Abstract
Cytometry is playing a crucial role in addressing the COVID‐19 pandemic. In this commentary—written by a variety of stakeholders in the cytometry, immunology, and infectious disease communities—we review cytometry's role in the COVID‐19 response and discuss workflow issues critical to planning and executing effective research in this emerging field. We discuss sample procurement and processing, biosafety, technology options, data sharing, and the translation of research findings into clinical environments. © 2020 International Society for Advancement of Cytometry
Keywords: SARS‐CoV2, COVID‐19, pandemic, flow cytometry, immune monitoring
The world is immersed in a global health challenge on a scale not seen since the 1918 influenza pandemic. COVID‐19, caused by the novel SARS‐CoV2 virus, has led to nearly 600,000 reported deaths worldwide (as of mid to July 2020) (1) and crippled economies. In the midst of this public health emergency, many researchers and laboratories have shifted focus toward the study of SARS‐CoV2. Presently, many aspects of SARS‐CoV2 infection are not fully understood, but there are active research efforts underway studying viral transmission and immune responses, as well as international efforts to develop vaccines and therapies.
The human body is made up of 37 trillion cells, which can be grouped in cell populations based on shared phenotypic identities or functional specialization. For the past several decades, cytometrists have been busy dissecting the heterogeneity of these cellular populations (2), and in the process revealing targets of viral infection, identifying protective immune cells, and characterizing the immune responses that lead to protection or to tissue damage. These are critical needs for the world's COVID‐19 response, so understandably cytometry is now playing a crucial role in SARS‐Cov2 research. As cytometric technologies are more widely implemented in this new research setting, workflow questions surrounding technology choice, biosafety protocols, quality control, and data sharing are emerging. Moreover, as cytometry is deployed for immune monitoring in vaccine and drug trials, it must be integrated into large studies, some of which are occurring across hospitals taxed by the hefty workloads of their local epidemic, with limited time and resources for planning or preparation; these issues present important challenges as well.
In this commentary, we—as stakeholders from various cytometry‐associated disciplines—highlight the value of cytometry in the study of COVID‐19, and chart a path for how cytometry can be applied and translated successfully to address this grave public health threat (Figure 1).
Figure 1.
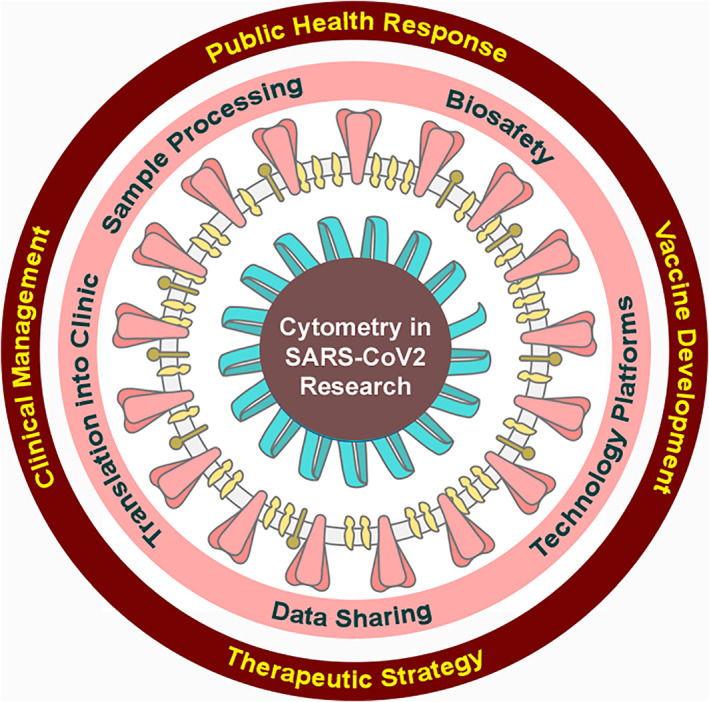
Considerations in COVID‐19 research are listed in the pink ring, and broad areas of relevance are described in the red ring. [Color figure can be viewed at wileyonlinelibrary.com]
cytometry's current and future role in combating COVID‐19
Cytometry, in all its various forms and with all its associated disciplines, has already built the foundation of basic research in COVID‐19 immunology (3). Within months of the declaration of a worldwide pandemic, our community has defined immunologic abnormalities in patients, found associations between immune characteristics and disease severity, and begun to characterize the T‐cell response to virus. The quick response of cytometrists to COVID‐19 research opportunities is not surprising; the early stages of COVID‐19 research have involved the “plug and play” of our existing toolbox into a new disease setting.
For a novel disease like COVID‐19, the identification and enumeration of different cell types are the foundation upon which further discoveries, and candidate interventions, are built. Early phenotypic analysis of immune cells in COVID patients showed that lymphopenia, and in particular a loss of T‐cells in circulation, was a hallmark of disease (4). Using high parameter flow cytometry, one study classified COVID‐19 patients into three groups, based on the immunophenotypic state of their T‐cell compartment: those patients with CD4+ T‐cell activation similar to that observed in acute infections (but only moderate CD8+ T‐cell activation), those with highly differentiated CD8+ T‐cells, and patients with little indication of immune activation or perturbation. Notably, individuals with the first immunophenotype (CD4+ T‐cell activation) tended to have more severe disease (5). Other studies have identified the loss of suppressive myeloid cells (6), characterized eosinophils as expanding in the first week (7), and revealed an increase in plasma‐blast B‐cells (8) as features of COVID‐disease that may be associated with disease severity.
