Abstract
The purpose of this commentary was to outline several key considerations and challenges for medical imaging departments during a global pandemic. Five public hospital medical imaging departments were identified in South‐East Queensland, Australia, to provide insight into their response to the COVID‐19 pandemic. Common themes were identified, with the four considered most pertinent documented in this commentary. Similar operational considerations and challenges were identified amongst all sites. This commentary intends to serve as a starting point for medical imaging departments in considering the planning and implementation of services in a pandemic scenario.
Keywords: COVID‐19, management, medical imaging, pandemic, radiography
This commentary considers multiple considerations and challenges for Medical Imaging Departments in responding to the COVID‐19 pandemic. It themes these considerations as infection control, resources, communication and change management.
Introduction
The COVID‐19 pandemic represents the largest, most dynamic challenge to global healthcare systems in living memory. As the virus and its impact spread, healthcare systems around the world have responded with innovative, large‐scale protective measures, reallocation of resources and changes in service delivery. Medical imaging has played an essential role in diagnosis, assisting in prognosis and evaluation of treatment interventions throughout the COVID‐19 pandemic. 1 , 2 , 3 , 4
COVID‐19 Global Timeline
On 31 December 2019, an epidemic consisting of cases with unexplained low respiratory tract infections was detected in Wuhan, China and reported to the World Health Organisation (WHO). 5 It would be later named severe acute respiratory syndrome (SARS) coronavirus 2 (SARS‐CoV‐2). 6 The WHO announced that this disease was caused by coronavirus disease 2019 (COVID‐19) on 11 February 2020. By the 11 March 2020, there had been 118,000 cases in 114 countries and over 4000 deaths, prompting the WHO to declare COVID‐19 a pandemic. 7 At the time of writing (30 June 2020), the WHO had reported over 10.1 million confirmed cases, with 502,278 deaths in 216 countries worldwide. 8
COVID‐19 in Australia
Australia’s first confirmed case of COVID‐19 was reported in late January 2020. 9 At 30 June 2020, Australia had recorded a total of 7834 cases, 104 deaths and 7,037 patients recovered. 10 Over 60% of Australian cases have been traced to overseas sources of infection. 11
Australia’s approach to responding to the pandemic was to ‘flatten the curve’. Based on modelling of different transmission rates, the ‘curve’ demonstrates the likely number of people who would contract COVID‐19 over a period of time. 12 The main intention behind flattening this curve was to keep demand for healthcare resources as low as possible, ideally below the capacity of the healthcare system to provide them. This was achieved by various physical distancing and contact tracing activities. Strategies implemented in Australia included, but were not limited to; international and state border closures, closure of non‐essential businesses, local lockdown measures particularly in aged care, physical distancing, working from home and closures of education facilities. 13 , 14 Figure 1 15 demonstrates the success of these strategies in slowing down the spread of COVID‐19. This enabled the healthcare system sufficient time to prepare, diversify and build capacity to cope with the likely increase in demand from patients presenting with suspected COVID‐19. Preparations included procurement of equipment, resource deployment, logistical arrangements and operational planning and were guided by experience and evidence in a collaborative and agile manner.
Figure 1.
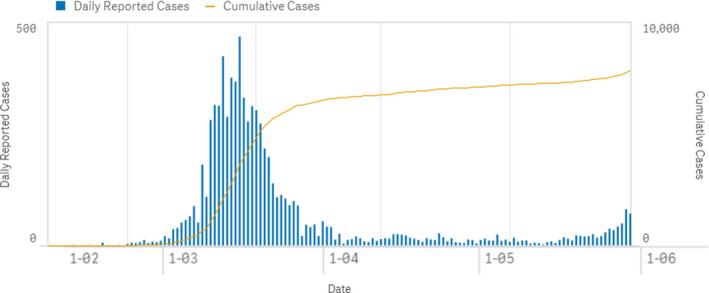
Daily and cumulative number of reported COVID‐19 cases in Australia in February to June 2020 – the ‘curve’ (permission obtained from Department of Health to reproduce the figure).
