020 was independently associated with worse outcomes [hazard ratio (HR) 2.23, 95% confidence interval (CI) 1.34–3.72; P = 0.002].
In the predefined subgroup analysis, among patients admitted from 2 March to 14 June 2020 (the COVID pandemic), cumulative survival in 2020 was significantly lower compared with 2019 (P = 0.001) (Figure 2B ). Conversely, in‐hospital outcomes were comparable in the population admitted from January to March (P = 0.55).
Sensitivity analyses confirmed that, when only patients admitted with HF in the first diagnostic position were considered, patients hospitalized in 2020 experienced more adverse outcomes than those hospitalized in 2019 (P = 0.019) (online supplementary Figure S2 ). Conversely, for patients admitted with HF in the second diagnostic position, differences in mortality were less pronounced (P = 0.49) (online supplementary Figure S3 ). Lastly, only nine patients had confirmed COVID‐19. The finding of worse mortality among HF patients admitted during the COVID‐19 pandemic was confirmed in a sensitivity analysis excluding patients with concurrent coronavirus infection (data not shown).
Discussion
Temporal trends of decompensated heart failure during COVID‐19
The impact of the COVID‐19 pandemic on health care systems has been all‐encompassing. Similarly to other cardiovascular conditions, 3 , 7 hospital admissions for decompensated HF have consistently declined during the outbreak. 2 , 4 To date, all available reports have focused on either admission for various cardiovascular conditions during the peak of the pandemic or COVID‐19‐related mortality in patients with underlying heart disease. 2 , 6 , 8 , 9 , 10 Although excess out‐of‐hospital mortality has been reported and attributed mainly to a higher incidence of pulmonary embolism, 11 an increase in HF‐related mortality has not been described to date. In the present analysis, we build on our previous findings regarding trends in HF hospitalization, 2 highlighting the resurgence of admissions following the peak of the pandemic and reporting an excess of HF‐related in‐hospital mortality.
We recently reported that, despite reduced hospitalization rates during COVID‐19, patients were more unwell compared with previous years. 2 This may be partially explained by a potential avoidance of hospital presentation unless absolutely necessary as a result of fear of infection with COVID‐19. Our present report highlights the fact that the significant drop in rates of hospitalization for HF was followed by a rebound in HF admissions after the peak of the pandemic, and a return to pre‐pandemic levels just before the release of lockdown measures (Figure 1 ). It extends our previously reported findings by incorporating a bigger cohort, recruited at two sites and with an extended capture of HF patients, using HES data and not just National HF Audit submissions (the National HF Audit requires only 70% of HES‐coded HF admissions with HF in the first diagnostic position to be submitted). There were similar trends for HF coded in the first and second diagnostic positions (online supplementary Figure S1 ). Whether this will be followed by a surge in HF hospitalization remains to be seen.
In our analysis, together with the significant reduction in HF hospitalization, we observed a difference in the place of management of HF patients. Although the demographic characteristics of patients were similar during COVID‐19 compared with 2019, a higher percentage of patients were managed in general medical wards, which is partially attributable to the reduced availability of cardiology beds and the redeployment of cardiology specialists to other areas. The changes in place of care were paralleled by a slightly shorter median length of hospitalization during COVID‐19 (6 days, IQR 3–11 days in 2020 vs. 7 days, IQR 2–13 days in 2019; P = 0.03), but it is not known if these changes are causally related. Whether the redeployment of HF specialists and redesign of pathways of outpatient care have contributed to changes in patient management remains unknown and requires future research. In other countries, virtual management of HF patients allowed continued direct access to specialist care. 12 Similarly, in our service, close telemonitoring of stable HF patients and the continuation of dedicated face‐to‐face clinic appointments for those with new incident HF and for patients with more advanced HF may have partially prevented the exacerbation of their clinical condition.
In‐hospital outcomes during COVID‐19
It has been widely reported that patients hospitalized for COVID‐19 with concomitant cardiac disease have a worse prognosis than those without a history of cardiac disease. 9 However, the in‐hospital mortality of patients admitted primarily with HF during the pandemic has not yet been reported. A recent study from Denmark 10 described a rebound in HF hospitalizations after lockdown ended, but did not observe any difference in mortality, which may relate to the relatively low impact of COVID‐19 in Denmark.