Beyond broad phenotypic and functional analysis, cytometry is also used for the critical task of analyzing and evaluating immune responses to viral components. A patient's immune response to specific viral components can be assessed by measuring functional outcomes such as proliferation, cytotoxicity, activation, cytokine secretion, or antibody production upon re‐exposure to viral antigens in vitro, or through the direct analysis of cells that bind antigen. The latter is possible using specialized fluorochrome‐tagged reagents called “peptide–MHC multimers,” for the analysis of viral antigen‐specific T‐cells, and antigen trimers for similar analysis of B‐cells. These tools will play a central role in the evaluation of vaccine candidates, as they are developed. Most cytometry‐related technologies are capable of analyzing both bulk and antigen‐specific immune responses with single‐cell resolution.
In the first peer‐reviewed results from a COVID‐19 vaccine‐trial, the NIH/Moderna mRNA1273 vaccine (9) was shown to generate SARS‐CoV2‐specific CD4+ T‐cells that expressed the TH1 cytokines IFNg, IL2, and TNF, but not the TH2 cytokines IL4 and IL13. Notably, past work in mouse models of coronavirus infection showed that immune‐mediated pathology was associated with TH2‐type responses, and TH1‐ and CD8‐biased responses in the animal model were associated with better outcomes (10, 11). Early COVID‐19 research has also demonstrated an important role for IL17‐producing T‐cells in disease (12), suggesting that anti‐IL17 blocking monoclonal antibodies (already available for use in other diseases) might have therapeutic benefit in COVID‐19 patients (13). Studies have also shown that antigen‐specific T‐cell responses are common in convalescent patients (CD4+ and CD8+ responses against SARS‐Cov2 are observed in 100% and 70% of recovered patients), and suggest cross‐reactive immunity (since up to 60% of unexposed patients have detectable SARS‐CoV2‐specific CD4+ T‐cells) (14). These studies only represent a few of the myriad of studies pre‐published on bioRxiv and medRxiv to date, many of which demonstrate the clear value of single cell, high parameter flow cytometry for patient‐ and animal model‐oriented COVID‐19 research.
Flow cytometry also offers a unique ability to purify certain cell subsets—or antigen‐specific cells—for downstream analysis using fluorescence‐activated cell sorting (FACS). FACS is a critical step for the development of one class of COVID‐19 therapeutics, known as passive immunotherapy. In these early phases of the pandemic, passive immunotherapy for COVID‐19 has largely involved the infusion of convalescent patient plasma, containing SARS‐CoV2 neutralizing antibodies, into severely ill patients. Using FACS, it is possible to identify the B‐cells making SARS‐CoV2 antibodies, sort them into single‐cell wells, clone them, and then characterize the neutralization ability of antibodies produced by each SARS‐CoV2‐specific B‐cell. The B‐cells that produce neutralizing antibodies can thereby be distinguished from those making non‐neutralizing antibodies (which do not prevent infection), and sequenced. Using this approach, the sequence of B‐cell receptor (i.e., antibody) genes that make neutralizing antibodies are revealed, and these sequences can be transferred to genetically engineered cell lines for the mass production of neutralizing antibodies, which can then be administered to patients (15). Mass produced, neutralizing antibody therapeutics (developed using cytometric technology) are the next phase of passive immunotherapies, and represent a potentially important disease treatment strategy with advantages over convalescent plasma.
sample quality, procurement, and processing
Given the rapid pace of COVID‐19 research, and the growing number of laboratories providing immune monitoring for COVID‐19 studies, there is an urgent need to harmonize sample collection across sites, and share information about sample stability and marker integrity with sample storage. It is incumbent upon COVID‐19 researchers to carefully define procedures and variables in their studies and to adhere to published standards and guidelines for sample processing and analysis. These steps will ensure that the field moves forward quickly, with robust and meaningful data.
In particular, sample quality presents a major challenge in the context of a rapidly unfolding pandemic. It is well known that variables such as collection tube, sample age, and storage conditions can affect cell viability, deplete some cell subsets, alter protein/transcript expression, or the ability to respond in a functional assay (16, 17). These factors may introduce experimental artifacts that affect data reliability, so understanding the impact of sample quality is critical and must be considered when interpreting data. However, with the rapid pace of SARS‐CoV2 research, and the reality of performing research work in the context of a busy clinical setting, extensive evaluation of the impact of preanalytical variables in advance may not be feasible. In these situations, which are not ideal, information from peer reviewed publications, guidelines, and standards, can provide the basis for defining criteria for sample rejection. It is beyond the scope of this communication to make specific recommendations, as the requirements for each individual assay will be different, but immunophenotyping assays provide an example of the need for very specific guidelines. In immunophenotyping, the impact of viability may depend on specimen type, storage conditions, and stability of the cellular population assessed (18). To further complicate matters, some immunophenotyping assays are performed in a whole blood matrix that includes mild proprietary fixation chemicals, which are designed to extend specimen stability. In this format, viability measurements are not possible. In contrast, immune function tests by ICS or ELISpot assays (which are commonly used to evaluate vaccine efficacy), often use a common threshold of >66% viable cells (19, 20). In any case, clear standards for sample rejection should be employed not only for settings governed by Good Clinical Lab Practice and regulatory guidelines but should also be seriously considered for nonregulated and nonclinical settings (21, 22).