The purpose of this commentary was to offer Australian medical imaging departments (MIDs) several operational perspectives on how different services responded to the COVID‐19 pandemic. Furthermore, it explores considerations for reviewing existing processes and preparing for a possible secondary COVID‐19 surge or similar future pandemic. This article sought the operational responses of five medical imaging departments within public hospitals in South East Queensland. These views and recommendations derive from the authors’ experiences, a review of current literature and resources, many of which are referenced throughout this commentary. Some recommendations are based on untestable assumptions, any of which may be reasonably challenged. The authors propose specific priorities for the purpose of preparing a medical imaging department for a pandemic. Implementation of these strategies should be carefully considered in line with local laws, prevailing conditions, organisational objectives and strategies.
Contributing Hospitals
In Queensland, public healthcare services are categorised into 6 levels, as outlined by the Clinical Skills Capability Framework (CSCF) which proposes minimum requirements for the provision of health services. 16 Table 1 presents the CSCF levels of hospitals whose MIDs contributed to this commentary. Each contributing hospital has a designated MID with a full suite of general diagnostic modalities and varying levels of subspecialty, nuclear medicine and interventional radiology capabilities. Staff that contributed to this pandemic response included managers, radiologists, radiographers, nuclear medicine technologists, nurses, medical imaging assistants and administrative support staff.
Table 1.
Clinical skills capabilities framework of contributing medical imaging departments.
| Name of hospital | Category (1–6) | Number of beds |
|---|---|---|
| The Royal Brisbane and Women’s Hospital | 6 | 1000 |
| Princess Alexandra Hospital | 6 | 1050 |
| Logan Hospital | 5 | 441 |
| The Sunshine Coast University Hospital | 5 | 567 |
| Nambour General Hospital | 4 | 150 |
Pertinent Themes
Following an initial online (via Microsoft Teams) discussion and serial emails, all sites detailed numerous aspects of the changes and considerations in their response to the pandemic. From these, four pertinent themes emerged; infection control, resources, communication and change management.
Infection Control
All authors agreed that the primary operational goal at the onset of the pandemic was infection control, specifically pertaining to the protection of staff and non‐infected patients, to ensure their safety. Staff were consistently reminded of their role regarding physical distancing (within and outside the workplace), cough etiquette and hand hygiene. Reminders were delivered via regular emails, informative posters, physical demarcation on the floor and barriers outlining suitable physical distancing in clinical and non‐clinical areas.
At the start of the pandemic, several staff were overseas and then returned to Australia. In complying with government direction, 17 these team members were required to enter self‐isolation and undergo COVID‐19 testing before returning to their workplaces. Staff were also encouraged to consider whether they met specific criteria as being ‘vulnerable staff’. These criteria were designed to identify those at high risk from the effects of COVID‐19, due to existing health conditions and/or personal circumstances. 18 Staff that identified as vulnerable were re‐deployed to lower risk areas within the MIDs to mitigate exposure, or elected to not attend work on medical advice. This ensured their safety was prioritised.
The provision and safe use of personal protective equipment (PPE) was a major concern for MID staff. The rapid rollout of mandatory PPE training for all employees ensured its appropriate and safe use whilst alleviating confusion. Training was limited to being non‐practical, due to requirements to preserve PPE by minimising non‐essential usage. Staff were commonly unable to ‘don and doff’ 19 until in a clinical scenario that required it, relying on written, pictorial or video learning resources to gain competency and reassurance. The utilisation of ‘spotters’ provided support, allayed fears and afforded important redundancy within this safety system. Clear, visible and accessible procedures regarding donning and doffing, room preparation, patient flow and post‐examination cleaning were vital, as staff were required to respond to rapidly changing information.
The potential for PPE breaches was of constant concern for staff performing medical imaging for patients infected with COVID‐19. Clear identification of patients who were confirmed or suspected of being COVID‐19 positive was paramount. Several sites used colours such as green (non‐suspected COVID‐19) and purple (suspected COVID‐19) to identify patient COVID‐19 status. Furthermore, sites allocated specific zones for patients suspected of being COVID‐19 positive. These clinical workflow strategies further reduced staff exposure and PPE use. The management of staff potentially exposed in the clinical environment was defined through local protocols developed by local infection control teams. All sites adopted documentation logs of all suspected COVID‐19 patients and staff involved in their imaging, for contact tracing purposes. All PPE breaches were followed up to provide reassurance or advice once the COVID‐19 status of the pertinent patient was determined.
