Abstract
Live unattenuated vaccines (LUVs) have been neglected for decades, due to widespread prejudice against their safety, even though they have successfully controlled yellow fever and adenovirus infection in humans as well as rinderpest and infectious bursal disease in animals. This review elucidated that LUVs could be highly safe with selective use of neutralizing antivirus antibodies, natural antiglycan antibodies, nonantibody antivirals, and ectopic inoculation. Also, LUVs could be of high efficacy, high development speed, and high production efficiency, with the development of humanized monoclonal antibodies and other modern technologies. They could circumvent antibody‐dependent enhancement and maternal‐derived antibody interference. With these important advantages, LUVs could be more powerful than other vaccines for controlling some viral diseases, and they warrant urgent investigation with animal experiments and clinical trials for defeating the COVID‐19 pandemic caused by the novel coronavirus SARS‐CoV‐2.
Keywords: antibody, antiviral, COVID‐19, glycan, safety, SARS‐CoV‐2, vaccine, virus
Highlights
Live unattenuated vaccines (LUVs) could be highly safe and effectively.
LUVs could be based on neutralizing antivirus antibodies, natural antiglycan antibodies, nonantibody antivirals, and ectopic inoculation.
LUVs for human use could be based on humanized monoclonal antibodies.
LUVs could circumvent antibody‐dependent enhancement and maternal‐derived antibody interference.
LUvs could be more powerful than other vaccines for controlling some viral diseases, including COVID‐19.
1. INTRODUCTION
The whole world is eagerly waiting for safe and effective vaccines to control the COVID‐19 pandemic caused by the novel coronavirus SARS‐CoV‐2. 1 , 2 , 3 However, there could be multiple pitfalls for development of a qualified COVID‐19 vaccine, as indicated by decades of research on vaccines against animal coronaviruses and other human coronaviruses. 4 , 5
Vaccines for viral diseases include whole‐virus vaccines and subunit vaccines. 2 , 3 , 4 , 5 , 6 , 7 , 8 , 9 , 10 , 11 , 12 , 13 , 14 , 15 Whole‐virus vaccines harbor live vaccines and inactivated vaccines, and subunit vaccines rely on virion subunits presented by proteins, DNA, messenger RNA (mRNA), viral vectors, or antigen process cells (APCs). 3 , 4 , 5 , 6 Live vaccines, which are usually more efficient and less costly, prevent 13 human viral diseases, much more than those prevented by inactivated vaccines (n = 6) or subunit vaccines (n = 4). 10 , 11 , 12 However, as of 6 August 2020, no live vaccines, but six inactivated vaccines, and 25 subunit vaccines (seven protein‐based, five DNA‐based, six mRNA‐based, four viral vector‐based, and three APC‐based) have entered clinical trials for COVID‐19. 3
Live vaccines are live attenuated vaccines (LAVs), with some exceptions of live unattenuated vaccines (LUVs). 12 , 13 , 14 , 15 , 16 , 17 , 18 , 19 , 20 , 21 LAVs are excellent in efficacy and cost, but they are time‐consuming in development and dangerous to those with immunodeficiency. They also have the risk of pathogenic reversion. 13 , 14 , 15 Surprisingly, as elucidated below, LUVs could circumvent these disadvantages of LAVs. LUVs have successfully controlled multiple viral diseases, 16 , 17 , 18 , 19 , 20 , 21 and could carry other important advantages. Therefore, LUVs could be powerful for controlling viral diseases, including COVID‐19. However, due to widespread prejudice against the safety of LUVs, the great potential of LUVs has been neglected for decades.
2. SAFETY MECHANISMS
Like LAVs, LUVs inhibit viral replication and thus minimize viral pathogenesis and save time for the rising of acquired immunity. Unlike LAVs, which rely on genomic mutations to inhibit viral replication, LUVs inhibit viral replication through one or more mechanisms other than genomic changes, as shown in Figure 1.
Figure 1.
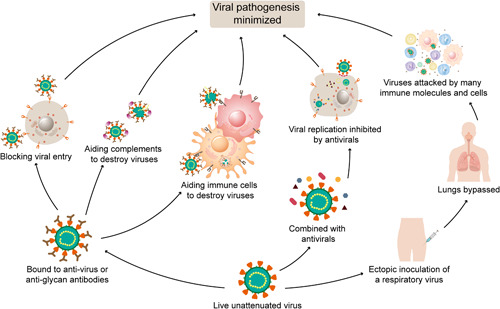
Safety mechanisms of live unattenuated vaccines based on antivirus antibodies, antiglycan antibodies, nonantibody antivirals, or ectopic inoculation
2.1. Antivirus antibody
This mechanism was discovered one century ago and possibly began with the control of rinderpest, which caused many deaths of cattle and buffalo worldwide six decades ago. 18 , 19 In the 1890s, Russian and South African scientists independently discovered that antibody‐containing immune serum taken from recovered animals and virus‐containing blood taken from infected animals, when given simultaneously, could safely induce long‐term immunity to rinderpest. This led to the birth of the antivirus antibody (AVA) LUV for rinderpest, and application of this vaccine eliminated rinderpest from southern Africa in 1905 and Russia in 1928. 18 , 19 Later, this LUV was replaced with a LAV not requiring immune sera for production. A limited supply of neutralizing AVA or immune sera has thwarted the application of AVA LUVs for long. 16 , 17 , 18 , 19 As elucidated below, humanized monoclonal antibodies (mAbs) can solve this problem and rejuvenate AVA LUVs.
