Abstract
The province of L'Aquila (Central Italy) was marginally affected by COVID‐19 pandemic, but changes in health care seeking behaviors were noticed. The authors retrospectively analyzed de‐identified data concerning all‐cause and cardiovascular hospitalizations, cardiovascular acute phase treatments, and in‐hospital cardiovascular deaths in the province of L'Aquila from January 1 to March 31, in 2020 and 2019. Incidence rate ratios (IRR) comparing 2020 and 2019 for admissions/procedures were calculated through Poisson regression. All‐cause and cardiovascular mortality in the examined time windows was also assessed. Less all‐cause (IRR 0.85, P < .001) and cardiovascular (IRR 0.73, P < .001) hospitalizations occurred in 2020 than in 2019. Less daily cardiovascular procedures were also performed (IRR: 0.74, P = .009). A disproportionate decrease in the number of procedures was observed in relation to cardiovascular hospitalizations in 2020 (−5.5%, P = .001). Unlike all‐cause mortality, more in‐hospital cardiovascular deaths occurred in March 2020 compared with March 2019 (+6.8%, P = .048).
Keywords: cardiovascular death, cardiovascular diseases, cardiovascular hospitalization, cardiovascular procedures, COVID‐19, SARS‐CoV‐2
1. INTRODUCTION
The spread of COVID‐19 pandemic was not homogeneous in Italy, with Northern regions bearing the greatest burden of the disease. In the Abruzzo region, in Central Italy, the province of L'Aquila is the closest to Rome, where the first two imported SARS‐CoV‐2‐positive cases have been detected as of January 29, 2020. With a population of 303 239 individuals and a total of 123 COVID‐19 cases (40.6/100 000) as of March 31, 2020, the area was among the less affected in Italy (Figure S1, panel A).
Specifically, no cases were recorded in the province of L'Aquila before March 3, 2020. A total of 6 patients tested positive for SARS‐CoV‐2 in the same area as of March 11, 2020 (15.8% of total regional cases [n.38]). As of March 31, 2020, 8.8% (N = 123) of total cumulative cases in the region (N = 1401) was from the province of L'Aquila.
Preliminary evidence indicates a reduction in hospital admissions for acute coronary syndromes following the COVID‐19 outbreak in Northern Italy. 1 In parallel, a decrease in coronary revascularization procedures in association with the pandemic has been described in Southern Italy. 2 Herein, the authors aimed at assessing whether the even marginal COVID‐19 burden in the area of L'Aquila had an impact on cardiovascular hospitalizations and outcomes.
The authors retrospectively analyzed de‐identified data from all patients admitted to the five hospitals located in the province of L'Aquila, Italy (L'Aquila, Avezzano, Sulmona, Castel di Sangro, Tagliacozzo) (Figure S1, panel B). Data collection occurred through automated extraction from the Local Health Authority registry. Our analysis included inpatient electronic health records relative to the time window from January 1 to March 31, in the years 2020 (study period) and 2019 (control period). The authors excluded patients who had been admitted to the hospital during the time window of interest, but had not been discharged or whose discharge status had not yet been recorded by March 31. Information of interest included patients' demographic characteristics (age, sex), major cardiovascular interventional procedures (coronary angioplasty, systemic fibrinolysis, endovascular procedures for stroke), diagnosis at discharge based on the International Classification of Diseases, 10th Revision, Clinical Modification, and clinical outcome (cardiovascular death). Data accuracy was checked for by study investigators. A priori established landmark dates were January 7, 2020, when the novel coronavirus was identified; January 29, 2020, when the first two foreign SARS‐CoV‐2‐positive patients were hospitalized in Italy; February 21, 2020, when the first Italian SARS‐CoV‐2‐positive case was diagnosed; and March 11, 2020, when the Italian government imposed national lockdown measures. The primary outcome was the daily hospitalization rate for any diagnosis in the time window of interest in the years 2019 and 2020; co‐secondary outcomes were the hospitalization rates for major cardiovascular diseases (coronary heart disease, cerebrovascular disease, pulmonary embolism), the rates of related acute phase treatments (coronary angioplasty for coronary artery disease; intravenous thrombolysis and endovascular treatment for ischemic stroke), and intra‐hospital all‐cause mortality and deaths attributable to major cardiovascular diseases in the same periods. The authors focused on March as the period of early diffusion of SARS‐CoV‐2 in Italy, including the province of L'Aquila, thus resulting in it being particularly appropriate to investigate changes in health care seeking behaviors. Hospitalization rates were obtained by dividing the number of cumulative admissions by the number of days in the time window of interest. Unadjusted incidence rate ratios (IRR) comparing the first quarter of 2020 with the same period in 2019 for the number of admissions/procedures on a daily or weekly basis were calculated using the Poisson regression. Case fatality rate (%) for the major cardiovascular diseases of interest was calculated by dividing the number of related deaths by that of the relative diagnoses in the time window of interest. In‐hospital all‐cause mortality was defined as death from any cause among hospitalized individuals in the same periods. All analyses were performed using R software (version 3.6.0). 3 The study was conducted in accordance with the Declaration of Helsinki and it was approved by the local Review Board.