A unique challenge in COVID‐19 research arises from delays in the release of patient samples, while SARS‐CoV2 testing is performed. This situation presents a major challenge, since the sample's condition may be questionable by the time it is received by the flow cytometry laboratory. Each investigator must weigh the risk/benefit of testing precious COVID‐19 patient samples, which may be of suboptimal condition, but if tested, a sample's condition should always be recorded. If a full understanding of the impact of preanalytical variables is not known at the time of testing, investigators are advised to conduct thorough preanalytical evaluation at a later date in order to establish acceptance criteria for sample quality (23). If this is done, the previously tested samples which would not have met the acceptance criteria can be flagged and removed from the final data set.
A second challenge arises from the lymphopenia observed in COVID‐19 patients. Immunophenotyping assays must be selected and designed to account for the low number of lymphocytes present in patient peripheral blood. FACS‐based purification of rare antigen‐specific cells for downstream immunoassays, which would typically be possible from 10 million healthy donor cells, may require two to three times more sample from COVID‐19 patients. A key step in experimental design will therefore be to assess the limit of detection and sensitivity of any assay used for COVID‐19 research. Similarly, the screening of samples for antigen‐specific T‐cell populations may be uniquely challenging in COVID‐19 patients. Investigators may need to employ highly multiplexed approaches (24), such as barcoding peptide–MHC Class I multimers with unique combinations of dyes, in order to acquire more information from a single, low yield sample.
The challenges described above highlight the critical need for efficiently and clearly sharing methodological information within the COVID‐19 scientific community in “real‐time” rather than relying on standard peer‐reviewed publication timelines. In an effort to meet this need, several journals, including Cytometry Part A, have adopted a process for expedited peer review. In order to have the most impact, it is especially important that the methods sections in the fast‐tracked publications are complete and include details of specimen collection and processing. Additionally, professional societies can facilitate the exchange of methodological information, using web‐based resources like those proposed at the conclusion of this article.
biosafety
Because SARS‐CoV2 is a novel pathogen, most institutions performing COVID‐19 research have had to perform risk assessments and develop biosafety strategies unusually quickly. The ability to perform COVID‐19 research is highly dependent on this process; in fact, in the United Kingdom, ethical approval for research is not granted without evidence that biosafety protocols are in place. In the United States, local institutional biosafety committees (IBCs) typically perform risk assessments independently of Institutional Review Boards (IRBs), but still biosafety approval is a critical step in the research process.
At the time of publication, in the United States, research using SARS‐CoV2‐infected blood must be performed under Biosafety Level 2 (BSL2) conditions, with enhanced precautions, at most institutions. These so‐called “BSL2+” (or BSL2/3) precautions include personal protective equipment (gloves, face mask, splash resistant gowns, eye protection, and head/shoe coverings), a system for positively disinfecting waste, as well as capped tubes and centrifuge buckets (opened only within a biosafety cabinet). The rationale for working with blood under these conditions (which are less strict than BSL3 requirements) stems from research showing that the blood is not a significant source of infectious virus. Although viral RNA can be detected in blood, to date, no viable virus has been recovered in the small studies that have been performed, and there have been no cases of laboratory‐acquired disease amongst people working with blood from SARS‐CoV2 patients or those infected with the agent responsible for 2003's South Asian SARS epidemic. Moreover, even transfusion of blood products containing SARS‐CoV2 RNA has not resulted in infection. BSL3 precautions are required, however, when propagating virus, working with tissues (25, 26) where active replication is present (such as BAL and lung), or when there is significant risk of exposure to aerosols containing infectious particles.
Cell sorting instruments and their varied potential to generate aerosols, represent a good example of why biosafety policies have to be developed based on local risk assessments. Classical droplet‐based sorters vary widely in their potential for aerosol generation, and the protocols to measure these aerosols may or may not be implemented locally. At some institutions, droplet‐generating sorters are encased in biological safety cabinets, reducing the risk of aerosol exposure. At other institutions, aerosol‐free microfluidic sorters are available for COVID‐19 research to replace droplet sorters.