Another AVA LUV was used successfully in controlling yellow fever in the 1930s. 16 , 17 Yellow fever is endemic in many countries in Africa and America for centuries and causes ∼30 000 deaths annually in recent years. 16 The LUC virus was a neurotropic strain, which grew in mouse brains and could cause severe systemic infection and encephalitis. 16 The LUV was prepared by mixing the live virus with immune serum collected from recovered people. A researcher was first inoculated with this vaccine in 1931. He was working at the Rockefeller Institute, where five researchers had died of the disease for developing yellow fever vaccines. He was hospitalized under strict isolation after the inoculation, and he did not show any symptoms. Then, his colleagues at the Rockefeller Institute were all vaccinated with the vaccine and safely obtained adequate immunity against the deadly disease. Then, this vaccine was safely used in the Western Hemisphere and England for several years. 16 Later, this LUV was replaced with a LAV not requiring immune sera for production. 16 , 17
Currently, an AVA LUV has been used successfully from the 1990s for the control of infectious bursal disease, an economically significant disease that affects chickens worldwide. 20 , 21 This LUV is a cocktail of a live pathogenic infectious bursal disease virus (IBDV) mixed with anti‐IBDV antibodies derived from hyperimmunized chicken sera. It is administered subcutaneously to day‐old chicks even in the presence of maternally derived antibodies (MDA). This LUV was found to be equal to or better than that of conventional LAVs in efficacy. 20 , 21 The success of this LUV indicates a potential approach to circumventing the MDA interference, which is a problem in vaccination against multiple viral diseases.
As per this mechanism, the live vaccine virus is mixed with enough neutralizing AVAs to form the virus‐antibody immune complexes, which inhibit the viral pathogenesis via three routes (Figure 1): blocking the virus to bind to its receptors on target cells, and thus blocking the viral entry and replication 22 , 23 , 24 ; activating the complement system to destroy the virus, via the binding of the antibody Fc fragments to complement proteins 25 ; presenting the virus to immune cells and aiding them to destroy the virus, via the binding of the antibody Fc fragments to the Fc receptors on the immune cells. 26 , 27 , 28 , 29 , 30 , 31 The virus could be destroyed through antibody‐dependent cell‐mediated cytotoxicity (ADCC) of natural killer cells and antibody‐dependent cellular phagocytosis (ADCP) of macrophages, dendritic cells, and other APCs. 26 , 27 , 28
In principle, AVA LUVs apply to all viruses except a few, such as human immunodeficiency virus (HIV) and African swine fever virus, 32 , 33 , 34 which can replicate efficiently in some immune cells carrying the Fc receptors, because AVA could aid the live pathogenic virus to enter and replicate in these cells through the Fc receptors.
The AVAs used for AVA LUV production are from the plasma or serum of recovered or vaccinated homologous hosts, which are of limited supply and contamination risk. 16 , 17 , 18 , 19 , 20 , 21 Humanized mAbs could be employed for the production of AVA LUVs because they can efficiently inhibit viral replication and aid complements and immune cells to destroy relevant viruses, and have been used successfully in the therapy of related viral diseases. 23 , 24 , 29 , 30 , 35 Moreover, the production of humanized mAbs has been highly efficient at relatively low cost. 24 , 35 One liter of Chinese hamster ovary (CHO) cell culture can produce 1 to 10 g humanized mAbs, 35 and thus 10 L of CHO cell culture could supply AVA for one million doses of an AVA LUV (<10μg/dose). 9 , 10 Therefore, this technology can rejuvenate AVA LUVs for preventing viral diseases.
To enhance the safety of LUVs based on humanized mAbs, it is better to use two or more humanized neutralizing mAbs targeting different epitopes for the production of an AVA LUV, like simultaneous use of handcuffs and fetters to lock some people and safely prevent them from committing crimes.
2.2. Antiglycan antibody
This mechanism is the same as AVA, except that the involved antibodies are antiglycan antibodies (AGAs), which are naturally abundant in hosts, usually due to frequent antigenic stimulation of gastrointestinal bacteria carrying the glycans. 12 , 36 AGAs produced in humans target over 100 kinds of glycans, including α1,3‐galactose (αGal) and N‐5‐glycolyl‐neuraminic acid. 31 , 37 Of these AGAs, anti‐αGal antibodies (anti‐αGal‐Abs) are the most abundant in humans, constituting ~1% of serum immunoglobulin G (IgG). 33 , 37 Anti‐αGal‐Abs also exist as IgA and IgG in milk, colostrum, saliva, and bile. 38 Thus, anti‐αGal‐Abs are the most suitable for human AGA LUVs. 12 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 , 51 , 52 , 53
Enveloped viruses replicating in cells of humans, apes, Old‐World monkeys lack αGal glycans (αGal‐Gs) because genomic mutations inactivated the enzyme α1,3 galactosyltransferase (α1,3GT) in these cells. 36 , 39 In contrast, enveloped viruses replicating in cells replicating nonprimate mammals, lemurs, or New‐World monkeys carry αGal glycans (αGal‐Gs) because these cells express active α1,3GT. 12 , 36 , 39 These viruses can bind to anti‐αGal‐Abs, and thus they can be used for producing AGA LUVs for humans.