A total of 5908 patients were hospitalized in the first quarter of 2020 (52.9% women, mean age 59.2 ± 24.9 years), with a mean daily admission rate of 64.9. In the same period in 2019, a total of 6852 patients were hospitalized (51.8% women, mean age 60.1 ± 24.6 years; 76.1 mean daily admissions; IRR 0.85, 95% CI 0.82‐0.88, P < .001). Before February 21, the curves of overall daily hospitalizations relative to the years 2019 and 2020 overlapped (Figure 1, panel A). After that landmark date, a clear divergence in the curves was observed. Significantly, less weekly overall hospital admissions occurred after March 5, 2020 compared with 2019 (Figure S2 panel A).
Figure 1.
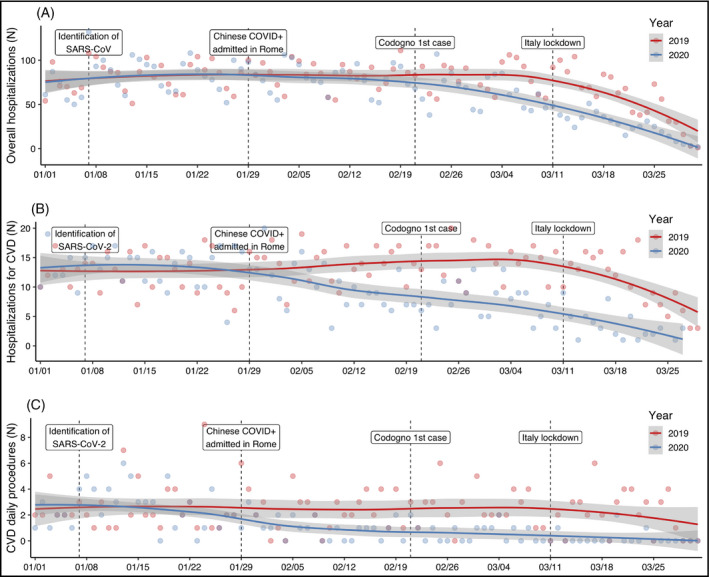
Distribution of daily hospital admissions for any diagnosis (panel A), major cardiovascular diseases (panel B), and related treatments (panel C) in the years 2019 (red) and 2020 (blue). Major cardiovascular diseases include coronary artery diseases, ischemic stroke, and pulmonary embolism; related treatments include coronary angioplasty, systemic thrombolysis, and endovascular procedures. Loess regression lines and relative ribbon standard errors are reported for 2019 (red) and 2020 (blue). The landmark dates specified in the text are also shown
Daily hospitalizations for major cardiovascular diseases in the time window of interest were significantly less in 2020 compared with 2019 (N = 809 in 2020, 42.9% women, mean age 74.6 ± 14.1 years; N = 1132 in 2019, 42.3% women, mean age 75.0 ± 13.8 years; IRR 0.73, 95% CI 0.67‐0.80, P < .001; Figure 1, panel B). Interestingly, divergence in the hospitalizations for major cardiovascular diseases was observed as early as of January 29. Further reduction in hospital admissions for major cardiovascular diseases was clearly visible after each subsequent landmark date in 2020, while the hospitalizations in 2019 remained relatively stable until early March. On a weekly basis, significantly less hospital admissions for major cardiovascular diseases occurred after February 12, 2020 compared with 2019 (Figure S2, panel B). Consistent with hospitalization data, the mean daily number of major cardiovascular procedures was significantly lower in the first quarter of 2020 compared with the same period in 2019 (Figure 1, panel C; total procedures: 219 in 2019, 112 in 2020; IRR: 0.74, 95% CI 0.59‐0.93, P = .009). Importantly, the rate of cardiovascular procedures in relation to cardiovascular hospitalizations indicated a disproportionate decrease in the number of procedures in the study period than in the control period (13.8% vs 19.3%, P = .0015). Also, significantly more intra‐hospital deaths attributable to major cardiovascular diseases occurred in March 2020 compared with the same month in 2019 (11.9% vs 6.1%, P = .048; Figure 2).