Some services considered alternative rostering arrangements to reduce the risk of exposure within departments, and the impact on operational capacity should a team member have become infected. Government advice required all close contacts of confirmed cases of COVID‐19 to isolate for 14 days. Therefore, a single positive test within a team could potentially have greatly reduced departmental service capacity, a scenario identified as catastrophic for smaller MIDs. Multiple options for developing team‐based rosters were considered by contributing sites. Shift overlap was approached differently between MIDs, with some removing it whilst others maintained it. Skill mix, staffing levels (particularly overnight), on‐call capability of staff and managers and the ability to work in pairs were all options considered throughout the 24‐hour period of service. A key challenge in developing a team‐based roster was the trigger for implementation. Factors included, number of unavailable staff (e.g. COVID‐19 contact/positive, school closures) and numbers of cases presenting to each site. None of the contributing MIDs were required to trigger their full pandemic rosters.
Resources
Staffing and equipment resource contingencies were considered by all contributing MIDs during the pandemic. Some services rapidly on‐boarded casual staff to prepare for potential shortfalls. Queensland Health also invited expressions of interest for healthcare workers, for rapid deployment if required. Many staff also cancelled leave, boosting staff levels and operational capacity.
At the height of the pandemic, PPE access was a significant challenge. This was intensified in smaller sites where management was often required to advocate for their staff to ensure PPE availability. Unfortunately, all sites experienced theft of these vital resources. Measures included locking up PPE and the provision of identified gatekeepers, to reduce theft and ensure ongoing accessibility. Centralisation of PPE resource management was implemented across contributing health services, providing regular and reliable supply of PPE. With the often overwhelming stream of information, identifying a facility PPE expert resource and trusting that resource was critical for staff safety. 20
The allocation of equipment resources in a rational, organised fashion was imperative in the early stages. All contributing MIDs designated specific equipment and examination rooms for positive and high‐risk COVID‐19 patients. This also occurred for mobile imaging equipment, which was assigned to specific clinical areas of need when a significant increase in demand for mobile chest X‐rays was noted. This challenge was overcome by the purchase, rapid acquisition and deployment of additional mobile X‐ray units. Importantly, the designation of equipment and rooms was accompanied by clear, documented workflows covering transport and imaging of patients within these specific areas. Clearly defined roles for all team members before and after examinations were assigned and communicated. The adoption of paired staff teams was imperative but required considerable re‐allocation of staffing resources. Providing such capacity for paired staff teams ensured limitation of staff exposure, the support of a spotter and reduction in PPE use.
Sonographers faced a unique challenge, as their work required close patient contact for extended periods. 21 All ultrasound examinations for suspected COVID‐19 cases required detailed discussion between referring and radiology teams prior to scanning. Protocoling for examinations by radiologists to limit scan times was imperative. Due to the increased risk, utilisation of ultrasound examinations in the presence of COVID‐19 was considered a last resort.
Consideration was given to the radiation safety of staff and the public when changes in clinical practice and new techniques were adopted. 22 Departments who worked closely with medical physics colleagues were quickly able to measure and address any concerns, ensuring staff and public safety in line with local Radiation Safety and Protection Plans (RSPPs). 23
Communication
Communication provides the greatest challenge to all organisations during a crisis. 24 During the pandemic’s initial phase, there was an overwhelming amount of information communicated through mainstream, digital and social media platforms. This created a sense of fear for staff, greatly impacting their ability to provide services. Much of this fear was alleviated through open, honest and transparent planning and decision‐making, supported by considered staff training. Departments quickly established a single, credible ‘point of truth’ for rapid communication and dissemination of reliable information. Many services adopted a single, daily email sent late in the day which collated all recent changes into one source. Providing staff time to assimilate information and absorb recent changes when starting shifts was adopted by some departments. Multiple forums for questions and answers during planning and training supported and reassured the staff of the organisational ability to manage the evolving crisis. New workplace instructions were drafted, reviewed and disseminated, outlining equipment designation, workflow changes, PPE and cleaning processes. These documents were revised multiple times following rapidly evolving advice from organisational leaders. These measures ensured consistent and inclusive messaging was communicated to all staff.