Like AVA LUVs, AGA LUVs inhibit viral replication through three routes: blocking the viral entry, aiding complements to destroy the virus, and aiding immune cells to destroy the virus (Figure 1). For example, in vitro incubation of eastern equine encephalitis virus‐carrying αGal‐Gs with human anti‐αGal‐Abs blocked the replication of ∼50% of the virions in Vero cells, whereas such inhibition was not detected with the virus lacking αGal‐Gs. 36 , 42 It has been found that anti‐αGal‐Abs can aid complements to destroy over ten species of viruses carrying αGal‐Gs, 36 , 42 , 43 , 44 , 45 , 46 , 47 , 48 and aid immune cells to kill HIV‐1 through ADCC and ADCP. 49 Multiple studies demonstrated that anti‐αGal‐Abs could even aid immune cells to kill cancer cells and play a key role in rejecting xenografts carrying αGal‐Gs through ADCC. 36 , 50
AGA LUVs have not been marketed for control of viral diseases, but AGAs probably have protected humans for millions of years against infectious diseases caused by viruses from nonprimate animals. 12 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 This protection process involves virus killing and viral antigen‐capture aided by AGA (Figure 1), and should induce certainly acquired immunity against these viruses. Therefore, many people have been naturally inoculated with AGA LUVs against various viruses, although the doses might be too low to induce strong acquired immunity.
Although AGA LUVs can form the immune complexes in vivo postinoculation, the vaccine virus should be mixed with AGAs during the vaccine production, to ensure that the immune complexes of AGAs and the live vaccine virus are well‐formed in time in all vaccine recipients. 12 , 36
Unlike AVAs, AGAs are naturally available and can bind to many species of viruses, if they replicate in proper cell lines and present the target glycans. 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 , 51 However, their antiviral efficacy could be lower than that of neutralizing AVAs. Therefore, AGA LUVs could cause diseases in some cases. Usually, they should be used along with other safety mechanisms.
2.3. Nonantibody antiviral
As per this mechanism, replication of the live vaccine virus is inhibited by an antiviral, which could be a chemical, peptide, or medicinal herb. Unlike antibodies, the antiviral is unable to aid complements or immune cells to destroy the virus, but able to inhibit the viral entry, genome synthesis, protein cleavage, or virion assembly, and thus inhibits the virus replication (Figure 1). 54
Antivirals have cured many people infected with viruses and help them acquire specific immunity against the viruses. Otherwise, these people could have died of the infections. Therefore, many people have been naturally inoculated with nonantibody antiviral (NAA) LUVs against various viruses with various safety and efficacy, although no NAA LUVs have been marketed.
Currently, around 90 NAAs have been approved for the therapy of viral diseases. 55 With computer modeling and other modern technologies, the discovery and marketing of efficacious antivirals will be accelerated. 56 , 57 This will offer more opportunities for the development of NAA LUVs.
Notably, effective antivirals could be ineffective for curing patients with viral diseases. 13 This is because, for instance, an effective antiviral that can effectively inhibit the replication of SARS‐CoV‐2, could not repair the damages in some organs caused by the viral replication. On the other side, complete inhibition of SARS‐CoV‐2 from the very beginning of the infection with an antiviral can prevent COVID‐19, even if the antiviral has limited efficacy to repair the damages caused by the viral replication. Therefore, remdesivir and chloroquine phosphate could be used for COVID‐19 NAA LUVs as they effectively inhibit the viral replication, although they are not highly effective for curing COVID‐19 patients. 13 , 58 , 59 , 60
NAA LUVs could cause diseases in some cases. Usually, they should be used along with other safety mechanisms.
2.4. Ectopic inoculation
This mechanism has been applied safely for 40 years for preventing adenovirus‐associated acute respiratory disease in United States recruits, using two wild‐type adenoviruses inoculated enterally to bypass the pathogenesis site of the lungs. 13 , 61 , 62 This ETI LUV safely reduced clinical cases caused by types 4 and 7 adenoviruses in United States recruits by over 99%. 62
Beyond enteral inoculation, we recently proposed that intramuscular inoculation of a respiratory virus could also reduce its pathogenesis (Figure 2). 12 If the live vaccine is inoculated nasally, the live vaccine virus can attach directly to and replicate efficiently in its favorite cells. In contrast, if the live vaccine is inoculated intramuscularly, immune molecules and cells of the whole body, particularly those in the circulation system, could readily identify, capture, and destroy the injected virus. Therefore, the live virus could have limited chances to replicate in humans, and their limited replication is also inhibited by innate immunity of the whole body. To test this mechanism, mice were inoculated with 106 50% egg‐infective dose (EID50) of H5N6 subtype of the avian influenza virus through nasal and intramuscular administration. 12 All the mice inoculated nasally developed severe pneumonia and encephalitis with the mortality of 70%, while all the mice inoculated intramuscularly maintained health throughout the experiment and produced adequate immunity against nasal challenge with 108 EID50 of the same virus. 12
Figure 2.