In summary, biosafety policies for COVID‐19 research should be developed at the institutional level, under the guidance of local safety experts, based on the kinds of samples, equipment, and workflows that will be used for a project. Moreover, these policies should be revisited frequently; SARS‐CoV2 is a novel agent, and our understanding of it is subject to change. Resources are available to guide this process (27, 28, 29), including those developed by the International Society for the Advancement of Cytometry's (ISAC) Biosafety Committee. ISAC's biosafety guidelines discuss broad principles (relevant for all pathogens) and also provide means for testing containment and monitoring/training staff.
cytometry technologies available to study COVID‐19
In recent years, cytometry has grown well beyond its roots in fluorescence‐based cell analysis. Technologies in the cytometry arsenal now include high‐parameter fluorescence flow cytometry, spectral flow cytometry, mass cytometry, molecular cytometry, single‐cell RNA‐sequencing, imaging flow cytometry, imaging mass cytometry, Isolight Single Cell Cytokine Secretion, CODEX, and spatial transcriptomics. In broad terms, these technologies can be grouped into those that measure mRNA transcripts versus protein (or both), or alternatively into technologies that query single‐cell suspensions versus those that examine tissues. These groupings are helpful in evaluating which technologies are best suited for a particular COVID‐19 study.
Solely in terms of the sheer volume of data provided, technologies that measure mRNA transcripts are unparalleled. In their most targeted form, these technologies—using for example BD Bioscience's Rhapsody system and Precise Assays—measure 400 predefined transcripts simultaneously from each cell in a sample. In the broadest implementation of mRNA analysis, the transcriptome can be measured (using various instrumentation and protocols), providing a broad characterization of cells. It is important to recognize the limitations of mRNA‐based platforms, however. First, gene expression is inherently noisy, occurring in bursts and with long silent phases. Moreover, post‐transcriptional regulation often governs the final expression of a protein, or its stability on the cell surface. These biological phenomena conspire to affect the correlation between mRNA and protein. Thus, a lack of mRNA expression does not necessarily mean the protein is absent; nor does the presence of an mRNA target prove expression of a protein. Second, sensitivity is heavily dependent on the depth of sequencing, which is impacted by the cost‐considerations, the expression levels of abundant and rare transcripts, and the number of cells examined. Single‐cell sequencing data are typically sparse, with many cell‐gene combinations absent. Third, these technologies are very low throughput and expensive. They are not well suited to quickly characterizing rare SARS‐CoV2‐specific T‐cells, for example, and are too expensive and labor‐intensive to deploy for large studies of COVID‐patients, (especially for studies that aim to collect samples for every patient admitted to an emergency room, e.g.). The latter consideration is critical. COVID‐19 is a disease with great heterogeneity, in terms of the severity of the disease, the age of patients, and the presence of absence of comorbidities. Powered appropriately, studies will be large and samples must be analyzed quickly, on‐demand, as they arrive. Single‐cell RNA sequencing is not well suited to such settings. Molecular cytometry, a related technology that replaces antibody fluorescent tags with oligonucleotide tags, overcomes some limitations of unimodal single cell RNA sequencing by directly measuring protein expression. However, the technique requires capture and isolation of single cells from a sample, using a single cell capture device (like the 10X Chromium or BD Rhapsody systems). These capture devices are limited to the capture of no more than 20,000 cells per capture, which is very low for immunophenotyping rare cell populations (but certainly sufficient to study immune landscapes); the analysis of more cells is certainly possible, but the need for additional materials increases cost and labor.
In contrast, single‐cell analysis of cellular proteins typically provides a good combination of throughput, cost, and data content (30). Technologies based on the measurement of cellular proteins include high‐parameter flow cytometry, spectral flow cytometry, mass cytometry, imaging flow cytometry, imaging mass cytometry, and CODEX. These technologies all use antibodies to mark cellular proteins; the antibodies carry different tags (e.g., fluorescent dyes, elemental isotopes) based on the method of detection used for each platform. In particular, high‐parameter flow, mass, and spectral cytometry can support the analysis of 1 million cells or more from each cell sample, and patient samples can be analyzed on automated platforms. The samples used for these studies are often stable for longer than those used for mRNA‐based studies, since generally proteins are less labile than mRNA transcripts, and less affected by changes in cellular environment. The primary keys to success when using these technologies are authentication/titration of antibodies (31) and standardization of instrumentation across sites (32) (which often presents a considerable challenge). A major limitation of these technologies is their relative complexity. For flow and spectral cytometry, the design of antibody panels is critical and time consuming; while for mass cytometry, instrument calibration, as well as reagent production and qualification can require considerable effort. In these regards, sharing of antibody panels across the COVID‐19 cytometry community may be very helpful (33), as would the creation of local “libraries” of antibody reagents.
Cytometry technologies may also be grouped by the matrix in which the measurements are made. Technologies that measure cells in suspension include: flow, mass, spectral, imaging flow, and molecular cytometry, along with IsoLight's single‐cell cytokine secretion platform and single cell RNA sequencing. Technologies that measure cells within tissue include imaging mass cytometry, CODEX, and spatial transcriptomics. In the most general terms, tissue‐based technologies will have little value for the study of patients with asymptomatic or mild disease, because these conditions are not accompanied by tissue pathology. Moreover, ethical approval is not likely to be granted to sample a lymph node or lung tissue in relatively healthy individuals. Blood is much more accessible and available for these patients, so studies that involve healthy or early stage individuals will likely use technologies that measure cells in suspension. Yet, it is important to remember that severe COVID‐19 disease typically manifests in lung tissue, so deploying tissue‐based technologies is likely to provide the biggest experimental value at a lower cost in understanding severe disease. Where tissue is not available, but interventional pulmonologists are accessible, an alternate approach for studying tissue‐resident immune cells is to perform bronchoalveolar lavages (BAL), which “wash” cells out of lungs for collection.