With strict adherence to physical distancing guidelines in the workplaces, alternative avenues of communication were identified and adopted. All contributing services successfully adopted Microsoft Office Teams 25 as a digital platform for communication through messaging, video conferencing and document storage. This application was accessible and available to all staff through personal mobile devices. A challenge in using this application was the inability of the organisational Wi‐Fi to reliably support video applications.
A co‐ordinated effort was undertaken by all departments to triage outpatient examinations and reschedule those considered non‐essential. Communication to patients was vital, to maintain their trust in departments and to show respect. Limited symptom screening of all patients was also implemented prior to arriving and on arrival to the departments. 21 This was to ensure staff safety and prevent spread by identifying patients at higher risk of being COVID‐19 positive prior to their examination.
Change Management
The COVID‐19 pandemic challenged healthcare leaders at all levels to respond to rapid changes in healthcare delivery, staff and community safety. During the early stages of the pandemic response, contributing sites noted that managing staff emotions by clear and accurate communication was vital. It was important to alleviate staff fears through advocating for access to PPE and appropriate staffing resources. Leadership groups met frequently (often daily) to update each other regarding changes and share challenges within their subspecialties. Staff were acknowledged, listened to and supported at all times. A multi‐faceted approach to the departments’ communication strategy reduced speculation and rumour and sought to engender trust in departmental leadership. Furthermore, these succinct communication strategies alleviated change fatigue amongst staff.
The hosting of students at the outset of the pandemic was noted as an ethical dilemma for departments. Staff were concerned about their responsibility for students with regard to students being exposed to COVID‐19 and the potential risk of infection. The ethical principles of autonomy and non‐maleficence were considered with respect to students, balancing the risk of harm to themselves with the unique learning opportunity. It was important for students and their education provider to receive clear communication regarding expectations, safety processes and training requirements. Further advice and guidelines were provided across Queensland Health regarding the support of students during the pandemic. 26 , 27 The employment of students to provide assistant roles to MI professionals was also considered. 28
Maintaining patient‐centred, quality care was achieved through encouraging staff to consider how changes imposed by the pandemic affected their patient interactions. One site noted the potential for the quality of patient‐staff interactions to be diminished due to the wearing of PPE – specifically the lack of facial expressions that the patient was able to perceive and the obscuration of staff members’ name badges. Staff placed a renewed focus on showing compassion through verbal means and touch (albeit through gloves) and writing their names on the outside of gowns and protective face shields.
Staff from contributing departments are employed under provisions of the Industrial Act 2016 29 through the Health Practitioners and Dental Officers (Queensland Health) Award 30 and the Health Practitioners and Dental Officers (Queensland Health) Certified Agreement (No. 2) 2016. 31 Together, these provide for a minimum safety net of enforceable conditions of employment for employees. These industrial frameworks rightly consider change management expectations including consultation with affected staff. The timeframes set out by these provisions to ensure appropriate consultation were impractical in the rapidly changing conditions of this pandemic, where staff, patient and community safety were paramount. Future consideration should be provided within industrial frameworks to facilitate rapid and temporary changes to the workforce to ensure employee safety. Staff were well supported by Unions with their advocacy of processes for identifying vulnerable staff and the provision of PPE for staff.
Summary
Although the COVID‐19 pandemic continues globally, Australia’s implementation of the ‘flatten the curve’ strategy has thus far been considered successful. However, the potential for a ‘second wave’ should be factored into future healthcare service planning. Medical imaging services should continue to rethink and redesign workflows leveraging on lessons learnt, to prepare for future surges or pandemic events. This commentary is intended to outline key themes to be considered regarding MIDs response to a pandemic. Many Australian MIDs will already have implemented similar strategies to those described and this commentary may only serve as a limited resource. Medical imaging services must continue to work alongside the COVID‐19 threat until a vaccine becomes available. The authors’ overall intent was to provide a resource as a guide for future pandemic events. Predicting the timing and severity of future pandemic events is impossible, but it is the intention that this commentary will contribute to the corporate memory of the radiographers in our unique field with respect to how MIDs responded.
Conflict of Interest
The authors declare no conflict of interest.
Acknowledgements
The authors acknowledge their colleagues for their commitment to providing safe, person‐centred medical imaging services through the COVID‐19 pandemic: Meg McKerrow, Ben Rowney, Max Tomsia, Angela McNeill, Mark Horder, Daniel Sgualdino, Colin Jeffries, Kelly Fordyce, Jacqui Roche, Michelle Doidge, Trish Hurst, Colin Baker, Cameron Robertson, Kaye Millard and Deanna Nicholls.