Differences between nasal and intramuscular inoculation of a respiratory virus
ETI is readily available but may only be suitable to respiratory viruses. ETI LUVs could cause diseases in some cases, and usually, they should be used along with other safety mechanisms, except that their safety has been well‐confirmed through animal experiments and clinical trials.
3. ADVANTAGES
LUVs could have multiple important advantages over other vaccines.
3.1. High safety
AVA LUVs using humanized neutralizing mAbs could be safer than LAVs because the live virus is always bound with the neutralizing antibodies, like people locked in handcuffs and fetters. Therefore, they could be used in humans with immunodeficiency. This is supported by multiple studies showing that humanized neutralizing mAbs effectively blocked infection and suppressed viremia in rhesus macaques and humans with immunodeficiency. 29 , 30 As demonstrated by the LUV for adenovirus infection, LUVs based on other safety mechanisms could also have adequate safety, particularly when two or more safety mechanisms are used simultaneously. Notably, animal experiments and clinical trials should be conducted to confirm whether a LUV is safe adequately. 9 , 10 , 11 , 12 , 13
3.2. High efficacy
Usually, LAVs are more efficacious than inactivated vaccines and subunit vaccines, and LUVs could be more efficacious than LAVs because their antigenic epitopes are the same as those of the wild‐type viruses. This is supported by the experiments, which showed that influenza LAVs based on rare codons without changes in antigenic epitopes were more efficacious than influenza cold‐adapted LAVs with changes in antigenic epitopes. 63 High efficacy of some LUVs was also demonstrated by the fact that the past three influenza pandemics, which could be considered as mass vaccination with influenza LUVs, all eliminated one ingrained subtype of influenza virus sharing the same subtype or some genomic segments with the pandemic virus from humans. 64 Furthermore, AVA LUVs and AGA LUVs can enhance their efficacy through immune opsonization: via the binding of the antibody Fc fragments to the Fc receptors on APCs; the antibodies assist APCs to capture, process, and present relevant antigenic epitopes to T and B cells. 27 , 31 , 51 , 52 , 53
3.3. High development speed
LUVs could be developed rapidly in many countries because they neither require time‐consuming and technology‐requiring attenuation of the virus, nor raise concern regarding pathogenic reversion. Development of AVA LUVs or NAA LUVs can be accelerated if relevant humanized neutralizing mAbs or effective antivirals have been available. AGA LUVs and ETI LUVs could be developed more rapidly, as these mechanisms are naturally available. 12
3.4. High production efficiency
LUVs could be produced efficiently, like LAVs. For instance, around 10 billion virions are required for producing one dose of inactivated influenza vaccine, and these virions could be used for producing 1000 doses of LUVs or LAVs. 12 , 63
3.5. Avoiding vaccination pitfalls
As LUVs could be highly efficacious, they have the potential to circumvent the vaccination risk of antibody‐dependent enhancement (ADE), a major potential pitfall for vaccine development. 60 , 65 ADE is a mechanism through which dengue viruses, feline coronaviruses, SARS coronavirus, and HIV viruses take advantage of low levels of antiviral antibodies to infect host cells. 65 Moreover, AVA LUVs and AGA LUVs could circumvent the interference of MDA, as indicated by the AVA LUV used for chicken infectious bursal disease. 20 , 21 Meanwhile, the protection effect of MDA could be unaffected with inoculation of AVA LUVs, as the LUVs can be bound with neutralizing antibodies before inoculation, and the vaccine virus cannot replicate efficiently in vivo. This is different from LAV inoculation, which usually consumes MDA significantly and thus reduces the protection effect of MDA against the relevant disease. Consequently, LAV recipients could be more susceptible to the disease for some days after LAV inoculation than before the inoculation. This could be another reason why LUVs could be safer than LAVs.
4. APPLICATIONS
With the above important advantages, LUVs could be powerful for controlling COVID‐19. AVA LUVs for COVID‐19 could be the safest and most efficient. Currently, over 60 humanized neutralizing mAbs have been under investigation for the therapy of COVID‐19, 3 , 22 , 23 , 24 greatly facilitating the development of AVA LUVs for COVID‐19. As humanized mAbs are usually produced using murine CHO cells, 22 they carry αGal glycans and can bind to anti‐Gal‐Abs, which are abundant in humans. 66 Moreover, LUVs can be inoculated intramuscularly. Therefore, the AVA LUVs can simultaneously utilize the mechanisms of AGA and ETI, further securing the safety and efficacy of the vaccines.