Figure 2.
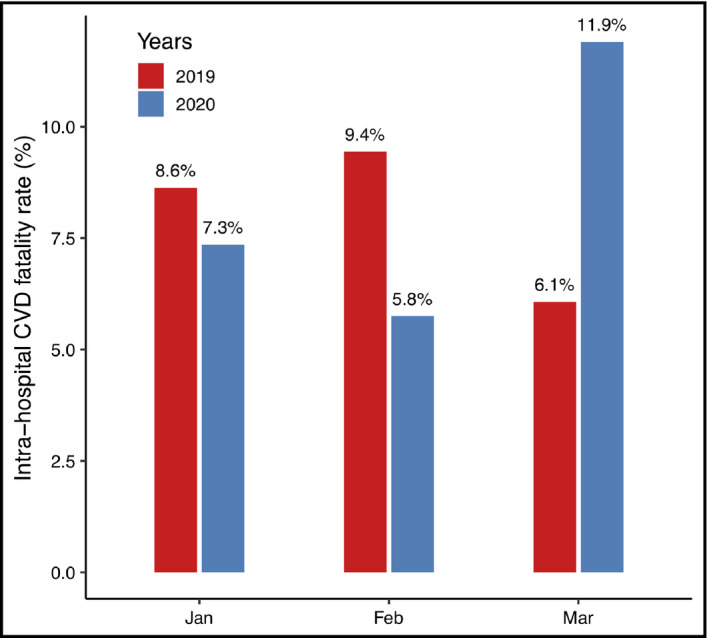
Monthly intra‐hospital case fatality rate (%) for major cardiovascular diseases in the time window of interest in 2019 (red) and 2020 (blue). Note the reverse trend in March compared with the two previous months
In terms of in‐hospital all‐cause mortality, less deaths occurred in 2020 (N = 279, 4.72%) compared with 2019 (N = 359, 5.24%) (IRR: 0.77, 95% CI 0.74‐0.80, P = .001; Figure S3).
Our findings indicate that changes in the hospitalization trends for major cardiovascular diseases and related procedures in a COVID‐19 low prevalence Italian area occurred as early as mid‐February, that is well before the establishment of national lockdown policies, while reduction in the overall hospitalizations was only evident in close temporal relationship with the initiation of lockdown. Further, an increased burden of cardiovascular‐related deaths was observed in March 2020, when the pandemic began to spread at the national level with relative sparing of the province of L'Aquila. The inflammatory burst that parallels a severe infection has been described as a possible explanation for adverse cardiovascular outcomes during the acute phase of an infectious disease. 4 , 5 The immune system activation against microbial antigens has also been described in association with increased risk of hypertension, which is a major cardiovascular risk factor and a common comorbidity in COVID‐19 patients. 6 , 7 According to the Italian National Institute of Statistics, however, COVID‐19 was only responsible for one death in the province of L'Aquila as of March 31, 2020. 8 Thus, the increased burden of cardiovascular deaths in the area could not be attributed to SARS‐CoV‐2 infection. Indeed, delayed hospital presentation could justify the adverse cardiovascular prognosis that the authors observed.
