Key Messages.
Self‐requested, screening, and diagnostic mammography examinations decreased 96%, 51%, and 6%, respectively, from pre‐COVID‐19 to COVID‐19.
Above a threshold (>20 new COVID‐19 cases/week), the difference of weekly mammography (pre‐COVID‐19 minus COVID‐19) showed a high positive correlation with weekly new COVID‐19 cases.
COVID‐19 (coronavirus disease 2019) has spread rapidly in China and other parts of the world since December 31, 2019. 1 The first reported COVID‐19 case in Taiwan was confirmed on January 21, 2020. Previously, Taiwan experienced hospital‐acquired severe acute respiratory syndrome (SARS) infections in 2003, so people hesitated to come to hospitals and risked SARS transmission then. 2 Similar to the SARS outbreak, many people in Taiwan have been afraid to visit hospitals during the COVID‐19 pandemic.
Taiwan implemented a mammography‐based nationwide screening for breast cancer in July 2004 that provides free biennial mammography to women between the ages of 45 and 69 years. 3 Self‐paid/self‐requested health checkups are also relatively prevalent in Taiwan. There was no official recommendation about mammography examinations in Taiwan during the pandemic. Mammography examinations for different purposes have continued during this pandemic in all Taiwan's hospitals. Since there is little evidence for an optimum mammography policy for either symptomatic or screening women during the COVID‐19 pandemic, we investigated the impact of the COVID‐19 pandemic on mammography utilization in southern Taiwan.
The hospital institutional review board approved this retrospective study. This study retrieved records for patients receiving mammography services in a 1455‐bed public, academic medical center that provides screening and diagnostic mammography in southern Taiwan. The test period (22 weeks) of the COVID‐19 pandemic was between the 1st and 22nd week in 2020. The pre‐COVID‐19 pandemic control period was between the 1st and 22nd week of 2019, when there was no evidence about the virus. COVID‐19 data were retrieved from Taiwan's National Health Command Center. We further categorized mammography data as self‐requested, national screening, and diagnostic based on procedure code. Self‐requested mammography refers to women schedule herself for a self‐paid mammography without an order from her physician. Screening mammography for women aged 45–69 years is further divided into five age groups. A recall rate refers to the percentage of screening mammography that is interpreted as suspicious.
As of May 31, 2020, Taiwan had 442 confirmed cases and seven deaths from COVID‐19 (Figure 1). About 37% fewer total mammography examinations were found in the COVID‐19 pandemic than 1 year earlier (3041 vs 4816, P < .001). Among 22 weeks, only 2 weeks had less total mammogram examination than previous years due to two long weekend holidays in 2019. The difference of 22 weekly mammography examinations (pre‐COVID‐19 minus COVID‐19) showed a low positive correlation with weekly new COVID‐19 cases (r = .30, P = .17) (Figure 2). Above a selected threshold number (>20 new COVID‐19 cases/week), the difference of weekly mammography showed a high positive correlation with weekly COVID‐19 cases (r = .96, P = .007). There was no significant difference in age (mean ± SD) of total mammography cases between COVID‐19 and pre‐COVID‐19 (51.19 ± 4.35 years and 55.11 ± 1.65 years, P = .21). The examinations for self‐requested, screening, and diagnostic mammography decreased 96%, 51%, and 6%, respectively, from pre‐COVID‐19 to COVID‐19. The proportion of mammography subgroups is significantly different between pre‐COVID‐19 and COVID‐19 (P < .001). The weekly volumes of mammography were significantly different in screening (P < .001) and self‐requested mammography (P < .001) between 2019 and 2020. However, the weekly volume of diagnostic mammography is not significantly different (P = .14). The age of women receiving screening mammography (mean ± SD) was 55.74 ± 7.52 and 55.45 ± 7.27 among the COVID‐19 and pre‐COVID‐19, respectively (P = .72). There were no age differences between 2019 and 2020 in three mammography subgroups (all >0.05). The women in the screening mammography group showed no significant difference between pre‐COVID‐19 and COVID‐19 by the proportion of each age group (P = .32). Age subgroups of screening mammography are listed in Table 1. The recall rate of screening mammography was 5.8% and 5.6% for pre‐COVID‐19 and COVID‐19, respectively (P = .91).
FIGURE 1.
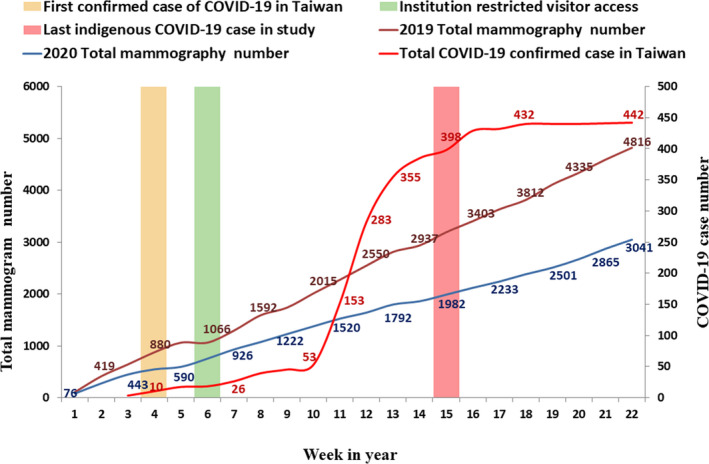
Weekly trend in the number of total mammography examinations in the periods of 2019 (pre‐COVID‐19) and 2020 (COVID‐19). A reference line shows a total number of confirmed COVID‐19 cases (including imported cases and indigenous cases) in Taiwan by weeks
FIGURE 2.