The simplest COVID‐19 LUVs rely on the mechanisms of AGA and ETI. These LUVs could be as simple as intramuscular inoculation of live SARS‐CoV‐2, which is produced using porcine PK‐15 cells and thus carries αGal‐Gs. 12 It is highly recommended that, during the vaccine production, the live virus is mixed with AGA purified from human sera, to ensure that the immune complexes of AGA and SARS‐CoV‐2 are well‐formed in time. 12 Although AGA LUVs could be less safe than AVA LUVs, they could be safe adequately for COVID‐19, and they can be developed and produced in many more countries with much higher efficiency. Notably, not only vaccine safety and efficacy, but also vaccine development speed and production efficiency are important for reducing deaths and losses caused by COVID‐19. 13 , 67
LUVs can be employed for the prevention of other viral diseases, such as respiratory syncytial virus infection, the leading cause of viral lower respiratory tract infection in children. 68 , 69 Tremendous efforts have not succeeded so far in marketing a vaccine for this disease. Multiple humanized neutralizing mAbs have been approved as therapeutics of this disease, and potential NAAs against this virus have also been reported. 68 , 69 These agents greatly facilitate the development of AVA LUVs or NAA LUVs for this respiratory disease. Again, AVA LUVs could be the safest and most efficacious for this disease, and they could simultaneously utilize the mechanisms of AGA and ETI. The AVA LUVs could circumvent the ADE pitfall and the MDA interference, both of which have been observed with this disease. 70
5. CONCLUSIONS
This article elucidates that LUVs could be highly safe with selective use of neutralizing AVAs, natural AGAs, NAAs, and ETI. It also suggests that LUVs could be of high efficacy, high development speed, and high production efficiency, with the aid of modern technologies. They could circumvent antibody‐dependent enhancement and MDA interference. With these important advantages, LUVs could be more potent than other vaccines for controlling some viral diseases, and they warrant urgent investigation using animal experiments and clinical trials for defeating the COVID‐19 pandemic.
CONFLICT OF INTERESTS
The authors declare that there are no conflict of interests.
AUTHOR CONTRIBUTION
JMC conducted this study alone.
ACKNOWLEDGMENTS
The author thanks Meng Yang and Jiwang Chen for their helpful assistance.
Chen J‐M. Live unattenuated vaccines for controlling viral diseases, including COVID‐19. J Med Virol. 2021;93:1943–1949. 10.1002/jmv.26453
DATA AVAILABILITY STATEMENT
The data supporting the views of this article are available from the corresponding author on request.
REFERENCES
- 1. World Health Organization . Coronavirus disease (COVID‐2019) situation reports. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports/. Accessed on 6 August 2020.
- 2. World Health Organization . The power of vaccines: still not fully utilized. https://www.who.int/publications/10-year-review/vaccines/en/. Accessed on 6 August 2020.
- 3. BioRender . COVID‐19 vaccine & therapeutics tracker. https://biorender.com/covid-vaccine-tracker. Accessed on 6 August 2020.
- 4. Zhang J, Zeng H, Gu J, et al. Progress and prospects on vaccine development against SARS‐CoV‐2. Vaccines. 2020;8:153. 10.3390/vaccines8020153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Tizard IR. Vaccination against coronaviruses in domestic animals. Vaccine. 2020;38:5123‐5130. 10.1016/j.vaccine.2020.06.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Corbett KS, Edwards D, Leist SR, et al. SARS‐CoV‐2 mRNA vaccine development enabled by prototype pathogen preparedness. Nature. 2020. 10.1101/2020.06.11.145920 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Zhu FC, Li YH, Guan XH, et al. Safety, tolerability, and immunogenicity of a recombinant adenovirus type‐5 vectored COVID‐19 vaccine: a dose‐escalation, open‐label, non‐randomised, first‐in‐human trial. Lancet. 2020;395:1845‐1854. 10.1016/S0140-6736(20)31208-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Gao Q, Bao L, Mao H, et al. Development of an inactivated vaccine candidate for SARS‐CoV‐2. Science. 2020;369:77‐81. 10.1126/science.abc1932 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Wang H, Zhang Y, Huang B, et al. Development of an inactivated vaccine candidate, BBIBP‐CORV, with potent protection against SARS‐CoV‐2. Cell. 2020;182:1‐9. 10.1016/j.cell.2020.06.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Hajj Hussein I, Chams N, Chams S, et al. Vaccines through centuries: major cornerstones of global health. Front Public Health. 2015;3:269. 10.3389/fpubh.2015.00269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. World Health Organization . Immunization, vaccines and biologicals. https://www.who.int/immunization/diseases/en/. Accessed on 6 August 2020.