J Med Radiat Sci 67(2020) 345–351
References
- 1. Redmond CE, Nicolaou S, Berger FH, Sheikh AM, Patlas MN. Emergency radiology during the COVID‐19 pandemic: the Canadian Association of Radiologists Recommendations for Practice. Can Assoc Radiol J 2020; 1–6. [DOI] [PubMed] [Google Scholar]
- 2. Tsou IYY, Liew CJY, Tan BP, et al. Planning and coordination of the radiological response to the coronavirus disease 2019 (COVID‐19) pandemic: the Singapore experience. Clin Radiol 2020; 75: 415–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Woznitza N, Nair A, Hare SS. COVID‐19: a case series to support radiographer preliminary clinical evaluation. Radiography (Lond) 2020; 26: e186–e188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Zhao Y, Xiang C, Wang S, Peng C, Zou Q, Hu J. Radiology department strategies to protect radiologic technologists against COVID19: experience from Wuhan. Eur J Radiol 2020; 127: 108996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. David SH, Esam IA, Tariq AM, et al. The continuing 2019‐nCoV epidemic threat of novel coronaviruses to global health — the latest 2019 novel coronavirus outbreak in Wuhan, China. Int J Infect Dis 2020; 91: 264–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Sohrabi C, Alsafi Z, O'Neill N, et al. World Health Organization declares global emergency: a review of the 2019 novel coronavirus (COVID‐19). Int J Surgery (London, England) 2020; 76: 71–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. World Health Organisation . Timeline of WHO's response to COVID‐19, 2020. Available from: https://www.who.int/news‐room/detail/29‐06‐2020‐covidtimeline (accessed 12 June 2020).
- 8. World Health Organisation . Coronavirus disease (COVID‐19) outbreak situation, 2020. Available from: https://www.who.int/emergencies/diseases/novel‐coronavirus‐2019 (accessed 30 June 2020).
- 9. Caly L, Druce J, Roberts J, et al. Isolation and rapid sharing of the 2019 novel coronavirus (SARS‐CoV‐2) from the first patient diagnosed with COVID‐19 in Australia. Med J Aust 2020; 212: 459–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Australian Government Department of Health . Total cases, recoveries, deaths, and new cases in the last 24 hours, 2020. Available from: https://www.health.gov.au/news/health‐alerts/novel‐coronavirus‐2019‐ncov‐health‐alert/coronavirus‐covid‐19‐current‐situation‐and‐case‐numbers#total‐cases‐recoveries‐deaths‐and‐new‐cases‐in‐the‐last‐24‐hours (accessed 30 June 2020).
- 11. Australian Government Department of Health . Australian COVID‐19 cases by source of infection, 2020. Available from: https://www.health.gov.au/news/health‐alerts/novel‐coronavirus‐2019‐ncov‐health‐alert/coronavirus‐covid‐19‐current‐situation‐and‐case‐numbers#cases‐by‐source‐of‐infection (accessed 30 June 2020).
- 12. Queensland Government . Flattening the curve, 2020. Available from: https://www.qld.gov.au/health/conditions/health‐alerts/coronavirus‐covid‐19/stay‐informed/flattening‐the‐curve (accessed 12 June 2020).
- 13. Queensland Government . Stop the spread – coronavirus (COVID‐19), 2020. Available from: https://www.qld.gov.au/health/conditions/health‐alerts/coronavirus‐covid‐19/protect‐yourself‐others/coronavirus‐prevention (accessed 13 June 2020).
- 14. Australian Government Department of Health . How to slow the spread. Available from: https://www.health.gov.au/news/health‐alerts/novel‐coronavirus‐2019‐ncov‐health‐alert/how‐to‐protect‐yourself‐and‐others‐from‐coronavirus‐covid‐19#how‐to‐slow‐the‐spread (accessed 13 June 2020).
- 15. Australian Government Department of Health . Daily and cumulative number if reported COVID‐19 cases in Australia, 2020. Available from: https://www.health.gov.au/news/health‐alerts/novel‐coronavirus‐2019‐ncov‐health‐alert/coronavirus‐covid‐19‐current‐situation‐and‐case‐numbers#daily‐reported‐cases (accessed 30 June 2020).