When deciding what approach is best for analyzing COVID19 samples, it is important to appreciate the inverse correlation between parameters and throughput. Fluorescence flow cytometry is still by far the most cost‐effective approach to single cell analysis, but it is limited by parameter space. As such, lower parameter flow cytometry may be seen as a technology used to confirm findings. At the other end of the scale, molecular cytometry provides the parameter space to perform very deep and comprehensive analysis of single cells. It is more likely to discover new and unappreciated heterogeneity, but it is generally not well suited to large studies, because cost considerations preclude scalability. The reality is that a combinatorial approach of very high parameter/low throughput “discovery” and focused, lower parameter/higher throughput confirmation will be the best approach. Studies will likely use mostly suspension cytometry technologies, because successful translation into a clinical setting will require more standardized approaches in which the key questions/parameters are distilled down to what is minimally required to call cell phenotype or function.
Particular cytometry technologies allow unique applications that could be of great value to COVID‐19 projects. In a previous section, we described how fluorescence flow cytometry offers live cell sorting, which plays a key role in the development of passive immunotherapy using neutralizing antibodies. Similarly, immunoassays that characterize cell functions like proliferation are uniquely performed in fluorescence flow cytometry (and likely spectral flow cytometry) settings. The beauty of these approaches is that other measurements can be multiplexed in a single step providing a deep, simultaneous characterization of cell phenotype and function. As described above, from a discovery perspective, we expect that molecular cytometry technology, with its unmatched information content, will yield great insight into SARS‐CoV2 pathogenesis. Using this technology, it is also possible to examine the clonality of T‐cells and B‐cells in COVID‐19 patient samples, by sequencing T‐cell receptor and immunoglobulin genes, respectively. This approach represents a powerful means to map the immune response to COVID‐19 antigens, a key element of vaccine studies. Finally, imaging flow cytometry technologies capture not only the average fluorescence of a marker bound to a cell but also the specific location of that signal on the cell. Currently available systems can measure up to 12 parameters per cell; however, since the output is based on digital imagery, it is possible to derive a near limitless number of parameters that often require advanced analysis approaches such as deep learning to extract meaning. In any case, this technology will likely provide information about where on the cell surface SARS‐CoV2 particles are bound.
data sharing
The efficient response of the scientific community to this pandemic will require the sharing of not only knowledge but also the data from which that knowledge is derived. This is especially important for data arising from technologies with high information content, like multidimensional cytometry. With the rapid pace of COVID‐19 research, it is unlikely that a laboratory generating a data set can completely mine their own data before publication, so opportunities to further extract knowledge are missed when data are not freely distributed in the community. A fine example of both the use and distribution of publicly available data sets is illustrated by the work of a Belgian research group (34), who provided an immune atlas of BAL specimens from patients with mild COVID‐, severe COVID‐, or non‐COVID‐related pneumonia. Data from non‐COVID‐related pneumonia were re‐analyzed from their previous study, providing important context for their COVID‐related findings. Similarly, a data set comparing healthy children and those with Kawasaki syndrome (a multisystem inflammatory disease) to the COVID‐related manifestation of this syndrome has recently been posted to medRxiv (35). This data set will be remarkably valuable because these syndromes are quite rare, and the COVID‐related manifestation was only very recently reported.
Publicly available flow cytometry data from COVID‐19 research are also being used in new and unique ways. A key challenge in flow cytometry centers around the discrimination of cells expressing a marker versus those that lack expression (“gating”). Gating can vary significantly between data analysts, and automated gating algorithms do not always capture the gates that human analysts would have set. This discordance can have downstream effects, making it harder to interpret comparisons between patient groups because some cell populations are over‐ or under‐represented in the dataset. This challenge may be solved by crowd‐sourcing gating across a wide range of analysts, as a new project is currently testing (36). This project “gamifies” publicly available flow cytometry datasets, allowing anyone—including the lay public—the opportunity to set their own gates as part of a web‐based video game.
translation of research findings into clinical environments
The objective of translational and clinical science has always been to accelerate the bench‐to‐bedside progress. This objective has never been more urgently needed as during the COVID‐19 pandemic. Much of the effort in SARS‐CoV2/COVID‐19 research is directed toward the identification of biomarkers that predict control or progression of disease, or assess novel therapeutic agents and strategies. Promising findings will need to be evaluated in clinical laboratories, for their potential to be incorporated into clinical care. In addition, there will be a strong push to develop the most interesting findings into diagnostic tests. These efforts will require laboratories to meet regulatory guidelines, which may be reviewed more quickly by regulators, but are unlikely to be substantially loosened or ignored. As such, the generation of high quality, well‐documented, quality‐controlled data from clinical laboratories and manufacturers is paramount.