Our analysis is the first to address the relationship between COVID‐19 and in‐hospital mortality in a large population of patients with acute decompensated HF. Patients hospitalized for HF during the first 6 months of 2020 had significantly worse outcomes compared with those hospitalized during the equivalent period in 2019 (Figure 2A ). Subgroup analysis suggested that this was driven by a higher incidence of in‐hospital mortality during the COVID‐19 pandemic (Figure 2B ). Conversely, being admitted in the first 2 months of 2020 was not associated with increased in‐hospital mortality.
Multivariable analysis revealed that, together with older age, being admitted in 2020 was independently associated with more adverse outcomes both in the total population and in those admitted during the COVID‐19 pandemic (HR 2.23, 95% CI 1.34–3.72; P = 0.002). There are several potential explanations for this. Firstly, as recently reported, patients hospitalized with HF during the pandemic were sicker and had higher New York Heart Association (NYHA) functioning class status and worse congestion compared with those hospitalized in the equivalent period in 2019. 2 Indeed, the previously described more advanced HF status at admission during COVID‐19 might result in higher in‐hospital mortality in this population. Secondly, and in contrast, although direct cardiac involvement of SARS‐CoV‐2 has not been demonstrated so far, concomitant asymptomatic and undiagnosed COVID‐19 infection cannot be excluded but seems unlikely given the number of tests performed on inpatients during the COVID‐19 pandemic. To date, this is the first report to show increased in‐hospital mortality in patients admitted primarily for HF during the COVID‐19 pandemic. Larger analyses are required to investigate the epidemiology and the mortality of HF patients over this troublesome year to detect whether changes in care may have played a role in this setting.
Limitations
This study was conducted in two HF referral centres in South London. Therefore, the results may not be generalizable to other places with different incidences of COVID‐19 and require further confirmation in widespread multicentre analysis. The present analysis was conducted on all admissions. Clinical characteristics, such as NYHA class, classification of HF and the degree of congestion, were not available for this analysis for all patients. Limiting the analysis to patients with available clinical data or presenting variables with a high percentage of missing values may have introduced selection bias and thereby confounded the results. The lower readmission rate in 2020 may be partially explained by the relatively short post‐discharge observational period. Further research is advocated to identify the predictors of the increased mortality during COVID‐19.
Conclusions
The COVID‐19 pandemic has placed enormous burdens on health care systems globally. The reduction in HF hospitalizations during the pandemic is paralleled by higher in‐hospital mortality and being admitted for HF in 2020 is independently associated with more adverse outcomes. Further studies are required to investigate the predictors of this higher mortality and to confirm these results in other countries.
Supporting information
Figure S1. Temporal trends of admission for heart failure in the first (left panel) and second (right panel) diagnostic positions during the COVID‐19 pandemic and in the corresponding period in 2019.
Figure S2. Kaplan–Meier curves for in‐hospital mortality in 2020 and 2019 for patients admitted with heart failure in the first diagnostic position.
Figure S3. Kaplan–Meier curves for in‐hospital mortality in 2020 and 2019 for patients admitted with heart failure in the second diagnostic position.
Acknowledgements
The authors are grateful to the staff of King's College Hospital and the Princess Royal University Hospital who helped in the fight against COVID‐19, and to all the staff who supported data collection.
Conflict of interest: none declared.
References
- 1. European Centre for Disease Prevention and Control . COVID‐19 situation update for the EU/EEA and the UK. https://www.ecdc.europa.eu/en/cases‐2019‐ncov‐eueea (6 August 2020).