- 12. Chen JM. SARS‐CoV‐2 replicating in non‐primate mammalian cells probably have critical advantages for COVID‐19 vaccines due to anti‐αGal antibodies: a minireview and proposals. J Med Virol. 2020;92. 10.1002/jmv.26312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Chen JW, Chen JM. Potential of live pathogen vaccines for defeating the COVID‐19 pandemic: history and mechanism. J Med Virol. 2020;92(9):1469–1474. 10.1002/jmv.25920 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Enjuanes Sánchez L, Jiménez‐Guardeño JM, Regla‐Nava JÁ, et al. Identification of the mechanisms causing reversion to virulence in an attenuated SARS‐CoV for the design of a genetically stable vaccine. PLOS Pathog. 2015;11:e1005215. 10.1371/journal.ppat.1005215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Pöyhönen L, Bustamante J, Casanova JL, Jouanguy E, Zhang Q. Life‐threatening infections due to live‐attenuated vaccines: early manifestations of inborn errors of immunity. J Clin Immunol. 2019;39:376‐390. 10.1007/s10875-019-00642-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Frierson JG. The yellow fever vaccine: a history. Yale J Biol Med. 2010;83:77‐85. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2892770/ [PMC free article] [PubMed] [Google Scholar]
- 17. Yan K, Vet LJ, Tang B, et al. A yellow fever virus 17D infection and disease mouse model used to evaluate a chimeric Binjari‐yellow fever virus vaccine. Vaccines. 2020;8:E368. 10.3390/vaccines8030368 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Food and Agriculture Organization . Ridding the world of rinderpest. https://assets.publishing.service.gov.uk/media/57a08b2040f0b652dd000af4/DFID_impact_case_study_Rinderpest_April2010_1_.pdf. Accessed on 6 August 2020.
- 19. Roeder P, Mariner J, Kock R. Rinderpest: the veterinary perspective on eradication. Philos Trans R Soc Lond B Biol Sci. 2013;368:20120139. 10.1098/rstb.2012.0139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Dey S, Pathak DC, Ramamurthy N, Maity HK, Chellappa MM. Infectious bursal disease virus in chickens: prevalence, impact, and management strategies. Vet. Med. (Auckl). 2019;10:85‐97. 10.2147/VMRR.S185159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Sedeik ME, El‐Shall NA, Awad AM, Abd El‐Hack ME, Alowaimer AN, Swelum AA. Comparative evaluation of HVT‐IBD vector, immune complex, and live IBD vaccines against vvIBDV in commercial broiler chickens with high maternally derived antibodies. Animals (Basel). 2019;9:72. 10.3390/ani9030072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Zost SJ, Gilchuk P, Case JB, et al. Potently neutralizing and protective human antibodies against SARS‐CoV‐2. Nature. 2020;584(7821):443–449. 10.1038/s41586-020-2548-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Wan J, Xing S, Ding L, et al. Human‐IgG‐neutralizing monoclonal antibodies block the SARS‐CoV‐2 infection. Cell Rep. 2020;32(3):107918. 10.1016/j.celrep.2020.107918 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Pelegrin M, Naranjo‐Gomez M, Piechaczyk M. Antiviral monoclonal antibodies: can they be more than simple neutralizing agents? Trends Microbiol. 2015;23:653‐665. 10.1016/j.tim.2015.07.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Hester CG, Frank MM. Complement activation by IgG containing immune complexes regulates the interaction of C1q with its ligands. Mol Immunol. 2019;116:117‐130. 10.1016/j.molimm.2019.10.004 [DOI] [PubMed] [Google Scholar]
- 26. Su B, Dispinseri S, Iannone V, et al. Update on Fc‐mediated antibody functions against HIV‐1 beyond neutralization. Front Immunol. 2019;10:2968. 10.3389/fimmu.2019.02968 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Wen YM, Shi Y. Immune complex vaccination. Curr Top Microbiol Immunol. 2019;423:95‐118. 10.1007/82_2019_153 [DOI] [PubMed] [Google Scholar]
- 28. Lambour J, Naranjo‐Gomez M, Piechaczyk M, Pelegrin M. Converting monoclonal antibody‐based immunotherapies from passive to active: bringing immune complexes into play. Emerg Microbes Infect. 2016;5:e92. 10.1038/emi.2016.97 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Salazar G, Zhang N, Fu TM, An Z. Antibody therapies for the prevention and treatment of viral infections. NPJ Vaccines. 2017;2:19. 10.1038/s41541-017-0019-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Caskey M, Klein F, Lorenzi JC, et al. Viraemia suppressed in HIV‐1‐infected humans by broadly neutralizing antibody 3BNC117. Nature. 2015;522:487‐491. 10.1038/nature14411 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Wang X, Wang B, Wen Y. From therapeutic antibodies to immune complex vaccines. NPJ Vaccines. 2019;4:2. 10.1038/s41541-018-0095-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Cunningham AL, Donaghy H, Harman AN, Kim M, Turville SG. Manipulation of dendritic cell function by viruses. Curr Opin Microbiol. 2010;13:524‐529. 10.1016/j.mib.2010.06.002 [DOI] [PubMed] [Google Scholar]
- 33. Kyle JL, Beatty PR, Harris E. Dengue virus infects macrophages and dendritic cells in a mouse model of infection. J Infect Dis. 2007;195:1808‐1817. 10.1086/518007 [DOI] [PubMed] [Google Scholar]