For successful translation of research findings to clinical environments, the process of generating robust data must begin in research settings and is accomplished by adhering to previously established criteria when performing research assays. These guidelines include: (1) the Minimal Information About T‐cell Assays (MIATA) project (37); (2) the International Conference of Harmonization of Technical Requirements for Registration of Pharmaceuticals for Human Use (38); (3) documentation describing Good Clinical Laboratory Practice (39); (4) the Clinical Laboratory and Standards Institute (CLSI) guideline H62: Validation of Assays Performed by Flow Cytometry (40). These guidelines supplement good flow cytometry practice (29) and present a framework for reporting flow cytometry data and qualification of flow cytometry assays in a manner that provides detailed documentation and is most consistent with the regulatory requirements for final approval of an assay or reagent for clinical use. An important example lies in data generated to support FDA‐approval of vaccine trials, where data from multicolor flow cytometry assays of T‐cell phenotype and function is often used to document the immunogenicity, or immune correlates of protection, for a vaccine candidate (41). There is a great deal of historic experience to draw from in this area, as validated flow cytometry panels have been in use in HIV vaccinology and immune monitoring for some time. Data to meet regulatory requirements, and indeed the antibody panels themselves, are likely to be easily ported to the SARS‐CoV2 settings by connecting the right researchers.
The key elements for successful translational and clinical science involve standardization (42), harmonization, and method validation. As we are still in the early days of SARS‐CoV2 research, progress in standardization and harmonization is critically needed. For example, descriptions of antigen‐specific T‐cell responses to SARS‐CoV2 have differed across studies because of the varying coverage of peptide pools. An important step forward will be to standardize reagents in the field, particularly peptide pools. Similarly, to enroll the number of patients required for studies of COVID‐19 pathogenesis or vaccine immunogenicity, multiple centers will be required. To compare results across multiple trial sites in a reliable and structured manner, external quality assurance programs, like those implemented for HIV/AIDS vaccine trials will be needed (43). Facilitating multicenter translational studies, antibody reagent mixtures dried in single test tubes can be produced on demand by major companies. Apart from driving assay standardization at the reagent level, the use of dried/lyophilized antibody panels for flow cytometry will also help in simplifying the experimental workflow and relieving the burden on hospital and research staff conducting critical research while dealing with a local epidemic. In sum, efforts to harmonize work from multiple SARS‐CoV2 laboratories will greatly benefit the public health response to COVID‐19.
conclusion
Professional societies that support cytometry can play an important role in the scientific response to COVID‐19. This May, the International Society for the Advancement of Cytometry (ISAC) formed its COVID‐19 Workgroup (https://isac-net.org/page/COVID-19). The group acts as a focal point, bringing together scientists worldwide working on SARS‐CoV2, or otherwise interested in the role of cytometry technologies and methodologies in the pandemic response. The group includes significant representation from the International Clinical Cytometry Society (ICCS) as well, because the COVID‐19 work performed in research settings will need to be translated rapidly into clinical laboratory settings.
Given the magnitude and severity of the pandemic, people across diverse disciplines—in research, industry, and clinical laboratories—have shifted their focus to SARS‐CoV2. The breadth and depth of science represented will surely benefit society, but the greatest benefits can only be realized if expertise is efficiently shared amongst scientists. Already, as addressed here, there are common questions emerging about how to plan for SARS‐CoV2 research, including issues of biosafety, sample procurement, experimental design, and data analysis. The ISAC COVID‐19 Workgroup will assist in these areas, providing a centralized source for biosafety guidelines, a forum to discuss experimental design, a networking directory to establish collaborations, and a connection to data repositories and analysis algorithms. In today's climate, with the unfortunate politicization of science, it is more important than ever that laboratories generate high quality, reproducible data with traceable, calibrated measurements; ISAC's COVID‐19 Workgroup will help shape that process.
Author Contributions
Andrew Filby: Conceptualization; project administration; writing‐original draft; writing‐review and editing. Evan Jellison: Conceptualization; project administration; writing‐original draft; writing‐review and editing. Guido Ferrari: Conceptualization; writing‐original draft; writing‐review and editing. Cherie Green: Conceptualization; writing‐original draft; writing‐review and editing. Sindhu Cherian: Project administration; writing‐original draft; writing‐review and editing. Jonathan Irish: Project administration; writing‐original draft; writing‐review and editing. Virginia Litwin: Conceptualization; project administration; writing‐original draft; writing‐review and editing.
Conflicts of Interest
The authors have no conflicts of interest to report.
Acknowledgments
The authors thank the other members of ISAC's COVID‐19 Working Group for helpful discussions (Paul Wallace, Maurice O'Gorman, Tomas Kalina, and Qianjun Zhang) and Suraj Saxena. The following authors would like to acknowledge support: Guido Ferrari was supported by External Quality Assurance Program Oversight Laboratory (EQAPOL) (HHSN272201000045C and HHSN272201700061C).