Interestingly, in‐hospital all‐cause mortality relative to the year 2020 did not exceed that of 2019; indeed, the lower number of global deaths in 2020 compared with 2019 was in line with data from the previous 5 years, 8 which might reflect the efficacy of primary and secondary prevention strategies (ie, healthy and active lifestyle, control of major personal and environmental risk factors). 9 , 10
Although the authors cannot infer the causal determinants of the observed findings, it is possible that changes in hospitalization patterns might explain the subsequent increase in cardiovascular deaths. Besides unmeasured factors and host‐specific features, 9 , 11 including forced lifestyle changes and related effects, it is possible that late hospital presentations and consequent greater disease severity affected eligibility and outcome of cardiovascular procedures, thus justifying the disproportion in cardiovascular deaths during the national lockdown period.
CONFLICT OF INTEREST
None.
AUTHOR CONTRIBUTIONS
CF conceived the article; LM extracted the data; LM and RDP checked for data accuracy; RDP performed data mining; RDP and CF interpreted the results; RDP drafted the manuscript; RDP, CF, LM, SA, SD'A, SC, DG, SS, and GD edited the manuscript; all Authors approved the final version of the manuscript.
Supporting information
Figure S1
Figure S2
Figure S3
Del Pinto R, Ferri C, Mammarella L, et al. Increased cardiovascular death rates in a COVID‐19 low prevalence area. J Clin Hypertens. 2020;22:1932–1935. 10.1111/jch.14013
Rita Del Pinto and Claudio Ferri contributed equally
REFERENCES
- 1. De Filippo O, D'Ascenzo F, Angelini F, et al. Reduced rate of hospital admissions for ACS during Covid‐19 outbreak in Northern Italy. N Engl J Med. 2020;383(1):88‐89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Piccolo R, Bruzzese D, Mauro C, et al. Population trends in rates of percutaneous coronary revascularization for acute coronary syndromes associated with the COVID‐19 outbreak. Circulation. 2020;141(24):2035‐2037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Rizzo ML. Statistical Computing with R, 2nd edn. Boca Raton, FL: CRC Press; 2019. [Google Scholar]
- 4. Corrales‐Medina VF, Madjid M, Musher DM. Role of acute infection in triggering acute coronary syndromes. Lancet Infect Dis. 2010;10(2):83‐92. [DOI] [PubMed] [Google Scholar]
- 5. Del Pinto R, Pietropaoli D, Monaco A, Desideri G, Ferri C, Grassi D. Non‐pharmacological strategies against systemic inflammation: molecular basis and clinical evidence. Curr Pharm Des. 2020;26(22):2620‐2629. [DOI] [PubMed] [Google Scholar]
- 6. Pietropaoli D, Del Pinto R, Ferri C, Ortu E, Monaco A. Definition of hypertension‐associated oral pathogens in NHANES. J Periodontol. 2019;90(8):866‐876. [DOI] [PubMed] [Google Scholar]
- 7. Pietropaoli D, Monaco A, D'Aiuto F, et al. Active gingival inflammation is linked to hypertension. J Hypertens. 2020. Epub ahead of print. 10.1097/HJH.0000000000002514 [DOI] [PubMed] [Google Scholar]
- 8. Istat . It english. www.istat.it/en/. Accessed July 22, 2020.
- 9. Del Pinto R, Pagliacci S, De Feo M, Grassi D, Ferri C, Italian Society of Hypertension and Federfarma . Prevalence of hypertension and associated cardiovascular risk factors among pharmacies customers: an Italian nationwide epidemiological survey. Eur J Prev Cardiol. 2020;27(11):1228‐1230. [DOI] [PubMed] [Google Scholar]
- 10. Pietropaoli D, Monaco A, Del Pinto R, Cifone MG, Marzo G, Giannoni M. Advanced glycation end products: possible link between metabolic syndrome and periodontal diseases. Int J Immunopathol Pharmacol. 2012;25(1):9‐17. [DOI] [PubMed] [Google Scholar]
- 11. Del Pinto R, Wright JT, Monaco A, Pietropaoli D, Ferri C. Vitamin D and blood pressure control among hypertensive adults: results from NHANES 2001–2014. J Hypertens. 2020;38(1):150‐158. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1
Figure S2
Figure S3