- 16. Queensland Health . Clinical Services Capability Framework, 2020. Available from: https://www.health.qld.gov.au/clinical‐practice/guidelines‐procedures/service‐delivery/cscf/hospitals/public (accessed 13 June 2020).
- 17. Australian Government Department of Health . Quarantine for coronavirus (COVID‐19). Available from: https://www.health.gov.au/news/health‐alerts/novel‐coronavirus‐2019‐ncov‐health‐alert/how‐to‐protect‐yourself‐and‐others‐from‐coronavirus‐covid‐19/quarantine‐for‐coronavirus‐covid‐19 (accessed 12 June 2020).
- 18. Queensland Government . Guide to identifying and supporting vulnerable employees (COVID‐19). Available from: https://www.forgov.qld.gov.au/guide‐identifying‐and‐supporting‐vulnerable‐employees‐covid‐19 (accessed 12 June 2020).
- 19. Queensland Health . Safe fitting and removal of personal protective equipment (PPE) for healthcare staff. Available from: https://www.health.qld.gov.au/__data/assets/pdf_file/0035/945755/covid19‐correct‐use‐ppe.pdf (accessed 13 June 2020).
- 20. Desborough J, Hall Dykgraaf S, Rankin D, Kidd M. The importance of consistent advice during a pandemic: an analysis of Australian advice regarding personal protective equipment in healthcare settings during COVID‐19. Aust J Gen Pract 2020; 49: 369–72. [DOI] [PubMed] [Google Scholar]
- 21. Basseal JM, Westerway SC, McAuley T. COVID‐19: Infection prevention and control guidance for all ultrasound practitioners. Australas J Ultrasound Med 2020; 23: 90–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Biomedical Technology Services ‐ Queensland Government Support Services . Radiation safety guidelines: mobile chest x‐ray examinations in wards and other temporary locations.
- 23. Queensland Health . Radiation safety and protection plans. Available from: https://www.health.qld.gov.au/system‐governance/licences/radiation‐licensing/regulation‐compliance/safety‐protection‐plan (accessed 13 June 2020).
- 24. Locatelli SM, LaVela SL, Hogan TP, Kerr AN, Weaver FM. Communication and information sharing at VA facilities during the 2009 novel H1N1 influenza pandemic. AJIC. Am J Infect Control 2012; 40: 622–6. [DOI] [PubMed] [Google Scholar]
- 25. Microsoft welcome to Microsoft teams [online]. Available from: https://docs.microsoft.com/en‐us/microsoftteams/teams‐overview (accessed 22 June 2020).
- 26. Queensland Health . Clinical Placements ‐ what's new. Available from: https://www.health.qld.gov.au/employment/clinical‐placement/whats‐new (accessed 24 June 2020).
- 27. Australian Health Practitioner Regulation Agency . National principles for clinical education during COVID‐19. Available from: https://www.ahpra.gov.au/News/COVID‐19/National‐principles‐for‐clinical‐education‐during‐COVID‐19.aspx (accessed 29 June 2020).
- 28. Allied Health Professions' Office of Queensland . Guidance Note ‐ Novel Coronavirus: Supervision for health practitioner level 1 roles. Available from: https://www.health.qld.gov.au/__data/assets/pdf_file/0028/956008/AH002338.pdf (accessed 13 June 2020).
- 29. Queensland Government . Industrial Relations Act 2016. Available from: https://www.legislation.qld.gov.au/view/html/inforce/current/act‐2016‐063 (accessed 30 June 2020).
- 30. Queensland Industrial Relations Commission . Health Practitioners and Dental Officers (Queensland Health) Award – State 2015. Available from: https://www.qirc.qld.gov.au/sites/default/files/health_practitioners_and_dental_officers_swc18.pdf?v=1542546229 (accessed 30 June 2020).
- 31. Queensland Industrial Relations Commission . Health Practitioners and Dental Officers (Queensland Health) Certified Agreement (No. 2) 2016. Available from: https://www.qirc.qld.gov.au/sites/default/files/2017_cb19.pdf?v=1542766418 (accessed 30 June 2020).