Literature Cited
- 1. Dong E, Du, H , & Gardner, L. An interactive web‐based dashboard to track COVID‐19 in real time. An interactive web‐based dashboard to track COVID‐19 in real time. Lancet Infect Dis 2020;20(5):533–534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Robinson JP, Roederer M. Flow cytometry strikes gold. Science 2015;350(6262):739–740. [DOI] [PubMed] [Google Scholar]
- 3. Vabret N, Britton GJ, Gruber C, Hegde S, Kim J, Kuksin M, Levantovsky R, Malle L, Moreira A, & Park MD et al. Immunology of COVID‐19: Current state of the science. Immunity 2020;52:910–941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L, Fan G, Xu J, Gu X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020;395(10223):497–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Mathew D, Giles JR, Baxter AE, Oldridge DA, Greenplate AR, Wu JE, Alanio C, Kuri‐Cervantes L, Pampena MB, D'Andrea K et al. Deep immune profiling of COVID‐19 patients reveals distinct immunotypes with therapeutic implications. Science 2020. 10.1126/science.abc8511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Schulte‐Schrepping J, Reusch N, Paclik D, Baßler K, Schlickeiser S, Zhang B, Krämer B, Krammer T, Brumhard S, Bonaguro L et al. Suppressive myeloid cells are a hallmark of severe COVID‐19. medRxiv 2020. [Google Scholar]
- 7.Rodriguez L, Pekkarinen P, Tadepally LK, Tan Z, Consiglio CR, Pou C, Chen Y, Mugabo CH, Quoc AN, Nowlan K et al. Systems‐level immunomonitoring from acute to recovery phase of severe COVID‐19. medRxiv 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Cervantes L, Pampena MB, Meng W, Rosenfeld AM, Ittner CAG, Weisman AR, Agyekum RS, Mathew D, Baxter AE, Vella LA et al. Comprehensive mapping of immune perturbations associated with severe COVID‐19. Sci Immunol 2020;5(49):eabd7114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Jackson L, Anderson EJ, Rouphael NG, Roberts PC, Makhene M, Coler RN, McCullough MP, Chappell JD, Denison MR, Stevens LJ, et al. An mRNA vaccine against SARS‐CoV2 ‐ preliminary report. N Engl J Med 2020. 10.1056/NEJMoa2022483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Graham BS. Rapid COVID‐19 vaccine development. Science 2020;368(6494):945–946. [DOI] [PubMed] [Google Scholar]
- 11. Corbett KS, Edwards DK, Leist SR, Abiona OM, Boyoglu‐Barnum S, Gillespie RA, Himansu S, Schäfer A, Ziwawa, CT , & DiPiazza, AT . SARS‐CoV‐2 mRNA vaccine design enabled by prototype pathogen preparedness. Nature 2020. 10.1038/s41586-020-2622-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Biasi D et al. Marked T‐cell activation, senescnece, exhaustion and skewing towards TH17 in patients with COVID‐19 pneumonia. Nat Commun 2020;11:3434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Pacha O, Sallman MA, Evans SE. COVID‐19: A case for inhibiting IL‐17? Nat Rev Immunol 2020;20:345–346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Mateus J, Grifoni A, Tarke A, Sidney J, Ramirez SI, Dan JM, Burger ZC, Rawlings SA, Smith DM, Phillips E et al. Selective and cross‐reactive SARS‐CoV‐2 T‐cell epitopes in unexposed humans. Science 2020;eabd3871. 10.1126/science.abd3871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Zost SJ, Gilchuk P, Chen RE, Case JB, Reidy JX, Trivette A, Nargi RS, Sutton RE, Suryadevara N, Chen EC et al. Rapid isolation and profiling of a diverse panel of human monoclonal antibodies targeting the SARS‐CoV2 spike protein. Nat Med 2020. 10.1038/s41591-020-0998-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Davis BH et al. Validation of cell‐based fluorescence assays: Practice guidelines from the ICSH and ICCS–part II–preanalytical issues. Cytom Part B 2013;84(5):286–290. [DOI] [PubMed] [Google Scholar]
- 17. Weinberg A et al. Optimization of storage and shipment of cryopreserved peripheral blood mononuclear cells from HIV‐infected and uninfected individuals for ELISPOT assays. J Immunol Methods 2010;363(1):42–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Diks AM et al. Impact of blood storage and sample handling on quality of high dimensional flow cytometric data in multicenter clinical research. J Immunol Methods 2019;475:112616. [DOI] [PubMed] [Google Scholar]
- 19. Russell ND et al. Moving to HIV type 1 vaccine efficacy trials: Defining T‐cell responses as potential correlates of immunity. J Infect Diseas 2003;187(2):226–242. [DOI] [PubMed] [Google Scholar]
- 20. Sanchez AM et al. The external quality assurance oversight laboratory (EQAPOL) proficiency program for IFN‐gamme enzyme‐linked ImmunoSpot (IFN‐g ELISpot) assay. J Immunol Methods 2014;409:31–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. CLSI . Clinical Flow Cytometric Analysis of Neoplastic Hematolymphoid Cells. 2nd ed. Wayne, PA: Clinical Laboratory Standards Institute, 2007. [Google Scholar]
- 22. CLSI . Enumeration of Immunologically Defined Cell Populations by Flow Cytometry. 2nd ed. Wayne, PA: Clinical Laboratory Standards Institute, 2007. [Google Scholar]