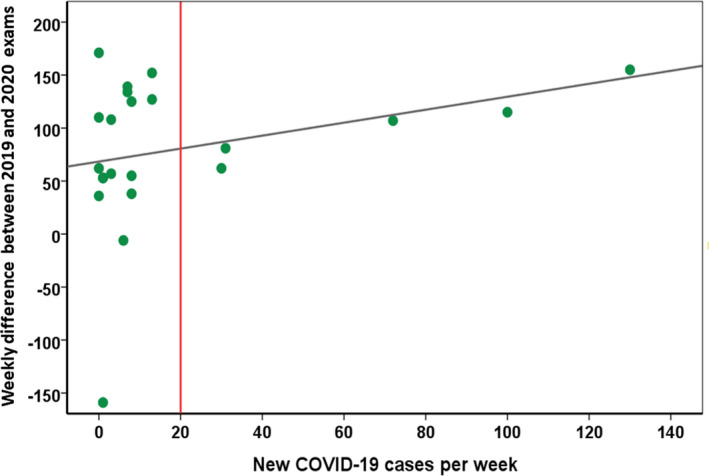
Correlation of new weekly COVID‐19 cases and weekly difference of total mammography examinations. The difference of weekly mammography examinations (2019 minus 2020) shows a low positive correlation with new weekly COVID‐19 cases (r = .30, P = .17). Above a selected threshold (>20 new COVID‐19 per week), the difference of weekly mammography shows a high positive correlation with weekly new COVID‐19 cases
TABLE 1.
Age subgroups of women receiving screening mammography during pre‐COVID‐19 and COVID‐19
| Age subgroup | Pre‐COVID‐19 (N = 3254) | COVID‐19 (N = 1774) |
|---|---|---|
| 45‐49 | 997 (30.1) | 563 (31.7) |
| 50‐54 | 656 (20.1) | 366 (20.6) |
| 55‐59 | 592 (18.2) | 343 (19.3) |
| 60‐64 | 557 (17.1) | 284 (16.0) |
| 65‐69 | 452 (13.9) | 218 (12.3) |
Numbers in parentheses are percentages.
The weekly new COVID‐19 cases could be a negative predictor of mammography examinations and public health compliance due to psychological responses, such as anxiety and fear in the COVID‐19 pandemic. Self‐requested mammography showed the greatest impact from the pandemic. The health management center had to shut down and reallocate the manpower to other services temporarily. The biennial screening mammography reduced by 51%. We found the decrease of screening mammography occurred in all age groups. The positive cases (recall rate) for screening mammography during the COVID‐19 period remained similar to the pre‐COVID‐19 period. Diagnostic mammography showed less impact from the pandemic. We found that women were weighing the benefits of mammography examinations against the risks of virus exposure.
The risk of delayed breast cancer diagnosis with worse outcomes should be very carefully weighed against the risk of virus exposure for patients and physicians. The American Society of Breast Surgeons and European breast specialists recommend that all medical facilities should postpone all breast screening. 4 , 5 However, diagnostic mammography in symptomatic women should be continued to avoid delayed diagnosis and worse cancer outcomes. 5 As Taiwan's hospital resources and medical staff were not limited during this pandemic, triage of breast cancer patients is not critical.
In summary, COVID‐19 has influenced the volume of mammography examinations, especially in self‐requested and screening mammography, more prominent above a threshold number of weekly new COVID‐19 cases.
CONFLICT OF INTEREST
Meng‐Yuan Tsai and other co‐authors have no conflict of interest.
AUTHORS' CONTRIBUTION
Dr Chou, Pan, Yang, Chiang, Huang, and Tsai all contributed to the research and writing of this manuscript.
ETHICAL APPROVAL
The study was approved by the institutional review board (IRB) of Kaohsiung Veterans General Hospital(KSVGH20‐CT7‐26). Written informed consent was waived.
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on reasonable request from the corresponding author. Some data are not publicly available due to their containing information that could compromise the privacy of research participants.
REFERENCE
- 1. Hy C, Sw J, Dp L, Tc N, Wt H, Hh L. Contact tracing assessment of COVID‐19 transmission dynamics in taiwan and risk at different exposure periods before and after symptom onset. JAMA Intern Med. 2020. Published online May 01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Chang HJ, Huang N, Lee CH, Hsu YJ, Hsieh CJ, Chou YJ. The impact of the SARS epidemic on the utilization of medical services: SARS and the fear of SARS. Am J Public Health. 2004;94(4):562‐564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Chou CP, Pan HB, Hsu GC, et al. Assessing the first 3 years of Taiwan's nationwide population‐based mammography screening program. Breast J. 2012;18(5):498‐499. [DOI] [PubMed] [Google Scholar]
- 4. Dietz JR, Moran MS, Isakoff SJ, et al. Recommendations for prioritization, treatment, and triage of breast cancer patients during the COVID‐19 pandemic. The COVID‐19 pandemic breast cancer consortium. Breast Cancer Res Treat. 2020;181(3):487‐497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Curigliano G, Cardoso MJ, Poortmans P, et al. Recommendations for triage, prioritization and treatment of breast cancer patients during the COVID‐19 pandemic. Breast. 2020;52:8‐16. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available on reasonable request from the corresponding author. Some data are not publicly available due to their containing information that could compromise the privacy of research participants.