- 34. Chen W, Zhao D, He X, et al. A seven‐gene‐deleted African swine fever virus is safe and effective as a live attenuated vaccine in pigs. Sci China: Life Sci. 2020;63:623‐634. 10.1007/s11427-020-1657-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Kunert R, Reinhart D. Advances in recombinant antibody manufacturing. Appl Microbiol Biotechnol. 2016;100:3451‐3461. 10.1007/s00253-016-7388-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Galili U. Human natural antibodies to mammalian carbohydrate antigens as unsung heroes protecting against past, present, and future viral infections. Antibodies. 2020;9:E25. 10.3390/antib9020025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Stowell SR, Arthur CM, McBride R, et al. Microbial glycan microarrays define key features of host‐microbial interactions. Nat Chem Biol. 2014;10:470‐476. 10.1038/nchembio.1525 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Hamadeh RM, Galili U, Zhou P, Griffiss JM. Anti‐alpha‐galactosyl immunoglobulin A (IgA), IgG, and IgM in human secretions. Clin Diagn Lab Immunol. 1995;2:125‐131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Galili U, Swanson K. Gene sequences suggest inactivation of α1‐3 Galactosyltransferase in catarrhines after the divergence of apes from monkeys. Proc Natl Acad Sci U S A. 1991;88:7401‐7404. 10.1073/pnas.88.16.7401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Montassier E, Al‐Ghalith GA, Mathé C, et al. Distribution of bacterial α1,3‐galactosyltransferase genes in the human gut microbiome. Front Immunol. 2020;10:3000. 10.3389/fimmu.2019.03000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Almeida IC, Ferguson MA, Schenkman S, Travassos LR. Lytic anti‐α‐galactosyl antibodies from patients with chronic Chagas’ disease recognize novel O‐linked oligosaccharides on mucin‐like glycosyl‐phosphatidylinositol‐anchored glycoproteins of Trypanosoma cruzi . Biochem J. 1994;304:793‐802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Repik PM, Strizki M, Galili U. Differential host dependent expression of α‐galactosyl glycans on viral glycoproteins: a study of Eastern equine encephalitis virus as a model. J Gen Virol. 1994;75:1177‐1181. 10.1099/0022-1317-75-5-1177 [DOI] [PubMed] [Google Scholar]
- 43. Takeuchi Y, Porter CD, Strahan KM, et al. Sensitization of cells and retroviruses to human serum by α1‐3 galactosyltransferase. Nature. 1996;379:85‐88. 10.1038/379085a0 [DOI] [PubMed] [Google Scholar]
- 44. Welsh RM, O'Donnell CL, Reed DJ, Rother RP. Evaluation of the Galα1‐3Gal epitope as a host modification factor eliciting natural humoral immunity to enveloped viruses. J Virol. 1998;72:4650‐4656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Preece AF, Strahan KM, Devitt J, Yamamoto F, Gustafsson K. Expression of ABO or related antigenic carbohydrates on viral envelopes leads to neutralization in the presence of serum containing specific natural antibodies and complement. Blood. 2002;99:2477‐2482. 10.1182/blood.v99.7.2477 [DOI] [PubMed] [Google Scholar]
- 46. Rother RP, Fodor WL, Springhorn JP, et al. A novel mechanism of retrovirus inactivation in human serum mediated by anti‐α‐galactosyl natural antibody. J Exp Med. 1995;182:1345‐1355. 10.1084/jem.182.5.1345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Hayashi S, Ogawa S, Takashima Y, Otsuka H. The neutralization of pseudorabies virus by anti‐α‐Galactocyl natural antibody in normal serum. Virus Res. 2004;99:1‐7. 10.1016/j.virusres.2003.09.008 [DOI] [PubMed] [Google Scholar]
- 48. Pipperger L, Koske I, Wild N, et al. Xenoantigen‐dependent complement‐mediated neutralization of LCMV glycoprotein pseudotyped VSV in human serum. J Virol. 2019;93:e00567‐19. 10.1128/JVI.00567-19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Perdomo MF, Levi M, Sällberg M, Vahlne A. Neutralization of HIV‐1 by redirection of natural antibodies. Proc Natl Acad Sci U S A. 2008;105:12515‐12520. 10.1073/pnas.0805777105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Shaw SM, Middleton J, Wigglesworth K, et al. AGI‐134: a fully synthetic α‐Gal glycolipid that converts tumors into in situ autologous vaccines, induces anti‐tumor immunity and is synergistic with an anti‐PD‐1 antibody in mouse melanoma models. Cancer Cell Int. 2019;19:346. 10.1186/s12935-019-1059-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Abdel‐Motal UM, Guay HM, Wigglesworth K, Welsh RM, Galili U. Increased immunogenicity of influenza virus vaccine by anti‐Gal mediated targeting to antigen presenting cells. J Virol. 2007;81:9131‐9141. 10.1128/JVI.00647-07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Abdel‐Motal UM, Wang S, Awad A, Lu S, Wigglesworth K, Galili U. Increased immunogenicity of HIV‐1 p24 and gp120 following immunization with gp120/p24 fusion protein vaccine expressing α‐Gal epitopes. Vaccine. 2010;28:1758‐1765. 10.1016/j.vaccine.2009.12.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Benatuil L, Kaye J, Rich RF, Fishman JA, Green WR, Iacomini J. The influence of natural antibody specificity on antigen immunogenicity. Eur J Immunol. 2005;35:2638‐2647. 10.1002/eji.200526146 [DOI] [PubMed] [Google Scholar]
- 54. Saxena A. Drug targets for COVID‐19 therapeutics: ongoing global efforts. J Biosci. 2020;45:87. 10.1007/s12038-020-00067-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Wikipedia . List of antiviral drugs. https://en.wikipedia.org/wiki/List_of_antiviral_drugs. Accessed on 6 August 2020.