- 23. Brown L et al. Recommendations for the evaluation of specimen stability for flow cytometric testing during drug development. J Immunol Methods 2015;418:1–8. [DOI] [PubMed] [Google Scholar]
- 24. Gangaev A, Ketelaars SLC, Patiwael S, Dopler A, Isaeva OI, Hoefakker K, De Biasi S, Mussini C, Guaraldi G, Girardis M et al. Profound CD8 T‐cell responses toward the SARS‐CoV2 ORF1ab in COVID‐19 patients. Res Square 2020. 10.21203/rs.3.rs-33197/v1 [DOI] [Google Scholar]
- 25. Sekulic M et al. Molecular detection of SARS‐CoV2 infection in FFPE samples and histopathologic findings in fatal SARS‐COV2 cases. Am J Clin Pathol 2020;154(2):190–200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Bradley BT, Maioli H, Johnston R, Chaudhry I, Fink SL, Xu H, Najafian B, Deutsch G, Lacy JM, Williams T et al. Histopathology and ultrastructural findings of fatal COVID‐19 infections in Washington state: A case series. Lancet 2020. 10.1016/S1040-6736(20)31305-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Holmes KL et al. International Society for the advancement of cytometry cell sorter biosafety standards. Cytometry A 2014;85(5):434–453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Cossarizza A et al. Handling and processing of blood specimens from patients with COVID‐19 for safe studies on cell phenotype and cytokine storm. Cytometry A 2020;97:668–673. 10.1002/cyto.a.24009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Cossarizza A et al. Guidelines for the use of flow cytometry and cell sorting in immunological studies. Eur J Immunol 2019;49(10):1457–1973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Chattopadhyay PK, Roederer M, & Bolton DL. A deadly dance: The choreography of host‐pathogen interactions, as revealed by single‐cell technologies. Nat Commun 2018;9(1):4638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Kalina T, Lundsten, K , & Engel P. Relevance of antibody validation for flow cytometry. Cytometry A 2019;97:126–136. [DOI] [PubMed] [Google Scholar]
- 32.Novakova M, Glier H, Brdičková N, Vlková M, Santos AH, Lima M, Roussel M, Flores‐Montero J, Szczepanski T, Böttcher S, et al. How to make usage of the standardized EuroFlow 8‐color protocols possible for instruments of different manufacturers. J Immunol Methods 2019;475:112388. 10.1016/j.jim.2017.11.007. [DOI] [PubMed] [Google Scholar]
- 33. Mahnke Y, Chattopadhyay P, & Roederer M. Publication of optimized multicolor immunofluorescence panels. Cytometry A 2010;77A:814–818. [DOI] [PubMed] [Google Scholar]
- 34. Wauters E, Van Mol P, Garg AD, Jansen S, Van Herck Y, Vanderbeke L, Bassez A, Boeckx B, Malengier‐Devlies B, Timmerman A et al. Discriminating mild from critical COVID‐19 by innate and adaptive immune single‐cell profiling of bronchoalveolar lavages. bioRxiv 2020. 10.1101/2020.07.09.196519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Consiglio R, Cotugno N, Sardh F, Pou C, Amodio D, Zicari S, Ruggiero A, Pascucci GR, Rodriguez L, Santilli V et al. The immunology of multisystem inflammatory syndrome in children with COVID‐19. medRxiv 2020. 10.1101/2020.07.08.20148353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. https://www.ccpgames.com/news/2020/fight-covid-19-by-playing-eve-online-in-new-phase-of-citizen-science
- 37. Janetzki S, Britten CM, Kalos M, Levitsky HI, Maecker HT, Melief, CJ, Old LJ, Romero P, Hoos A, & Davis MM. MIATA – Minimal information about T‐cell assays. Immunity 2009;31(4):527–528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Singh J. International conference on harmonization of technical requirements for registration of pharmaceuticals for human use. J Pharmacol Pharmacother 2015;6(3):185–187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Ezzelle J, Rodriguez‐Chavez IR, Darden JM, Stirewalt M, Kunwar N, Hitchcock R, Walter T, & D'Souza MP. Guidelines on good clinical laboratory practice. J Pharm Biomed Anal 2008;46(1):18–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. CLSI . Validation of Assays Performed by Flow Cytometry. 1st ed. Wayne, PA: Clinical Laboratory Standards Institute, 2020. [Google Scholar]
- 41. Gray G, Huang Y, Grunenberg N, Laher F, Roux S, Andersen‐Nissen E, De Rosa SC, Flach B, Randhawa AK, Jensen R et al. Immune correlates of the Thai RV144 HIV vaccine regimen in South Africa. Sci Trans Med 2019;11:510–517. 10.1126/scitranslmed.aax1880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Kalina T. Reproducibility of flow cytometry through standardization: Opportunities and challenges. Cytometry A 2019;97A:137–147. [DOI] [PubMed] [Google Scholar]
- 43. Staats J, Enzor JH, Sanchez AM, Rountree W, Chan C, Jaimes M, Chan RC, Gaur A, Denny TN, & Weinhold KJ. Toward development of a comprehensive external quality assurance program for polyfunctional intracellular cytokine staining assays. J Immunol Methods 2014;409:44–53. [DOI] [PMC free article] [PubMed] [Google Scholar]