- 2. Bromage DI, Cannata A, Rind IA, Gregorio C, Piper S, Shah AM, McDonagh TA. The impact of COVID‐19 on heart failure hospitalization and management: report from a heart failure unit in London during the peak of the pandemic. Eur J Heart Fail 2020;22:978–984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Pessoa‐Amorim G, Camm CF, Gajendragadkar P, De Maria GL, Arsac C, Laroche C, Zamorano JL, Weidinger F, Achenbach S, Maggioni AP, Gale CP, Poppas A, Casadei B. Admission of patients with STEMI since the outbreak of the COVID‐19 pandemic. A survey by the European Society of Cardiology. Eur Heart J Qual Care Clin Outcomes 2020;6:210–216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. De Rosa S, Spaccarotella C, Basso C, Calabro MP, Curcio A, Filardi PP, Mancone M, Mercuro G, Muscoli S, Nodari S, Pedrinelli R, Sinagra G, Indolfi C; Società Italiana di Cardiologia and the CCU Academy Investigators Group . Reduction of hospitalizations for myocardial infarction in Italy in the COVID‐19 era. Eur Heart J 2020;41:2083–2088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. De Filippo O, D'Ascenzo F, Angelini F, Bocchino PP, Conrotto F, Saglietto A, Secco GG, Campo G, Gallone G, Verardi R, Gaido L, Iannaccone M, Galvani M, Ugo F, Barbero U, Infantino V, Olivotti L, Mennuni M, Gili S, Infusino F, Vercellino M, Zucchetti O, Casella G, Giammaria M, Boccuzzi G, Tolomeo P, Doronzo B, Senatore G, Grosso Marra W, Rognoni A, Trabattoni D, Franchin L, Borin A, Bruno F, Galluzzo A, Gambino A, Nicolino A, Truffa Giachet A, Sardella G, Fedele F, Monticone S, Montefusco A, Omede P, Pennone M, Patti G, Mancone M, De Ferrari GM. Reduced rate of hospital admissions for ACS during Covid‐19 outbreak in northern Italy. N Engl J Med 2020;383:88–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Bhatt AS, Moscone A, McElrath EE, Varshney AS, Claggett BL, Bhatt DL, Januzzi JL, Butler J, Adler DS, Solomon SD, Vaduganathan M. Declines in hospitalizations for acute cardiovascular conditions during the COVID‐19 pandemic: a multicenter tertiary care experience. J Am Coll Cardiol 2020;76:280–288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Hall ME, Vaduganathan M, Khan MS, Papadimitriou L, Long RC, Hernandez GA, Moore CK, Lennep BW, McMullan MR, Butler J. Reductions in heart failure hospitalizations during the COVID‐19 pandemic. J Card Fail 2020;26:462–463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Noah N. The STROBE initiative: STrengthening the Reporting of OBservational studies in Epidemiology (STROBE). Epidemiol Infect 2008;136:865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Inciardi RM, Adamo M, Lupi L, Cani DS, Di Pasquale M, Tomasoni D, Italia L, Zaccone G, Tedino C, Fabbricatore D, Curnis A, Faggiano P, Gorga E, Lombardi CM, Milesi G, Vizzardi E, Volpini M, Nodari S, Specchia C, Maroldi R, Bezzi M, Metra M. Characteristics and outcomes of patients hospitalized for COVID‐19 and cardiac disease in Northern Italy. Eur Heart J 2020;41:1821–1829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Andersson C, Gerds T, Fosbol E, Phelps M, Andersen J, Lamberts M, Holt A, Butt JH, Madelaire C, Gislason G, Torp‐Pedersen C, Kober L, Schou M. Incidence of new‐onset and worsening heart failure before and after the COVID‐19 epidemic lockdown in Denmark: a nationwide cohort study. Circ Heart Fail 2020;13:e007274. [DOI] [PubMed] [Google Scholar]
- 11. Benzakoun J, Hmeydia G, Delabarde T, Hamza L, Meder JF, Ludes B, Mebazaa A. Excess out‐of‐hospital deaths during the COVID‐19 outbreak: evidence of pulmonary embolism as a main determinant. Eur J Heart Fail 2020;22:1046–1047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Salzano A, D'Assante R, Stagnaro FM, Valente V, Crisci G, Giardino F, Arcopinto M, Bossone E, Marra AM, Cittadini A. Heart failure management during the COVID‐19 outbreak in Italy: a telemedicine experience from a heart failure university tertiary referral centre. Eur J Heart Fail 2020;22:1048–1050. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1. Temporal trends of admission for heart failure in the first (left panel) and second (right panel) diagnostic positions during the COVID‐19 pandemic and in the corresponding period in 2019.
Figure S2. Kaplan–Meier curves for in‐hospital mortality in 2020 and 2019 for patients admitted with heart failure in the first diagnostic position.
Figure S3. Kaplan–Meier curves for in‐hospital mortality in 2020 and 2019 for patients admitted with heart failure in the second diagnostic position.