- 56. Raimondi MT, Donnaloja F, Barzaghini B, et al. Bioengineering tools to speed up the discovery and preclinical testing of vaccines for SARS‐CoV‐2 and therapeutic agents for COVID‐19. Theranostics. 2020;10:7034‐7052. 10.7150/thno.47406 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Everts M, Cihlar T, Bostwick JR, Whitley RJ. Accelerating drug development: antiviral therapies for emerging viruses as a model. Annu Rev Pharmacol Toxicol. 2017;57:155‐169. 10.1146/annurev-pharmtox-010716-104533 [DOI] [PubMed] [Google Scholar]
- 58. Wang M, Cao R, Zhang L, et al. Remdesivir and chloroquine effectively inhibit the recently emerged novel coronavirus (2019‐nCoV) in vitro. Cell Res. 2020;30:269‐271. 10.1038/s41422-020-0282-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Samudrala PK, Kumar P, Choudhary K, et al. Virology, pathogenesis, diagnosis and in‐line treatment of COVID‐19. Eur J Pharmacol. 2020;883:173375. 10.1016/j.ejphar.2020.173375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Cao X. COVID‐19: immunopathology and its implications for therapy. Nat Rev Immunol. 2020;20:269‐270. 10.1038/s41577-020-0308-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Couch RB, Chanock RM, Cate TR, et al. Immunization with types 4 and 7 adenovirus by selective infection of the intestinal tract. Am Rev Respir Dis. 1963;88(Suppl):394‐403. 10.1164/arrd.1963.88.3P2.394 [DOI] [PubMed] [Google Scholar]
- 62. Choudhry A, Mathena J, Albano JD, Yacovone M, Collins L. Safety evaluation of adenovirus type 4 and type 7 vaccine live, oral in military recruits. Vaccine. 2016;34:4558‐4564. 10.1016/j.vaccine.2016.07.033 [DOI] [PubMed] [Google Scholar]
- 63. Stauft CB, Yang C, Coleman JR, et al. Live‐attenuated H1N1 influenza vaccine candidate displays potent efficacy in mice and ferrets. PLOS One. 2019;14:e0223784. 10.1371/journal.pone.0223784 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Chen JM, Sun YX, Chen JW. Potential for elimination of SAR‐CoV‐2 through vaccination as inspired by elimination of multiple influenza viruses through natural pandemics or mass vaccination. J Med Virol. 2020;92 10.1002/jmv.26162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Wang SF, Tseng SP, Yen CH, et al. Antibody‐dependent SARS coronavirus infection is mediated by antibodies against spike proteins. Biochem Biophys Res Commun. 2014;451:208‐214. 10.1016/j.bbrc.2014.07.090 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Wallner J, Sissolak B, Sommeregger W, Lingg N, Striedner G, Vorauer‐Uhl K. Lectin bio‐layer interferometry for assessing product quality of Fc‐ glycosylated immunoglobulin G. Biotechnol Prog. 2019;35:e2864. 10.1002/btpr.2864 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Rubin R. Challenge trials—could deliberate coronavirus exposure hasten vaccine development? JAMA. 2020;324:12‐14. 10.1001/jama.2020.9881 [DOI] [PubMed] [Google Scholar]
- 68. Sesterhenn F, Yang C, Bonet J, et al. De novo protein design enables the precise induction of RSV‐neutralizing antibodies. Science. 2020:368. 10.1126/science.aay5051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Yang SNY, Atkinson SC, Audsley MD, Heaton SM, Jans DA, Borg NA. RK‐33 is a broad‐spectrum antiviral agent that targets DEAD‐Box RNA helicase DDX3X. Cells. 2020;9:170. 10.3390/cells9010170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Mejias A, Rodríguez‐Fernández R, Oliva S, Peeples ME, Ramilo O. The journey to a respiratory syncytial virus vaccine. Ann Allergy Asthma Immunol. 2020;125:36‐46. 10.1016/j.anai.2020.03.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data supporting the views of this article are available from the corresponding author on request.


